Abstract
Endoscopic stapling of Zenker’s diverticulum (ZD) is now established practice in the UK and is routinely performed by the vast majority of otolaryngologists. Both The National Confidential Enquiry into Peri-Operative Deaths and the National Institute for Health and Clinical Excellence recommended that the procedure be undertaken at specialist centres and that each department should audit their respective outcomes. Despite the abundance of review articles, it remains unclear what variables a meaningful audit is required to collate and what gold standards every department in the UK undertaking surgery for ZD should aspire to achieve. The objective was to review the outcomes of endoscopic stapling of Zenker’s diverticulum at this institution. In addition, a review of other UK departments was undertaken to formulate minimum clinical standards and recommendations of best practice. Review of patient case notes and a structured search of PubMed were used as materials. Fifteen retrospective case series were identified from the literature search which fulfilled the inclusion criteria. Fifty-one patients were identified from the present audit. When these were added to the review, a total of 585 patients were available for meta-analysis. 540 (92.3%) were successfully stapled. Forty-five (7.7%) procedures were abandoned intra-operatively. The most common reason was difficulty assessing the small pouch. The majority of patients (92%) had resumed oral intake by the second post-operative day. Most patients (87%) were discharged by the second post-operative day. Outcomes were good with over 90% reporting resolved or significantly improved symptoms. Minor complications included dental trauma, transient hoarseness and sore throat causing delayed resumption of oral intake. The overall perforation rate was 4.8%. One death was reported. In conclusion endoscopic stapling of pharyngeal pouch is a safe procedure that is associated with good outcomes and low complication rates. No death has been reported since 2000 in the UK. The data presented in this review represent current clinical standards reported over the past 15 years by UK departments and serve as a useful benchmark for any future audits undertaken. Level of evidence 3A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The number of operations on Zenker’s diverticulum (ZD) in England, United Kingdom (UK) has seen an upward trend over the past 10 years (Fig. 1). The appreciation of the pivotal role of the cricopharyngeus muscle in the pathogenesis of pouch formation has shifted the emphasis on treatment from diverticulotomy to cricopharyngeal myotomy. The development of endoscopic techniques, particularly endoscopic stapling, has led to the re-evaluation of the treatment of ZD. This technique has gained increasing popularity within the past 20 years and has revolutionised surgical management in the UK. In 1996, up to 15% of otolaryngologists in the UK were familiar with this technique [1]. It is now established practice in the UK, routinely performed by 89% of otolaryngologists surveyed[2]. In fact, 83% of the surgeons regard this technique as first choice treatment of ZD.
Trends in operations on pharyngeal pouch (OPCS code E23.3) in England from 2000 to 2010 according to age groups. (source: Hospital Episode Statistics, http://www.hesonline.nhs.uk)
Both The National Confidential Enquiry into Peri-Operative Deaths (NCEPOD) [3] and the National Institute for Health and Clinical Excellence (NICE) [4] recommended that the procedure be undertaken at specialist centres and that each department should audit their respective outcomes. However, surgical outcomes have been sporadically reported in the literature. This is compounded by dissimilar clinical data presented by each study which is frequently derived from small study cohorts. Despite the abundance of review articles, it remains unclear what variables a meaningful audit is required to collate and what gold standards UK departments should aspire to achieve.
The aim of this study was to review the surgical and patient reported outcomes of endoscopic stapling of ZD at our institution. In addition, a review of other UK departments was undertaken to formulate minimum clinical standards and recommendations of best practice. It is envisaged that this review will inform on any future audits undertaken which offers a UK specific perspective and context. This will also enhance our ability to counsel patients regarding peri-operative care, complications and expected outcomes as well as facilitate the development of patient information material.
Methods
This was a retrospective study, approved by the institution’s Clinical Information and Audit Department (reference 3968-10/11). Patients were identified from electronic hospital database and cross-referenced with theatre records, operation lists and patient case notes (hard copy, micro-film). The review period was restricted from January 1999 to June 2011. The following Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures (OPCS 4th revision) codes were used: E23.2 Operations on pharyngeal pouch, Y26.3 Stapling of organ NOC, Y76.3 Endoscopic approach to other body cavity. The clinical and surgical variables audited were determined by first reviewing previously published studies. A systematic search of the US Library of Medicine (PubMed) was performed using MeSH keywords (Zenker diverticulum, pharynx, endoscopy). The literature review was limited from 1995 to 2010, and restricted to English-language articles only. Citations and abstracts were then reviewed for relevance. Only studies reporting outcomes following endoscopic stapling from UK departments were eligible for inclusion. Citations without an abstract, review articles and correspondence letters were excluded, as were single case reports.
