Abstract
Background
When pregnant patients require surgery, whether to perform an operation open or laparoscopic is often debated. We evaluated the impact of laparoscopy for common general surgical problems in pregnancy to determine safety and trends in operative approach over time.
Methods
Pregnant patients undergoing appendectomy or cholecystectomy were identified using the National Surgical Quality Improvement Program (NSQIP) database. We analyzed demographics, operative characteristics, and outcomes. Univariate comparison and multivariate regression analysis (MVA) were performed adjusting for confounding factors: age, body mass index (BMI), diabetes, and smoking, and an additional MVA was performed for perforated cases.
Results
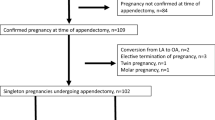
A total of 1999 pregnant patients between 2005 and 2012 were evaluated. Of 1335 appendectomies, 894 were performed laparoscopically (LA) and 441 open (OA). For 664 cholecystectomies, 606 were laparoscopic (LC) and 58 open (OC). There were no deaths. For LA versus OA, patient characteristics were not different {age: 27.7 vs. 28.2 years, p = 0.19; diabetes: 1.8 vs. 0.9 %, p = 0.24; smoking: 19 vs. 16.1 %, p = 0.2} except for BMI (27.9 vs. 28.4 kg/m2; p = 0.03). LA had shorter operative times (ORT), length of stay (LOS), and fewer postoperative complications compared to OA. In MVA, difference between approaches remained statistically significant for ORT (<0.0001), LOS (<0.01), and wound complications (<0.01). MVA was performed for perforated cases alone: LA had equal ORT (p = 0.19) yet shorter LOS (p = <0.001). The majority of LA were performed in the last 4 years versus the first 4 years (61 vs. 39 %, p < 0.001). For LC versus OC, patient characteristics were not different: age (28.3 vs. 28.7 years; p = 0.33), BMI (31.4 vs. 33.2 kg/m2, p = 0.25), diabetes (2.8 vs. 3.5 %, p = 0.68), and smoking (21.1 vs. 25.9 %, p = 0.4). LC had a shorter ORT, LOS, and fewer postoperative complications than OC. In MVA, the difference between approaches remained statistically significant for ORT (<0.0001), LOS (<0.0001), and minor complications (<0.01). In MVA for cholecystitis with perforation, no difference was seen for LOS, ORT, or postoperative complications (p > 0.05). The percentage of LC cases appeared to increase over time (89 vs. 93 %, p = 0.06).
Conclusion
While fetal events are unknown, LA and LC in pregnant patients demonstrated shorter ORT, LOS, and reduced complications and were performed more frequently over time. Even in perforated cases, laparoscopy appears safe in pregnant patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
With the incidence of acute abdomen occurring in up to 1 in 500 pregnancies, the likelihood of operating on a pregnant patient as a General Surgeon is felt to be inevitable [1]. Appendectomy and cholecystectomy are the most common non-obstetrical operations in pregnant patients [1–5]. The highest incidence is appendicitis, which occurs in 0.04–0.2 % of all pregnancies; this representing 25 % of non-obstetric operations performed during pregnancy [1, 2, 4]. Cholecystitis during pregnancy affects approximately 0.1 % of pregnant patients despite 1–3 % of pregnant patients having cholelithiasis [4].
The controversy of laparoscopy in pregnancy and the effects of pneumoperitoneum have been analyzed. Physiologic concerns of pneumoperitoneum in the gravid patient and further influence of positioning such as Trendelenburg are cumulative in decreasing thoracic cavity compliance, decreasing functional reserve capacity, increasing peak airway pressures, and worsening ventilation–perfusion mismatch [5]. While innovations such as gasless pneumoperitoneum in pregnant patients have been trialed [6], the need for such mechanisms is in debate [7]. No differences have been identified that could not be resolved by adjusting minute ventilation when assessing end-tidal CO2, arterial CO2, or pH during all stages of insufflation or postoperatively; likewise, any compromise of hemodynamics can be minimized with such maneuvers as left uterine displacement and lowering intra-abdominal pressures to 12 mmHg [8]. Acknowledging the results of these previously studied factors in the pregnant patient and formulating a safe plan of execution, the General Surgeon may somewhat surrender the apprehension of utilizing the laparoscopic approach when operating on the gravid patient. With the incidence of surgery and safety of laparoscopy in pregnancy identified, we studied the impact of laparoscopy for common general surgical problems in pregnancy using a national dataset to determine safety and trends of application over time.
