Abstract
Background
Dual-Knife® (Olympus) and Hydride-Knife® are new needle knives frequently used for submucosal dissection because of their safety and precision. In this study we aimed to evaluate the efficacy and safety of such devices in the diverticulopexy by flexible endoscopy.
Methods
From February 2009 to March 2013, 42 patients (25 men), mean age 74.5, with symptomatic Zenker’s diverticulum, were included in a non-randomized prospective multicenter study. The symptoms described by all patients include dysphagia, regurgitation and/or swallowing disorders. The diverticulopexy was performed with the Dual-Knife® or Hydrid-Knife®, after septum exposure with the diverticuloscope, and terminated with distal tip clips positioning. All complications were noted. Patients’ symptoms were regularly assessed during follow-up visits or telephone interviews.
Results
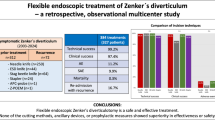
The first endoscopy treatment was successful for all patients. Thirty-seven patients (88 %) had symptoms improvement after the first treatment. The recurrence rate was 14 % (6 patients); a second endoscopic treatment was required 12 months on average after the first treatment, with 100 % efficiency. Mid-term (16 months) efficiency was 91.67 % after 1 to 3 endoscopic treatments. A total of 55 procedures were performed without perforation or significant bleeding and 3 patients underwent surgery. In multivariate analysis, the diverticulum size and the type of dissection knife were not risks factors for recurrence.
Conclusions
Endoscopic diverticuloscope-assisted diverticulotomy with submucosal dissection knives is a safe and effective alternative treatment for patients with a symptomatic Zenker’s diverticulum measuring between 2 and 10 cm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Zenker’s diverticulum is a rare disease which impacts an estimated 2/10000 inhabitants per year [1]. Zenker’s diverticulum is described as a posterior herniation of the mucosa and submucosa located at the mouth of Killian, probably facilitated by hypertonia of the cricopharyngeal muscle [2] (Fig. 1).
It usually occurs in patients over 70 years old often leading to dysphagia, difficulty in swallowing, regurgitation, and sometimes repeated inhalations. The treatment consists in diverticulopexy, i.e., a myotomy of the cricopharyngeal muscle and a section of the septum between the esophagus and the diverticulum. The septum incision prevents the retention of food in the diverticulum. The benefit of treatment with rigid endoscopy compared to open surgery was demonstrated with a reduction in postoperative morbidity and comparable efficacy [3, 4]. Treatment with flexible endoscopy has been evaluated since 1995 [5] with several different instruments: argon plasma coagulation (APC) probe, needle knives, hot biopsy forceps [5, 6]. These instruments are not designed for tissue dissection. Thus, we decided to evaluate the benefit of submucosal dissection knives: the Dual-Knife® (Olympus endotherapy) and Hydride-Knife® (Fig. 2A, B). The main objective of the study was to evaluate the efficacy and safety of submucosal dissection knives for endoscopic treatment of Zenker’s diverticulum by flexible endoscopy.
Materiel and methods
Method and patients
From February 2009 to January 2013, 42 consecutive patients with symptomatic Zenker’s diverticulum, diagnosed during a gastroscopy and/or barium swallow, were included in a prospective multicenter study.
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki, in compliance with good clinical practice and according to local regulations. This work was not supported financially or otherwise by any external sources.
The size of the diverticulum was estimated endoscopically and radiographically compared to the cervical vertebral bodies. Exclusion criteria were the minimum or maximum size of the diverticulum (diverticulum sizes > 10 cm or < 1.5 cm were excluded), contraindication to general anesthesia, major bleeding disorders, “American Society of Anaesthesiologists’’(ASA) physical status classification >3, multiple diverticula and esophageal strictures.
