Abstract
This investigation assessed the impact of temporal resolution during a videofluoroscopic evaluation of swallowing (VFSS) on measures of duration and kinematics. Thirty adult and ten infant swallow studies, all acquired at 30 frames and 30 pulses per second, were obtained from a New Mexico hospital. All swallow studies were altered to simulate 15 and 5 pulses per second. Duration measures included pharyngeal response time, duration of upper esophageal sphincter (UES) opening, velopharyngeal closure duration and total swallow duration. Kinematic measures were assessed in adults only and included peak hyoid position and extent of UES opening during the swallow. Analysis of outcome measures was performed and compared across the three temporal resolutions (30, 15, and 5 pulses per second). For data points where normative values are available, we evaluated the impact of temporal resolution on clinical determination (i.e., did a change in pulse rate alter the clinical classification). Kinematic and duration measures were altered with changes in pulse rate and these changes increased as temporal resolution decreased. For outcome measures where normative values are available, accuracy of clinical determination decreased with decreased pulse rate. Temporal resolution impacts duration and kinematic measures. However, the direction of these changes is unpredictable, indicating sensitivity and specificity are both affected. Without a predictable impact, the use of lower pulse rates may alter clinical impressions and treatment recommendations yielding inappropriate treatment goals and treatment duration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Oropharyngeal swallowing disorders are often assessed via videofluoroscopic evaluation of swallowing (VFSS), a procedure that employs ionizing radiation. Current digital technology supports various acquisition factors, specifically frame rate and pulse rate. Pulse rate, or fluoroscopy rate, refers to the number of x-ray beams being administered per second. Each time the x-ray beam is pulsed an image is acquired. Frame rate refers to the number of stored images per second. In many modern fluoroscopes a setting of continuous equates to 30 pulses per second (PPS), and the frame rate is typically set to match the pulse rate for optimum viewing quality. When pulse rate is lowered and frame rate is maintained at 30 frames per second (FPS), the result is a reduction in unique images based on the pulse rate. For example, if 15 PPS are recorded at 30 FPS, the video will contain 30 FPS with 15 unique images each repeated twice.
For evaluation of swallowing, Steele [1] and Martin-Harris and colleagues [2] maintain that 30 unique images per second is the optimal temporal resolution, which means that data is acquired at 30 frames and 30 pulses per second. Yet, across the Unites States, VFSS is performed using pulse rates ranging from four to 30 pulses per second [1, 3]. While this manuscript is not meant to serve as a tutorial on radiographic terminology, it is helpful to understand that by reducing frame rate (number of stored images per second) or pulse rate (the number of unique fluoroscopic images), you are reducing the temporal resolution of the study. Although high resolution may improve our understanding of the swallow physiology, higher resolution comes with greater radiation exposure.
Figure 1 visually highlights the challenge of assessing swallow function using VFSS. In brief, the radiation dose associated with an exam is related to pulse rate and study duration. While there are other notable variables that link to radiation exposure (e.g., tissue density), this paper focuses on a variable that is under the control of the practitioner—pulse rate. The risk of cancer, although relatively low [4], increases as radiation exposure increases [5], particularly in the thyroid gland [6], and radiation absorption is greater in pediatric patients [7, 8]. Standardized study procedures, such as the MBSImP, may help to reduce study duration thereby lowering radiation exposure. However, currently there are no data evaluating changes in radiation exposure for pediatric patients when a validated standardized protocol is followed [6]. The concept of ALARA, or As Low as Reasonably Achievable [9], explains that any procedure involving ionizing radiation must keep exposure as low as possible while still achieving the task at hand. To justify a procedure, its benefit must exceed the risk of the radiation exposure itself. A typical response to protect patients is to lower the radiation exposure. To do this, one can reduce the total duration of the videofluoroscopic exam and/or reduce the pulse rate. While a lower acquisition rate yields a lower radiation dose, it also reduces the temporal resolution, thereby sacrificing some of the details which may be necessary to determine diagnoses and dictate treatment decisions.
Bonilha and colleagues [10] illustrated the clinical consequences of reduced pulse rate by noting changes in six of the 17 MBSImP scores across five different patients, which ultimately altered treatment recommendations. Although there are multiple variables that may influence interpretation of videofluoroscopic swallow studies, this investigation is focused on timing (duration) and movement (kinematics). Reductions in temporal resolution (i.e., data acquisition rate) may impact the interpretation of the assessment by altering our ability to obtain accurate measures of the timing of swallow events, such as the bolus entering the pharynx, swallow initiation, the bolus entering the upper esophageal sphincter, or pharyngeal transit time, and the kinematic actions associated with the swallow, such as maximal height of hyo-laryngeal elevation and extent of UES opening [10, 11].
