Abstract
The majority of patients with Parkinson’s disease (PD) develop swallowing, speech, and voice (SSV) disorders. Importantly, swallowing difficulty or dysphagia and related aspiration are life-threatening conditions for PD patients. Although PD treatments have significant therapeutic effects on limb motor function, their effects on SSV disorders are less impressive. A large gap in our knowledge is that the mechanisms of SSV disorders in PD are poorly understood. PD was long considered to be a central nervous system disorder caused by the death of dopaminergic neurons in the basal ganglia. Aggregates of phosphorylated α-synuclein (PAS) underlie PD pathology. SSV disorders were thought to be caused by the same dopaminergic problem as those causing impaired limb movement; however, there is little evidence to support this. The pharynx, larynx, and tongue play a critical role in performing upper airway (UA) motor tasks and their dysfunction results in disordered SSV. This review aims to provide an overview on the neuromuscular organization patterns, functions of the UA structures, clinical features of SSV disorders, and gaps in knowledge regarding the pathophysiology underlying SSV disorders in PD, and evidence supporting the hypothesis that SSV disorders in PD could be associated, at least in part, with PAS damage to the peripheral nervous system controlling the UA structures. Determining the presence and distribution of PAS lesions in the pharynx, larynx, and tongue will facilitate the identification of peripheral therapeutic targets and set a foundation for the development of new therapies to treat SSV disorders in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a progressing neurodegenerative disorder diagnosed by the presence of classic movement symptoms, including tremor, bradykinesia and muscle rigidity, and postural instability [1, 2]. PD was long considered to be a central nervous system (CNS) disorder caused by the lose of dopaminergic neurons in the basal ganglia. The pathological hallmark of PD is aggregates of phosphorylated α-synuclein (PAS) within the CNS neurons [1, 3]. However, studies have demonstrated that PAS pathology is distributed not only in the CNS but also in the peripheral nervous system (PNS) [4,5,6,7,8,9,10].
At the peripheral level, PAS aggregates have been found mainly in the autonomic pathways. Beach and colleagues [11,12,13,14,15,16,17,18,19,20,21] and others [22,23,24,25,26,27,28,29] performed extensive studies to detect PAS pathology in multiple peripheral organs and tissues, including cervical vagus nerve (X) [11], stomach [11, 22], colon [12, 16, 23, 24], minor salivary and submandibular glands [13, 14, 16,17,18,19, 25], cardiac plexus [20, 26, 27], skin [16, 21, 28, 29], and retina [15]. Biopsy of periperal tissues such as colon, skin, and submandibular glands has been performed to detect PAS pathology and identify histological biomarkers for PD. While a simple and validated biomarker for PD is still lacking, studies by Beach and colleagues [13, 14, 16, 18, 19] showed that submandibular glands in PD had relatively high densities of PAS aggregates and its needle biopsy has the potential for PD diagnosis. However, further work with large trials is needed to assess the efficacy of the peripheral tissue biopsies for a more precise and early diagnosis of PD [30].
More recently, PAS pathology has been also demonstrated in the PD pharynx. Mu and colleagues [31,32,33,34] were the first to investigate autopsied pharynges from subjects with clinically diagnosed and neuropathologically confirmed PD. Specifically, PAS aggregates were identified in the motor [31] and sensory [32] pharyngeal nerves, muscles [33], and mucosa [34]. The authors demonstrated muscle fiber atrophy in the PD pharynx [33], and this has been confirmed by a subsequent independent study [35]. These findings point to the possibility that direct PAS damage to the peripheral motor and sensory nerves innervating the upper airway (UA) structures would contribute, at least in part, to swallowing, speech, and voice (SSV) disorders commonly seen in PD patients. However, it remains unknown if the PNS controlling the larynx and tongue as well as other surrounding structures is affected by the PAS pathology. Further studies are needed to determine the presence and distribution of PAS pathology in the aerodigestive/vocal tract for better understanding the mechanisms of SSV disorders and for the development of novel therapies to treat impaired SSV in PD.
SSV Disorders in PD
SSV deficits in PD represent a large clinical challenge. Up to 90% of patients with PD develop SSV disorders, including dysphagia, dysarthria, and dysphonia. Dysphagia affects 50–80% of PD patients and 25–50% of PD patients experience aspiration [36,37,38,39,40]. Oropharyngeal dysphagia can be particularly devastating, as it can result in life-threatening conditions such as choking, aspiration pneumonia, and death [41,42,43,44,45]. It has been estimated that up to 70% of patients with PD die from aspiration pneumonia [46, 47].
It is generally believed that SSV disorders are caused by the same dopaminergic problem as that causing impaired limb movements (i.e., bradykinesia and rigidity) [38, 48]. However, there is no correlation between overall muscle rigidity score and dysphagia [48, 49]. Although currently available PD treatments have significant therapeutic effects on limb motor functions, their effects on SSV disorders are disappointing [36, 37, 50,51,52,53,54]. Therefore, some researchers postulated that SSV disorders may be not caused solely by a reduction in basal ganglia dopamine activity [50, 55, 56]. Despite the high incidence of SSV disorders in PD, their pathophysiological mechanisms are poorly understood. This gap in our understanding is a significant barrier to developing effective therapies for the treatment of SSV disorders.
Pharynx, larynx, and tongue play a vital role in swallowing, airway protection, phonation, speech, and respiration. These functions are frequently impaired in PD. In this review, advanced knowledge regarding the specialized neuromuscular organization patterns and functions of the UA structures as well as clinical features of the disordered SSV in PD are presented below for better understanding the mechanisms of SSV disorders and for further detecting PAS pathology and developing new therapies targeting the UA structures.
The Pharynx
The pharynx is a tube-like structure located between oral cavity and esophagus and serves as an aerodigestive/vocal tract. The pharyngeal walls are formed by three segmentally arranged superior, middle, and inferior pharyngeal constrictor (SPC, MPC, and IPC) muscles as well as the paired stylopharyngeus, salpingopharyngeus, and palatopharyngeus muscles. During swallowing, contraction of the pharyngeal constrictors (PCs) constricts the pharyngeal lumen to drive a bolus downward to the esophagus [57]. During respiration, PCs activate to stiffen the pharyngeal walls, thus avoiding pharyngeal collapse and maintaining airway patency [58]. During speech, the muscular pharyngeal walls also activate to shape the vocal tract [59].
The pharynx receives its motor innervation from the pharyngeal branches of the glossopharyngeal (IX) and vagus (X) nerves, which form the so-called pharyngeal plexus (Fig. 1A). In humans, the X nerve provides motor innervation to all the PCs [60, 61]. While it is generally described that the IX nerve only innervates the stylopharyngeus muscle [60], our studies using Sihler’s stain, a whole-mount nerve staining technique, and Karnovsky-Roots acetylcholinesterase (AChE) stain showed that IX also provides motor branches to innervate the inner layer of the PCs [61]. The IX, X, and internal superior laryngeal nerve (ISLN) provide sensory nerve supply to the pharyngeal mucosa [60, 62, 63] and play a crucial role in many UA reflexes. The areas with dense sensory nerve terminals include lateral and posterior pharyngeal walls innervated by the IX and X nerves [62, 63]. These densely innervated areas are consistent with the well-known areas that initiate pharyngeal swallowing [57, 64].
