Abstract
Background
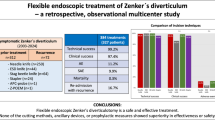
Currently there are three main treatment options for Zenker’s diverticulum (ZD): surgery, rigid endoscopy and flexible endoscopy. After primary success, recurrence can be as high as 19 % for surgery, 12.8 % for rigid endoscopy and 20 % for flexible endoscopy. Flexible endoscopy may represent an ideal treatment option for recurring ZD. The aims of this paper are to evaluate the efficacy and safety of flexible endotherapy for recurring ZD after surgery and/or endoscopic stapling and to compare the treatment outcome between naive and recurring patients.
Methods
Data on patients that underwent flexible endotherapy for ZD between January 2010 and January 2015 were collected. Patients were divided into those with recurrences after surgery and/or endoscopic stapling and those who did not have previous treatments. Dysphagia, regurgitation, and respiratory symptom severity before the procedure were graded. The outcome parameters were: complications, symptom improvement after the first treatment, number of treatment sessions, rate of complete remission and relapses. These parameters were then compared between patients groups.
Results
Twenty-five recurring patients were included. Treatment was carried out successfully in all patients. Two adverse events occurred; they were successfully managed conservatively. After the first treatment, there was a significant reduction in dysphagia, regurgitation and respiratory symptoms scores. The median number of treatments was 1 (IQR 0.25, range 1–3): symptom remission was achieved in 84 % patients and partial improvement in 16 %. Relapsing symptoms occurred in 20 % patients; they were successfully managed with an additional treatment session. Results were compared with data on 34 consecutive naive patients treated within the same time span; no differences of the outcome parameters were revealed.
Conclusions
Flexible endotherapy for ZD recurrences after surgery and endoscopic stapling appears to be safe and effective, and its efficacy and safety profile seems to be comparable between recurring and naive patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Zenker’s diverticulum (ZD) is an outpouching of mucosa and submucosa that develops in an area of weakness of the lower posterior hypopharynx known as Killian’s triangle. It has an estimated prevalence between 0.01 and 0.11 % of the general population, and it develops mainly in elderly males [1, 2]. Its pathogenesis is still poorly defined: it is believed, however, that increased intraluminal pressure in conjunction with an impaired relaxation of the upper esophageal sphincter plays a pivotal role in promoting the herniation of mucosa and submucosa through Killian’s triangle [3].
The main symptoms attributable to ZD are dysphagia, regurgitation and cough/aspiration, although it lead to more severe but rare complications such as aspiration pneumonia, weight loss, fistulization, bleeding and vocal cords paralysis [1–3].
Currently there are three main treatment options for ZD: open surgery (i.e., transcervical diverticulectomy/diverticulopexy with myotomy of the cricopharyngeal muscle), rigid endoscopy (i.e., endoscopic stapling or CO2 laser treatment) and flexible endoscopy. All treatment options have a satisfactory success rate (80–100 % for surgery, 90–100 % for rigid endoscopy and 43–100 % for flexible endoscopy), but symptom recurrence can be as high as 19 % for surgery, 12.8 % for rigid endoscopy and 20 % for flexible endoscopy [2, 4–7]. In addition surgery is associated with significant morbidity and mortality rates, which can be as high as 30 and 3 %, respectively. Reported morbidity for rigid endoscopy is 3 and 1.5 % for flexible endoscopy [8–10].
Treatment of recurrences after surgery or endoscopic stapling can be technically challenging. Endoscopic stapling of small residual pouches poses some issues: an adequate bite of the common wall between the diverticulum and the esophagus cannot be achieved in a significant number of patients, and a higher risk of perforation is encountered when small pouches are stapled [11–13]. Moreover, the staple over staple effect may lead to unpredictable scarring and fibrosis that can lead to persisting dysphagia despite an apparent success of the procedure [14]. In addition, surgery is an invasive procedure and aging patients may not be fit for repeated surgery due to associated comorbidities.