The purpose of this investigation was to increase or reinforce our current knowledge of the balance between reducing radiation exposure by lowering the pulse rate while maintaining a high diagnostic yield across the age range of individuals with feeding and swallowing disorders. The first aim was to evaluate the impact of lower pulse rates on (a) measures of swallow duration in adult and infant swallow studies, and (b) kinematic measures in adults. This was accomplished by using swallow studies acquired using 30 frames/pulses per second as a standard and comparing measures from two lower pulse rates —15 pulses per second and 5 pulses per second. The second aim was to assess if lower pulse rates altered the clinical interpretation of a given measure. Specifically, using available normative data, we evaluated if clinical determination (i.e., within normal limits or outside normal limits) changed as a function of pulse rate.
Methods
Experiment 1: Impact of Pulse Rate on Duration and Kinematic Measures in Adult Swallow Studies
Participants
In this retrospective within-subject design, we used VFSS data from 30 adults who were referred for an instrumental swallow evaluation due to a suspected swallowing problem. With a goal to portray generalizable variation in swallowing severity, we selected swallow studies from patients with varied complexity of oral intake. That is, we selected six studies each from individuals across five diet categories (Table 1). These participant criteria were used only in the identification of swallow studies to be included in this investigation. They were not used to cluster data analysis. Inclusion criteria was (1) that VFSS was originally recorded and stored at 30 FPS and PPS and (2) the VFSS included at least one 5 mL thin liquid swallow (IDDSI level 1), and one 5 mL extremely thick/pureed bolus swallow (IDDSI level 4).
Data collection
All swallow studies were imported into TIMS Medical Review Software for viewing. As the key concern is the difference in interpretation across pulse rates and not the actual interpretation, some typical aspects of videofluoroscopic analysis were eliminated in this evaluation of impact on duration and kinematic data. As is typical, duration and kinematic measures were extracted from individual swallows. Two specific bolus swallows were selected from each swallow study–5 mL thin liquid (IDDSI Level 1) and a spoonful of pudding or puree (IDDSI Level 4). These were chosen to provide an opportunity to observe the impact of changes in pulse rate on the swallow physiology across a range of viscosities while maintaining consistency across studies. In all selected views, the patient was seated in a lateral position, with no purposeful compensatory strategies implemented.
Studies were imported into FIJI software, a freely available image analysis software [12], and all 30 PPS videos were digitally resampled to simulate 15 and 5 pulses per second. To simulate a consistent frame rate and vary pulse rate, deleted frames were replaced with duplicates of prior images, thus eliminating unique images. The result was a total of two lower pulse rates to be evaluated and compared to the 30 PPS condition: 15 and 5 PPS.
Outcome measures
For this investigation we selected commonly used measures based on literature review. A summary of outcome measures is listed in Table 2. Swallow duration was assessed by measuring swallow reaction time (SRT) (aka, pharyngeal delay time), pharyngeal response time (PRT), and UES open duration (UESOD). These measures were calculated using the procedures described by Steele and colleagues [13]. Briefly, duration measures were calculated using the following time points–bolus passing the mandible (BPM), onset of hyoid burst (HYB), upper esophageal sphincter opening (UESO), upper esophageal sphincter closure (UESC), and swallow onset (SO). These time points were then used to calculate swallow durations. See Table 2 for formulas.
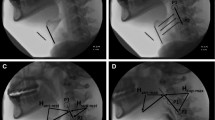
Kinematic measures included peak hyoid position (PHP) and the extent of UES opening (UESOE) associated with a swallow. Like Steele et al. [13], peak hyoid position (i.e., x-y coordinates) and extent of UES opening associated with the swallow were measured using a distance relative to the length and angle from the top (i.e., anterior-inferior corner) of C2 to the top (i.e., anterior-inferior corner) of C4. Measures are reported as a percent of the C2-C4 reference scaler.
Data analysis
Measures were completed using an iterative process. After extraction of measures from five participants for adults and two participants for infants, measures from two raters were compared. When differences occurred, these were reviewed until consensus was achieved. Consensus discussions resulted in refinement of rules for identification of time point measures.
Descriptive analysis, nonparametric statistical analysis, effect size, and clinical interpretation were performed on this data set. For each outcome measure, within a given subject, the 30 pulse condition was used as the standard for comparison. For descriptive analysis, two difference scores were calculated. Using 30 PPS as the benchmark for each outcome measure, 15 and 5 PPS were compared by calculating a difference between the data obtained from 30 PPS and each lower pulse rate. Across participants, there was no predictable trend in changes in duration (i.e., becoming longer or shorter with changes in pulse rate). Therefore, for descriptive and statistical analysis, absolute value was employed.