A number of variables were defined to maintain uniformity in the meta-analysis. The day of the operation was defined as Day 0. Thus, a patient who was discharged the day after the operation was regarded to have stayed in hospital for 1 day. Abandoned procedures were those where endoscopic stapling could not be performed intra-operatively due to technical reasons and where an alternative procedure was then undertaken (e.g. external diverticulotomy, CO2 laser). Such procedures were categorised as conversion.
Results
Fifteen retrospective case series were identified which fulfilled the inclusion criteria [5–19]. Four case reports detailing complications during endoscopic stapling were excluded from the meta-analysis as it was not possible to determine the overall rate of complications from the respective departments [20–23]. A correspondence letter proposing suitable criteria for day case pharyngeal pouch stapling was also excluded for lack of patient data [24], as was another which described a novel endoscopic surgical technique [25].
Patient demographics, selection criteria and pre-operative investigations
Fifty-one patients were identified from the present audit. When these were added to the review (n = 534), a total of 585 patients were available for meta-analysis. The male to female ratio was 2:1, with a mean age of 72.8 years (range 49–86). Patients commonly presented with dysphagia (73%), regurgitation (36%) and weight loss (15%). Other less common presenting symptoms included recurrent chest infections, globus pharyngeus, choking sensation and hoarseness. A neck lump was uncommon and was observed in only 0.2% of all cases. All patients were diagnosed following barium swallow or videofluoroscopy. The decision for surgery was based solely on patient symptomatology.
Peri-operative details
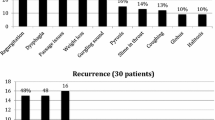
The mean duration of the operation was 22 min (range 10–35). Antibiotics were not routinely given. A naso-gastric tube (NGT) was not routinely inserted unless post-operative nutritional support was required or there was concern about the possibility of perforation. Of the 585 cases reviewed, 540 (92.3%) were successfully stapled. Forty-five (7.7%) procedures were abandoned intra-operatively. The most common reason was difficulty accessing the small pouch. This was encountered in 42% of the abandoned cases (Fig. 2). Access to the pharyngeal pouch was also compounded by stiff cervical spine (27%) and prominent dentition (18%). Of these 45 cases, 24 (53.3%) were converted to an alternative procedure: external approach in 23 patients and 1 patient had endoscopic CO2 laser surgery. These procedures were either performed during the same anaesthetic or at a later date following further discussion with the patient. Departments that proceeded with an external procedure in the same anaesthetic would routinely incorporate this possibility into their consent process.
In uncomplicated surgery, 84% of patients had resumed oral intake within 24 h of surgery and 92% by the second post-operative day (Fig. 3). In earlier studies, patients were kept nil-by-mouth for longer periods after surgery for observation. Only a handful of cases were day case procedures (Fig. 4). Two-thirds of patients were discharged the day after surgery and 87% were discharged by the second post-operative day. Delays in discharge amongst patients who had uncomplicated surgery were due to social circumstances, slow resumption of oral intake and the requirement for nutritional supplementation via NGT feeding.
Complications
A total of 52 complications were reported giving an overall complication rate of 9.6% (Table 1). The most commonly reported minor complication was dental trauma (0.9%), followed by mucosal laceration (0.6%) and post-operative chest pain (0.4%). There was one case where the NGT was inserted into the oesophagus as a guide but was inadvertently stapled. These complications were managed conservatively although hospital discharge was delayed in those who had slow resumption of oral intake.