Methods
Study design
Data source
This study, which was conducted with the approval of the Carolinas Medical Center Institutional Review Board, retrospectively examined the outcomes of appendectomy and cholecystectomy in pregnant patients comparing laparoscopic versus open technique utilizing the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database. The methodology of collection within this database has been previously described [9, 10]. We compared early years (time period (TP)1: 2005–2008) to late years (TP2: 2009–2012) to identify time trends of utility of laparoscopy for appendectomy and cholecystectomy in pregnancy. Patients were categorized based on the current procedural terminology (CPT) codes for laparoscopic appendectomy (44970, 44979), open appendectomy (44950, 44960), laparoscopic cholecystectomy (47562, 47563), and open cholecystectomy (47600, 47605), and data were collected only for pregnant patients as defined by the corresponding NSQIP variable pregnancy in patient characteristics. The exact gestational age or trimester of the pregnancy is not collected in the NSQIP database. To specifically analyze high-risk patients with perforated cases, postoperative diagnosis based on ICD-9 codes was used for appendicitis (540.0, 540.1) and cholecystitis (575.0, 575.4) as well as independently identifying patients having cholecystitis with biliary obstruction (574.01, 574.11). Evaluation of ICD-9 codes with respect to threatened preterm labor (644.03), preterm labor (644.2), fetal distress (656.8), or fetal demise (656.4) was performed. No results could be identified for preterm labor or any fetal outcomes for either appendectomy or cholecystectomy from the database and therefore could not be analyzed.
Data collection
Patient characteristics such as age, sex, race, BMI, tobacco use, and comorbidities were collected. Perioperative information such as surgeon specialty, type of anesthesia, operative time, and length of stay (LOS) was identified. Postoperative outcomes such as pneumonia, venous thromboembolic event, stroke, myocardial infarction, sepsis, acute or progressive renal failure, superficial surgical site infection (SSI), deep SSI, organ space SSI, return to the operating room, and 30-day mortality were included. Overall wound complications as well as minor and major overall complications were classified as previously published [11].
Statistical analysis
Standard statistical analysis was performed using Pearson’s Chi-square and Fisher’s exact tests for categorical variables and unpaired t test or Kruskal–Wallis test for nonparametric continuous data and ordinal variables as appropriate to obtain a two-tailed p value; statistical significance was defined as p < 0.05. Additionally, multivariate logistic regression analysis (MVA) adjusting for confounding factors including age, body mass index (BMI), and comorbidities was performed. MVA was additionally performed on cases involving perforation to identify the outcomes in these high-risk clinical scenarios. All data were analyzed using Statistical Analysis Software, version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
Laparoscopic appendectomy
Patient characteristics
A total of 1335 pregnant patients underwent appendectomy between 2005 and 2012 in NSQIP hospitals: 894 were laparoscopic cases (LA) and 441 were performed open (OA). Full demographics and patient characteristics are listed in Table 1. Patients undergoing LA compared to OA were of equal age (27.7 ± 6.2 vs. 28.2 ± 6.3 years, p = 0.19), race (76.4 % Caucasian vs. 76.7 % Caucasian, p = 0.93), and comorbidities except for a lower body mass index (BMI) (27.9 ± 6.9 vs. 28.4 ± 6.1 kg/m2, p = 0.03). Compared to OA, patients who underwent LA had equal tobacco use within the last year (19.0 vs. 16.1 %, p = 0.19) but an increased pack year history (0.85 ± 5.6 vs. 0.42 ± 1.9, p = 0.04). They had equivalent low rates of chronic obstructive pulmonary disease (0.11 vs. 0 %, p = 1.0), congestive heart failure (0.11 vs. 0 %, p = 1.0), and renal failure (0.11 vs. 0 %, p = 1.0). Inpatient status was higher for the OA patients compared to the LA group (95.5 vs. 80.7 %, p ≤ 0.0001).
Operative characteristics
Full operative details are listed in Table 2. Overall, most appendectomies were performed by General Surgeons (99.5 %) with equally low rates in the LA and OA groups performed by OB/GYN physicians (0.11 vs. 0.23 %, respectively, p = 0.6). General anesthesia was used in the majority of cases (95.1 %), with a higher use of spinal anesthesia in the OA group versus LA (12.7 vs. 0.67 %, p = <0.0001). A total of 71 patients (7.9 %) in the LA group were identified as high risk with a designation of perforation compared to 49 (11.1 %) in the open group (p = 0.06). For operative time, in univariate analysis, LA versus OA was significantly different (47.1 ± 20.2 vs. 52.1 ± 25.1 min, p < 0.001). Following MVA, which controlled for confounding factors, a statistically significant difference remained with an adjusted mean (± SE) of 51.7 ± 2.8 min in the LA group compared to 57.3 ± 3.0 min in the OA group (p < 0.0001). In MVA for cases of perforation alone, operative time for LA with adjusted mean (± SE) of 60.2 ± 14.0 min was not significantly different compared to 67.4 ± 14.8 min in the OA group (p = 0.19).