To compare differences from the measure obtained in the 30-pulse condition to the data obtained from the two lower pulse rate conditions, statistical analysis was performed using a Friedman test for analysis of repeated-measures which rank orders variables for a given participant with a 0.05 p value cut-off for significance. Post hoc pairwise comparisons were performed for statistically significant measures using a Wilcoxon Signed Ranks test.
For outcome measures where normative data are available, we evaluated if changes in temporal resolution (i.e., lower pulse rate) altered clinical interpretation. For adult videos, normative data were extracted from Steele et al. [13]. Data obtained from the 30 PPS condition were divided into those that were within normal limits (i.e., defined as within the 95th percent confidence interval for adult studies (95CI)) and those that were impaired (i.e., outside the 95CI). Agreement was assessed between the clinical determination obtained from the 30 PPS condition and the lower pulse rate conditions. Accuracy of agreement, which was calculated using the formula (TP + TN)/(TP + FN + FP + TN) where TP = true positive, TN = true negative, FP = false positive, FN = False negative, was calculated for 15 and 5 PPS when compared to the 30 PPS condition.
Experiment 2: Impact of Pulse Rate on Duration Measures in Infant Swallow Studies
Participants
Videofluoroscopic studies obtained from ten infants who were referred for an instrumental swallow evaluation due to feeding and/or swallowing problems were used in this investigation (Table 1). These studies were extracted from a publicly available repository of swallow studies [14]. With a goal to portray generalizable variation in feeding and swallowing severity, we selected five studies from infants who were NPO and being assessed for oral intake readiness and five studies from infants who had some degree of oral intake experience. Similar to experiment one, these participant criteria were used only in the identification of swallow studies to be included in this investigation and not for data analysis. Inclusion criteria was (1) that the VFSS was originally recorded and stored at 30 FPS and PPS and (2) the VFSS included at least one clearly visualized 10 s clip of bottle feeding.
Data collection
All swallow studies were imported into TIMS Medical Review Software for viewing. A ten second clip was chosen where there was limited movement artifact and consistent attempts at sucking from the bottle. Like experiment one, clips were imported into FIJI software, and digitally resampled to simulate 15 and 5 PPS.
Outcome measures
Swallow duration was assessed by measuring duration of velar contact associated with the swallow (VCD), UES open duration (UESOD), and total swallow duration (TSD). These measures were calculated using the procedures described by Dharmarathna and colleagues [15]. Briefly, duration measures were calculated using the following time points—downward mandibular thrust associated with expression from the bottle, onset of velum to pharyngeal wall (VPon), offset of velum from pharyngeal wall (VPoff), onset of upper esophageal sphincter opening (UESO), and upper esophageal sphincter closure (UESC) (Table 2).
Data analysis
Data and statistical analysis for experiment two mirrored the procedures employed in experiment one with one exception. Duration measures obtained from infant swallow studies were not compared to a normative database to assess impact of pulse rate on clinical determination. For infant studies, comparison of data to normative values is difficult given that available data sets are from infants who were referred for a swallow study due to feeding or swallowing concerns. See for example, Dharmarathna et al. [15] and Henderson et al. [16]. In this investigation, for infant videos we compared our data to the data available from this literature.
Reliability
Intra-rater reliability was performed on 10% of measures. Given the differing number of unique images across the pulse rate conditions, agreement was considered acceptable when a point was within a specified number of unique images. For the 30-pulse rate condition, we defined agreement as a range of plus or minus ten unique images. We narrowed it down to plus or minus five unique images for the 15-pulse rate condition, and further reduced it to plus or minus two unique images for the 5-pulse rate condition. Intra-rater agreement occurred with greater than 90% accuracy.
Inter-rater reliability was performed on all data points and was assessed by comparing the measures from two independent raters where at least one rater had more than 25 years of clinical experience. The intraclass correlation coefficient for the study variables was determined to be 0.93 (95% CI: 0.88, 0.96), indicating high reliability and a statistically significant association (p < 0.001). Although studies were reviewed in a random order and raters were blinded to the pulse rate condition, due to the differences in swallow detail, it was not hard for reviewers to determine the pulse rate while reviewing the video clips. When disagreement occurred, two raters reviewed the data points until consensus was achieved. The agreed upon data points were used in the data analysis.
Power Analysis
A power analysis was performed to assess if the number of samples used in these experiments were sufficient to test the hypothesis. For experiment one, post-hoc analysis revealed that power equals 0.84 given a sample of 30 and an assumed level of significance of 0.05, with a small effect size (0.25) and three measurement conditions per participant. For experiment two, post hoc analysis revealed power equal to 0.89 given a sample of 10 and an assumed level of significance of 0.05, with a moderate effect size (0.5) and three measurement conditions per participant.
