Abstract
Patients with Parkinson’s disease (PD) have progressive and pervasive disorders of airway protection. Recent work has highlighted the relationship between reflex and voluntary cough and swallowing safety. The goal of this study was to test the sensitivity and specificity of several airway protective and disease-specific factors for predicting swallowing safety outcomes in PD. Sixty-four participants (44 males) completed measures of voluntary and reflex cough, and swallowing safety. Clinical predictors included disease severity and duration, and cough airflow and sensitivity measures. ROC and Chi-square analyses identified predictors of swallowing safety (penetration–aspiration score) in PD. Disease duration significantly discriminated between patients with normal and abnormal swallowing safety (p = 0.027, sensitivity: 71 %, specificity: 55.4 %). Cough reflex sensitivity significantly discriminated between patients who penetrated above the level of the vocal folds and those with more severe penetration/aspiration (p = 0.021, sensitivity: 71.0 %, specificity 57.6 %). Urge-to-cough sensitivity (log–log linear slope) was the only variable which significantly discriminated between patients with penetration versus aspiration (p = 0.017, sensitivity: 85.7 %, specificity 73.2 %). It is important to identify the factors which influence airway protective outcomes in PD especially given that aspiration pneumonia is a leading cause of death. Results from this study highlight the ecological validity of reflex cough in the study of airway protection and this study further identifies important factors to consider in the screening of airway protective deficits in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aspiration pneumonia is the leading cause of death in Parkinson’s disease (PD) [1–5] and it is becoming increasingly clear that dysphagia, or disordered swallowing, alone cannot explain the pathogenesis of this infection. Instead, it is likely the pervasive and progressive dysfunction of a continuum of airway protective behaviors, including swallowing and cough, that results in the high incidence of aspiration pneumonia. Researchers have identified the cooccurrence of cough dysfunction (dystussia) and dysphagia in people with PD [6–8]. However, it is unclear how the motor and sensory aspects of cough relate to or predict swallowing dysfunction. Further specifying these relationships is essential to enhance the assessment and management approaches we utilize in people with PD who do not adequately protect their airway during swallowing. More importantly, it may assist in the early identification of patients with airway protective deficits; therefore, improving long-term pulmonary outcomes.
Cough is the most important of the multiple airway protective behaviors for ejecting material from the lower airways. It can be produced voluntarily (e.g., on command) or reflexively in response to a stimulus in the airway. Impairment of this clearing mechanism, in conjunction with impaired swallowing, is of significant health concern because this results in uncompensated or undercompensated aspiration. Multiple studies have identified that voluntary and reflex cough may be indicators of swallowing dysfunction (e.g., [6–12]). Yet, it remains unclear whether disease-specific factors, such as disease severity or duration, voluntary cough, or reflex cough measures are most predictive of swallowing dysfunction in PD. Therefore, the aim of this study was to test the sensitivity and specificity of several airway protective and disease-specific factors as predictive measures of swallowing outcomes in PD. It was hypothesized that measures of reflex cough, including sensory perception measures and airflow parameters, would be the most robust indicators of swallowing dysfunction as compared to measures of voluntary cough airflow and disease-specific factors. We hypothesized that reflex cough would be superior in predicting swallowing outcomes given their similarities as airway protective behaviors, each triggered by a salient sensory stimulus in the upper airway and requiring reconfiguration of the ventilator breathing cycle.
Methods
Airway protective outcomes were tested in 64 participants with mild to moderate PD. Participants were tested while on optimal dopaminergic medication. These data were collected over two prospective studies which received ethical approval by the University of Florida Institutional Review Board. Participants were recruited from the University of Florida Center for Movement Disorders and Neurorestoration based on consecutive referral to Speech-Language Pathology over a two-year time period. Fellowship-trained Movement Disorders Neurologists diagnosed PD using the United Kingdom (UK) brain bank criteria and defined disease severity using the Unified Parkinson’s Disease Rating Scale (UPDRS) and the Hoehn and Yahr (H&Y) Scale. Participant demographic information, including disease duration (defined as time since onset of first PD symptoms), is in Table 1. All participants provided written informed consent prior to the initiation of any study procedures.