Outcomes
In univariate analysis, the average LOS was shorter in the LA versus the OA groups (2.3 ± 5.8 vs. 3.3 ± 2.5 days, p < 0.0001), and this difference remained significant after MVA controlled for confounding factors of age, BMI, and comorbidities with an adjusted mean (± SE) (2.7 ± 0.7 vs. 3.7 ± 0.7 days, p = 0.003). Even in cases of perforation after MVA, LOS was shorter for LA compared to OA with an adjusted mean (± SE) of 2.3 ± 1.4 versus 4.5 ± 1.5 days, respectively (p = 0.0002). In univariate analysis of complication outcomes for LA versus OA, overall wound complications favored LA over OA (0.67 vs. 3.9 %, p < 0.0001), as well as minor complications (2.8 vs. 5.4 %, p = 0.02); they had equally low rates of major complications (1.2 vs. 1.6 %, p = 0.6). There was one reported case of threatened preterm labor for each approach (p > 0.5). In MVA, overall wound complications were higher in OA patients compared to LA with an odds ratio (OR) of 6.4 (95 % confidence interval (CI) 2.5–16.0, p < 0.0001); the same was true for superficial SSI (OR 6.0, 95 % CI 2.2–16.6, p = 0.0005). OA patients also had 2.5 times increased odds of minor complications versus LA (95 % CI 1.3–4.5, p = 0.004). For cases of perforation in MVA, OA remained at an increased risk for overall wound complications with an OR 6.2 (95 % CI 1.1–33.8, p = 0.04). Details of outcomes for univariate and multivariate analyses are as outlined in Tables 3 and 4, respectively. Return to the operating room was equivalent for LA versus OA (1.5 vs. 2.7 %, p = 0.11), and no 30-day maternal mortality was identified for either operative approach.
Laparoscopic cholecystectomy
Patient characteristics
A total of 664 pregnant patients undergoing cholecystectomy were identified in the NSQIP database between 2005 and 2012; 606 cases were performed laparoscopically (LC) and 58 open (OC). Full demographics and patient characteristics are listed in Table 5. Patients who underwent LC compared to OC were of equal age (28.3 ± 6.5 vs. 28.7 ± 9.8 years, p = 0.33), and the majority of patients were Caucasian (70.6 vs. 66 %, p = 0.48), with equivalent comorbidities except for an increased rate of hypertension (3.3 vs. 8.6 %, p = 0.04). For the LC compared to the OC, there were equal rates of current tobacco use and history of use. Inpatient status was higher for the OC patients compared to LC (98.3 vs. 65.2 %, p < 0.0001).
Operative characteristics
Complete operative details are listed in Table 6. Overall, most cholecystectomies were performed by General Surgeons (99.6 %) with equal rates of other services performing cholecystectomies in the LC and OC groups (0.5 vs. 0 %, respectively, p = 1.0). General anesthesia was used in nearly all cases (99.7 %), with no difference in other types of anesthetic use (0.33 vs. 0 %, p = 1.0). A total of 35 patients (5.8 %) in the LC group were identified as high risk with a designation of perforation compared to two (3.5 %) among the OC patients (p = 0.76). Additionally, patients diagnosed with cholecystitis with associated biliary obstruction occurred in 1.2 % of the LC patients versus 1.7 %, in those undergoing OC (p = 0.52). For operative time in univariate analysis, LC versus OC had a significant difference (64.4 ± 29.7 vs. 110.6 ± 82.3 min, p < 0.0001), and after MVA controlling for confounding factors, a significant difference remained with an adjusted mean (± SE) of 65.6 ± 5.0 min in the LC group compared to 111.3 ± 6.9 min in the OC group (p < 0.0001). In MVA for cases of perforation, operative times in LC appeared shorter with adjusted mean (± SE) of 52.6 ± 17.2 min in the LC group compared to 95.7 ± 32 min in the OC group but was not statistically significant (p = 0.1).
Outcomes
In univariate analysis, the average LOS was shorter following LC versus the OC (3.0 ± 4.1 vs. 6.5 ± 7.8 days, p < 0.0001), and this difference remained statically significant on MVA after controlling for the confounding factors of age, BMI, and comorbidities with an adjusted mean (± SE) of 3.6 ± 0.6 versus 7.2 ± 0.8 days (p < 0.0001). In the evaluation of perforated cases with MVA, LOS was equivalent in the LC group with an adjusted mean (± SE) of 3.3 ± 1.2 versus 6.1 ± 2.1 days than in the OC (p = 0.11). In univariate analysis of complications for LC versus OC, overall wound complications appeared to trend toward being in favor of LC over OC (0.66 vs. 3.5 %, p = 0.09) and were significantly less for minor complications (1.7 vs. 6.9 %, p = 0.03). A low but equal rate of major complications were seen (0.66 vs. 1.7 %, p = 0.37). In MVA, OC patients were at increased risk of minor complications, with an OR of 5.2 (95 % CI 1.7–15.6, p = 0.004). For cases of perforation, MVA demonstrated that OC did not have a statistically significant increased risk of minor complications as so few events occurred (p > 0.05). Details of outcomes for univariate and multivariate analyses are as outlined in Tables 7 and 8, respectively. Return to the operating room was equivalent for LC versus OC (1.5 vs. 3.5 %, p = 0.25), and no 30-day maternal mortality was identified for either operative approach.