Effect size was calculated to estimate the strength relationship between pairwise comparisons. Given that the data is non-parametric, effect size (r) was estimated from z values by dividing z by the square root of n [17].
Results
Of the 70 swallow video clips (one thin and one puree swallow from 30 adult participants and 10 s segments of sucking from 10 infant participants), one adult study was removed from the data analysis due to suboptimal image quality. The average difference for duration and kinematic measures obtained in the 15 and 5 PPS condition compared to data obtained in the 30 PPS condition are displayed in Figs. 2, 3 and 4. Direction of changes (i.e., did durations get larger or smaller) are displayed for each duration measure in Fig. 5.
Direction of differences (in ms) for 15 and 5 PPS compared to 30 PPS for (a) adults for swallow reaction time, pharyngeal response time, upper esophageal sphincter open duration. and (b) infants for total swallow duration, velopharyngeal closure duration, and upper esophageal sphincter open duration. Note that for each measure and temporal resolution, along the x-axis data are ordered from smallest to highest to easily display the span of differences. The y-axis represents the amount of difference in ms
Impact of Pulse Rate on Duration in Adult Studies
A Friedman test was conducted to determine whether duration measures differed across pulse rates and showed a significant difference (chi square (8) = 187; p < 0.001). Pairwise analyses are presented below to determine the specific duration measures and pairs where statistical differences occurred.
Swallow reaction time (SRT)
On average, measures of swallow reaction time were altered as a function of pulse rate in both thin and puree consistency swallows (Fig. 2). Using a Wilcoxon signed rank test for both IDDSI-1 and IDDSI-4 boluses, SRT was statistically different across pulse rates for both thin and pureed consistency in three of the four pairwise comparisons (IDDSI-1: z = 2.4, p = 0.02, r = 0.5, for 15 PPS compared to 30, and z = 1.3, p = 0.19, and r = 0.3 for 5 PPS compared to 30; IDDSI-4: z = 2.5, p = 0.01, r = 0.5 for 15 PPS compared to 30, and z = 2.8, p < 0.01, r = 0.5 for 5 PPS compared to 30). Figure 5 shows an increased distance from the 30 PPS measure (reflected as the zero line in Fig. 5) with decreased pulse rate. This occurred in both the negative (shorter reaction time measured) and positive (longer reaction time measured) directions.
Guided by normative data from Steele et al. [13], we assessed the impact of pulse rate on clinical classification. Across the 29 thin liquid adult video clips in the 30 PPS condition, six were within the 95CI and 23 fell outside that window. When the data from the 30 PPS condition is compared to the 15 PPS condition, of the six that were within the 95CI in the 30 PPS condition, five retained their clinical determination (identified as agreement in Fig. 6) and one moved outside the 95CI (identified as change in Fig. 6) (Fig. 6a). In the 5 PPS condition, all six videos that were judged to be within the 95CI during the 30 PPS condition were judged to be outside the 95CI. For the 23 videos that were outside the 95CI in the 30 PPS condition, 20 of the 23 retained that determination in both the 15 and 5 PPS condition. Accuracy of clinical determination was 86% for 15 PPS and 69% for 5 PPS (Table 3).
Agreement of clinical determination across pulse rates for duration measures (peak hyoid position, and upper esophageal sphincter open duration) obtained from adult participants. In” refers to the number of videos that were measured to be within the 95CI in the 30 PPS condition. “Out” refers to the number of videos that were measured to be outside the 95CI in the 30 PPS condition. Each column represents the number of videos that were in agreement with (or changed from) the clinical determination assigned in the 30PPS condition
Pharyngeal response time
PRT was statistically different for thin consistency when comparing 15 to 30 PPS, but not when comparing 5 to 30 PPS, and it was not significantly different for puree consistency (IDDSI-1: z = 2.6, p = 0.01, r = 0.5 for 15 PPS compared to 30, and z = 1.0, p = 0.32, r = 0.2 for 5 PPS compared to 30; IDDSI-4: z = 1.7 and, p = 0.1, r = 0.3 for 15 PPS compared to 30, and z = 1.2, p < 0.23, r = 0.2, for 5 PPS compared to 30).
Across the 29 adult thin liquid swallow video clips in the 30 PPS condition, using the normative data from Steele et al. [13], seven were within the 95CI and 22 fell outside that window. Of the seven that were within the 95CI in the 30 PPS condition, when compared to the results from the 15 PPS condition, four retained their clinical determination and three moved outside the 95CI (Fig. 6b). In the 5 PPS condition all seven videos that were judged to be within the 95CI during the 30PPS condition were judged to be outside the 95CI. For the 22 videos that were outside the 95CI in the 30 FPS/PPS condition, 17 retained that determination in the 15 PPS condition and all 22 retained that determination in the 5 PPS condition. Using contingency data to assess accuracy, the 15 PPS condition had an accuracy rate of 72%; the 5 PPS condition had an accuracy rate of 76% (Table 3).
