Abstract
Background
Pancreaticoduodenectomy remains as the only treatment that offers a chance for cure in patients with pancreatic ductal adenocarcinoma (PDAC) of the head of the pancreas. In recent years, laparoscopic pancreaticoduodenectomy (LPD) has been introduced as a feasible alternative to open pancreaticoduodenectomy (OPD) when performed by experienced surgeons. This study reviews and compares perioperative results and long-term survival of patients undergoing LPD versus OPD at a single institution over a 20-year time period.
Methods
From 1995 to 2014, 612 patients underwent PD and 251 patients were found to have PDAC. These latter patients were reviewed and divided into two groups: OPD (n = 193) and LPD (n = 58). LPD was introduced in November 2008 and performed simultaneous to OPD within the remaining time period. Ninety-day perioperative outcomes and long-term survival were analyzed.
Results
Patient demographics were well matched. Operative time was significantly longer with LPD, but blood loss and transfusion rate were lower. Postoperative complications, intensive care unit stay, and overall hospital stay was similar. OPD was associated with larger tumor size; LPD was associated with greater lymph node harvest and lower lymph node ratio. LPD was performed by hand-assist method in 3 (5.2 %) patients and converted to open in 14 (24.1 %). Neoadjuvant therapy was performed in 17 (8.8 %) patients for OPD and 4 (6.9 %) for LPD. The estimated median survival was 20.3 months for OPD and 18.5 months for LPD. Long-term survival was similar for 1-, 2-, 3-, 4-, and 5-year survival for OPD (68, 40, 24, 17 and 15 %) and for LPD (67, 43, 43, 38 and 32 %), respectively.
Conclusion
LPD provides similar short-term outcomes and long-term survival to OPD in the treatment of PDAC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pancreatic ductal adenocarcinoma (PDAC) is the fourth leading cause of cancer mortality in the USA, with more than 30,000 deaths annually [1]. Despite a variety of neoadjuvant and adjuvant treatment protocols, surgical resection remains the only opportunity for cure in patients diagnosed with PDAC
Since publication of the first series of laparoscopic cholecystectomy in the late 1980s, the field of minimally invasive surgery has expanded dramatically and is now utilized for treatment of almost all gastrointestinal malignancies. Many oncological procedures have been proven not only feasible and safe, but also oncologically equivalent to traditional open procedures regarding both immediate operative benchmarks (margins, lymph node retrieval, and morbidity) and long-term outcomes (survival).
The role of laparoscopy in pancreatic surgery for PDAC had previously been primarily used for staging and palliation. Laparoscopic staging was shown at the time to be superior to radiographic cross-sectional imaging for visualizing small, occult liver, and peritoneal metastases and aided in avoiding non-therapeutic laparotomy in patients with advanced disease [2]. While the adoption of laparoscopic pancreatic surgery is still not universal, distal resections have been proven to be safe and feasible with significant advantages over the open counterpart. Laparoscopic distal pancreatectomy is routinely performed for PDAC at many centers [3]. For proximal resections, however, the complexity of the procedure and lack of data regarding clear benefits have appropriately resulted in slow adoption of the technique [4, 5].
Pancreaticoduodenectomy (PD) is one of the most complex gastrointestinal surgical procedures, including resection of the duodenum, head and uncinate process of the pancreas, and distal common bile duct, with reconstructive anastomoses involving the stomach, pancreatic remnant, and biliary tract. From the first description written by Gagner and Pomp in 1994 [6] that questioned its feasibility, several studies were published with an increasing number of laparoscopic PD (LPD). In the beginning, the majority of patients underwent PD for benign or borderline lesions. In 2007, a series reported by Palanivelu and colleagues of 45 patients with benign and malignant disease undergoing LPD demonstrated that the procedure might not only be feasible, but it might have advantages compared with open PD (OPD) [7]. An increasing number of studies also showed that patients with PDAC could be treated with minimally invasive techniques with similar oncological results [8]. For this reason, the oncological outcomes of the laparoscopic approach in pancreatic surgery have now become a major focus of studies [3, 8–11]. Other recent studies regarding LPD with vascular resections were published with similar outcomes to OPD [9, 12].
