Abstract
Background
For many years, intraoperative cholangiography during cholecystectomy to aid definition of the biliary anatomy and to detect choledocholithiasis has been advocated. Although radiation exposure in fluoroscopic procedures is a concern, few available data exist regarding the radiation exposure incurred during intraoperative cholangiography. This study aimed to determine the average radiation exposure sustained during this procedure.
Methods
Radiation dose data were recorded between 5 September 2007 and 21 July 2008 for 108 consecutive patients undergoing laparoscopic cholecystectomy with intraoperative cholangiography. Dose area product values were used to calculate the entrance skin dose, an indicator of potential skin damage, and the effective dose, an indicator of long-term cancer risk, for each patient.
Results
The median age of the 108 patients (67% females) included in the data analysis was 51 years (range, 17–87 years). The mean entrance skin dose during intraoperative cholangiography was 0.0069 ± 0.0066 Gy, and the mean effective dose was 0.18 ± 0.17 mSv. No results exceeded the threshold of 2 Gy for skin damage, and the lifetime risk for the development of new cancer due to intraoperative cholangiography was less than 0.001%.
Conclusion
Radiation doses administered during intraoperative cholangiography are safe and do not represent a contraindication to this procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
For many years, intraoperative cholangiography during cholecystectomy to aid definition of the biliary anatomy and to detect choledocholithiasis has been advocated [1]. However, there remains local and national heterogeneity in the implementation of routine or selective policies for intraoperative cholangiography during laparoscopic cholecystectomy.
The evidence base is equivocal, and to date, no randomized controlled trial has been conducted to demonstrate a definite reduction in postoperative complications after laparoscopic cholecystectomy with the routine use of intraoperative cholangiography compared with a selective policy. Nevertheless, some authors assert that intraoperative cholangiography should be performed routinely for all patients undergoing laparoscopic cholecystectomy because this allows early detection of bile duct injury [2], whereas others advocate a selective policy of intraoperative cholangiography in laparoscopic cholecystectomy [3].
Although increased radiation exposure in routine intraoperative cholangiography is a concern [3], few data are available regarding the radiation exposure incurred as part of the procedure. Radiation exposure may cause skin damage in the short term and increased cancer risk in the long term [4]. This study therefore aimed to determine the average radiation exposure sustained during laparoscopic cholecystectomy with routine intraoperative cholangiography.
Methods
From 5 September 2007 to 21 July 2008, the study enrolled 121 patients undergoing laparoscopic cholecystectomy in a single tertiary referral hepatopancreaticobiliary unit. Radiation dose data such as time of exposure and dose area product (DAP) were obtained from the hospital computed radiology information system database (CRIS, Healthcare Software Systems, Derby, UK). The entrance skin dose (ESD) and the effective dose (ED) were calculated as described later. Radiographic exposure was under the control of the operating surgeon.
Intraoperative cholangiography
All patients undergoing laparoscopic cholecystectomy in the hepatopancreaticobiliary unit had attempted intraoperative cholangiography. The cystic duct was isolated and cannulated with a 5-Fr infant feeding tube (Unomedical, New South Wales, Australia) for performance of intraoperative cholangiography. To obtain the cholangiogram, 20 ml of Urograffin 150 (Scherring Healthcare Ltd, West Sussex, UK) was injected in 2- to 3-ml bursts. The presence of abnormal anatomy, choledocholithiasis, and flow of contrast into the second part of the duodenum were noted. Incidentally detected choledocholithiasis at intraoperative cholangiography was managed preferentially using postoperative endoscopic retrograde cholangiopancreatography (ERCP). None of the patients underwent laparoscopic bile duct exploration.
The procedures were performed in an operating theater using the same model of a mobile C-arm device (Siemens Siremobil Compact L; Siemens UK, Camberley, UK) with image intensifier sizes of 17 and 23 cm as well as filtration of 3 mm Al. The imaging was posteroanterior, with the anode placed below the operating table (Maquet Alphamaxx; Maquet, Rustatt, Germany). The distance between the X-ray tube focus and the patient was estimated to be about 30 to 50 cm depending on the thickness of the patient. For the purpose of calculating skin dose, it was considered to be 40 cm.