UES open duration
UESOD is statistically different when comparing 30 PPS to 5 PPS for thin consistency only (IDDSI-1: z = 0.2, p = 0.9 a, r < 0.1 for 15 PPS compared to 30, and z = 2.0, p = 0.04, r = 0.4, for 5 PPS compared to 30; IDDSI-4: z = 0.1, p = 0.9, r < 0.1 for 15 PPS compared to 30 and z = 1.0, p = 0.3, r = 0.2, for 5 PPS compared to 30). All other pairwise comparisons were insignificant.
Across the 29 adult thin liquid video clips in the 30 PPS condition, using the normative data from Steele et al. [13], six were within 95CI and 23 fell outside that window. Of the six that were within the 95CI in the 30 PPS condition, when compared to measures obtained in the 15 PPS condition, four retained their clinical determination and two moved outside the 95CI (Fig. 6c). In the 5 PPS condition, all six videos that were judged to be within the 95CI during the 30 PPS condition, were judged to be outside the 95CI. For the 23 videos that were outside the 95CI in the 30 PPS condition, 21 retained that determination in both the 15 PPS condition and 5 PPS condition. Using contingency data to assess accuracy, the 15 PPS condition had an accuracy rate of 79%; the 5 PPS condition had an accuracy rate of 76% (Table 3).
Impact of Pulse Rate on Duration in Infant Studies
Three duration measures were evaluated in 10 infants and included TSD, velopharyngeal closure VPCD, and UESOD. Using a Friedman test for repeated measures of nonparametric data, duration measures in infants did not differ statistically (TSD: chi-square (2) = 4.6, p = 0.1; VPCD: chi-square (2) = 1.5, p = 0.5; UESOD: chi-square (2) = 0.7, p = 0.7). However, the average difference in duration measures increased as pulse rate decreased (Fig. 4). Figure 5b shows that across all duration measures, direction of change was inconsistent (i.e., sometimes the duration was shorter and sometimes the duration was longer).
To assess if the duration data obtained from our infant participants compared favorably to other data sets, Table 4 displays the average duration data obtained from previous investigations. These are compared to the average duration data obtained in this investigation in the 30 PPS condition. Overall, the data obtained in this investigation compares well for VPCD, but not for TSD and UESOD.
Impact of Pulse Rate on Kinematic Measures in Adults
A Friedman test was conducted to determine whether kinematic measures differed across pulse rates. The results showed a significant difference (chi square (5) = 220; p < 0.001). Pairwise analyses are presented below to determine the specific pairs where statistical differences occurred.
Peak hyoid position Differences in measurements of PHP increased as pulse rate decreased (Fig. 3). PHP was statistically different when comparing 30 PPS to 15 PPS and 30 to 5 PPS across both consistencies (IDDSI–1: z = 2.3, p = 0.02, r = 0.4 for 15 PPS compared to 30 PPS, and z = 2.9, p = 0.004, r = 0.5 for 5 PPS compared to 30 PPS; IDDSI-4: z = 2.2, p = 0.03, r = 0.4 for 15 PPS compared to 30 PPS, and z = 3.0, p = 0.003, r = 0.6 for 5 PPS compared to 30 PPS).
Using norms from Steele et al. [13], in the 30 PPS condition, five videos were measured to be within the 95CI; 24 were outside the 95CI range. When comparing this clinical determination to measures from 15 PPS, of the five that were within the 95CI in the 30 PPS condition, three maintained that clinical determination (Fig. 7a). In the 5 PPS condition four retained the clinical determination that they received in the 30 PPS condition. For the 24 that were outside the 95CI in the 30 frame condition, all retained that clinical determination in both lower frame conditions. Accuracy of clinical determination was 93% for 15 PPS and 97% for 5 PPS (Table 3).
Agreement of clinical determination across pulse rates for kinematic measures (peak hyoid position, and extent of upper esophageal sphincter opening) obtained from adult participants.“In” refers to the number of videos that were measured to be within the 95CI in the 30 PPS condition. “Out” refers to the number of videos that were measured to be outside the 95CI in the 30 PPS condition. Each column represents the number of videos that were in agreement with (or changed from) the clinical determination assigned in the 30PPS condition
Extent of UES opening There is an increased difference in the UESOE measures as pulse rate decreased (Fig. 3). UESOE was statistically different when comparing 30 PPS to 15 PPS in puree but not thin consistency (IDDSI-1: z = 1.1, p = 0.2, r = 0.2; IDDSI-4: z = 3.2, p = 0.002, r = 0.6). UESOE was statistically different when comparing 30 PPS to 5 PPS across consistency (IDDSI-1: z = 3.6, p < 0.001, r = 0.7; IDDSI-4: z = 4.3, p < 0.001, r = 0.8).