Approach over time
Appendectomy
For appendectomy, the majority of LAs were performed in the last 4 years (TP2: 2009–2012) versus the first 4 years of the NSQIP database (TP1: 2005–2008) (60.7 vs. 39.3 %, p < 0.001), and the percentage of patients undergoing LA increased over time (62 vs. 71 %, p = 0.001). Inpatient status for LA decreased over time (85.8 vs. 77.4 %, p = 0.002) and similarly for OA (97.7 vs. 93.4 %, p = 0.03), although the majority still required an inpatient stay. For LA, operative time decreased from TP1 to TP2 (49.5 ± 21.4 vs. 45.5 ± 19.3 min, p = 0.009). Operative time for OA in TP1 versus TP2 remained the same (51.7 ± 24.5 vs. 52.4 ± 25.7 min, p = 0.8). LOS decreased over time for LA (2.6 ± 6.9 vs. 2.1 ± 4.9 days, p = 0.007) but remained the same for OA (3.3 ± 2.6 vs. 3.3 ± 2.4 days, p = 0.99).
Cholecystectomy
For cholecystectomy, the proportion of LC cases trended toward an increase over time (89 vs. 93 %, p = 0.06); a similar number of LC cases were seen when comparing the early years (TP1) versus the later years (TP2) (53 vs. 48 %, p = 0.22). Inpatient status for LC remained the same over time (67.4 vs. 63.2 %, p = 0.28) and similarly for OC (100 vs. 95.7 %, p = 0.4), with the majority still requiring an inpatient stay. Operative times were similar from TP1 to TP2 for LC (66.0 ± 31.1 vs. 62.9 ± 28.2 min, p = 0.22) and OC (121 ± 99.7 vs. 94.8 ± 41.8 min, p = 0.67). LOS remained similar over time as well for LC (3.0 ± 3.6 vs. 2.9 ± 4.5 days, p = 0.28) and OC (7.2 ± 9.9 vs. 5.4 ± 2.6 days, p = 0.53).
Discussion
In this study of 1999 pregnant patients over 8 years, the laparoscopic approach to appendectomy and cholecystectomy resulted in a significant decrease in operative time, length of stay, and minor complications compared to open surgery. Furthermore, LA patients had fewer wound and overall major complications compared to those undergoing an open operation. Even after controlling for confounding patient factors, the LC and LA groups had a significant reduction in overall minor and wound complications, operative time, and length of stay. In cases of perforation, LA had a shorter LOS when contrasted to the open approach. Unfortunately, fetal outcomes were not captured within the NSQIP database.
The use of laparoscopy throughout all trimesters has not always been widely accepted [12–14], but in numerous series published during the course of the last 25 years, laparoscopy has been cited as used during all trimesters [15–29]. The first described case of laparoscopic appendectomy was performed during the 8th week of pregnancy, followed thereafter with a 1990 case series of six patients averaging 16.3 weeks of gestation; each had no reported complications. Overall, when considering the effects of laparoscopic appendectomy on fetal outcomes, reported rates of fetal demise are low, ranging from 0 to 4.8 % [19, 20, 22, 30–33]. According to the CDC, the current rate of fetal loss surveying all pregnancies in the USA excluding elective abortions is 17 % [34]. Preterm labor or preterm delivery has been identified after laparoscopic appendectomy, although rates remain low ranging from 0 to 29 % with a median of 8.1 % [12, 19–22, 24, 30–32, 35]. While the event of intrauterine insufflation causing preterm delivery and fetal demise has been reported [36], the event is quite rare. Techniques such as no insufflation until after scope visualization of the intraperitoneal cavity are recommended due to the risk of uterine injury [20]. The literature reports operative times in laparoscopic appendectomy ranging from 29.9 to 64 min compared to 28.9–58 min in the open approach [12, 19–22, 24, 30, 31, 37]. Likewise, length of stay in single-center series publications ranged from 1.2 to 4.7 days for laparoscopic appendectomy versus 1.4–6.9 days in open appendectomy [19, 21–23, 30, 31, 35]. Our study had a perforated appendicitis rate of 7.9–11.1 %, similar to current reported rates of 7–26 % [20, 22–24, 31, 38]. Although not captured here, rates of negative appendectomy range from 23 to 43 % [24, 32, 39]; considering the risks of surgery, increasing diagnostic accuracy is beneficial. Yet, diagnostic efficiency is also important given that rates of perforated appendicitis in the pregnant patient increase to 43 % if symptoms persist for longer than 24 h [40]. Concerns of worsened fetal outcomes are associated with cases of perforated appendicitis with increased rates of fetal demise reported as high as 14 % [39]. When evaluating the difference in clinical presentation, recent studies have evaluated the location of the appendix frequently being displaced to the right upper quadrant or outside a radius of 45 mm from the iliac crest [41, 42], and correlation between change in location of appendix and point of maximal tenderness has been seen [43]. To make the appropriate diagnosis, imaging is recommended over clinical judgment alone. Given its safety in these cases, the most effective strategy may be magnetic resonance imaging (MRI). MRI is associated with a negative appendectomy rate of 2.8 % compared to 7.5 % from computed tomography scan imaging with a comparable delay in diagnosis of 8 versus 5.8 %, respectively [44].