Flexible endoscopy may represent an optimal treatment option for patients relapsing after either surgery or endoscopic stapling. This approach can be effectively used to treat small diverticuli and does not require general anesthesia or neck hyperextension [15]. In addition, flexible endoscopic treatment allows shorter procedure time and a reduced hospital stay. These characteristics make this approach ideal for elderly patients with comorbidities or patients with small residual pouches that may not always be suitable for surgery or endoscopic stapling. While many published series on flexible endoscopic treatment for ZD quote successful treatment of relapsing patients after surgery or rigid endoscopic treatment, there is actually no data on the outcome of the procedure for this specific subset of patients [15–22].
The primary aim of this study is to evaluate our experience with flexible endoscopic treatment of ZD in patients with recurrences after surgery or endoscopic stapling. The secondary aim is to compare the outcomes of treatment carried out in naïve patients (i.e., patients that did not have previous treatments for ZD) and those treated for a recurrence.
Materials and methods
Patients and ethics considerations
We retrospectively evaluated data on patients that underwent flexible endoscopic septum division for a symptomatic ZD at our department from January 2010 to January 2015 and matched our inclusion and exclusion criteria (Table 1). Patients were fully informed of the aims and nature of the procedure, and written informed consent for the procedure and data collection were obtained. This study was carried out according to the principles of the Declaration of Helsinki and of good clinical practice. Data were collected retrospectively hence ethics committee approval was not required, according to local regulations.
Demographic and clinical information were collected, and patients were subsequently divided into those who underwent previous treatments (either surgery or endoscopic stapling) and those who did not. Before the procedure and on every follow-up, dysphagia was assessed with the Dakkak and Bennett scale and regurgitation and respiratory symptoms with a numeric analogue scale (NAS) (Table 2) [23]. All patients underwent a barium esophagography prior to the procedure to characterize the diverticulum. Morton and Bartley classification was used to measure the size of diverticula [24].
Endoscopic procedure
All procedures were performed under deep sedation with a continuous infusion of propofol. Fentanyl citrate was used for analgesia. A 9.9-mm endoscope (GIF-H180 J; Olympus, Tokyo, Japan) was carefully introduced until the diverticulum was visible. With the guidance of the endoscope, a soft duck bill diverticuloscope (ZDO-22-30; Cook Medical, Winston-Salem, North Carolina) was introduced to expose and straddle the diverticular septum. As per our standard protocol, if the horizontal length of septum was 2 cm or less, a single incision along the midline of the septum was carried out to dissect mucosa and fibers of cricopharyngeal muscle (CP). In case of larger diverticula (with a septum length >2 cm), two parallel incisions approximately 1 cm deep were performed and a monopolar snare was used to remove the part of septum in between. One to three clips were then placed at the bottom of the incision to prevent mucosal dissection from underlying muscle and perforation. The depth of the incisions was balanced in order to achieve a near complete horizontal CP myotomy without excessive risk of perforation. After the procedure, PPI, analgesics and antiemetics were administered. Routine antibiotic prophylaxis was not used.
Post-procedure esophagrams were carried out to rule out perforation and to assess esophageal transit on the day of the procedure. Inflammation markers (CRP and WBC) were measured on blood samples 6, 12 and 24 h from the procedure. The patients were allowed to have liquids on day 2 and were discharged if no adverse events occurred and the esophagrams excluded perforations. They were instructed to have a soft/liquid diet for the first week after the procedure. Patients were then contacted via telephone 7 days from the procedure to assess their conditions and were assessed at our outpatient clinic 2 months from the procedure.
Afterward patients were contacted via telephone at 6-months intervals to assess their symptoms and to plan additional treatments in case of relapses.
Outcome parameters and statistics
Descriptive statistics were expressed as median, interquartile range (IQR) and range for continuous variables, and the scores were considered as continuous variables. The outcome parameters used in this study are rate of complications, symptom improvement after the first treatment, number of treatments required to achieve remission, rate of complete symptom remission after a treatment and rate of relapse. Complications were graded with the classification by Cotton et al. [25]. A relapse was defined as a symptom recurrence after complete remission or as a symptom worsening after partial remission. The Pearson’s Chi-square test or Fisher’s exact test, if appropriate, were used for categorical variables, and the Mann–Whitney U test was used for continuous variables. The same test was used to determine score differences before and after treatment. A p value <.05 was considered as statistically significant. Statistical analysis was carried out using R v 2.1.3.