The most common major complication was perforation of the oesophagus or pouch, observed in 26 patients (4.8%). Most of these patients (18/26) were managed conservatively with intravenous antibiotics and NGT feeding. There were also seven reported cases of surgical emphysema, one pneumothorax and one neck abscess; all of which were managed conservatively. Hospital discharge was expectantly delayed, ranging from 7 to 31 days. The remaining eight patients who suffered an iatrogenic perforation had surgical repair—four external approach repair and three endoscopic. One patient succumbed to mediastinitis following a pectoralis major flap repair of the perforation. This patient underwent uneventful stapling and was discharged the next day but returned to hospital 48 h later with a large pharyngeal perforation. Thus, the mortality rate following endoscopic stapling of pharyngeal pouch in the available data set was 0.2%.
Outcomes
The follow-up period varied widely between the studies, ranging from 1 to 79 months. None of the studies utilised a validated questionnaire or quality of life tool to measure the benefit of surgery. Symptom resolution following surgery was subjectively reported as either resolved, improved, no change or worse. Resolution was reported by 73% of patients, whilst another 18% reported improved symptoms following the surgery. No change in dysphagia was reported by 8% of patients and 1% noted that symptoms were worse after surgery.
A total of 69 patients presented with persistent or recurrent symptoms during the follow-up period. It was not always possible to determine from the 15 studies if all patients who had surgery remained alive during the follow-up period or if those who had abandoned endoscopic procedures were included in the follow-up data. If, however, it was assumed that all 69 had successful stapling then the recurrence rate was 12.8% (69/540). Of these, 58 (84%) had further surgery, of which 40 (69%) had repeat endoscopic stapling and the remainder an external procedure (31%).
Discussion
Endoscopic stapling of Zenker’s diverticulum in the United Kingdom
The data presented in this review is unique when compared to previously published studies as it is a summary of surgical outcomes from UK departments over the past 15 years since the first cohort was reported. It serves as a useful benchmark for future audits undertaken by UK departments which reflects the prevailing incidence of ZD in the UK, case load of a typical department, and surgeons’ experience (Table 2).
Endoscopic stapling is a relatively safe procedure that is associated with a short hospital stay and low rate of morbidity. Most patients (87%) are discharged by the second post-operative day. Outcomes are good with over 90% reporting resolved or significantly improved symptoms. The true incidence of minor complications is unknown. The low rates of minor complications collated in this review is likely under represented, which is unsurprising given the retrospective nature of most studies evaluated. Chang et al. [26] noted that the most common complication in their consecutive series of 150 patients was dental trauma (7.3%), followed by transient hoarseness (0.7%). The incidence of dental trauma may be mitigated by the use of custom made dental guards in addition to careful manipulation of the diverticuloscope [19].
The perforation rate in this review was higher than that previously quoted by Mirza et al. [27] (4.8 vs. 2.8%). Conversely, the mortality rate from another review was double (0.4 vs. 0.2%) [28]. It is clear that these differences are dependent on the selection criteria of studies evaluated. Case reports of major complications or mortality may raise the overall incidence. One other UK mortality was identified in the literature review but was not included in the meta-analysis as it was not possible to determine the overall case load of the reporting department [23]. If this case was included, the re-calculated mortality rate would have risen to 0.3%. Thus, we believe the 4.8% perforation and 0.2% mortality rates are better representative overall outcome data for the UK.
The relatively high rate of recurrence (12.8%) may be due to the portion of septum which remains undivided by the stapler. Determining the point at which stapler division of the septum should end may be difficult, as too shallow a division will lead to persistence of symptoms while too deep a division risks perforation with mediastinitis. The CO2 laser may be useful in dividing the residual septum or when there is a poor view of the pouch after the stapling gun has been inserted. Despite early reports of higher complications with endoscopic laser division, this technique may yet have a role and deserves further appraisal.
When the perforation rate is compared with outcomes from large case series from a single institution, the overall rate in the UK appears to be much higher. Chang et al. [26]. reported only one perforation (0.7%) in 150 consecutive cases. In a much larger series, van Overbeek [29] reported similarly low rates of serious complications. Whilst direct comparisons may be inappropriate given the difference in patient characteristics, the higher rate of perforation could be attributed to the low number of procedures performed by UK surgeons. Nearly two-thirds of surgeons reported performing less than five procedures annually [2]. Both NCEPOD and NICE have recommended sub-specialisation amongst surgeons [3, 4]. Given the relatively low number of pouch surgeries undertaken by a typical UK department, centralisation of pharyngeal pouch surgery could be a viable option in a similar hub-and-spoke system as for head and neck surgery. This would not only concentrate surgeons’ experience, but also facilitate targeted training of juniors and ultimately enhance patient outcomes.