(A) Photograph of a human semipharynx processed with Sihler’s stain, a whole-mount nerve staining technique, showing the pharyngeal plexus formed by the pharyngeal branches of the X and IX nerves innervating the superior, middle and inferior pharyngeal constrictor (i.e., SPC, MPC and IPC) and cricopharyngeus (CP) muscles. 1, pharyngeal branch of the X nerve (Ph-X); 2, pharyngeal branch of the IX nerve (Ph-IX); IX-L, lingual branch of the IX nerve; ESLN, external superior laryngeal nerve; ISLN, internal superior laryngeal nerve; UE, upper esophagus. (B-C) Photomicrographs of longitudinal sections of a cervical X nerve trunk (B) and Ph-X (C) from a PD subject with dysphagia. The sections were immunostained for PAS. Note that there are numerous PAS-immunoreactive axons (darkly stained threads and dots) in both the nerve X and Ph-X. (D) A cross-section of IPC muscle from a PD subject with dysphagia stained with monoclonal antibody NOQ7-5-4D specific for type I myofibers (dark staining). Note that there are numerous small atrophied myofibers in the IPC muscle. Original magnification: (B-D) 200x
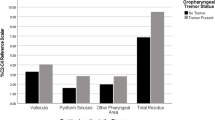
In PD pharynx, we demonstrated for the first time that there were PAS lesions in the sensory and motor nerves and their innervating targets [31,32,33,34] (Fig. 1B-D). Sensory nerve degeneration induced by PAS lesions could impair swallowing initiation. Motor nerve degeneration results in muscle denervation, fiber atrophy, fiber type grouping, and fast-to-slow myosin heavy chain transformation [33, 61]. All these PD-induced neuromuscular alterations could affect muscle contractile properties. Notably, the density of PAS lesions is greater in PD patients with dysphagia versus those without dysphagia [31,32,33,34]. These findings indicate that oropharyngeal dysphagia in PD is related to the extent of the PAS lesions in the pharyngeal sensory and motor nerves and their innervating mucosa and muscles.
The Larynx
The larynx is an important organ for voice production, airway protection, respiration, and swallowing. The performance of these functions relies largely on normal sensory imputs and normal vocal fold movements controlled by five intrinsic laryngeal muscles, including thyroarytenoid (TA), posterior cricoarytenoid (PCA), lateral cricoarytenoid (LCA), interarytenoid (IA), and cricothyroid (CT) muscles innervated by the laryngeal nerves (Fig. 2A and B). The laryngeal muscles are functionally divided into three groups: adductors (i.e., TA, LCA, and IA), abductor (i.e., PCA), and tensor (i.e., CT) of the vocal fold. Adductor and abductor muscles are innervated by the recurrent laryngeal nerve (RLN), whereas the tensor CT muscle receives its motor innervation from external superior laryngeal nerve (ESLN) [60]. Sanders and colleagues [65,66,67,68] investigated the innervation of the human larynx in detail by using Sihler’s stain and provided a number of new findings. In brief, almost all of the intrinsic laryngeal muscles are composed of neuromuscular compartments, each of which is innervated by a distinct nerve branch. In addition, multiple communicating nerves between RLN, ESLN, and ISLN have been identified. These findings are important for better understanding laryngeal functions and motor dysfunction caused by a number of neurological diseases, including PD. Sensory innervation of the mucosa overlaying the larynx and laryngopharynx is from the ISLN and sensory fibers in the RLN [60, 62, 63]. Sihler’s stain showed that the mucosa covering the laryngeal surface of epiglottis innervated by the superior branch of the ISLN and arytenoid and postcricoid regions innervated by the inferior branch of the ISLN has high density of sensory nerve terminals (Fig. 2C and D) [62, 63]. These areas have abundant receptors that elecite swallowing and reflex glottic closure [69,70,71].
(A) Schematic, showing the human larynx (lateral view) and its innervating nerves. (B) Schematic, showing locations of the intrinsic laryngeal muscles (lateroposterior view). Note that cervical X nerve gives off superior laryngeal nerve (SLN) and recurrent laryngeal nerve (RLN). SLN further divides into its internal (ISLN) and external (ESLN) branches to supply the mucosa and cricothyroid (CT) muscle, respectively. The RLN innervates the remaining muscles (i.e., posterior cricoarytenoid, PCA; thyroarytenoid, TA; lateral cricoarytenoid, LCA; and interarytenoid, IA). E, epiglottis; H, hyoid bone; TC, thyroid cartilage. (C-D) Sihler’s stained human laryngeal mucosa showing the branching and distribution patterns of the ISLN and sensory nerve terminals in the mucosa overlaying the laryngeal surface of the epiglottis (C) and postcricoid region (D) (Printed with permission from Fig. 4 in the article by Mu and Sanders [63]). Note that both areas are innervated by dense sensory plexus
During swallowing, the larynx is closed to protect the airway by adduction of the true vocal folds, approximation of the false vocal folds, and approximation of the arytenoids to the base of the epiglottis and epiglottic inversion [72]. Laryngeal motor system is frequently affected in PD as indicated by a number of abnormalities observed in the PD larynx. For instance, laryngeal examinations have revealed that more than 90% of PD patients have incomplete, delayed or totally absent reflex glottic closure during swallowing [55, 73], and vocal fold bowing (VFB) with a glottic gap [74,75,76,77,78,79]. This gap between the vocal folds leads to a loss of air and reduced voice intensity during phonation, thereby leading to a characteristic breathy voice, and possibly aspiration during swallowing. The vocal fold atrophy and bowing could be related to aspiration. However, the cause of VFB has not been determined. These clinical observations suggest that the laryngeal motor nerves are most likely affected in PD. Laryngeal motor dysfunction could result in impaired vocal fold movements, vocal fold atrophy and bowing, and incomplete glottic closure.
Laryngeal sensory nerve dysfunction also results in dysphagia and aspiration. As ISLN innervates the mucosa of the larynx and the laryngopharynx, it plays a critical role in airway protection [71, 80]. Stimulation of the ISLN or laryngeal receptors in the mucosa readily elicits reflex swallowing [57, 81], laryngeal closure [82,83,84,85], and coughing [86,87,88,89]. Dysphagia, aspiration, and reduced laryngeal cough reflex are commonly seen after nerve transection or complete anesthesia of the ISLN [80, 90,91,92]. PD patients with dysphagia and aspiration have decreased cough sensitivity [93,94,95]. Loss of laryngeal sensation as indicated by the absence of cough upon aspiration is a risk factor for aspiration pneumonia [96].