Using norms from Steele et al. [13], in the 30 PPS condition, 13 were measured as within the 95CI; 16 were outside the 95CI range. When comparing this clinical determination from the 30 PPS condition to those obtained from measures in the 15 PPS condition, of the 13 that were within the 95CI, 12 maintained that clinical determination (Fig. 7b). In the 5 PPS condition 11 of the 13 retained the clinical determination of within 95CI. For the 16 that were outside the 95CI in the 30 PPS condition, 15 retained that clinical determination in both the 15 and 5 pulse conditions. Using contingency data to assess accuracy, the 15 PPS rate condition had an accuracy rate of 93%; the 5 PPS condition had an accuracy rate of 89% (Table 3).
Discussion
The purpose of this investigation was to assess the impact of temporal resolution on measures of swallow events and swallow related oropharyngeal movements in infants and adults. More importantly, we evaluated the impact that temporal resolution had on clinical determination of a given measure.
Duration Measures
The difference in duration measures increased as pulse rate decreased. Notably, for adults in addition to increased measurement differences with lower pulse rates, where normative values were available, lower pulse rates resulted in a shift in clinical interpretation. This impacted individuals who were within normal limits in the 30 PPS condition more than it did those that were categorized as disordered. In fact, across all three duration measures, all adult participants whose duration data were within normal limits in the 30 PPS condition were measured as outside normal limits in the 5 PPS condition. This level of analysis was not possible for the infant participants given that infant normative databases for swallow durations are not available. Also, even if duration measures are unaffected by pulse rate in infant studies, it does not mean that safety and efficiency are also statistically unaltered across pulse rates.
The difference in swallow reaction time that we observed in this investigation links well to previous data comparing MBSImP ratings across two pulse rates—30 and 15 [10]. Bonilha and colleagues noted that initiation of the pharyngeal swallow, which is akin to swallow reaction time, was more vulnerable to reductions in pulse rate than other MBSImP components. They reported that 80% of the swallows with changes in the initiation of pharyngeal swallow were perceived to have worse, or slower, pharyngeal initiation at 15 PPS than 30 PPS. In contrast, Mulheren et al. [11] found a trend for swallowing events, including pharyngeal transit time and initiation of pharyngeal swallow, to be generally perceived as faster at 15 PPS than 30 PPS across boluses.
Measures of duration are less sensitive to reductions in pulse rate in infants when compared to adults. While these data show that duration measures from infant swallow studies may not be sensitive to changes in pulse rate, caution is warranted in broad interpretation. That is, given the small number of infant participants, and the fact that duration is only one aspect of swallow physiology, the lack of statistical difference as a function of pulse rate does not imply that lower pulse rates are acceptable for interpretation of infant swallow studies. Indeed, further evaluation is warranted to address this issue.
If we consider variation across individuals, our data adds light to the inconsistencies reported in these previous investigations with smaller n values. Recall that differences were noted between 30 PPS and the lower pulse rates; however, the direction of the difference (i.e., longer or shorter in duration) was highly variable. With lower pulse rates some participants were viewed as more disordered and some were viewed as less impaired. In fact, for thin liquid swallows, clinical determination changed for four participants in the 15 PPS condition. Of those four, two were measured as better and two were measured as worse. This increased to nine participants in the 5 PPS condition. Of these nine, eight were measured as worse and one was measured as better. The bottom line, however, is clear. The further we stray from a 30 PPS data acquisition standard, the less likely we are to have adequate resolution for accurate clinical interpretation, and the fact that the directionality of the difference is unpredictable makes it impossible to offer a mathematical correction when lower pulse rates are used. Either way, if someone is misdiagnosed as having a more severe swallow deficit or a less severe swallow deficit, there are clinical implications. The clinical implication of perceived longer duration of SRT is that a speech-language pathologist (SLP) may make inaccurate conclusions and provide unnecessary or incorrect treatment. An incorrect shorter measurement means that an oropharyngeal dysfunction may be missed and an individual with swallow deficits may not receive treatment. Our findings indicate that the accuracy of duration is lost with reductions in temporal resolution and is not systematic (i.e., may consistently yield longer or shorter interpretations of durations). When shorter durations are noted, the clinician may fail to implement treatment when necessary, putting the individual at heightened risk for aspiration and its associated sequelae [20].