Recommendations for better practice
There is currently no accepted guideline for patient assessment and selection for surgery. The literature abounds with recommendations for best practice and techniques to minimise complications. Endoscopic assessment of the ZD prior to stapling allows measurements of the length of the septum to decide the appropriate length of the staple gun that can be inserted. Carcinoma arising within the pouch may be rare but will be missed if debris is not first irrigated from the diverticulum before inspection. Bradley et al. [30] recommended excision of the pouch sac in patients less than 65 years and those who have a large pouch. If endoscopic diverticulotomy was performed, long-term patient follow-up was advised.
Veenker and Cohen [31] suggested that every patient should be assessed by a speech and language therapist to identify other swallowing abnormalities such as cricopharyngeal (CP) spasm (Fig. 5). Patients who have a symptomatic ZD but are not surgical candidates may be offered a trial of medical anti-reflux therapy. However, medical treatment alone for ZD is rarely successful. Recently, several investigators have reported favourable outcomes following botulinum toxin injection, although symptomatic improvement was transient [32, 33]. This is a potentially viable treatment option for patients who are unfit for surgery or have small pouches.
Suggested management pathway for Zenker’s diverticulum by Veenker and Cohen [31]
Access to small pouches can be difficult and may be associated with a higher incidence of iatrogenic perforation. Casso et al. [14] reported that 57% of patients with small pouches (<2.5 cm) suffered a complication, including one who had an iatrogenic perforation. The swallowing result was reported as being significantly better in large pouches (>4 cm). Similar observations were also reported by Tsikoudas et al. [15].
Hilton and Brightwell [34] proposed that the width of the intervening soft tissue between pouch and oesophagus is a specific feature that should be considered on any pre-operative barium swallow. In addition to pouch characteristics certain patient variables also influence surgical success, in particular the ability to access the pouch endoscopically. Although the presence of dentition was a common reason to abandon endoscopic surgery, Bloom et al. [35] also noted that a shorter neck (7.2 ± 1.2 cm), shorter hyomental distance (5.0 ± 1.1 cm) and higher BMI (27.2 ± 4.0) correlated with failure to expose the ZD. Collectively, these radiological and patient variables are important to inform on potential success at endoscopic stapling and serves as a reminder to exercise greater vigilance during surgery. It may be acceptable to under divide rather than over divide the septum and risk a perforation, although the recurrence rate may be higher [36].
The number of abandoned procedures was not insignificant (7.7%). Some patients may derive symptomatic improvement with dilatation of the cricopharyngeus [37]. However, the options faced by those who remain symptomatic are limited: either re-attempting an endoscopic approach or consideration of an external procedure. The latter option may be complicated by the level of post-operative support required which may not be available to all departments, supporting the rationale of concentrating pharyngeal pouch surgery in sub-specialised units. In the meantime, departments undertaking endoscopic stapling should review their practices to formulate strategies to deal with abandoned cases and management options for iatrogenic perforations should also be reviewed with appropriate protocol set in place.
Day case procedures appear to be de rigueur in otolaryngology at present. Day case endoscopic stapling, however, is not standard practice in the UK. The surgical procedure itself may be quick but given that most patients are elderly it is conceivable that many would require a minimum overnight stay in hospital. Both reported fatal cases in the UK re-attended hospital within 48 h of seemingly uneventful surgery. This post-operative management ethos was challenged by Gross et al. [38] who noted that there was no evidence to suggest that more conservative post-operative management of patients was safer. Over 70% of their case series were managed successfully on an outpatient basis. In addition to those who suffered an iatrogenic complication, patients with significant medical or mental comorbidities and those lacking sufficient social support were managed as in-patients.