The aim of our study was to review and compare the perioperative results and long-term survival of patients with PDAC who underwent laparoscopic versus OPD at a single institution over a 20-year period.
Materials and methods
From 1995 to 2014, information regarding patients undergoing pancreatic resection was collected and retained in an institutional review board-approved database, including demographics, operative variables, postoperative outcomes, pathologic findings, and extended follow-up. Preoperative characteristics included age, sex, comorbidities, body mass index, American Society of Anesthesiologists (ASA) score, and use of neoadjuvant treatments. Operative details included operative time (incision to close of the wound), estimated blood loss, and blood product transfusion (obtained from the anesthesia record). Use of laparoscopy, vascular resection, and concomitant resection was obtained from the operative report. Postoperative outcomes were tracked for 3 months (90 days) after surgery in our comprehensive electronic medical record, and all complications were recorded and graded according to the Clavien system [13]. Final overall patient complication grade was given to the highest rated complication grade in the postoperative time period. Minor complications included grades I and II, while major complications included grades III–V. Pancreatic fistula (PF) [14], delayed gastric emptying [15], and postpancreatectomy hemorrhage [16] were scored and graded according to standard international consensus definitions. Length of stay was recorded and did not include the day of the operation, but included the day of discharge, while readmission was tracked for all patients to any hospital for 90 days after surgery. Reoperation and readmission were defined as any unplanned operation or admission, respectively, within 90 days of the primary procedure related to the pancreatic resection. Final pathology, margin status, and lymph node involvement were recorded as well. These recorded data were compared in an intent-to-treat analysis and reported below.
Preoperative workup included appropriate cross-sectional imaging to exclude distant metastases. All patients underwent a preoperative medical examination, but no specific criteria including age or comorbidity were used to determine eligibility for surgery. Similarly, no objective patient criteria were used to exclude patients from undergoing an LPD. Radiographic evidence for vascular involvement or a history of previous surgery or altered foregut anatomy was taken into consideration, but were not absolute contraindications for an attempted minimally invasive approach.
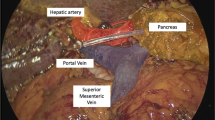
The surgical procedures were performed by multiple high-volume experienced hepato-pancreato-biliary or transplant surgeons over the course of the study period. However, since 2008, PD (including all LPD in this study) were performed only by two surgeons (J.A.S. and H.J.A.). LPD was performed as previously described [4]. Briefly, the abdomen was entered through a supraumbilical 12-mm incision, and abdominal exploration was performed to exclude metastatic disease. Five (3–12-mm trocars and 2–5-mm trocars) accessory port sites were used to perform the resection in a standard fashion. The specimen was extracted by extending the small midline incision and sent to pathology to confirm negative margins by frozen section analysis. Pneumoperitoneum was reinstated, and the reconstruction was performed laparoscopically. A single-layer hepaticojejunostomy was constructed first, followed by a two-layer duct to mucosa pancreaticojejunostomy. Lastly, gastrointestinal reconstruction was performed with an end-to-side duodenojejunostomy. A single drain was placed behind the pancreaticobiliary reconstructions.
Descriptive statistics for categorical variables were reported as frequency and percentage; continuous variables were reported median (range). Categorical variables were compared between OPD and LPD patients using Chi-square test or Fisher’s exact test, and continuous variables were compared using two sample t test or Wilcoxon rank sum test, where appropriate. Kaplan–Meier method was used to calculate 1- to 5-year survival statistics. Cox regression model was used to identify univariate and multivariate risk factors for survival. All univariately significant risk factors, together with OPD/LPD, were included in multivariate model. All statistical tests were two-sided with the alpha level set at 0.05 for statistical significance.
Results
All patients
In the study time period, 612 patients underwent PD. Of these, 251 patients underwent PD for curative intent for the diagnosis of PDAC, including OPD (n = 193) and LPD (n = 58). Prior to October of 2008, all PD for PDAC were performed by open techniques (n = 120). After this time, both OPD (n = 73) and LPD (n = 58) techniques for PDAC were performed simultaneously. Table 1 shows the demographic data. Patient sex, age, body mass index, and medical comorbidities were similar but there were significantly more patients with ASA of IV in the OPD group.