All patients were intubated under general anesthesia and positioned in the left lateral decubitus position. Procedures were performed with a standard video gastroscope (GIFQ 180 or 160Z, Olympus Optical Co., Tokyo, Japan). The endoscopic technique was to introduce diverticuloscope (ZD overtube, ZDO −22 ± 30; Wilson-Cook, Winston-Salem, North Carolina, USA) on the gastroscope and then to expose the septum to achieve diverticulopexy. The first step was to introduce the diverticuloscope on the gastroscope, after being abundantly lubricated. Then, the gastroscope was carefully pushed into the esophagus and a 0.035 mm guidewire was positioned in the stomach. The diverticuloscope was moved forward over the gastroscope, up to the black mark. Alternating rotational movements allowed placing one flap in the esophagus and another one in the diverticulum in order to expose the septum (Fig. 3).
The diverticulotomy consisted of performing a cricopharyngeal muscle myomotomy with the submucosal dissection knife Dual-Knife® (KD-650U Olympus) or Hydrid-Knife®. The dissection of the septum with a stream of endocut (Erbotom ICC 200/350; ERBE ElecTübingen, Germany) was considered as complete when all the muscle fibers were severed. At the end of the procedure, 1 or 2 endoclips were placed at the distal tip of the cut to prevent microperforation. The endoscopic techniques for first and secondary procedures are described in the attached films (video1 and 2; Fig. 4). The next day, the patient resumed liquid and solid oral feeding. If there were no complications, patients were discharged within 48 h after surgery. In the case of pain or fever immediately following the procedure, the patient was left to fast and nasogastric suction was put in place and, if necessary, a scanning was done to look for complications. The efficacy and safety of treatment was evaluated by follow-up visits or telephone interviews. Despite regular monitoring of the patients after the procedure, 6 of them were lost to follow-up. The Dakkak and Bennett [7] score of dysphagia (score 0, no dysphagia; score 1, dysphagia to solids; score 2, dysphagia with semi-solids; score 3, dysphagia with liquids; score 4, aphagia) was used to quantify dysphagia. The symptoms of regurgitation, sensation of choking and coughing were measured in term of their frequency (0: Not at all, 1: Several times a month, 2: Several times a week, 3: daily). Clinical success was defined as improvement or disappearance of dysphagia and/or regurgitation. Occasional recurrence of symptoms (less than once per week) was not considered a treatment failure. Treatment failure was defined as the absence of improvement within 1 month after the procedure. All complications during the procedure and at follow-up were recorded.
A First treatment with diverticuloscope and Dual-Knife®. Dissection starts from the middle of the septum and continue by cutting, step by step, until the last muscle fiber (from Video 1). B Second treatment with diverticuloscope and Dual-Knife®. Second treatment procedures often lead to a more important bleeding (but still moderate) and to shorter size of cut. The methodology remains the same as for a first procedure (from video 2)
Statistics
Data is expressed as mean (±SD), median confidence interval (CI) [95 %], or percentage depending on the type of data. Clinical symptoms (dysphagia, regurgitation, suffocation, and cough) were compared by calculating a mean score at T0 (before surgery), T1 (short-term), and T2 (mid-term). The Student’s test on paired data was used. Predictors of recurrence were analyzed; univariate analysis followed by multivariate analysis was performed. Significance level α = 0.05 was applied. All statistical analyses were performed using SAS V9.1 software (SAS Institute, Cary, NC, USA).
Results
Patients
The median age of the 42 patients was 74.5, CI95 [70.0–80.0] years, and mean body mass index (BMI) was 23.5, CI95 [22.0–25.0] kg/m2. The general condition of the patients evaluated by the ASA score (respectively 53 % for score 2, 45 % for score 3, and 2 % for score 1). Patients’ symptoms were listed in Table 1. The median size of the diverticulum was 35.0, CI95 [30.0–35.0] mm before endoscopic treatment. One patient was referred to us after rigid endoscopy failure, due to the inability to expose the septum. No patient received prophylactic antibiotherapy.