Sensory dysfunction of the larynx and laryngopharynx in PD patients has been demonstrated by using sensory testing. In the 1990s, Aviv and colleagues [97,98,99] developed a new technique for sensory testing using a modified endoscope, known as fiberoptic endoscopic evaluation of swallowing with sensory testing. Laryngopharyngeal sensitivity can be determined by endoscopically delivering air pulse stimuli to the mucosa innervated by the ISLN. Studies have demonstrated that PD patients with dysphagia have decreased laryngopharyngeal sensitivity [100,101,102,103,104]. Approximately 75% of the people with dysphagia have severe laryngopharyngeal sensory deficits and patients with sensory deficits often have laryngeal penetration and aspiration [99].
Clearly, motor and/or sensory dysfunction of the larynx could result in dysphonia, dysphagia, aspiration, and aspiration pneumonia. Motor nerve lesions are associated with vocal fold atrophy and bowing and impaired vocal fold movement, whereas sensory nerve pathology could diminish laryngeal sensation that impairs swallowing, glottic closure, and cough reflexes. All of these changes could affect swallowing and laryngeal protective mechanisms. However, it remains unknown if the laryngeal nervous systems are affected by PAS pathology in PD. Further studies are needed to determine the presence and distribution of the PAS pathology in the PD larynx.
The Tongue
The tongue is a muscular organ located on the floor of the oral cavity. The tongue muscles include extrinsic and intrinsic. Extrinsic muscles, including genioglossus (GG), styloglossus (SG), and hyoglossus (HG), have one attachment to a bone outside the tongue while the other end inserts into the tongue body. Intrinsic muscles, including superior longitudinalis (SL), inferior longitudinalis (IL), transversus (T) and verticalis (V), originate and insert within the tongue body without bony attachments (Fig. 3A).
(A) Schematic, showing the human tongue and its anatomical correlations with the larynx and pharynx as well as other structures. CP, cricopharyngeus; CT, cricothyroid; GG, genioglossus; HG, hyoglossus; IL, inferior longitudinal; IPC, inferior pharyngeal constrictor; M, mandible; MPC, middle pharyngeal constrictor; SG, styloglossus; SPC, superior pharyngeal constrictor; TC, thyroid cartilage; TH, thyrohyoid; UE, upper esophagus. (B) Photograph of a human tongue processed with Sihler’s stain, showing branching and distribution patterns of the nerves to the tongue (Printed with permission from Fig. 1A in the article by Mu and Sanders [108]). Note that the XII nerve is divided into lateral (green circle) and medial (purple circle) divisions at the posterior tongue to supply the tongue muscles. The lingual branch of the IX nerve (IX-L) gives off multiple secondary branches to supply the mucosa overlaying the posterior one-third of the tongue and vallate papillae (black dots). Lingual nerve (LN) splits off a bundle of branches to supply the mucosa covering the anterior two-thirds of the tongue. There are a number of communicating branches between LN and XII
The tongue is able to move in all directions and change in shapes for its diverse functions in chewing, swallowing, speech, and respiration. At least five specific tongue movements have been described, including tongue rolling, folding, twisting, cloverleaf, and a pointing tongue [105, 106]. These tongue movements and shape changes are accomplished by coordinative actions of different tongue muscles. The extrinsic tongue muscles participate primarily in protrusion (GG), retraction (SG + HG), depression (HG + GG), and elevation (SG + PG) of the tongue, as well as side-to-side tongue movement (GG). The intrinsic tongue muscles are involved in tongue-shape changes and movements. For example, contractions of the longitudinal muscles (i.e., SL and IL) shorten, retract, and curl the tip and sides of the tongue (SL for dorsiflexion and IL for ventroflexion of the tip of the tongue). Activation of the T muscle narrows and elongates the tongue, whereas activation of the V muscle flattens, broadens, and elongates the tongue [60, 107]. Therefore, the tongue muscles are generally divided into protrudors (i.e., GG, T and V) and retractors (i.e., SG, HG, SL and IL). Contractions of the protrudors move the tongue forward, whereas contractions of the retractors pull the tongue backward. In addition to protruding the tongue, the GG is responsible for side-to-side movement of the tongue [60].
Motor control of the human tongue is poorly understood, and considerable controversies and uncertainties concerning its innervation still remain [108]. It is generally described that hypoglossal nerve (XII) innervates all the tongue muscles, except for the PG muscle, which is innervated by the pharyngeal branch of the X nerve [60]. The mucosa overlaying the tongue is supplied by lingual nerve (LN) and lingual branch of the IX nerve (IX-L) (Fig. 3B) [60]. Sihler’s stain showed that the XII is divided into a lateral and a medial division that control tongue muscle activities. The lateral XII supplies nerve branches to innervate longitudinally arranged tongue muscles (i.e., SG, HG, SL and lateral IL), whereas the medial XII gives off motor branches to supply GG, T and V, and medial IL muscles. More importantly, Sihler’s stained human tongue specimens demonstrated that the LN supplies not only the mucosa of the tongue, but also the IL and SL muscles. In addition, numerous communicating branches between the LN and XII have been identified [108]. These findings suggest that LN may not be a pure sensory nerve as traditionally described. This hypothesis gains support from studies by Saigusa and colleagues (2006) [109], who demonstrated that some motor fibers from the motor root of the trigeminal nerve enter into and travel within the LN and supply the IL and SL muscles. However, it has never been definitively shown that the LN nerve has motor functions. Therefore, further studies are needed to document if the LN contains motor axons by using anatomical and enzyme-histochemical methods. Detailed information about accurate innervation of the tongue muscles is helpful for a better understanding of the physiology and pathophysiology of the tongue and for future studies on the PD tongue.
Studies have demonstrated that the tongue muscles play an important role in chewing, swallowing, speech, and respiration and that these tongue-related motor tasks are carried out by coordination of extrinsic and intrinsic muscles [110,111,112,113,114,115]. Dysfunction of the tongue has been demonstrated in patients with PD. Videofluoroscopy of swallowing in PD patients shows that the tongue has difficulty forming and controlling the food bolus and that it does not propel the bolus immediately. Instead, it moves the bolus forward and backward repetitively [116]. Slower tongue movements can be associated with hypokinesia related to PD basal ganglia pathology and/or PD-induced peripheral nerve degeneration as seen in the pharyngeal motor and sensory nerves (Fig. 1B and C). PD pathology affects sensorimotor processing, motor control, and muscle weakness that impair tongue movements during chewing, swallowing, and speech. The tongue is the most important articulator of speech. PD patients typically have hypokinetic dysarthria characterized by hypophonia (decreased loudness) and dysprosody (monotony). PD speech, known as hypokinetic dysarthria, affecting about 90% of patients with PD [37, 117, 118], is a particularly disabling problem that influences social interactions and alters daily living activities [119]. Unfortunately, impaired voice, speech, and swallowing are the PD symptoms with a poor response to classical pharmacologic and surgical (deep brain stimulation) PD treatments [for review, see 120, 121]. Therefore, some authors postulated that the mechanism of speech disorders may differ from that of limb motor impairment in PD [for review, see 118].