Operative variables are given in Table 2. LPD was associated with significantly longer operative time (median 375 vs 518 min, p < 0.001), but decreased blood loss (median 600 vs 250 mL, p < 0.001) and decreased use of packed red blood cell transfusions (46.6 vs 25.9 %, p = 0.005). The need for vascular resection or total pancreatectomy was similar for both groups. Use of a hand-assist technique was required in 3 (5.2 %) patients, and conversion from LPD to open was required in 14 (24.1 %). All conversions were performed for venous involvement requiring vein resection (n = 11) or adherence to the underlying vasculature from the result of pancreatitis/desmoplastic reaction (n = 3). Twenty patients (34.5 %) underwent LPD with vein resection, including 11 patients with conversion to open as mentioned previously, and nine patients underwent a totally laparoscopic vein resection.
Table 3 contains the postoperative outcomes for both groups. Overall, complications were similar between the two groups. Median hospital (9 vs 6 days, p < 0.0001) and intensive care stay (1 vs 0 days, p = 0.016) were significantly decreased in the LPD group. Major morbidity (30.1 vs 22.4 %, p = 0.170) and mortality (5.2 vs 3.4 %, p = 0.737) over 90 days was similar for both OPD and LPD, respectively. Table 4 contains the pathologic details. PDAC stage, node involvement, and negative margin rates were similar between the two groups. LPD was associated with more T1 tumors and a smaller tumor size, but a higher number of lymph node harvests. The rate of initiation of adjuvant therapy (73.5 vs 75.9 %, p = 0.858) and time to start of adjuvant therapy (55 vs 54 days, p = 0.578) were similar between OPD and LPD, respectively.
Mean follow-up was 24.5 ± 27.4 months in the OPD group and 19.6 ± 17.4 months in the LPD group. The Kaplan–Meier estimated median survival was 20.3 and 18.5 months for OPD and LPD, respectively. Table 5 and Fig. 1 show similar estimated 1- to 5-year survival for both groups. Figure 2 shows similar stage-for-stage survival for patients with stage II PDAC groups by excluding all those with stage I PDAC in both groups. On the univariate Cox proportional hazard model (Table 6), significant predictors of survival included increased tumor size (>3 cm), major complications (Clavien III–V), significant blood loss (>500 mL), positive margins (RI/R2), and elevated lymph node ratio [(LNR) > 0.2]. All other factors including LPD versus OPD were not significant predictors. On the multivariate Cox proportional model, only increased major complications, positive margins, and an elevated LNR remained significant.
Discussion
Effective treatment of PDAC has proven to be a challenging endeavor for the medical and surgical community. Non-surgical treatments concentrate on palliation while operative interventions can often be associated with high morbidity and likely eventual recurrence. Therefore, multimodality approach to the treatment of PDAC is encouraged, emphasizing treatments that maximize quality and quantity of remaining life. Significant attempts are being made to improve the performance and overall recovery from the surgical intervention with an additional focus on factors that may also improve the overall survival from PDAC. Improving the safety of the operation will potentially allow a higher percentage of patients to undergo operative treatment and gain the survival advantages, or even cure, associated with surgical intervention. LPD has been performed at our institution with the intent to improve outcomes and the overall patient’s experience while recovering from surgery. Furthermore, given the improved access and visualization of the laparoscopic approach, LPD may, in experienced hands, have the potential of resulting in a better oncologic operation. Definitive evidence of this, however, will be difficult to show due to the relatively small series and low survival in a pathologic process such as PDAC.
In our previous publication, the operation was associated with similar morbidity and mortality to OPD, but with improvements of surrogate oncologic markers such as blood loss, transfusion rates, lymph node retrieval, and LNR for patients with malignant disease [4]. Therefore, this study was performed in order to evaluate the long-term survival of patients undergoing LPD versus OPD focusing on PDAC.