Technical results
Fifty-five endoscopic procedures were performed by five gastroenterologists specialized in interventional gastrointestinal endoscopy, in three centers in France. Eleven patients had two endoscopic treatments and two patients had three treatments. All patients had a complete dissection of the cricopharyngeal muscle up until the last muscular fibers. For the first procedures, the dissection was performed with the Needle-Knife® (n = 9, 17 %), later on we replaced it with the submucosal dissection knives (Dual-Knife® n = 31, 45 % and Hydride-Knife® n = 13, 24 %). With the Needle-Knife®, the incision seemed too fast and difficult to control, more specifically, the incision of the last muscle fibers lacked precision. On the other hand, with Dual-Knife® and Hydride-Knife®, we were able to incise with precision and security.
The diverticuloscope which was easily positioned and the endotracheal tube did not get in the way for its introduction. In two patients, the diverticuloscope could not be positioned because of the small size of the diverticulum (<20 mm). In one case, diverticulotomy was performed without overtube because of good septum exposure. In another case, diverticulotomy required the use of a cap. Only three patients did not have prophylactic endoclip application and 2 patients received more than 2 clips to stop a per-procedure bleeding. The median Length of Hospital Stay (LOHS) was 3 days, CI95 [2.0–3.0]. All patient characteristics are listed in Table 1.
Clinical results
Among the 42 patients treated with one to three endoscopic procedures, mid-term (16 months) efficiency was 92.3 % without major complications. Thirty-seven patients (88 %) had a significant reduction in symptoms after the first endoscopic treatment. The scores of dysphagia and regurgitation were significantly improved both at 6-month and 16-month follow-up assessments. The mean dysphagia score was 1.98 ± 0.84 before treatment and dropped to 0.54 ± 0.79 at 6 months after endoscopic treatment (p < 0.001). At the end of follow-up, 36 patients were contacted. The score of dysphagia was obtained by phone call or face-to-face interview. The mean dysphagia score was 0.06 ± 0.25 at 16 months (p < 0.01) (Table 2). Regurgitation, suffocation sensations, and chronic cough were significantly improved (Table 3).
In multivariate analysis, BMI parameters, size of the diverticulum, LOHS, and type of knife were modeled as they were significant in univariate (LOHS) or showed a trend (BMI, diverticulum size, and knife categories) (Table 4). LOHS is the only predictive parameter of recurrence (odds ratio (OR) = 0.17 [0.03–0.91] p = 0.04). The risk of recurrence is 5.9 times more important when the patient is hospitalized for more than 3 days (OR = 0.17).
Complications
Five patients presented moderate per-procedure bleeding. They were treated by a soft coagulation with Dual-Knife at first intention and, in case of failure, with Coagrasper® clamp (Olympus). The objective was to stop the bleeding and to be able to achieve the diverticulotomy for all patients. Among the 10 patients (23, 8 %) who underwent a second endoscopic treatment, one patient had per-procedure bleeding also endoscopically treated. These pre-procedure hemorrhages were not considered as complications because they did not prolong hospital stay and did not require transfusion. No cases of delayed hemorrhaging were described.
Pharyngeal pain associated with endoscopic treatment and/or orotracheal intubation occurred in 4 patients after the first or second endoscopic treatment. Analgesic treatment of Class 1 and/or 2 was necessary and sufficient for a few days.
Fever occurred in 3 patients requiring antibiotics for a week but no infectious complications occurred. All blood cultures were negative and there were no oropharyngeal abscess. No cases of subcutaneous emphysema, pneumomediastinum, or mediastinitis were described, neither during the first session of endoscopic treatment nor during recurrences.
For all patients, a liquid diet was started the day after the endoscopic procedure and discharge was possible in all cases a few days later (3 days post-procedure on average).
Follow-up
The immediate and long-term follow-up made us to create various groups (Fig. 5).
“Immediate success” group (n = 37/42)
Among the 42 patients, 37 (88 %) were clinically improved after the first endoscopic session and 33/36 (91.67 %) patients after one or more endoscopic treatments. Ten patients had a second endoscopic treatment which was effective in 8 cases. Three patients were operated on. Six patients, successfully treated by the first endoscopic treatment, were lost to follow-up during the first 6 months of the study (possible causes: change of residence/incorrect contact information…).