The radiation doses were measured by the DAP in cGy/cm2 using an inbuilt ionization chamber. The DAP is the absorbed dose-to-air averaged over the area of the X-ray beam in a plane perpendicular to the beam axis multiplied by the area of the beam in that plane. Measurement of DAP thus gives an indication of the total radiation energy received by the patient. With a knowledge of the organs and tissues irradiated, conversion factors can be used to convert the DAP into an effective radiation dose.
The installed DAP meter was calibrated by means of an independent DAP meter (VacuDAP 2000; VacuTec Meβtechnik, Dresden, Germany) with traceable calibration. The DAP values were entered manually into an online database at the time of the procedure. The equipment also was audited regularly and subjected to 6-month servicing by the manufacturer.
Exposure calculations
The DAP values from the C-arm were used to calculate the ED. The ESD reflects the amount of radiation absorbed at any given point on the skin and corresponds to the risk for skin damage. The incidence of skin damage increases significantly once a threshold of 2 Gy is exceeded.
The ESD was calculated from the DAP based on an X-ray beam diameter of 23 cm at the image intensifier and therefore was approximately a 9 × 9-cm beam at the patient’s skin. To account for the fact that the X-ray field is not always sited at the same place on the patient’s skin but may cover an area approximately three times the instantaneous beam area, the calculation was repeated using an area of 243 cm2.
The ED is an indicator of the risk for radiation-induced malignancy later in life after exposure to a given level of radiation. The ED was derived from the DAP data by the PCXMC 1·5 computer program (STUK; Radiation and Nuclear Safety Authority, Helsinki, Finland). These calculations assumed a tube voltage of 90 kVp.
Results
The radiation dose data were recorded between 5 September 2007 and 21 July 2008 for 121 consecutive patients undergoing laparoscopic cholecystectomy with intraoperative cholangiography. Data from 13 patients were incomplete, so these patients were excluded from the study. The median age of the remaining 108 patients (67% females) included in the data analysis was 51 years (range, 17–87 years) (Fig. 1). There were no bile duct injuries in this cohort of patients, and no patients underwent laparoscopic bile duct exploration.
During the same study period, a further 8 patients underwent planned open cholecystectomy, 6 patients underwent conversion from laparoscopic to open cholecystectomy, and 20 patients underwent laparoscopic cholecystectomy without cholangiography due to technical difficulties. All these patients were therefore excluded from the study.
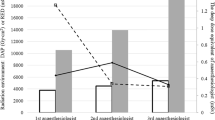
Based on an irradiation area of 243 cm2, the mean ESD during intraoperative cholangiography was 0.0069 ± 0.0066 Gy. This represents a low ESD, with no results approaching the threshold of 2 Gy for skin damage. The mean ED for intraoperative cholangiography was 0.18 ± 0.17 mSv (Table 1).
Based on epidemiologic studies suggesting a 5% risk for the development of lethal cancer per sievert of radiation exposure [5], the lifetime risk for the development of new cancer due to intracholangiography equals less than 0.001%.
Discussion
Although intraoperative cholangiography is common, no studies have investigated the degree of radiation exposure experienced by patients in clinical practice. As reflected in our sample, many patients undergoing laparoscopic cholecystectomy with intraoperative cholangiography are young, including females of childbearing age (Fig. 1). Therefore, a consideration of actual radiation exposure levels during intraoperative cholangiography in clinical practice is of clinical importance.
In addition to increasing the risk for cancer, radiation exposure causes skin damage through a deterministic mechanism. Skin damage is seen when radiation exposure exceeds a threshold dose that kills a critical number of cells [6]. A 2-Gy radiation dose may cause transient damage to skin, clinically manifesting as erythema. Doses of 3 Gy may lead to transient hair loss, so 2 Gy is considered a safe threshold for radiation dose to skin [7].
The radiation dose has a stochastic effect on the development of malignancy. Although the probability of malignancy increases with the total dose of administered radiation, ultimate severity is independent of the total dose administered [7].
Long-term epidemiologic studies suggest a 5% risk for the development of lethal cancer per sievert of radiation exposure (with a mean latency of 10 to 20 years after exposure) [5]. Based on our estimated effective dose, the lifetime risk for the development of new cancer due to cholangiography therefore equals less than 0.001%. Deterministic effects such as skin damage have a well-defined threshold: approximately 2 Gy for any skin damage (erythema), as reinforced by the latest guidelines of the International Committee on Radiation Protection (ICRP) [5].