The first published article with respect to LC in a pregnant patient was published by Pucci et al. [45] as a case report of a woman in her third trimester with no report of postoperative complications or effect on maternal–fetal outcome. Current rates of fetal demise following laparoscopic cholecystectomy are low ranging from 0 to 5.2 % [24–29, 46–49]. Rates of preterm labor or preterm delivery average 0–20 % [24–26, 47–49] for laparoscopic cholecystectomy. Little evidence exists of these preterm deliveries’ effect on the fetus with commonly stated APGAR (appearance, pulse, grimace, activity, respiration) scores at 1 and 5 min ranging 7–9 and 8.9–9, respectively [46, 47, 50]. When examining operative outcomes for cholecystectomy comparing the laparoscopic and open approach, operative times averaged 59–93 versus 49–118 minutes for LC and OC, respectively [24–26, 28, 46, 47, 49]; these are similar to our findings of longer operative times in the open approach. When considering the risks associated to evaluate the duct in the operating room for a pregnant patient, an intraoperative cholangiogram ranges between 0.02 and 0.05 cGy (centrigray) [51] while ERCP averages 0.04 cGy [52], all within an acceptable exposure range during pregnancy under 5 cGy with the additional practice of shielding the fetus during the procedure [53]. Yet, intraoperative ultrasound can be the safest approach as it negates the risk of bleeding and pancreatitis that can be associated with ERCP, but requires a skilled laparoscopist for accurate interpretation [54]. When considering operating on a pregnant patient in cases of biliary colic and symptomatic cholelithiasis, comparisons of surgery versus watchful waiting have demonstrated that relapse of symptoms requiring hospitalization range from 23 to 38 % and commonly require operation after readmission [29, 48].
Historically, the second trimester has been considered the safest time to operate and deferment until that time period, if possible, was recommended [55–57]. However, many review studies, including the current SAGES (Society of American Gastrointestinal and Endoscopic Surgeons) guidelines, do not limit the trimester that the laparoscopic approach can be utilized as outcomes of fetal loss and preterm delivery demonstrate equivalent risk [15, 16, 58, 59]. Yet, some studies have argued that the third trimester is higher risk upon initial access secondary to the gravid uterus [13, 60]. Repositioning of the trocars is recommended [24, 37, 58–62] which has been described by gaining initial access in the midline halfway between the xiphoid and umbilicus [60] or in the location of the left midclavicular subcostal margin (Palmer’s point) [63] as feasible and safe. Additional considerations during the procedure include maintaining CO2 insufflation between 12 and 15 mmHg [8, 58, 61] and, especially in the third trimester, placing the patient in a left lateral decubitus position [8, 58, 62, 63]. The central dictum of treatment emphasizes the best way to take of the baby is to take care of the mother, as we have applied throughout time for such disciplines as trauma emergency care [64, 65].
Limitations
This study is limited due to the inability to evaluate fetal outcomes as it is not identified within the NSQIP dataset. In addition, maternal obstetric outcomes affected by surgery beyond 30 days are not part of the data collected. Additionally, gestational age or trimester of pregnancy would be helpful pieces of information when delineating trends and outcomes.
Conclusion
While the incidence of fetal events is unknown, this study of nearly two thousand laparoscopic appendectomies and laparoscopic cholecystectomies performed across the country in pregnant patients demonstrated shorter operative time, length of stay, and reduced wound complications even when controlling for confounding variables. We also demonstrate that the use of laparoscopy has increased for both appendectomy and cholecystectomy over time. Even in the case of perforated appendix or gallbladder, laparoscopy appears safe in pregnant patients when looking at the mother.