Second endoscopic treatment
Ten out of 42 patients (26 %) had a second endoscopic treatment on average after 12.4 months (range 1–36). For the patients who did not respond to the first endoscopic treatment, morphological examinations (gastroscopy and barium swallow) showed the persistence of a residual diverticulum.
“Immediate failure” group (n = 5/42) without any clinical improvement
Four out of the 5 patients in this group underwent “early” second endoscopic procedures within the 4 months after the index one (3.4 months on average). A significant improvement in dysphagia and regurgitation occurred for 2 patients. This second endoscopic treatment was ineffective for the remaining 2 patients who underwent surgery. One of them had a 10-cm-long diverticulum and surgical treatment was successful. The second patient had significant psychological disorders whose symptoms were difficult to associate with an organic cause. In this case, surgical treatment was also ineffective.
The fifth patient of this group had a small (20 mm) and symptomatic (mainly regurgitation) diverticulum. The primo endoscopic treatment failed due to difficulties to position the diverticuloscope. The endoscopic procedure was successful despite poor tolerance (oropharyngeal pain and fever). But the patient refused a second endoscopic procedure to undergo surgery. Unfortunately, the surgery performed 6 months after the first endoscopic treatment did not bring any improvement.
“Recurrences” group (n = 6/42) with recurrence after initial symptoms improved or resolved
A second endoscopic treatment was effective in all cases. Two patients had three endoscopic interventions because of symptom relapse after the second endoscopic treatment. At follow-up, these two patients described a significant improvement in dysphagia and regurgitation. No one in this recurrence group had surgery.
Discussion
The results of our study show the interest and benefits of submucosal dissection knives in the flexible endoscopic treatment of Zenker’s diverticulum with a mid-term clinical efficacy of 91.67 % without any perforation.
Zenker’s diverticulum is formed by a herniation of hypopharyngeal mucosa between the inferior pharyngeal constrictor muscle and the cricopharyngeal sphincter through an area of muscular junction weakness known as Killian triangle. Inadequate relaxation of the cricopharyngeal muscle hinders the normal flow of food into the esophagus and creates an area of high pressure in the hypopharynx. Fibrosis in muscle fibers and gradual tension on the esophageal walls lead to the formation of a posterior diverticulum. Between the diverticulum and the esophageal lumen, a bridge of tissue composed of mucosa, submucosa, connective tissue, and muscle fibers make up the septum [5]. Endoscopic treatment of Zenker’s diverticulum consists in performing a diverticulopexy by dissecting the cricopharyngeal muscle up until the last muscle fibers. The difficulty of this technique is to dissect to improve the clinical efficacy, but to stop the dissection just after cutting the last muscle fiber to avoid perforation risk [6]. The end of the dissection has to be very precise and progressive. The main risk is to continue the dissection too deep, over the muscle, provoking perforation. Until now the studies evaluating flexible endoscopy treatment of Zenker’s diverticulum were done using non-specific tissue dissection instruments as the Needle-Knife®, the hot biopsy forceps or the APC. The Needle-Knife® is dedicated to the pre-cut or infundibulotomy during Endoscopic Retrograde CholangioPancreatography (ERCP), with difficult access to the common bile duct [8–13]. The Needle-Knife® allows precise dissection, but the dissection is often too fast and difficult to control due to the small contact area on the tissues. Hot biopsy forceps were used for resection of colonic polyps [5, 14]. Hot biopsy forceps used in endocut mode lacked precision because they generated a stream of coagulation which diffuses into the tissue. The APC is designed for hemostasis of hemorrhagic lesions or destruction of tumor lesions [15–17]. For APC, there was no precise control of the dissection because the argon gas diffusion in the superficial tissues was random and perforation risk could be increased [17]. A single study evaluated a submucosa dissecting tool, the Hook-Knife®, useful for the dissection of tissue in traction [18]. But the fast tissue dissection was difficult to control and required reorienting the tip of the Hook-Knife® before each use.