Minimum dataset for audit
Standardisation of clinical variables collated for audit would be necessary to make meaningful assessments of current practice within a single department, and would allow comparison of outcomes across different departments. A minimum dataset should include patient demographics, size of pouch, abandoned procedures, conversion, complications, and outcome (Table 3). In an increasingly patient-centered health service and with the strong emphasis on patient-reported outcomes, it is important for surgeons to provide evidence of the benefit of their interventions. The Glasgow Benefit Inventory may be a suitable instrument to assess the effects of endoscopic stapling on the health status of patients. Self-reported symptom-specific outcomes can be measured using the Eating Assessment Tool-10 (EAT-10) [39]. The EAT-10 is a validated tool and can be utilised as a clinical instrument to document the initial dysphagia severity and monitor the treatment response.
Conclusion
Endoscopic stapling of pharyngeal pouch is a safe procedure that is associated with good outcomes and low complication rates. Mortality is rare and is a consequence of iatrogenic perforation, complicated by mediastinitis. No death has been reported since 2000 in the UK. Appropriate patient selection and surgical technique may mitigate against complications and improve long-term outcomes. The data presented in this review represents current clinical standards reported over the past 15 years by UK departments and serves as a useful benchmark for any future audits undertaken. A prospective audit administered centrally by the British Association of Otorhinolaryngology Head and Neck Surgery (ENT.UK) may be useful to produce national guidelines for best practice and clinical standards.
References
Newbegin CJ (1996) Endoscopic stapling diverticulotomy of pharyngeal pouch. Ann R Coll Surg Engl 78:400–401
Siddiq MA, Sood S (2004) Current management in pharyngeal pouch surgery by UK otorhinolaryngologists. Ann R Coll Surg Engl 86:247–252
Pharyngeal pouch surgery. The Report of the National Confidential Enquiry into Perioperative Deaths 1996/19977. http://www.ncepod.org.uk/1996_7.htm. Accessed 6 August, 2011
IPG22 Interventional procedure overview of endoscopic stapling of pharyngeal pouch. http://www.nice.org.uk/Guidance/IPG22, Accessed 6 August, 2011
Koay CB, Bates GJ (1996) Endoscopic stapling diverticulotomy for pharyngeal pouch. Clin Otolaryngol Allied Sci. 21:371–376
Baldwin DL, Toma AG (1998) Endoscopic stapled diverticulotomy: a real advance in the treatment of hypopharyngeal diverticulum. Clin Otolaryngol Allied Sci 23:244–247
van Eeden S, Lloyd RV, Tranter RM (1999) Comparison of the endoscopic stapling technique with more established procedures for pharyngeal pouches: results and patient satisfaction survey. J Laryngol Otol 113:237–240
Sood S, Newbegin CJ (2000) Endoscopic stapling of pharyngeal pouches in patients from the Yorkshire region. J Laryngol Otol 114:853–857
Jaramillo MJ, McLay KA, McAteer D (2001) Long-term clinico-radiological assessment of endoscopic stapling of pharyngeal pouch: a series of cases. J Laryngol Otol 115:462–466
Counter PR, Hilton ML, Baldwin DL (2002) Long-term follow-up of endoscopic stapled diverticulotomy. Ann R Coll Surg Engl 84:89–92
Mirza S, Dutt SN, Minhas SS, Irving RM (2002) A retrospective review of pharyngeal pouch surgery in 56 patients. Ann R Coll Surg Engl 84:247–251
Raut VV, Primrose WJ (2002) Long-term results of endoscopic stapling diverticulotomy for pharyngeal pouches. Otolaryngol Head Neck Surg 127:225–229
Weller MD, Porter MJ, Rowlands J (2004) An audit of pharyngeal pouch surgery using endoscopic stapling: the patient’s viewpoint. Eur Arch Otorhinolaryngol 261:331–333
Casso C, Lalam M, Ghosh S, Timms M (2006) Endoscopic stapling diverticulotomy: an audit of difficulties, outcome, and patient satisfaction. Otolaryngol Head Neck Surg 134:288–293