Kinematic Measures
Kinematic measures allow us to assess movement of structures during the swallow. Broadly speaking, if movement is reduced, there may be inadequate pressure on the bolus to support safe and efficient bolus transit through the pharynx. In this investigation we measured two kinematic aspects of swallowing–PHP during the swallow and UESOE during bolus passage. In general, more UES distension and hyolaryngeal displacement is typically associated with a safer and more efficient swallow. In this investigation, on average, as pulse rate decreased, the accuracy of kinematic measures was reduced. This may impact our judgement of swallow efficiency. If a clinician observes minimal hyolaryngeal displacement during the swallow, their concern for the swallow’s safety would likely increase as the airway entrance may not be adequately deflected away from bolus flow. If poor hyolaryngeal trajectory is combined with poor laryngeal vestibule closure, there is additional concern for swallow safety.
If UESOE is inaccurately measured as more inadequate than it actually is, there may be concern regarding the efficiency of bolus passage through the UES. This concern becomes particularly relevant when assessing it in conjunction with pharyngeal residue. In such cases, the SLP may be misled into overestimating the impact of reduced UES opening on swallow inefficiencies. Consequently, they may underestimate the influence of other physiologic events that are contributing to the inefficiency.
Like duration measures, the impact of temporal resolution was not predictably systematic. Thus, this may result in an altered treatment duration and unnecessary sacrifices of the patient’s quality of life when receiving unnecessary treatment or not receiving necessary treatment.
Limitations
The goal of this study was to assess the impact of lower temporal resolutions (achieved by reducing pulse rate) during data acquisition on the clinical analysis across a group with varied levels of swallowing disorders. This was done by varying participants by diet type. In the contingency analysis we noted that those that were measured as within normal limits were more susceptible to change in clinical determination when lower pulse rates were employed. With a larger number of participants in each of the severity ranks we may better understand the direction of impact on measures when lower pulse rated are used.
Kinematic analysis was only performed on adult participants limiting the available data for the infant population.
While the study provides insight into the impact of pulse rate on timing and biomechanical aspects of swallowing, the absence of measures related to safety and efficiency limits the comprehensiveness of the findings. This constrains our ability to make wholistic judgements on the impact of reduced pulse rates on assessment of swallow physiology.
Lastly, as there is a lack of consensus for pediatric kinematic normative data, the conclusions regarding impact of framerate compared to published norms should be interpreted with caution.
Conclusions
A VFSS serves as a diagnostic tool to provide specific information on physiology and pathophysiology of swallowing events. Our data show that alterations in pulse acquisition rates impact objective measures used in clinical decision making. Using 30 PPS as a reference, reductions in pulse rate led to alterations in duration and kinematics measures and these differences increased as pulse rate decreased. While there is a tendency for reduced temporal resolution to yield changes in objective measures, there is no predictable pattern that results from reductions in temporal resolution. In the absence of a systematic impact of temporal resolution on the evaluation of swallow physiology, a lower temporal resolution may lead to an inaccurate diagnosis and therefore a misguided treatment plan. Overdiagnosis of swallow deficits can lead to unnecessary treatment, which will waste an individual’s finances, time, and peace of mind. Alternatively, if a clinician fails to recognize an existing deficit, the patient is at risk of untreated physiological problems which may sacrifice their health. While these data are sufficient to question reductions in frame rate or pulse rate, duration and kinematic measures are not the sole variables to access patient swallow function. Some consideration should be given to safety and efficiency measures.
Data Availability
Raw data are available from the DysphagiaBank which is stored in the TalkBank repository and located at https://aphasia.talkbank.org/access/English/Other/Dysphagia/UNM-access/UNM.html.
References
Steele CM. The blind scientists and the elephant of swallowing: a review of instrumental perspectives on swallowing physiology. J Texture Stud. 2015;46(3):122–37. https://doi.org/10.1111/jtxs.12101.
Martin-Harris B, Canon CL, Bonilha HS, Murray J, Davidson K, Lefton-Greif MA. Best practices in modified barium swallow studies. Am J Speech Lang Pathol. 2020;29(2S):1078–93. https://doi.org/10.1044/2020_AJSLP-19-00189.
Tibbets J, Palmer PM. A survey of New Mexico practice patterns in the evaluation of swallowing disorders. Oral presentation: ASHA Annual Convention, San Diego; 2020. (Convention canceled).
Bonilha HS, Martin-Harris B, O’Rourke AK, Tipnis SV. Radiation exposure in modified barium swallow studies. Curr Opin Otolaryngol Head Neck Surg. 2020;28(6):371–5. https://doi.org/10.1097/MOO.0000000000000665.
Lin EC. Radiation risk from medical imaging. Mayo Clinic Proceedings. 2010;85(12):1142–1146. https://doi.org/10.4065/mcp.2010.0260.