However, previous studies have yet to directly examine whether the motor and sensory nerves, muscles, and mucosa in the larynx and tongue are affected by PAS pathology in PD. We hypothesize that PAS pathology may affect the larynx and tongue and degeneration of the peripheral nerves controlling the UA could contribute, at least in part, to SSV disorders.
Conclusions and Future Research Directions
This review provides an overview on the neuromuscular organization patterns, functions of the pharynx, larynx, and tongue, clinical features of SSV disorders, and gaps in knowledge regarding the pathophysiology underlying SSV disorders in PD. This information could be helpful for further research on these anatomically complex and functionally important structures to elucidate the pathophysiological mechanisms of disordered SSV in PD.
Although anti-PD treatments, including pharmacologic and deep brain stimulation interventions, have significant therapeutic effects on limb motor functions, their effects on SSV disorders are less impressive or poor [120, 121]. Therefore, a variety of behavioral and rehabilitative interventions such as the Lee Silverman voice treatment (LSVT) [for review, see 122], EMST (expiratory muscle strength training) device [for review, see 123], and others have been used and demonstrated to be beneficial for improving SSV deficits in some, if not all, PD subjects. As the pathophysiological mechanisms underlying disordered SSV in PD are poorly understood, effective treatment for SSV deficits is still lacking. As our prior work demonstrated PAS lesions in the pharyngeal nerves in PD, we hypothesize that PAS-induced peripheral nerve degeneration could contribute, at least in part, to SSV disorders in PD. However, further work is needed to test this hypothesis as described below.
First, although PAS lesions have been identified in PD pharynx [31,32,33,34] (Fig. 1B-D), more studies are needed to determine whether the tongue, larynx, and other UA structures are affected by PAS pathology. Determining the presence and distribution of PAS lesions in the PNS controlling the UA structures will facilitate the identification of peripheral therapeutic targets and set a foundation for the development of new therapies to treat SSV disorders.
Second, further work is needed to determine the relationship between the severity of PAS pathology in the UA structures and SSV severity as indicated by patient’s clinical evaluations including UPDRS ratings (i.e., swallowing score: 0–4; and speech score: 0–4) and/or findings from objective SSV evaluations.
Third, the relative contributions of PNS vs. CNS pathology to SSV disorders in PD need to be determined by investigating how PNS and CNS pathologies correlate with SSV deficits. This may be done by comparing the severity of PNS pathology with the brain PAS severity and staging of brain synuclein presence using the Unified Staging System for Lewy Body Disorders (USSLBD) developed by Beach and colleagues [124]. The reliability and validity of the USSLBD has been confirmed by subsequent independent studies [125, 126]. Such work is necessary for testing our hypothesis as described above.
Finally, neuronal Lewy pathology in the hypoglossal nucleus (HN) and nucleus ambiguus (NA) in PD needs to be examined as HN controls the tongue and NA controls the larynx and pharynx. At present, there is no consensus regarding whether both nuclei are affected by PD pathology. Some authors identified Lewy bodies and Lewy neurites in the NA in subjects with Lewy body dysphagia [127]. However, others found no Lewy pathology in the NA in their PD samples [6, 128, 129]. Therefore, further studies are needed to examine the HN and NA to see if they are affected in PD for better understanding the pathways of the PAS pathology affecting the PNS controlling the UA structures.
Taken together, identification of the PAS lesions in the UA structures and determination of the relationships between SSV deficits and severity of PAS pathology in the PNS vs. CNS are critical for uncovering the pathophysiological mechanisms of disordered SSV in PD. Demonstration of the PAS pathology in the PNS controlling the UA structures may open up a new avenue to develop new therapies to treat SSV disorders in PD. At present, there are candidate anti-synuclein monoclonal antibodies (ASMAs) and drugs that are designed to stop or reverse PAS. For instance, ASMAs have already been in clinical trials [for review, see 130]. However, the therapeutic potential of systemic use of ASMAs or drugs targeting PAS aggregates in the brain may be limited because their high molecular weight cannot cross the blood brain barrier. In contrast, if SSV disorders in PD are caused primarily or partially by PAS pathology in the PNS, intravenous administration or focal injection of these ASMAs and/or drugs would be effective to dissolve PAS lesions in peripheral organs such as the UA structures for treatment of SSV disorders in PD.
Data Availability
The data sources used in this review are publicly available and referenced accordingly in the article. Any additional information or data used in this review can be obtained by contacting the corresponding author.
Abbreviations
- AChE:
-
Acetylcholinesterase
- ASMA:
-
Anti-synuclein monoclonal antibody
- CNS:
-
Central nervous system
- CP:
-
Cricopharyngeus
- CT:
-
Cricothyroid muscle
- ESLN:
-
External superior laryngeal nerve
- GG:
-
Genioglossus
- HG:
-
Hyoglossus
- HN:
-
Hypoglossal nucleus
- IA:
-
Interarytenoid muscle
- IL:
-
Inferior longitudinalis
- IPC:
-
Inferior pharyngeal constrictor
- ISLN:
-
Internal superior laryngeal nerve
- IX:
-
Glossopharyngeal nerve
- IX-L:
-
Lingual branch of the IX nerve
- LCA:
-
Lateral cricoarytenoid muscle
- LN:
-
Lingual nerve
- MPC:
-
Middle pharyngeal constrictor
- NA:
-
Nucleus ambiguous
- PAS:
-
Phosphorylated α-synuclein
- PC:
-
Pharyngeal constrictor
- PCA:
-
Posterior cricoarytenoid muscle
- PD:
-
Parkinson’s disease
- Ph-IX:
-
Pharyngeal branch of the IX nerve
- Ph-X:
-
Pharyngeal branch of the X nerve
- PNS:
-
Peripheral nervous system
- RLN:
-
Recurrent laryngeal nerve
- SG:
-
Styloglossus
- SL:
-
Superior longitudinalis
- SLN:
-
Superior laryngeal nerve
- SPC:
-
Superior pharyngeal constrictor
- SSV:
-
Swallowing,speech and voice
- T:
-
Transversus
- TA:
-
Thyroarytenoid muscle
- UA:
-
Upper airway
- UE:
-
Upper esophagus
- USSLBD:
-
Unified Staging System for Lewy Body Disorders
- V:
-
Verticalis
- VFB:
-
Vocal fold bowing
- X:
-
Vagus nerve
- XII:
-
Hypoglossal nerve
References
Jankovic J. Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79(4):368–76.