Dual-Knife® and probably Hydride-Knife® are the best instruments for submucosal dissection. Their tips are slightly flared, allowing a more gradual dissection than with the Hook-Knife® or the Needle-Knife® by slightly hooking onto the tissue. The flared tips of Dual-Knife® and Hydride-Knife® allow grasping the exact amount of tissue to be dissected, as for a submucosal dissection. These dissection knives are more precise because they are more progressive, and allow for better control of the section compared to the Needle-Knife® used in some patients at the beginning of the study. In addition, unlike the Hook-Knife®, these dissection knives do not necessitate systematic reorientation. For these reasons, we thought dissection knives (Dual-Knife® and Hydride-Knife®), which are more accurate for tissue dissection, would be more suitable to dissect the last cricopharyngeal muscle fibers. Dual-Knife® and Hydride-Knife® allowed us to select the amount of tissue to be dissected, and cutting the last millimeters without increasing the risk of perforation. In our study, no cases of perforation (mediastinal or subcutaneous emphysema, mediastinitis) were reported. On the contrary, previous studies with APC, hot biopsy forceps, Needle-Knife®, and Hook-Knife® showed the following perforation risks: 18–23 % [14], 4.7 % [13], 10–23 % [8, 11], and 3.1 % [17]. In these cases, conservative treatment with nasogastric tube introduction antibiotherapy and few days of fasting is sufficient. The use of a diverticuloscope and the systematic clip also reduces the risk of perforation [6, 9, 13]. Furthermore, this risk does not seem to increase during a second endoscopic treatment [13, 18].In the literature, the clinical efficacy of endoscopic treatment in the long-term is evaluated at 80 to 90 % [8, 9, 11, 13, 14, 17, 18] and mainly depends on the dissection depth [19]. Recurrences occur in about 20 % of the cases, 5 to 7 months after the first endoscopic treatment [12, 13].
In our study, the recurrence rate was 14 % and the second treatment session was performed at 12 months on average. Treatment with dissection knives seemed more effective and longer lasting, which is probably related to the larger depth of dissection. Since the last muscle fibers of cricopharyngeal sphincter were easily identified and dissected. In multivariate analysis, only the mean LOHS was identified as a risk factor for recurrence (Table 4). The LOHS increase is directly associated to the safety of endoscopic treatment. Patients who had a poor tolerance to treatment had more recurrences than others. The clinical recurrence of endoscopic treatment was probably due to insufficient dissection area (for 6 patients). Four patients were affectively treated with a second endoscopic treatment and two patients underwent a third endoscopic treatment, with successful outcomes. All surgical patients (N = 3) had previous endoscopic treatment failure, due to long (10 cm) or short (2 cm) diverticula.
In previous studies, in case of symptom recurrence, a second endoscopic procedure can effectively treat patients in 70 to 78 % of cases [12, 13]. In our series, 100 % of patients were improved after a second endoscopic treatment. A third session may be necessary in rare cases, and exceptionally, a surgical indication is required after endoscopic treatment failure (<5 %) [20].
Surgical treatment seems to be more effective after a first session with a lower recurrence rate [21] but it is subject to a high morbidity (10 %), vocal cord paralysis (8.6 %), cervical hematoma requiring surgical drainage, salivary fistula (6 %), purulent mediastinitis (3.9 %), and an assessed 1 % mortality rate [3]. If the morbidity of treatment with rigid endoscopy is lower than for surgical treatment, it remains much higher than flexible endoscopy with 2–4 % major complications: bleeding requiring surgical hemostasis, vocal cord paralysis, perforation requiring surgical treatment, infectious pneumonia, and mediastinitis requiring surgical drainage [4, 22].