As noted previously [4], the patients undergoing LPD and OPD in this study were well matched. Prior to 2008, all PD were performed open, but after 2008, both LPD and OPD were performed simultaneously without any specific inclusion/exclusion criteria other than extensive vascular involvement. LPD was also associated with longer operative times, lower estimated blood loss, and fewer overall blood transfusions than OPD. This finding was highlighted by our previous report [4] and in a meta-analysis of LPD in 2014 [5]. Similar to our study, decreased blood loss and need for subsequent blood transfusions have been shown to be independent predictors of survival after resection for PDAC [17–19]. Therefore, LPD may optimistically be associated with improved survival compared with OPD in those with PDAC. Of course, this would be best evaluated by a randomized controlled study to exclude the possibility of selection bias.
A subgroup analysis of all OPD performed from 2008 to 2014 was performed to assess whether there were any changes to our comparison to the LPD group. In this analysis, we did not find any differences in the demographics of the patients or the overall survival. However, there were small changes and improvements in this contemporary OPD group that included decreased blood transfusions, decreased intensive care and hospital stay, and increased lymph node resections than now equal LPD for the above-mentioned operative variables and outcomes. All other complications and tumor selection comparisons did not have any significant changes. This likely reflects the use of updated pancreatic protocols and pathways as well as operative technique that rarely lead to changes in long-term survival.
Similarly, others have identified postoperative complications as factors that may decrease the overall survival after pancreatectomy for PDAC [20]. This finding was confirmed in our study that showed major complications to be an independent predictor of worsened survival. Clearly, major postoperative complications will at least delay the administration of chemotherapy or the ability to tolerate the full course. In this study, postoperative outcomes were quite similar between the two groups, although hospital stay was shorter for LPD. Despite this, LPD was not associated with a shorter time interval to initiating chemotherapy or with a higher percentage of patients beginning adjuvant therapies. Another group reported a significantly higher proportion of patients who had a delay or lack of adjuvant therapy after undergoing OPD compared to those undergoing LPD [21]. Nationwide, however, it appears that minimally invasive PD is not associated with an increased use or earlier initiation of adjuvant therapy according to a recently published National Cancer Database study [10]. This may be related more to the established practice protocols of time to initiate chemotherapy after PD regardless of if the operation was performed by OPD or LPD. At our institution, adjuvant therapy is aggressively recommended for all patients within 6–8 weeks of the operation as long as the patient has sufficiently recovered from the operation, regardless of the operative approach. Therefore, it stands to reason that time to initiate or rates of receiving adjuvant therapy will only be enhanced once improved complication rates from the operation are realized.
LPD was associated with significantly increased lymph node harvest. The corresponding LNR was lower for LPD but did not reach statistical significance. LNR has been shown to predict overall survival from PDAC by our multivariate analysis and several other groups [22–25], but it is likely that overall survival is not truly affected by removing additional peripancreatic lymph nodes. Rather, a low LNR is more likely to represent more accurate lymph node staging by increasing the denominator of resected lymph nodes and potentially, a reflection on a complete and adequate oncologic resection for an aggressive malignancy such as PDAC. This factor, similar to a high negative margin rate, low blood loss, reasonable complication rate, and high adjuvant therapy use among others, is just one part of the contemporary multidisciplinary treatment of PDAC.
Overall survival, for both groups and matched stage for stage, was not statistically improved for those undergoing LPD versus OPD. Nevertheless, LPD was associated with an impressive 32 % 5-year survival. It remains to be seen whether this will continue with the accrual of more patients and further follow-up of current patients. Due to incomplete disease recurrence data in this study, it also remains to be seen whether LPD is associated with a significantly longer progression-free survival as others have found [21]. Similar to Croome et al., we also found that the technique of LPD did not reach statistical significance as a predictor of improved or worsened overall survival for PDAC after PD using univariate and multivariate analyses.