Results
Between January 2010 and January 2015, 69 consecutive patients underwent flexible endoscopic septum division. After checking for inclusion and exclusion criteria, a total of 59 patients were included in the study. Among them, 25 had previous treatments at other institutions (17 endoscopic stapling, eight surgeries). Demographic and clinical information is summarized in Table 3. No significant differences in terms of sex, age, diverticulum size and symptoms scores were observed between both patient groups.
Outcome of flexible endoscopic treatment of recurring ZD
Double-incision technique was used in 18 patients (72 %), while in the remaining seven (28 %) single-incision technique was used. Treatment was carried out successfully in all patients. The Needle knife (Cook Medical, Winston-Salem, North Carolina) was used in six patients, the Hook knife (Olympus, Tokyo, Japan) in nine and the SB knife (Sumitomo-Bakelite, Tokyo, Japan) in 15. Peri-procedural complications developed in two patients (8 %): one micro-perforation (i.e., not visible during endoscopy but revealed by the post-procedural esophagram) and one case of moderate bleeding. The micro-perforation was treated conservatively by keeping the patient NPO and treated with intravenous broad spectrum antibiotics and parenteral nutrition. An esophagram carried out 7 days after the procedure revealed a complete healing of the perforation, and the patient was discharged the day after. The bleeding was successfully stopped by using hemostatic forceps (Coagrasper; Olympus, Tokyo, Japan). The patient did not require blood transfusions. The patient was kept NPO and under observation for 48 h and then discharged. Both adverse events were graded as mild.
After the first treatment, there was a significant reduction in dysphagia (p < .01), regurgitation (p < .01) and respiratory symptom scores (p < .01) (Table 4). Eleven patients, despite improvement, had residual symptoms. Among them, seven underwent further treatment session resulting in symptom remission in all, and four declined further treatment (Table 5). The median number of treatment sessions was 1 (IQR 0.25; range 1–3): symptom remission was achieved in 21 patients (84 %), while four (16 %) had a substantial symptom improvement: they were able to have an almost free diet hence declined further treatment. The median follow-up duration was 18 months (IQR 29, range 6–58). Five patients had recurrence of symptoms after flexible endoscopic treatment (median time of recurrence 17 months, IQR 12, range 6–42), successfully treated with an additional treatment, without any complications. The overall outcome of the procedure is summarized in Fig. 1.
Comparison of outcomes between naïve patient and patients with recurring ZD
No differences were found in techniques used (p = .99) or devices employed (p = .11) or follow-up durations (p = .91) between patient groups. No significant differences were found in terms of rate of complications (p = .99), patients requiring extra treatments (p = .36), rate of remissions (p = .99) and rate of relapses (p = .50) between patient groups (Table 6).
Discussion
There is limited published evidence on the outcome of treatment of ZD relapses after surgery and endoscopic stapling. Studies on the outcome of surgery and/or rigid endoscopic treatment for ZD relapses have been published in the past (Table 7) [10–13, 26]. Both treatment options appear to be safe and effective. However, data on either follow-up or symptom relief are limited.
Flexible endoscopic treatment has, however, many significant advantages in comparison with surgery and rigid endoscopic treatment. It is minimally invasive, does not require general anesthesia and can be repeated without additional risks [15]. In addition, it is effective in treating small diverticular pouches that may not be easily accessible with surgical or and endoscopic stapling techniques.
This is the first series of patients treated with flexible endoscopic septum division for relapsing symptoms after ZD surgery or endoscopic stapling. All treated patients had a significant symptom improvement, and complete symptom relief was achieved in 84 % of them. The occurrence of complication was relatively low, and no major, life threatening complications occurred. During follow-up, relapses occurred in five patients after a median of 17 months. All relapsing patients were successfully treated with one additional treatment session and remained symptom-free throughout the follow-up period.