Rodriguez-Oroz MC, Jahanshahi M, Krack P, Litvan I, Macias R, Bezard E, Obeso JA. Initial clinical manifestations of Parkinson’s disease: features and pathophysiological mechanisms. Lancet Neurol. 2009;8(12):1128–39.
Samii A, Nutt JG, Ransom BR. Parkinson’s disease. Lancet. 2004;363(9423):1783–93.
Comi C, Magistrelli L, Oggioni GD, Carecchio M, Fleetwood T, Cantello R, Mancini F, Antonini A. Peripheral nervous system involvement in Parkinson’s disease: evidence and controversies. Parkinsonism Relat Disord. 2014;20(12):1329–34.
Ma C, Zhang W, Cao M. Role of the peripheral nervous system in PD pathology, diagnosis, and treatment. Front Neurosci. 2021;15:598457. https://doi.org/10.3389/fnins.2021.598457.
Del Tredici K, Rub U, De Vos RA, Bohl JRE, Braak H. Where does Parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol. 2002;61(5):413–26.
Jellinger KA. Neuropathological spectrum of synucleinopathies. Mov Disord. 2003;18(Suppl 6):2–12.
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K. Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res. 2004;318(1):121–34.
Braak H, Del Tredici K. Invited article: nervous system pathology in sporadic Parkinson disease. Neurology. 2008;70(20):1916–25.
Beach TG, Adler CH, Sue LI, Vedders L, Lue L, White CL 3rd, et al. Multi-organ distribution of phosphorylated alpha-synuclein histopathology in subjects with Lewy body disorders. Acta Neuropathol. 2010;119(6):689–702.
Beach TG, Adler CH, Sue LI, Shill HA, Driver-Dunckley E, Mehta SH, et al. Vagus nerve and stomach synucleinopathy in Parkinson’s disease, incidental Lewy body disease, and normal elderly subjects: evidence against the “body-first” hypothesis. J Parkinsons Dis. 2021;11(4):1833–43.
Beach TG, Corbillé AG, Letournel F, Kordower JH, Kremer T, Munoz DG, et al. Multicenter assessment of immunohistochemical methods for pathological alpha-synuclein in sigmoid colon of autopsied Parkinson’s disease and control subjects. J Parkinsons Dis. 2016;6(4):761–70.
Beach TG, Adler CH, Dugger BN, Serrano G, Hidalgo J, Henry-Watson J, et al. Submandibular gland biopsy for the diagnosis of Parkinson disease. J Neuropathol Exp Neurol. 2013;72(2):130–6.
Beach TG, Adler CH, Serrano G, Sue L, Walker DG, Dugger BN, et al. Prevalence of submandibular gland synucleinopathy in Parkinson’s disease, dementia with Lewy bodies and other Lewy body disorders. J Parkinsons Dis. 2016;6(1):153–63.
Beach TG, Carew J, Serrano G, Adler CH, Shill HA, Sue LI, et al. Phosphorylated α-synuclein-immunoreactive retinal neuronal elements in Parkinson’s disease subjects. Neurosci Lett. 2014;571:34–8.
Chahine LM, Beach TG, Brumm MC, Adler CH, Coffey CS, Mosovsky S, et al. In vivo distribution of α-synuclein in multiple tissues and biofluids in Parkinson disease. Neurology. 2020;95(9):e1267–e84.
Chahine LM, Beach TG, Adler CH, Hepker M, Kanthasamy A, Appel S, et al. Central and peripheral α-synuclein in Parkinson disease detected by seed amplification assay. Ann Clin Transl Neurol. 2023;10(5):696–705.
Adler CH, Dugger BN, Hinni ML, Lott DG, Driver-Dunckley E, Hidalgo J, et al. Submandibular gland needle biopsy for the diagnosis of Parkinson disease. Neurology. 2014;82(10):858–64.
Adler CH, Dugger BN, Hentz JG, Hinni ML, Lott DG, Driver-Dunckley E, et al. Peripheral synucleinopathy in early Parkinson’s disease: submandibular gland needle biopsy findings. Mov Disord. 2016;31(2):250–6.
Serrano GE, Shprecher D, Callan M, Cutler B, Glass M, Zhang N, et al. Cardiac sympathetic denervation and synucleinopathy in Alzheimer’s disease with brain Lewy body disease. Brain Commun. 2020;2(1):fcaa004.
Manne S, Kondru N, Jin H, Serrano GE, Anantharam V, Kanthasamy A, et al. Blinded RT-QuIC analysis of α-synuclein biomarker in skin tissue from Parkinson’s disease patients. Mov Disord. 2020;35(12):2230–9.
Braak H, de Vos RAI, Bohl J, Del Tredici K. Gastric alpha-synuclein immunoreactive inclusions in Meissner’s and Auerbach’s plexuses in cases staged for Parkinson’s disease-related brain pathology. Neurosci Lett. 2006;396(1):67–72.
Wakabayashi K, Takahashi H, Ohama E, Ikuta F. Parkinson’s disease: an immunohistochemical study of Lewy body-containing neurons in the enteric nervous system. Acta Neuropathol. 1990;79(6):581–3.
Lebouvier T, Neunlist M, Bruley des Varannes S, Coron E, Drouard A, N’Guyen JM, et al. Colonic biopsies to assess the neuropathology of Parkinson’s disease and its relationship with symptoms. PLoS ONE. 2010;5(9):e12728.
Cersosimo MG, Perandones C, Micheli FE, Raina GB, Beron AM, Nasswetter G, et al. Alpha-synuclein immunoreactivity in minor salivary gland biopsies of Parkinson’s disease patients. Mov Disord. 2011;26(1):188–90.
Amino T, Orimo S, Itoh Y, Takahashi A, Uchihara T, Mizusawa H. Profound cardiac sympathetic denervation occurs in Parkinson disease. Brain Pathol. 2005;15(1):29–34.
Orimo S, Uchihara T, Nakamura A, Mori F, Kakita A, Wakabayashi K, Takahashi H. Axonal alpha-synuclein aggregates herald centripetal degeneration of cardiac sympathetic nerve in Parkinson’s disease. Brain. 2008;131(Pt 3):642–50.
Dabby R, Djaldetti R, Shahmurov M, Treves TA, Gabai B, Melamed E, Sadeh M, Avinoach I. Skin biopsy for assessment of autonomic denervation in Parkinson’s disease. J Neural Transm (Vienna). 2006;113(9):1169–76.
Miki Y, Tomiyama M, Ueno T, Haga R, Nishijima H, Suzuki C, et al. Clinical availability of skin biopsy in the diagnosis of Parkinson’s disease. Neurosci Lett. 2010;469(3):357–9.
Lee JM, Derkinderen P, Kordower JH, Freeman R, Munoz DG, Kremer T, et al. The search for a peripheral biopsy indicator of α-synuclein pathology for Parkinson Disease. J Neuropathol Exp Neurol. 2017;76(1):2–15.