Recently, French surgeons have reported on 46 patients undergoing LPD and compared them to the same number of OPD in the same time period. They note that LPD is a long and technically difficult procedure that is associated with increased rate of PF, bleeding, and need for reoperation. They concluded that LPD is not indicated for the treatment of resectable periampullary tumors, mainly due to the increased risk of PF [11]. In our study, PF was seen at an equal and acceptably low rate for both LPD and OPD. Similarly, upon further analysis, PF was not associated with decreased overall survival as was also previously noted by other centers [26]. Overall, the results of this study conclude that LPD has comparable short-term results and is clearly not associated with worse long-term survival after PD for PDAC.
Despite our findings, this study had limitations that must be acknowledged. First, our study was a retrospective analysis. We performed an intent-to-treat analysis and based on our current practice, there are very few patients that are absolutely excluded from undergoing LPD. Nevertheless, LPD was associated with a smaller tumor size, more T1 tumors, and fewer ASA IV patients. Secondly, this study was performed over the course of a 20-year time period. While the practice has remained fairly stable, there have certainly been improvements over this time frame in preoperative imaging studies, surgical technique, perioperative care, as well as neoadjuvant and adjuvant therapy administration. However, time period analysis did not show any difference in survival for patients treated in the first half of the series compared to the second half. Thirdly, many patients undergoing PD at our institution undergo adjuvant therapy at outside facilities. Therefore, full adjuvant therapy details including completeness of treatment, tolerance of dull dose treatments, and recurrence data are limited. In fact, a recent subanalysis of the ESPAC-3 study suggests that the completion of adjuvant therapies rather than the earlier initiation was a more important independent factor for survival prognosis [27]. Certainly, a comprehensive, prospective, multicenter, randomized study would be optimal to better underline the role of a minimally invasive approach in the treatment of pancreatic adenocarcinoma.
In conclusion, this study shows that LPD appears to be safe and feasible with similar short-term outcomes and long-term survival to OPD in the treatment of PDAC. Moreover, as LPD is often characterized by less intraoperative blood loss, lower transfusion rates, and improved lymph node harvests, a survival benefit for this technique may be conceivable if analyzed in greater numbers over a long period of time. Nonetheless, in an attempt to optimize all surgeon-related factors, focused efforts brought on by concepts acquired during performance of LPD conveyed to OPD have also resulted in improvements in OPD seen in the past few years.
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
Kubota K (2011) Recent advances and limitations of surgical treatment for pancreatic cancer. World J Clin Oncol 2:225–228
Stauffer JA, Coppola A, Mody K, Asbun HJ (2016) Laparoscopic versus open distal pancreatectomy for pancreatic adenocarcinoma. World J Surg 40:1477–1484
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the accordion severity grading system. J Am Coll Surg 215:810–819
Correa-Gallego C, Dinkelspiel HE, Sulimanoff I, Fisher S, Vinuela EF, Kingham TP, Fong Y, DeMatteo RP, D’Angelica MI, Jarnagin WR, Allen PJ (2014) Minimally-invasive vs open pancreaticoduodenectomy: systematic review and meta-analysis. J Am Coll Surg 218:129–139
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8:408–410
Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Rajapandian S, Madhankumar MV (2007) Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg 205:222–230
Adam MA, Choudhury K, Dinan MA, Reed SD, Scheri RP, Blazer DG 3rd, Roman SA, Sosa JA (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262:372–377
Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, Kendrick ML (2015) Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg 19:189–194 (discussion 194)
Nussbaum DP, Adam MA, Youngwirth LM, Ganapathi AM, Roman SA, Tyler DS, Sosa JA, Blazer DG 3rd (2016) Minimally invasive pancreaticoduodenectomy does not improve use or time to initiation of adjuvant chemotherapy for patients with pancreatic adenocarcinoma. Ann Surg Oncol 23:1026–1033