For rigid endoscopic diverticulotomy, endoscopic laser CO2 and stapling technique could reduce adverse effects and improve efficacy. Endoscopic stapling technique has become increasingly popular. This technique allows simultaneously cutting and sealing of the wound edge, contributing to a lower incidence of perforation and bleeding. It is also free of thermal damage to recurrent laryngeal nerves. In a recent review of 93 studies about Zenker’s diverticulum surgical interventions, Yuan et al. identified 44 studies (n = 1800 patients) reporting endoscopic stapling technique results, with the following adverse effects: dental injuries (2.0 %, 36/1,800), esophageal mucosal damages (1.6 %, 29/1,728), and perforations (1.6 %, 29/1,728) [23]. Recently, Repici et al. compared the flexible needle-knife technique (n = 28) with the rigid stapling technique (n = 30) and found similar outcomes in: hospital stay, symptom relief percentage, and complication rate (1/28 vs. 2/30). However, procedure time in the rigid stapling group was significantly longer than that in the flexible needle-knife group (63 vs. 42 min) [24]. Only 1 patient with endoscopic stapling procedure developed recurrence within the 20-month mean follow-up period. Endoscopic CO2 technique provides a better visualization of the diverticular bridge and an easier control of the operation. Yuan et al. also noticed that, patients undergoing CO2 laser technique, experienced less pain and took food more readily in first postoperative days. In their review, Yuan et al. selected 19 studies (n = 1060 patients) with CO2 laser technique, with a complication rate of 9, 3 and 0, 2 % of mortality [1].
The recurrence rate is probably higher than for flexible endoscopy treatment. In addition, flexible endoscopy allows better exposure and visualization of the diverticulum compared to rigid endoscopy, especially in patients with retrognathia, short neck, and decreased mobility of the neck. In 15–68 % of cases, conversion to open surgery is necessary [21].
The limitations of this study relate to the small number of patients, the absence of a control group for comparative statistical analysis, and the lack of long-term follow-up.
In conclusion, the treatment of Zenker’s diverticulum by flexible endoscopy with submucosal dissection knives (Dual-Knife® and Hydride-Knife®) is an effective technique in 92.3 % of the cases after 1 to 3 endoscopic treatments. Recurrence is relatively common (14 %) in the first year and is effectively treated with a second endoscopic treatment. The risk of perforation is minimal when dissection knives are used with a diverticuloscope and clips. The diverticulopexy by flexible endoscopy should emerge as the first-line treatment of symptomatic Zenker’s diverticulum measuring between 2 and 10 cm deep.
References
Watemberg S, Landau O, Avrahami R (1996) Zenker’s diverticulum: reappraisal. Am J Gastroenterol 91(8):1494–1498
Peters JH, Mason R (1999) The physiopathological basis for Zenker’s diverticulum. Chirurgfévr 70(7):741–746
Smith SR, Genden EM, Urken ML (2002) Endoscopic stapling technique for the treatment of Zenker diverticulum vs standard open-neck technique: a direct comparison and charge analysis. Arch Otolaryngol Head Neck Surg 128(2):141–144
Chang CY, Payyapilli RJ, Scher RL (2003) Endoscopic staple diverticulostomy for Zenker’s diverticulum: review of literature and experience in 159 consecutive cases. Laryngoscope 113(6):957–965
Mulder CJ, den Hartog G, Robijn RJ, Thies JE (1995) Flexible endoscopic treatment of Zenker’s diverticulum: a new approach. Endoscopy 27(6):438–442
Costamagna G, Iacopini F, Tringali A, Marchese M, Spada C, Familiari P et al (2007) Flexible endoscopic Zenker’s diverticulotomy: cap-assisted technique vs. diverticuloscope-assisted technique. Endoscopy 39(2):146–152