Mu L, Sobotka S, Chen J, Su H, Sanders I, Adler CH, et al. Alpha-synuclein pathology and axonal degeneration of the peripheral motor nerves innervating pharyngeal muscles in Parkinson’s disease. J Neuropathol Exp Neurol. 2013;72(2):119–29.
Mu L, Sobotka S, Chen J, Su H, Sanders I, Nyirenda T, et al. Parkinson disease affects peripheral sensory nerves in the pharynx. J Neuropathol Exp Neurol. 2013;72(7):614–23.
Mu L, Sobotka S, Chen J, Su H, Sanders I, Adler CH, et al. Altered pharyngeal muscles in Parkinson’s disease. J Neuropathol Exp Neurol. 2012;71(6):520–30.
Mu L, Chen J, Sobotka S, Nyirenda T, Benson B, Gupta F, et al. Alpha-synuclein pathology in sensory nerve terminals of the upper aerodigestive tract of Parkinson’s disease patients. Dysphagia. 2015;30(4):404–17.
Curtis JA, Molfenter SM, Troche MS. Pharyngeal area changes in Parkinson’s disease and its effect on swallowing safety, efficiency, and kinematics. Dysphagia. 2020;35(2):389–98.
Sapir S, Pawlas AA, Ramig LO, et al. Voice and speech abnormalities in Parkinson disease: relation to severity of motor impairment, duration of disease, medication, depression, gender, and age. J Med Speech-Language Pathol. 2001;9:213–26.
Sapir S, Ramig L, Fox C. Voice, speech and swallowing disorders. In: Factor S, Weiner W, editors. Parkinson disease: diagnosis and clinical management. New York: Demos Medical Publishing; 2008. pp. 77–97.
Robbins JA, Logemann JA, Kirshner HS. Swallowing and speech production in Parkinson’s disease. Ann Neurol. 1986;19(3):283–7.
Stroudley J, Walsh M. Radiological assessment of dysphagia in Parkinson’s disease. Br J Radiol. 1991;64(766):890–3.
Bird MR, Woodward MC, Gibson EM, Phyland DJ, Fonda D. Asymptomatic swallowing disorders in elderly patients with Parkinson’s disease: a description of findings on clinical examination and videofluoroscopy in sixteen patients. Age Aging. 1994;23(3):251–4.
Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116(2):455–78.
Gorell JM, Johnson CC, Rybicki BA. Parkinson’s disease and its comorbid disorders: an analysis of Michigan mortality data, 1970 to 1990. Neurology. 1994;44(10):1865–8.
Wermuth L, Stenager EN, Stenager E, Boldsen J. Mortality in patients with Parkinson’s disease. Acta Neurol Scand. 1995;92(1):55–8.
Beyer MK, Herlofson K, Arsland D, Larsen JP. Causes of death in a community-based study of Parkinson’s disease. Acta Neurol Scand. 2001;103(1):7–11.
Fernandez HH, Lapane KL. Predictors of mortality among nursing home residents with a diagnosis of Parkinson’s disease. Med Sci Monit. 2002;8(4):CR241–6.
Mehanna R, Jankovic J. Respiratory problems in neurologic movement disorders. Parkinsonism Relat Disord. 2010;16(10):628–38.
Won JH, Byun SJ, Oh BM, Park SJ, Seo H. Risk and mortality of aspiration pneumonia in Parkinson’s disease: a nationwide database study. Sci Rep. 2021;11:6597.
Hunker CJ, Abbs JH, Barlow SM. The relationship between parkinsonian rigidity and hypokinesia in the orofacial system: a quantitative analysis. Neurology. 1982;32(7):749–54.
Ali GN, Wallace KL, Schwartz R, DeCarle DJ, Zagami AS, Cook IJ. Mechanisms of oral-pharyngeal dysphagia in patients with Parkinson’s disease. Gastroenterology. 1996;110(2):383–92.
Hunter PC, Crameri J, Austin S, Woodward MC, Hughes AJ. Response of parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry. 1997;63(5):579–83.
Duff J, Sime E. Surgical interventions in the treatment of Parkinson’s disease (PD) and essential tremor (ET): medial pallidotomy in PD and chronic deep brain stimulation (DBS) in PD and ET. Axone. 1997;18(4):85–9.
Kompoliti K, Wang QE, Goetz CG, Leurgans S, Raman R. Effects of central dopaminergic stimulation by apomorphine on speech in Parkinson’s disease. Neurology. 2000;54(2):458–62.
Kent RD, Duffy JR, Slama A, Kent JF, Clift A. Clinicoanatomic studies in dysarthria: review, critique, and directions for research. J Speech Lang Hear Res. 2001;44(3):535–51.
Sapir S, Ramig L, Fox C. Speech and swallowing disorders in Parkinson disease. Curr Opin Otolaryngol Head Neck Surg. 2008;16(3):205–10.
Leopold NA, Kagel MC. Pharyngo-esophageal dysphagia in Parkinson’s disease. Dysphagia. 1997;12(1):11–8.
Ertekin C, Tarlaci S, Aydogdu I, Kiylioglu N, Yuceyar N, Turman AB, et al. Electrophysiological evaluation of pharyngeal phase of swallowing in patients with Parkinson’s disease. Mov Disord. 2002;17(5):942–9.
Doty RW. Neural organization of deglutition. In: Code CF, editor. Handbook of physiology. Section 6, Alimentary canal. Volume 4. Washington, D.C.: American Physiological Society; 1968. pp. 1861–902.
Kuna ST, Smickley JS, Vanoye CR. Respiratory-related pharyngeal constrictor muscle activity in normal human adults. Am J Respir Crit Care Med. 1997;155:1991–9.
Minifie FD, Abbs JH, Tarlow A, Kwaterski M. EMG activity within the pharynx during speech production. J Speech Hear Res. 1974;17:497–504.
Standring S, Ellis H, Healy JC, Johnson D, Williams A. Gray’s anatomy. The anatomical basis of clinical practice. 39th ed. New York: Churchill Livingstone; 2005.
Mu L, Sanders I. Neuromuscular specializations within human pharyngeal constrictor muscles. Ann Otol Rhinol Laryngol. 2007;116(8):604–17.
Sanders I, Mu L. Anatomy of the human internal superior laryngeal nerve. Anat Rec. 1998;252(4):646–56.
Mu L, Sanders I. Sensory nerve supply of the human oro- and laryngopharynx: a preliminary study. Anat Rec. 2000;258(4):406–20.
Pommerenk WT. A study of the sensory areas eliciting the swallowing reflex. Am J Physiol. 1928;84:36–41.
Sanders I, Wu BL, Mu L, Li Y, Biller HF. The innervation of the human larynx. Arch Otolaryngol Head Neck Surg. 1993;119(9):934–9.