References
Augustin G, Majerovic M (2007) Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol 131(1):4–12 Epub 2006/09/20
Choi JJ, Mustafa R, Lynn ET, Divino CM (2011) Appendectomy during pregnancy: follow-up of progeny. J Am Coll Surg 213(5):627–632 Epub 2011/08/23
Wittich AC, DeSantis RA, Lockrow EG (1999) Appendectomy during pregnancy: a survey of two army medical activities. Mil Med 164(10):671–674 Epub 1999/11/02
Gilo NB, Amini D, Landy HJ (2009) Appendicitis and cholecystitis in pregnancy. Clin Obstet Gynecol 52(4):586–596 Epub 2010/04/16
Biscette S, Yoost J, Hertweck P, Reinstine J (2011) Laparoscopy in pregnancy and the pediatric patient. Obstet Gynecol Clin N Am 38(4):757–776 Epub 2011/12/03
Iafrati MD, Yarnell R, Schwaitzberg SD (1995) Gasless laparoscopic cholecystectomy in pregnancy. J Laparoendosc Surg 5(2):127–130 Epub 1995/04/01
Sesti F, Pietropolli A, Sesti FF, Piccione E (2013) Gasless laparoscopic surgery during pregnancy: evaluation of its role and usefulness. Eur J Obstet Gynecol Reprod Biol 170(1):8–12 Epub 2013/06/12
Bhavani-Shankar K, Steinbrook RA, Brooks DC, Datta S (2000) Arterial to end-tidal carbon dioxide pressure difference during laparoscopic surgery in pregnancy. Anesthesiology 93(2):370–373 Epub 2000/07/26
Khuri SF, Daley J, Henderson W, Barbour G, Lowry P, Irvin G et al (1995) The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg 180(5):519–531 Epub 1995/05/01
Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB et al (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228(4):491–507 Epub 1998/10/28
Ross SW, Oommen B, Wormer BA, Walters AL, Matthews BD, Heniford BT et al (2015) National outcomes of laparoscopic Heller myotomy: operative complications and risk factors for adverse events. Surg Endosc. Epub 2015/01/16
Moreno-Sanz C, Pascual-Pedreno A, Picazo-Yeste JS, Seoane-Gonzalez JB (2007) Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. J Am Coll Surg 205(1):37–42 Epub 2007/07/10
Eom JM, Hong JH, Jeon SW, Choi JS, Lee JH, Kim HO et al (2012) Safety and clinical efficacy of laparoscopic appendectomy for pregnant women with acute appendicitis. Ann Acad Med Singap 41(2):82–86 Epub 2012/04/14
Holzer T, Pellegrinelli G, Morel P, Toso C (2011) Appendectomy during the third trimester of pregnancy in a 27-year old patient: case report of a “near miss” complication. Patient Saf Surg 5(1):11 Epub 2011/05/18
Walsh CA, Tang T, Walsh SR (2008) Laparoscopic versus open appendicectomy in pregnancy: a systematic review. Int J Surg 6(4):339–344 Epub 2008/03/18
Machado NO, Grant CS (2009) Laparoscopic appendicectomy in all trimesters of pregnancy. J Soc Laparoendosc Surg 13(3):384–390 Epub 2009/10/02
Schreiber JH (1987) Early experience with laparoscopic appendectomy in women. Surg Endosc 1(4):211–216 Epub 1987/01/01
Schreiber JH (1990) Laparoscopic appendectomy in pregnancy. Surg Endosc 4(2):100–102 Epub 1990/01/01
Gurbuz AT, Peetz ME (1997) The acute abdomen in the pregnant patient. Is there a role for laparoscopy? Surg Endosc 11(2):98–102 Epub 1997/02/01
Lemieux P, Rheaume P, Levesque I, Bujold E, Brochu G (2009) Laparoscopic appendectomy in pregnant patients: a review of 45 cases. Surg Endosc 23(8):1701–1705 Epub 2008/12/06
Jeong JS, Ryu DH, Yun HY, Jeong EH, Choi JW, Jang LC (2011) Laparoscopic appendectomy is a safe and beneficial procedure in pregnant women. Surg Laparosc Endosc Percutan Tech 21(1):24–27 Epub 2011/02/10
Chung JC, Cho GS, Shin EJ, Kim HC, Song OP (2013) Clinical outcomes compared between laparoscopic and open appendectomy in pregnant women. Can J Surg 56(5):341–346 Epub 2013/09/27
Peled Y, Hiersch L, Khalpari O, Wiznitzer A, Yogev Y, Pardo J (2014) Appendectomy during pregnancy—is pregnancy outcome depending by operation technique? J Matern Fetal Neonatal Med 27(4):365–367 Epub 2013/06/26
Rollins MD, Chan KJ, Price RR (2004) Laparoscopy for appendicitis and cholelithiasis during pregnancy: a new standard of care. Surg Endosc 18(2):237–241 Epub 2003/12/24