The efficacy and safety profile of flexible endoscopic septum division appear to be comparable between naive and relapsing patients, with no significant differences in terms of complications, symptom remission and relapses requiring additional treatment (Table 5). An interesting observation was that patients who relapsed after surgery/stapling required more flexible endotherapy sessions in order to achieve symptom remission when compared with naive patients, although this did not reach statistical significance. This can be partially explained by the relatively limited sample size, but another plausible explanation could be that due to fibrosis and scarring from previous treatment, persisting ZD may be more resilient to septum division. Moreover, the limited follow-up duration could have prevented us from detecting additional required treatments in this subset of patients. The overall outcome of the procedure was, however, good, and all relapses were treated successfully. For these reasons, previous surgery and/or endoscopic stapling should not be viewed as a contraindication for flexible endoscopic septum division in patients with ZD. Flexible endoscopic treatment of ZD relapses after surgery can be accomplished without modifying the technique. The presence of metallic staples in patients relapsing after rigid endoscopic treatment requires additional considerations: depending on the configuration of the residual septum and on the positioning of the staples, the incision (for either the single or the double technique) can be performed medially to the staples (i.e., leaving them in place). If there is a sizable portion of the septum below the staples (i.e., 1 cm or more), the “stapled” portion of the septum can be removed with the double-incision technique. In any case, the presence of staples does not pose significant issues when performing flexible endoscopic septum division.
Our results are comparable with other series of patients treated for ZD relapses with surgery and/or stapling in terms of success, efficacy and safety alike [14, 16–20]. However, flexible endoscopy has significant advantages over other treatment options: it is the least invasive option, can be repeated in case of further relapses and does not pose increased technical challenge in patients who underwent surgery and/or endoscopic stapling beforehand.
In our series, we encountered no significant differences of the size of the diverticular pouch between naive and relapsing patients. This can be explained by the limited sample size of our series, and another plausible explanation could be the fact that patients previously treated with endoscopic stapling accounted for the majority of relapsing patients (68 %). On contrary to surgery, the core technique of endoscopic stapling is the transection of the diverticular septum; hence, there is no change in the actual size of the diverticular pouch. Hence, patients relapsing after endoscopic stapling treatment are likely to have diverticular pouches comparable, in terms of size, to naive patients.
The main limitations of our study are the limited sample size and relatively short follow-up. The relatively limited follow-up of our series could potentially have prevented the detection of additional relapses after flexible endoscopic treatment and of secondary relapses (i.e., further relapses after a first relapse).
Conclusion
This is the first study with the largest number of patients to evaluate flexible endoscopic treatment of ZD with recurrence after surgery and endoscopic stapling that also compared the outcome with the naïve patients (i.e., patients that did not have previous treatments for ZD). Our results clearly suggest that the flexible endotherapy is a safe, feasible and efficient treatment in patient with recurrence after surgery or rigid endoscopic stapling. Based on our result and experience, we propose flexible endotherapy should be considered as first line treatment in patients with ZD who relapse after surgery. Larger prospective studies with longer follow-ups are required to fully evaluate this treatment option for patients with relapsing ZD.
References
Siddiq MA, Sood S, Strachan D (2001) Pharyngeal pouch (Zenker’s diverticulum). Postgrad Med J 77:506–511
Ferreira LE, Simmons DT, Baron TH (2008) Zenker’s diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus 21:1–8