Sanders I, Wu BL, Mu L, Biller HF. The innervation of the human posterior cricoarytenoid muscle: evidence for at least two neuromuscular compartments. Laryngoscope. 1994;104(7):880–4.
Mu L, Sanders I, Wu BL, Biller HF. The intramuscular innervation of the human interarytenoid muscle. Laryngoscope. 1994;104(1 Pt 1):33–9.
Mu L, Sanders I. The human cricothyroid muscle: three muscle bellies and their innervation patterns. J Voice. 2009;23(1):21–8.
Storey AT. Laryngeal initiation of swallowing. Exp Neurol. 1968;20(3):359–65.
Shingai T, Shimada K. Reflex swallowing elicited by water and chemical substances applied in the oral cavity, pharynx, and larynx of the rabbit. Jpn J Physiol. 1976;26(5):455–69.
Stedman H, Bradley R, Mistretta C, et al. Chemosensitive responses from the cat epiglottis. Chem Senses. 1980;5:233–45.
Kawasaki A, Fukuda H, Shiotani A, Kanzaki J. Study of movements of individual structures of the larynx during swallowing. Auris Nasus Larynx. 2001;28(1):75–84.
Leopold NA, Kagel MC. Laryngeal deglutition movement in Parkinson’s disease. Neurology. 1997;48(2):373–6.
Hanson DG, Gerratt BR, Ward PH. Cinegraphic observations of laryngeal function in Parkinson’s disease. Laryngoscope. 1984;94(3):348–53.
Smith ME, Ramig LO, Dromey C, Perez KS, Samandari R. Intensive voice treatment in Parkinson disease: laryngostroboscopic findings. J Voice. 1995;9(4):453–9.
Perez KS, Ramig LO, Smith ME, Dromey C. The Parkinson larynx: tremor and videostroboscopic findings. J Voice. 1996;10(4):354–61.
Stelzig Y, Hochhaus W, Gall V, Henneberg A. [Laryngeal manifestations in patients with Parkinson disease]. Laryngorhinootologie. 1999;78(10):544–51.
Blumin JH, Pcolinsky DE, Atkins JP. Laryngeal findings in advanced Parkinson’s disease. Ann Otol Rhinol Laryngol. 2004;113(4):253–8.
Sinclair CF, Gurey LE, Brin MF, Stewart C, Blitzer A. Surgical management of airway dysfunction in Parkinson’s disease compared with Parkinson-plus syndromes. Ann Otol Rhinol Laryngol. 2013;122(5):294–8.
Addington WR, Stephens RE, Gilliland K, Miller SP. Tartaric acid-induced cough and the superior laryngeal nerve evoked potential. Am J Phys Med Rehabil. 1998;77(6):523–6.
Doty RW, Bosma JF. An electromyographic analysis of reflex deglutition. J Neurophysiol. 1956;19(1):44–60.
Miller A. The neuroscientific principles of swallowing and dysphagia. San Diego: Singular Publishing Group, Inc.; 1999.
Bradley RM. Sensory receptors of the larynx. Am J Med. 2000;108(Suppl 4a):47S–50S.
Medda BK, Kern M, Ren J, Xie P, Ulualp SO, Lang IM, Shaker R. Relative contribution of various airway protective mechanisms to prevention of aspiration during swallowing. Am J Gastrointest Liver Physiol. 2003;284(6):G933–9.
Shaker R, Ren J, Bardan E, Eastering C, Dua K, Xie P, Kern M. Pharyngoglottal closure reflex: characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology. 2003;49(1):12–20.
Murakami Y, Kirchner JA. Mechanical and physiological properties of reflex laryngeal closure. Ann Otol Rhinol Laryngol. 1972;81(1):59–71.
Nishino T, Tagaito Y, Isono S. Cough and other reflexes on irritation of airway mucosa in man. Pulm Pharmacol. 1996;9(5–6):285–92.
Andreatta RD, Mann EA, Poletto CJ, Ludlow CL. Mucosal afferents mediate laryngeal adductor responses in the cat. J Appl Physiol. 2002;93(5):1622–9.
Meyer TK. The larynx for neurologists. Neurologist. 2009;15(6):313–8.
Addington WR, Stephens RE, Goulding RE. Anesthesia for the superior laryngeal nerves and tartaric acid-induced cough. Arch Phys Med Rehabil. 1999;80(12):1584–6.
Venker-van Haagen AJ, Van den Brom WE, Hellebrekers LJ. Effect of superior laryngeal nerve transection on pharyngeal muscle contraction timing and sequence of activity during eating and stimulation of the nucleus solitarius in dogs. Brain Res Bull. 1999;49(6):393–400.
Jafari S, Prince RA, Kim DY, Paydarfar D. Sensory regulation of swallowing and airway protection: a role for the internal superior laryngeal nerve in humans. J Physiol. 2003;550(Pt 1):287–304.
Luschei ES, Ramig LO, Baker KL, Smith ME. Discharge characteristics of laryngeal single motor units during phonation in young and older adults and in persons with Parkinson disease. J Neurophysiol. 1999;81(5):2131–9.
Merati AL, Heman-Ackah YD, Abaza M, Altman KW, Sulica L, Belamowicz S. Common movement disorders affecting the larynx: a report from the neurolaryngology committee of the AAO-HNS. Otolaryngol Head Neck Surg. 2005;133(5):654–65.
Pitts T, Bolser D, Rosenbek J, Troche M, Sapienza C. Voluntary cough production and swallow dysfunction in Parkinson’s disease. Dysphagia. 2008;23(3):297–301.
Niimi A, Matsumoto H, Ueda T, Takemura M, Suzuki K, Tanaka E, et al. Impaired cough reflex in patients with recurrent pneumonia. Thorax. 2003;58(2):152–3.
Aviv JE, Martin JH, Keen MS, Debell M, Blitzer A. Air pulse quantification of supraglottic and pharyngeal sensation: a new technique. Ann Otol Rhinol Laryngol. 1993;102(10):777–80.
Aviv JE. Sensory discrimination in the larynx and hypopharynx. Otolaryngol Head Neck Surg. 1997;116(3):331–4.
Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B, Close LG. FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol. 1998;107(5 Pt 1):378–87.
Aviv JE, Spitzer J, Cohen M, Ma G, Belafsky P, Close LG. Laryngeal adductor reflex and pharyngeal squeeze as predictors of laryngeal penetration and aspiration. Laryngoscope. 2002;112(2):338–41.
Hammer MJ, Murphy CA, Abrams TM. Airway somatosensory deficits and dysphagia in Parkinson’s disease. J Parkinsons Dis. 2013;3(1):39–44.
Setzen M, Cohen MA, Mattucci KF, Perlman PW, Ditkoff MK. Laryngopharyngeal sensory deficits as a predictor of aspiration. Otolaryngol Head Neck Surg. 2001;124(6):622–4.