Abuabara SF, Gross GW, Sirinek KR (1997) Laparoscopic cholecystectomy during pregnancy is safe for both mother and fetus. J Gastrointest Surg 1(1):48–52 discussion Epub 1997/01/01
Glasgow RE, Visser BC, Harris HW, Patti MG, Kilpatrick SJ, Mulvihill SJ (1998) Changing management of gallstone disease during pregnancy. Surg Endosc 12(3):241–246 Epub 1998/04/16
Buser KB (2009) Laparoscopic surgery in the pregnant patient: results and recommendations. J Soc Laparoendosc Surg 13(1):32–35 Epub 2009/04/16
Othman MO, Stone E, Hashimi M, Parasher G (2012) Conservative management of cholelithiasis and its complications in pregnancy is associated with recurrent symptoms and more emergency department visits. Gastrointest Endosc 76(3):564–569 Epub 2012/06/27
Dhupar R, Smaldone GM, Hamad GG (2010) Is there a benefit to delaying cholecystectomy for symptomatic gallbladder disease during pregnancy? Surg Endosc 24(1):108–112 Epub 2009/06/12
Kirshtein B, Perry ZH, Avinoach E, Mizrahi S, Lantsberg L (2009) Safety of laparoscopic appendectomy during pregnancy. World J Surg 33(3):475–480 Epub 2009/01/13
Sadot E, Telem DA, Arora M, Butala P, Nguyen SQ, Divino CM (2010) Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc 24(2):383–389 Epub 2009/06/25
McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM (2007) Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg 205(4):534–540 Epub 2007/10/02
Corneille MG, Gallup TM, Bening T, Wolf SE, Brougher C, Myers JG et al (2010) The use of laparoscopic surgery in pregnancy: evaluation of safety and efficacy. Am J Surg 200(3):363–367 Epub 2010/08/31
Ventura SJ, Curtin SC, Abma JC, Henshaw SK (2012) Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990-2008. Natl Vital Stat Rep 60(7):1–21 Epub 2012/09/14
Cheng HT, Wang YC, Lo HC, Su LT, Soh KS, Tzeng CW et al (2014) Laparoscopic appendectomy versus open appendectomy in pregnancy: a population-based analysis of maternal outcome. Surg Endosc. Epub 2014/08/31
Friedman JD, Ramsey PS, Ramin KD, Berry C (2002) Pneumoamnion and pregnancy loss after second-trimester laparoscopic surgery. Obstet Gynecol 99(3):512–513 Epub 2002/02/28
Affleck DG, Handrahan DL, Egger MJ, Price RR (1999) The laparoscopic management of appendicitis and cholelithiasis during pregnancy. Am J Surg 178(6):523–529 Epub 2000/02/12
Flum DR, Morris A, Koepsell T, Dellinger EP (2001) Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA 286(14):1748–1753 Epub 2001/10/12
Ito K, Ito H, Whang EE, Tavakkolizadeh A (2012) Appendectomy in pregnancy: evaluation of the risks of a negative appendectomy. Am J Surg 203(2):145–150 Epub 2011/07/26
Tamir IL, Bongard FS, Klein SR (1990) Acute appendicitis in the pregnant patient. Am J Surg 160(6):571–575 discussion 5-6. Epub 1990/12/01
Pates JA, Avendanio TC, Zaretsky MV, McIntire DD, Twickler DM (2009) The appendix in pregnancy: confirming historical observations with a contemporary modality. Obstet Gynecol 114(4):805–808 Epub 2009/11/06
House JB, Bourne CL, Seymour HM, Brewer KL (2014) Location of the appendix in the gravid patient. J Emerg Med 46(5):741–744 Epub 2014/02/04
Hodjati H, Kazerooni T (2003) Location of the appendix in the gravid patient: a re-evaluation of the established concept. Int J Gynaecol Obstet 81(3):245–247 Epub 2003/05/28
Kastenberg ZJ, Hurley MP, Luan A, Vasu-Devan V, Spain DA, Owens DK et al (2013) Cost-effectiveness of preoperative imaging for appendicitis after indeterminate ultrasonography in the second or third trimester of pregnancy. Obstet Gynecol 122(4):821–829 Epub 2013/10/03
Pucci RO, Seed RW (1991) Case report of laparoscopic cholecystectomy in the third trimester of pregnancy. Am J Obstet Gynecol 165(2):401–402 Epub 1991/08/01
Barone JE, Bears S, Chen S, Tsai J, Russell JC (1999) Outcome study of cholecystectomy during pregnancy. Am J Surg 177(3):232–236 Epub 1999/04/29
Curet MJ, Allen D, Josloff RK, Pitcher DE, Curet LB, Miscall BG et al (1996) Laparoscopy during pregnancy. Arch Surg 131(5):546–550 discussion 50-1. Epub 1996/05/01