The maximum ESD of our cohort was 0.044 Gy. A threshold of 2.5 Gy is thought to induce sterility in reproductive tissue [5], and we can deduce from observed ESD that cholangiography will fall safely below this threshold.
The mean DAP observed in this study was among the lowest of all fluoroscopic radiologic procedures and equivalent to that seen in common orthopedic investigations such as plain limb radiographs [8] (Table 2). The radiation dose is a potentially harmful side effect of radiologic procedures, and concerns have recently been raised about high exposure entailed in endovascular repair of aortic aneurysms [9]. However, compared with this technically more complex and longer procedure, the calculated effective dose and DAP recorded in this study were 50 and 100 times lower, respectively (Table 2). This correlates with the relatively short mean screening time observed for cholangiography (0.53 min). The DAP in our cohort was 40 times lower than that seen in ERCP [10, 11]. This finding suggests that intraoperative cholangiography imparts a significantly lower radiation dose than that received by patients undergoing an ERCP.
Radiation absorption by medical staff was not recorded in this study. However, a strong correlation between staff radiation exposure and patient DAP data has been demonstrated [12]. Therefore, in light of the low DAP values and the protective equipment used by operating theater personnel during intraoperative cholangiography, staff radiation exposure is unlikely to be significant.
This study demonstrates that the levels of radiation exposure sustained during laparoscopic cholecystectomy with intraoperative cholangiography are safe. Therefore, the radiation dose sustained during intraoperative cholangiography does not represent a contraindication to this procedure.
References
Mirrizi P (1937) Operative cholangiography. Surg Gynecol Obstet 65:702–710
Connor S, Garden OJ (2006) Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg 93:158–168
Metcalfe MS, Ong T, Bruening MH, Iswariah H, Wemyss-Holden SA, Maddern GJ (2004) Is laparoscopic intraoperative cholangiogram a matter of routine? Am J Surg 187:475–481
International Commission on Radiological Protection (2000) Avoidance of radiation injuries from medical interventional procedures. ICRP Publication 85. Pergamon Press, Oxford
International Commission on Radiological Protection (2008) Recommendations of the ICRP annals of the ICRP v. 37/2-4. ICRP Publication 103. Elsevier, Stockholm
International Commission on Radiological Protection (1991) 1990 recommendations of the International Commission on Radiological Protection. ICRP Publication 60. Pergamon Press, Oxford
Miller DL, Balter S, Noonan PT, Georgia JD (2002) Minimizing radiation-induced skin injury in interventional radiology procedures. Radiology 225:329–336
Crawley MT, Rogers AT (2000) Dose-area product measurements in a range of common orthopaedic procedures and their possible use in establishing local diagnostic reference levels. Br J Radiol 73:740–744
Weerakkody RA, Walsh SR, Cousins C, Goldstone KE, Tang TY, Gaunt ME (2008) Radiation exposure during endovascular aneurysm repair. Br J Surg 95:699–702
Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM (1996) Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc 44:287–292
Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, Vassilaki AE, Maniatis PN, Karagiannis JA, Koulentianos ED (2003) Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosimetry 106:241–246
Williams JR (1997) Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Br J Radiol 70:498–503
Efstathopoulos EP, Karvouni E, Kottou S, Tzanalaridou E, Korovesis S, Giazitzoglou E, Katritsis DG (2004) Patient dosimetry during coronary interventions: a comprehensive analysis. Am Heart J 147:468–475
Miller DL, Balter S, Cole PE, Lu HT, Schueler BA, Geisinger M, Cardella JF, George JS, Miller GL III, Anderson J (2003) Radiation doses in interventional radiology procedures: the RAD-IR study: part I: overall measures of dose. J Vasc Interv Radiol 14:711–727
Miller DL, Balter S, Cole PE, Lu HT, Berenstein A, Albert R, Schueler BA, Georgia JD, Noonan PT, Russell EJ, Malisch TW, Vogelzang RL, Geisinger M, Cardella JF, George JS, Miller GL III, Anderson J (2003) Radiation doses in interventional radiology procedures: the RAD-IR study: part II: skin dose. J Vasc Interv Radiol 14:977–990
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karthikesalingam, A., Markar, S.R., Weerakkody, R. et al. Radiation exposure during laparoscopic cholecystectomy with routine intraoperative cholangiography. Surg Endosc 23, 1845–1848 (2009). https://doi.org/10.1007/s00464-008-0279-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0279-0