Cook IJ, Gabb M, Panagopoulos V, Jamieson GG, Dodds WJ, Dent J, Shearman DJ (1992) Pharyngeal (Zenker’s) diverticulum is a disorder of upper esophageal sphincter opening. Gastroenterology 103:1229–1235
Dzeletovic I, Ekbom DC, Baron TH (2012) Flexible endoscopic and surgical management of Zenker’s diverticulum. Expert Rev Gastroenterol Hepatol 6:449–465
Costantini M, Zaninotto G, Rizzetto C, Narne S, Ancona E (2004) Oesophageal diverticula. Best Pract Res Clin Gastroenterol 18:3–17
Mantsopoulos K, Psychogios G, Künzel J, Zenk J, Iro H, Koch M (2012) Evaluation of the different transcervical approaches for Zenker diverticulum. Otolaryngol Head Neck Surg 146:725–729
Leong SC, Wilkie MD, Webb CJ (2012) Endoscopic stapling of Zenker’s diverticulum: establishing national baselines for auditing clinical outcomes in the United Kingdom. Eur Arch Otorhinolaryngol 269:1877–1884
Chang CY, Payyapilli RJ, Scher RL (2003) Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope 113:957–965
Bonafede JP, Lavertu P, Wood BG, Eliachar I (1997) Surgical outcome in 87 patients with Zenker’s diverticulum. Laryngoscope 107:720–725
Dzeletovic I, Ekbom DC, Baron TH (2013) Flexible endoscopic and surgical management of Zenker’s diverticulum. Expert Rev Gastroenterol Hepatol 6(4):449–466
Scher RL (2003) Endoscopic staple diverticulostomy for recurrent Zenker’s diverticulum. Laryngoscope 113:63–67
Visosky AM, Parke RB, Donovan DT (2008) Endoscopic management of Zenker’s diverticulum: factors predictive of success or failure. Ann Otol Rhinol Laryngol 117:531–553
Casso C, Lalam M, Ghosh S, Timms M (2006) Endoscopic stapling diverticulotomy: an audit of difficulties, outcome, and patient satisfaction. Otolaryngol Head Neck Surg 134:288–293
Buchanan MA, Riffat F, Mahrous AK, Fish BM, Jani P (2013) Endoscopic or external approach revision surgery for pharyngeal pouch following primary endoscopic stapling: which is the favoured approach? Eur Arch Otol Laryngol 270(5):1707–1710
Battaglia G, Antonello A, Realdon S, Cesarotto M, Zanatta L, Ishaq S (2015). Flexible endoscopic treatment for Zenker’s diverticulum with the SB Knife. Preliminary results from a single centre experience. Dig Endosc. doi:10.1111/den.12490
Mulder CJ, Costamagna G, Sakai P (2001) Zenker’s diverticulum: treatment using a flexible endoscope. Endoscopy 33:991–997
Hashiba K, De Paula AL, Da Silva JG, Cappellanes CA, Moribe D, Castillo CF, Brasil HA (1999) Endoscopic treatment of Zenker’s diverticulum. Gastrointest Endosc 49(1):93–97
Evrard S, Le Moine O, Hassid S, Devière J (2003) Zenker’s diverticulum: a new endoscopic treatment with a soft diverticuloscope. Gastrointest Endosc 58(1):116–120
Rabenstein T, May A, Michel J, Manner H, Pech O, Gossner L, Ell C (2007) Argon plasma coagulation for flexible endoscopic Zenker’s diverticulotomy. Endoscopy 39:141–145
Huberty V, El Bacha S, Blero D, Le Moine O, Hassid S, Devière J (2013) Endoscopic treatment for Zenker’s diverticulum: long-term results (with video). Gastrointest Endosc 77(5):701–707
Laquière A, Grandval P, Arpurt JP, Boulant J, Belon S, Aboukheir S, Laugier R, Penaranda G, Curel L, Boustière C (2015). Interest of submucosal dissection knife for endoscopic treatment of Zenker’s diverticulum. Surg Endosc 29(9):2802–2810
Verdonck J, Morton RP (2014) Systematic review on treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-014-3267-0
Dakkak M, Bennett JR (1992) A new dysphagia score with objective validation. J Clin Gastroenterol 14(2):99–100
Morton RP, Bartley JR (1993) Inversion of Zenker’s diverticulum: the preferred option. Head Neck 15(3):253–256
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Adam SI, Paskhover B, Sasaki CT (2013) Revision Zenker diverticulum: laser versus stapler outcomes following initial endoscopic failure. Ann Otol Rhinol Laryngol 122(4):247–253
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Author G. Battaglia received 10 SB knives by Sumitomo-Bakelite Ltd. (Tokyo, Japan) as a free trial sample. Other Authors (A. Antonello, S. Ishaq, L. Zanatta, M. Cesarotto, M. Costantini) have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Antonello, A., Ishaq, S., Zanatta, L. et al. The role of flexible endotherapy for the treatment of recurrent Zenker’s diverticula after surgery and endoscopic stapling. Surg Endosc 30, 2351–2357 (2016). https://doi.org/10.1007/s00464-015-4482-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4482-5