Setzen M, Cohen MA, Perlman PW, Belafsky PC, Guss J, Mattucci KF, Ditkoff M. The association between laryngopharyngeal sensory deficits, pharyngeal motor function, and the prevalence of aspiration with thin liquids. Otolaryngol Head Neck Surg. 2003;128(1):99–102.
Hammer MJ, Barlow SM. Laryngeal somatosensory deficits in Parkinson’s disease: implications for speech respiratory and phonatory control. Exp Brain Res. 2010;201(3):401–9.
He X, Zhang JF, Li ZX, Liu C, Yang LT, Wang N, et al. The traits of five types of tongue movement in Han of Shaanxi, China. Anat Sci Int. 2012;87(4):181–6.
Kappert KDR, van Dijk S, Wellenstein D, van Alphen MJA, van Son RJJH, Smeele LE, Balm AJM. Five specific tongue movements in a healthy population. Dysphagia. 2021;36(4):736–42.
Sanders I, Mu L. A three-dimensional atlas of human tongue muscles. Anat Rec (Hoboken). 2013;296(7):1102–14.
Mu L, Sanders I. Human tongue neuroanatomy: nerve supply and motor endplates. Clin Anat. 2010;23(7):777–91.
Saigusa H, Tanuma K, Yamashita K, Saigusa M, Niimi S. Nerve fiber analysis for the lingual nerve of the human adult subjects. Surg Radiol Anat. 2006;28(1):59–65.
Sawczuk A, Mosier KM. Neural control of tongue movement with respect to respiration and swallowing. Crit Rev Oral Biol Med. 2001;12(1):18–37.
Miller AJ. Oral and pharyngeal reflexes in the mammalian nervous system: their diverse range in complexity and the pivotal role of the tongue. Crit Rev Oral Biol Med. 2002;13(5):409–25.
Napadow VJ, Chen Q, Wedeen VJ, Gilbert RJ. Biomechanical basis for lingual muscular deformation during swallowing. Am J Physiol. 1999;277(3):G695–701.
Palmer PM, Jaffe DM, McCulloch TM, Finnegan EM, Van Daele DJ, Luschei ES. Quantitative contributions of the muscles of the tongue, floor-of-mouth, jaw, and velum to tongue-to-palate pressure generation. J Speech Lang Hear Res. 2008;51(4):828–35.
Hiiemae KM, Palmer JB. Tongue movements in feeding and speech. Crit Rev Oral Biol Med. 2003;14(6):413–29.
Bailey EF, Fregosi RF. Coordination of intrinsic and extrinsic tongue muscles during spontaneous breathing in the rat. J Appl Physiol. 2004;96(2):440–9.
Tjaden K. Speech and swallowing in Parkinson’s disease. Top Geriatr Rehabil. 2008;24(2):115–26.
Johnson JA, Pring TR. Speech therapy and Parkinson’s disease: a review and further data. Br J Disord Commun. 1990;25(2):183–94.
Brabenec L, Mekyska J, Galaz Z, Rektorova I. Speech disorders in Parkinson’s disease: early diagnostics and effects of medication and brain stimulation. J Neural Transm (Vienna). 2017;124(3):303–34.
Ma EP, Yiu EM. Voice activity and participation profile: assessing the impact of voice disorder on daily activities. J Speech Lang Hear Res. 2001;44(3):511–24.
Schulz GM, Grant MK. Effects of speech therapy and pharmacologic and surgical treatments on voice and speech in Parkinson’s disease: a review of the literature. J Commun Disord. 2000;33(1):59–88.
Pinto S, Ozsancak C, Tripoliti E, Thobois S, Limousin-Dowsey P, Auzou P. Treatments for dysarthria in Parkinson’s disease. Lancet Neurol. 2004;3(9):547–56.
Pu T, Huang M, Kong X, Wang M, Chen X, Feng X, Wei C, Weng X, Xu F. Lee Silverman voice treatment to improve speech in Parkinson’s disease: a systemic review and meta-analysis. Parkinsons Dis. 2021;3366870. https://doi.org/10.1155/2021/3366870.
Mancopes R, Smaoui S, Steele CM. Effects of expiratory muscle strength training on videofluoroscopic measures of swallowing: a systematic review. AJSLP. 2020;29:335–56.
Beach TG, Adler CH, Lue L, Sue LI, Bachalakuri J, Henry-Watson J, et al. Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropath. 2009;117(6):613–34.
Adler CH, Beach TG, Zhang N, Shill HA, Driver-Dunckley E, Caviness JN, et al. Unified staging system for Lewy body disorders: clinicopathologic correlations and comparison to Braak staging. J Neuropathol Exp Neurol. 2019;78(10):891–9.
Attems J, Toledo JB, Walker L, Gelpi E, Gentleman S, Halliday G, et al. Neuropathological consensus criteria for the evaluation of Lewy pathology in post-mortem brains: a multi-center study. Acta Neuropathol. 2021;141(2):151–72.
Kovari E, Burkhardt K, Lobrinus JA, Bouras C. Lewy body dysphagia. Acta Neuropathol. 2007;114(3):295–8.
Braak H, Rub U, Gai WP, Del Tredici K. Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm (Vienna). 2003;110(5):517–36.
Hawkes CH, Del Tredici K, Braak H. Parkinson’s disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol. 2007;33(6):599–614.
Fields CR, Bengoa-Vergniory N, Wade-Martins R. Targeting alpha-synuclein as a therapy for Parkinson’s disease. Front Mol Neurosci. 2019;12:229.
Acknowledgements
This work was supported by the Department of Defense, Defense Health Program, Congressionally Directed Medical Research Programs (CDMRP), Parkinson’s Research Program under Award No. HT9425-23-1-0481 (to Dr. Liancai Mu). Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. We are grateful to the Banner Sun Health Research Institute Brain and Body Donation Program of Sun City, Arizona for the provision of human biological materials. The Brain and Body Donation Program has been supported by the National Institute of Neurological Disorders and Stroke (U24 NS072026 National Brain and Tissue Resource for Parkinson’s Disease and Related Disorders), the National Institute on Aging (P30AG019610 and P30AG072980, Arizona Alzheimer’s Disease Center), the Arizona Department of Health Services (contract 211002, Arizona Alzheimer’s Research Center), the Arizona Biomedical Research Commission (contracts 4001, 0011, 05-901 and 1001 to the Arizona Parkinson’s Disease Consortium) and the Michael J. Fox Foundation for Parkinson’s Research. The authors thank the anonymous reviewers for their constructive comments on this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mu, L., Chen, J., Li, J. et al. Mechanisms of Swallowing, Speech and Voice Disorders in Parkinson’s Disease: Literature Review with Our First Evidence for the Periperal Nervous System Involvement. Dysphagia (2024). https://doi.org/10.1007/s00455-024-10693-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00455-024-10693-3