Bonilha HS, Wilmskoetter J, Tipnis S, Horn J, Martin-Harris B, Huda W. Relationships between radiation exposure dose, time, and projection in videofluoroscopic swallowing studies. Am J Speech Lang Pathol. 2019;28(3):1053–9. https://doi.org/10.1044/2019_AJSLP-18-0271.
Cohen MD. Can we use pulsed fluoroscopy to decrease the radiation dose during video fluoroscopic feeding studies in children? Clin Radiol. 2009;64(1):70–3. https://doi.org/10.1016/j.crad.2008.07.011.
Layly J, Marmouset F, Chassagnon G, et al. Can we reduce Frame Rate to 15 images per Second in Pediatric Videofluoroscopic Swallow studies? Dysphagia. 2020;35(2):296–300. https://doi.org/10.1007/s00455-019-10027-8.
Strauss KJ, Kaste SC. The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients—a white paper executive summary. Pediatr Radiol. 2006;36(S2):110. https://doi.org/10.1007/s00247-006-0184-4.
Bonilha HS, Blair J, Carnes B, et al. Preliminary investigation of the effect of pulse rate on judgments of swallowing impairment and treatment recommendations. Dysphagia. 2013;28(4):528–38. https://doi.org/10.1007/s00455-013-9463-z.
Mulheren RW, Azola A, González-Fernández M. Do ratings of swallowing function differ by videofluoroscopic rate? An exploratory analysis in patients after acute stroke. Arch Phys Med Rehabil. 2019;100(6):1085–90. https://doi.org/10.1016/j.apmr.2018.10.015.
Schindelin J, Arganda-Carreras I, Frise E, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9(7):676–82. https://doi.org/10.1038/nmeth.2019.
Steele CM, Peladeau-Pigeon M, Barbon CAE, et al. Reference values for healthy swallowing across the range from thin to extremely thick liquids. J Speech Lang Hear Res. 2019;62(5):1338–63. https://doi.org/10.1044/2019_JSLHR-S-18-0448.
Palmer PM, Padilla AH, MacWhinney B. The development and implementation of a data repository for swallow studies. Dysphagia 2023, 1–8.
Dharmarathna I, Miles A, Fuller L, Allen J. Quantitative video-fluoroscopic analysis of swallowing in infants. Int J Pediatr Otorhinolaryngol. 2020;138:110315. https://doi.org/10.1016/j.ijporl.2020.110315.
Henderson M, Miles A, Holgate V, Peryman S, Allen J. Application and verification of quantitative objective videofluoroscopic swallowing measures in a pediatric population with dysphagia. J Pediatr. 2016;178:200–e2051. https://doi.org/10.1016/j.jpeds.2016.07.050.
Wuensch KL. Nonparametric effect size estimators. https://core.ecu.edu/wuenschk/docs30/Nonparametric-EffectSize.pdf. Published July 19, 2020. Accessed November 1, 2023.
Weckmueller J, Easterling C, Arvedson J. Preliminary temporal measurement analysis of normal oropharyngeal swallowing in infants and young children. Dysphagia. 2011;26(2):135–43. https://doi.org/10.1007/s00455-010-9283-3.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8. https://doi.org/10.1007/bf00417897.
Palmer PM, Padilla AH. Risk of an adverse event in individuals who aspirate: a review of current literature on host defenses and individual differences. Am J Speech Lang Pathol. 2022;31(1):148–62. https://doi.org/10.1044/2021_AJSLP-20-00375.
Acknowledgements
The authors wish to acknowledge TIMS for their donation of viewing software and to all the individuals whose assessments were used in this project, Brian MacWhinney PhD and the team at TalkBank for allowing us to develop and store a repository database to support research like this, Philip Dale PhD for his advice throughout this project, Camella Rosenberg for her statistics consults, and to the students in the UNM Swallow Disorders Research Lab for their guidance, time, and assistance throughout this endeavor.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors contributed to data collection and analysis. The first draft of the manuscript was written by [Phyllis Palmer] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
No animals were used in this study. Human data involved retrospective data that was collected for clinical purposes. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was waived.
Conflict of Interest
Author A declares that she has no conflicts. Author B declared that he has no conflicts. Author C declares that she has no conflicts. Author D declares that she has no conflicts. Author E declares that she has no conflicts. Author F declares that she has no conflicts.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palmer, P.M., Padilla, A.H., Murray, S.C. et al. The Impact of Videofluoroscopic Pulse Rate on Duration and Kinematic Measures in Infants and Adults with Feeding and Swallowing Disorders. Dysphagia (2024). https://doi.org/10.1007/s00455-024-10709-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00455-024-10709-y