Dakkak M, Bennett JR (1992) A new dysphagia score with objective validation. J Clin Gastroenterol 14(2):99–100
Ishioka S, Sakai P, Maluf Filho F, Melo J (1995) Endoscopic incision of Zenker’s diverticula. Endoscopy 27:433–437
Evrard S, Le Moine O, Hassid S, Devière J (2003) Zenker’s diverticulum: a new endoscopic treatment with a soft diverticuloscope. Gastrointest Endosc 58(1):116–120
Sakai P, Ishioka S, Maluf-Filho F, Chaves D, Moura EG (2001) Endoscopic treatment of Zenker’s diverticulum with an oblique-end hood attached to the endoscope. Gastrointest Endosc 54(6):760–763
Hashiba K, de Paula AL, da Silva JG, Cappellanes CA, Moribe D, Castillo CF et al (1999) Endoscopic treatment of Zenker’s diverticulum. Gastrointest Endosc 49(1):93–97
Vogelsang A, Preiss C, Neuhaus H, Schumacher B (2007) Endotherapy of Zenker’s diverticulum using the needle-knife technique: long-term follow-up. Endoscopy 39(2):131–136
Huberty V, El Bacha S, Blero D, Le Moine O, Hassid S, Devière J (2013) Endoscopic treatment for Zenker’s diverticulum: long-term results (with video). Gastrointest Endosc 77(5):701–707
Christiaens P, De Roock W, Van Olmen A, Moons V, D’Haens G (2007) Treatment of Zenker’s diverticulum through a flexible endoscope with a transparent oblique-end hood attached to the tip and a monopolar forceps. Endoscopy 39(2):137–140
Mulder CJ (1999) Zapping Zenker’s diverticulum: gastroscopic treatment. Can J Gastroenterol 13(5):405–407
Pech O, May A, Gossner L, Mayer G, Abdollahnia R, Ell C (2002) Endoscopic therapy for Zenkers’s diverticulum by means of argon plasma coagulation. Z Gastroenterol 40(7):517–520
Rabenstein T, May A, Michel J, Manner H, Pech O, Gossner L et al (2007) Argon plasma coagulation for flexible endoscopic Zenker’s diverticulotomy. Endoscopy 39(2):141–145
Repici A, Pagano N, Romeo F, Danese S, Arosio M, Rando G et al (2010) Endoscopic flexible treatment of Zenker’s diverticulum: a modification of the needle-knife technique. Endoscopy 42(7):532–535
Richtsmeier WJ (2005) Myotomy length determinants in endoscopic staple-assisted esophagodiverticulostomy for small Zenker’s diverticula. Ann Otol Rhinol Laryngol 114(5):341–346
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC et al (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Katzka DA, Baron TH (2013) Transoral flexible endoscopic therapy of Zenker’s diverticulum: is it time for gastroenterologists to stick their necks out? Gastrointest Endosc 77(5):708–710
Koch M, Mantsopoulos K, Velegrakis S, Iro H, Zenk J (2011) Endoscopic laser-assisted diverticulotomy versus open surgical approach in the treatment of Zenker’s diverticulum. Laryngoscope 121(10):2090–2094
Yuan Y, Zhao Y-F, Hu Y, Chen L-Q (2013) Surgical treatment of Zenker’s diverticulum. Dig Surg 30(3):207–218
Repici A, Pagano N, Fumagalli U, Peracchia A, Narne S, Malesci A et al (2011) Transoral treatment of Zenker diverticulum: flexible endoscopy versus endoscopic stapling. A retrospective comparison of outcomes. Dis Esophagus 24(4):235–239
Acknowledgments
We thank the patients, the nurses for their important contribution, Terri Galli for the English review and Laurence Lecomte for her support during the study and the publication process.
Disclosures
A. Laquière, P. Gerandal, J. P. Arpurt, J. Boulant, S. Belon, S. Aboukheir, R. Laugier, G. Penaranda, L. Curel, and C. Boustière have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MOV 57494 kb)
Supplementary material 2 (MOV 31003 kb)
Rights and permissions
About this article
Cite this article
Laquière, A., Grandval, P., Arpurt, J.P. et al. Interest of submucosal dissection knife for endoscopic treatment of Zenker’s diverticulum. Surg Endosc 29, 2802–2810 (2015). https://doi.org/10.1007/s00464-014-3976-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3976-x