Dokmak S, Fteriche FS, Aussilhou B, Bensafta Y, Levy P, Ruszniewski P, Belghiti J, Sauvanet A (2015) Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 220:831–838
Palanisamy S, Deuri B, Naidu SB, Vaiyapurigoundar Palanisamy N, Natesan AV, Palanivelu PR, Parthasarathy R, Palanivelu C (2015) Major venous resection and reconstruction using a minimally invasive approach during laparoscopic pancreaticoduodenectomy: one step forward. Asian J Endosc Surg 8:468–472
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Buchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25
Kneuertz PJ, Patel SH, Chu CK, Maithel SK, Sarmiento JM, Delman KA, Staley CA 3rd, Kooby DA (2011) Effects of perioperative red blood cell transfusion on disease recurrence and survival after pancreaticoduodenectomy for ductal adenocarcinoma. Ann Surg Oncol 18:1327–1334
Sutton JM, Kooby DA, Wilson GC, Squires MH 3rd, Hanseman DJ, Maithel SK, Bentrem DJ, Weber SM, Cho CS, Winslow ER, Scoggins CR, Martin RC 2nd, Kim HJ, Baker JJ, Merchant NB, Parikh AA, Abbott DE, Edwards MJ, Ahmad SA (2014) Perioperative blood transfusion is associated with decreased survival in patients undergoing pancreaticoduodenectomy for pancreatic adenocarcinoma: a multi-institutional study. J Gastrointest Surg 18:1575–1587
Nagai S, Fujii T, Kodera Y, Kanda M, Sahin TT, Kanzaki A, Yamada S, Sugimoto H, Nomoto S, Takeda S, Morita S, Nakao A (2011) Impact of operative blood loss on survival in invasive ductal adenocarcinoma of the pancreas. Pancreas 40:3–9
Kang CM, Kim DH, Choi GH, Kim KS, Choi JS, Lee WJ (2009) Detrimental effect of postoperative complications on oncologic efficacy of R0 pancreatectomy in ductal adenocarcinoma of the pancreas. J Gastrointest Surg 13:907–914
Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, Kendrick ML (2014) Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 260:633–638 (discussion 638-640)
Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD, Wolfgang C, Hruban RH, Schulick RD, Yeo CJ, Choti MA (2007) Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 141:610–618
Riediger H, Keck T, Wellner U, Zur Hausen A, Adam U, Hopt UT, Makowiec F (2009) The lymph node ratio is the strongest prognostic factor after resection of pancreatic cancer. J Gastrointest Surg 13:1337–1344
Slidell MB, Chang DC, Cameron JL, Wolfgang C, Herman JM, Schulick RD, Choti MA, Pawlik TM (2008) Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol 15:165–174
Zhan HX, Xu JW, Wang L, Zhang GY, Hu SY (2015) Lymph node ratio is an independent prognostic factor for patients after resection of pancreatic cancer. World J Surg Oncol 13:105
Ausania F, Cook N, Jamieson N, Huguet E, Jah A, Praseedom R (2010) Impact of pancreatic leaks on survival following pancreaticoduodenectomy. JOP 11:226–229
Valle JW, Palmer D, Jackson R, Cox T, Neoptolemos JP, Ghaneh P, Rawcliffe CL, Bassi C, Stocken DD, Cunningham D, O’Reilly D, Goldstein D, Robinson BA, Karapetis C, Scarfe A, Lacaine F, Sand J, Izbicki JR, Mayerle J, Dervenis C, Olah A, Butturini G, Lind PA, Middleton MR, Anthoney A, Sumpter K, Carter R, Buchler MW (2014) Optimal duration and timing of adjuvant chemotherapy after definitive surgery for ductal adenocarcinoma of the pancreas: ongoing lessons from the ESPAC-3 study. J Clin Oncol 32:504–512
Acknowledgments
The authors would like to acknowledge Mauricia Buchanan for her assistance in collecting data for the purpose of this study and the Mayo Clinic in Florida Division of Biomedical Statistics and Informatics for the statistical analysis.
Funding
Funding for statistical support provided by the Cancer Focused Research team at Mayo Clinic in Jacksonville, Florida.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Stauffer, Coppola, Villacreses, Johnson, Mody, and Asbun and Mrs. Li have no conflicts of interest or financial ties to disclose in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Stauffer, J.A., Coppola, A., Villacreses, D. et al. Laparoscopic versus open pancreaticoduodenectomy for pancreatic adenocarcinoma: long-term results at a single institution. Surg Endosc 31, 2233–2241 (2017). https://doi.org/10.1007/s00464-016-5222-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5222-1