Tsikoudas A, Eason D, Kara N, Brunton JN, Mountain RE (2006) Correlation of radiologic findings and clinical outcome in pharyngeal pouch stapling. Ann Otol Rhinol Laryngol 115:721–726
Paleri V, Najim O, Meikle D, Wilson JA (2007) Microlaryngoscopic repair of iatrogenic pharyngeal pouch perforations: treatment of choice? Head Neck 29:189–192
Lieder A, Nasseri F, Sharma A, Jani P (2008) Safety and efficacy of endoscopic pharyngeal pouch stapling in a large UK study. Clin Otolaryngol 33:127–130
Harris RP, Weller MD, Porter MJ (2010) A follow up audit of pharyngeal pouch surgery using endoscopic stapling. Eur Arch Otorhinolaryngol 267:939–943
Yeo JC, Mackenzie K (2010) Pharyngeal pouch surgery in north Glasgow: NICE (National Institute for Health and Clinical Excellence) practice or not? J Laryngol Otol 124:533–537
Kubba H, Hussain SS (1998) Stapler failure in pharyngeal diverticulectomy: a suggested modification in surgical technique. J R Coll Surg Edinb 43:31–32
Hilton M, Brightwell AP (2000) Oesophageal perforation during stapling of a pharyngeal pouch: adverse clinical incident report. J Laryngol Otol 114:549–550
Arunachalam PS, Cameron DS (2001) Persistent foreign body sensation and pharyngeal pain due to retention of staples: an interesting sequelae of endoscopic stapling procedure. J Laryngol Otol 115:425–427
Nix PA (2001) Delayed oesophageal perforation following endoscopic stapling of a pharyngeal pouch. J Laryngol Otol 115:668
Porter MJ, Kim D (2010) Endoscopic pharyngeal pouch surgery as a day case. Clin Otolaryngol 35:162–163
Jennings SJ, Wild DC, Beasley N, Sharp JF (2006) How we do it: improving the success of endoscopic pharyngeal pouch stapling. Clin Otolaryngol 31:550–552
Chang CY, Payyapilli RJ, Scher RL (2003) Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope 113:957–965
Mirza S, Dutt SN, Irving RM (2003) Iatrogenic perforation in endoscopic stapling diverticulotomy for pharyngeal pouches. J Laryngol Otol 117:93–98
Sen P, Bhattacharyya AK (2004) Endoscopic stapling of pharyngeal pouch. J Laryngol Otol 118:601–606
van Overbeek JJ (2003) Pathogenesis and methods of treatment of Zenker’s diverticulum. Ann Otol Rhinol Laryngol 112:583–593
Bradley PJ, Kochaar A, Quraishi MS (1999) Pharyngeal pouch carcinoma: real or imaginary risks? Ann Otol Rhinol Laryngol 108:1027–1032
Veenker E, Cohen JI (2003) Current trends in management of Zenker diverticulum. Curr Opin Otolaryngol Head Neck Surg 11:160–165
Spinelli P, Ballardini G (2003) Botulinum toxin type A (Dysport) for the treatment of Zenker’s diverticulum. Surg Endosc 17:660
Katsinelos P, Chatzimavroudis G, Zavos C, Pilpilidis I, Paroutoglou G, Kountouras J (2009) Long-term botulinum toxin treatment for dysphagia due to large epiphrenic diverticulum in elderly patients: a report of two cases. Dysphagia 24:109–113
Hilton M, Brightwell AP (2000) Oesophageal perforation during stapling of a pharyngeal pouch: adverse clinical incident report. J Laryngol Otol 114:549–550
Bloom JD, Bleier BS, Mirza N, Chalian AA, Thaler ER (2010) Factors predicting endoscopic exposure of Zenker’s diverticulum. Ann Otol Rhinol Laryngol 119:736–741
Visosky AM, Parke RB, Donovan DT (2008) Endoscopic management of Zenker’s diverticulum: factors predictive of success or failure. Ann Otol Rhinol Laryngol 117:531–537
Allen J, White CJ, Leonard R, Belafsky PC (2010) Effect of cricopharyngeus muscle surgery on the pharynx. Laryngoscope 120:1498–1503
Gross ND, Cohen JI, Andersen PE (2004) Outpatient endoscopic Zenker diverticulotomy. Laryngoscope 114:208–211
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ (2008) Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 117:919–924
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leong, S.C., Wilkie, M.D. & Webb, C.J. Endoscopic stapling of Zenker’s diverticulum: establishing national baselines for auditing clinical outcomes in the United Kingdom. Eur Arch Otorhinolaryngol 269, 1877–1884 (2012). https://doi.org/10.1007/s00405-012-1945-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-1945-3