Lu EJ, Curet MJ, El-Sayed YY, Kirkwood KS (2004) Medical versus surgical management of biliary tract disease in pregnancy. Am J Surg 188(6):755–759 Epub 2004/12/28
Cosenza CA, Saffari B, Jabbour N, Stain SC, Garry D, Parekh D et al (1999) Surgical management of biliary gallstone disease during pregnancy. Am J Surg 178(6):545–548 Epub 2000/02/12
Sungler P, Heinerman PM, Steiner H, Waclawiczek HW, Holzinger J, Mayer F et al (2000) Laparoscopic cholecystectomy and interventional endoscopy for gallstone complications during pregnancy. Surg Endosc 14(3):267–271 Epub 2000/03/31
Karthikesalingam A, Markar SR, Weerakkody R, Walsh SR, Carroll N, Praseedom RK (2009) Radiation exposure during laparoscopic cholecystectomy with routine intraoperative cholangiography. Surg Endosc 23(8):1845–1848 Epub 2009/01/02
Kahaleh M, Hartwell GD, Arseneau KO, Pajewski TN, Mullick T, Isin G et al (2004) Safety and efficacy of ERCP in pregnancy. Gastrointest Endosc 60(2):287–292 Epub 2004/07/28
Mossman KL, Hill LT (1982) Radiation risks in pregnancy. Obstet Gynecol 60(2):237–242 Epub 1982/08/01
Machi J, Tateishi T, Oishi AJ, Furumoto NL, Oishi RH, Uchida S et al (1999) Laparoscopic ultrasonography versus operative cholangiography during laparoscopic cholecystectomy: review of the literature and a comparison with open intraoperative ultrasonography. J Am Coll Surg 188(4):360–367 Epub 1999/04/09
Committee SG (1998) Guidelines for laparoscopic surgery during pregnancy. Society of American Gastrointestinal Endoscopic Surgeons (SAGES). Surg Endosc 12(2):189–190. Epub 1998/02/28
Fatum M, Rojansky N (2001) Laparoscopic surgery during pregnancy. Obstet Gynecol Surv 56(1):50–59 Epub 2001/01/05
Date RS, Kaushal M, Ramesh A (2008) A review of the management of gallstone disease and its complications in pregnancy. Am J Surg 196(4):599–608 Epub 2008/07/11
Guidelines Committee of the Society of American G, Endoscopic S, Yumi H (2008) Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy: this statement was reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), September 2007. It was prepared by the SAGES Guidelines Committee. Surg Endosc 22(4):849–861. Epub 2008/02/22
Jackson H, Granger S, Price R, Rollins M, Earle D, Richardson W et al (2008) Diagnosis and laparoscopic treatment of surgical diseases during pregnancy: an evidence-based review. Surg Endosc 22(9):1917–1927 Epub 2008/06/17
de Perrot M, Jenny A, Morales M, Kohlik M, Morel P (2000) Laparoscopic appendectomy during pregnancy. Surg Laparosc Endosc Percutan Tech 10(6):368–371 Epub 2001/01/09
Malangoni MA (2003) Gastrointestinal surgery and pregnancy. Gastroenterol Clin N Am 32(1):181–200 Epub 2003/03/15
Nezhat FR, Tazuke S, Nezhat CH, Seidman DS, Phillips DR, Nezhat CR (1997) Laparoscopy during pregnancy: a literature review. J Soc Laparoendosc Surg 1(1):17–27 Epub 1997/01/01
Chohan L, Kilpatrick CC (2009) Laparoscopy in pregnancy: a literature review. Clin Obstet Gynecol 52(4):557–569 Epub 2010/04/16
Shah KH, Simons RK, Holbrook T, Fortlage D, Winchell RJ, Hoyt DB (1998) Trauma in pregnancy: maternal and fetal outcomes. J Trauma 45(1):83–86 Epub 1998/07/29
Drost TF, Rosemurgy AS, Sherman HF, Scott LM, Williams JK (1990) Major trauma in pregnant women: maternal/fetal outcome. J Trauma 30(5):574–578 Epub 1990/05/01
Disclosures
Drs. Heniford, Augenstein, and Lincourt have previously been awarded surgical research and education grants and honoraria from W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Inc. Drs. Cox, Huntington, Blair, and Tanushree Prasad have no potential conflicts or disclosures relevant to this work.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cox, T.C., Huntington, C.R., Blair, L.J. et al. Laparoscopic appendectomy and cholecystectomy versus open: a study in 1999 pregnant patients. Surg Endosc 30, 593–602 (2016). https://doi.org/10.1007/s00464-015-4244-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4244-4