Criteria for inclusion were: (1) diagnosis of idiopathic PD (either tremor-predominant or rigid-predominant) by a certified movement disorders neurologist; (2) H&Y scale stages I–IV; and (3) between 35 and 85 years of age to allow for a broad sampling of PD duration and severity. Exclusionary criteria were: (1) history of other neurological disorders; (2) history of head, neck, or lung cancer; (3) history of chronic respiratory disorders/diseases; (4) smoking in the last 5 years; (5) uncontrolled hypertension; (6) difficulty complying due to neuropsychological dysfunction; or (7) failure of screening test of pulmonary function (i.e., FEV1/FVC < 75 %).
Cough Evaluation
Participants were seated and outfitted with a facemask covering the nose and mouth. The facemask was coupled to a pneumotachograph, differential pressure transducer, and had a side port with a one-way inspiratory valve for nebulizer connection. The nebulizer was a DeVilbiss T-piece connected to a dosimeter that delivered aerosolized solution during inspiration with a delivery duration of two seconds. Participants completed a single breath capsaicin challenge with three randomized blocks of 0, 50, 100, and 200 μM capsaicin. The capsaicin was dissolved in a vehicle solution consisting of 80 % physiological saline, 20 % ethanol. The maximum concentration of 200 μM was chosen because it has previously been identified as a suprathreshold concentration for eliciting reflex cough in healthy adults [13]. Participants were seated comfortably for an initial 30 s of quiet breathing in order to acclimate to the facemask. Participants were given the instruction “cough if you need to” prior to and during capsaicin delivery. There was a minimum of one minute between each presentation of capsaicin during which participants were provided water. Participants also completed three sequential voluntary cough epochs during which they were cued to “cough as if something went down the wrong tube.” This set of instructions was provided as a natural prompt for the induction of voluntary cough that would generate a similar number of voluntary coughs per cough epoch as reflex coughs per epoch, allowing for comparison between cough types [11, 12, 14]. The cough airflow signal from both reflex and voluntary cough tasks was recorded to a laptop computer via Power Lab Data Acquisition System (ADInstruments).
Swallowing Evaluation
Swallowing was assessed by a certified Speech-Language Pathologist. Participants were positioned in the lateral viewing plane while seated and self-administered a three ounce thin liquid challenge bolus of barium sulfate contrast solution. Images were acquired from a Siemens radiographic/fluoroscopic unit and recorded at 30 frames per second. No instructions regarding manner of swallowing were given to maintain natural swallowing behavior. The selected swallowing outcome measure was the penetration–aspiration scale (PA) [15]. The PA Scale, a valid ordinal measure, was used to quantify the presence of penetration and aspiration during the swallowing of the three ounce bolus. This measure is often used in clinical practice and as an outcome measure in research studies.
Outcome Measures
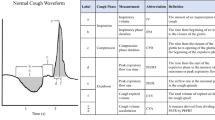
Cough Airflow Measures
Airflow measurements were derived from the reflex and voluntary cough waveforms. Measurements included compression phase duration (CPD), peak expiratory flow rate (PEFR), and peak expiratory flow rise time (PEFRT). Cough volume acceleration (CVA) was computed as PEFR/PEFRT.
Cough Threshold
The total number of coughs was counted from the first cough epoch (defined as the first cough, and all subsequent cough reaccelerations following one inspiration) with each presentation of capsaicin. These measures were made from the recorded cough airflow signals. The concentration of capsaicin that elicited the reliable two-cough response (Cr2) was recorded and identified as the measure of cough threshold. A ‘reliable’ Cr2 was defined as at least two coughs produced within 30 s following presentation of the stimulus, in two of three trials of that concentration.
Urge to Cough (UTC)
Following each capsaicin trial, participants rated their UTC using a modified Borg Rating Scale, where 1 was no UTC, and 10 was maximal UTC. The medians of the UTC ratings were plotted against capsaicin concentration on a log–log scale and a linear regression line was used to fit the data. The slope of the line was used as a measure of UTC sensitivity to capsaicin and was compared between groups.
Disease-Specific Factors
Disease-specific factors were determined from chart review of the associated Neurology visit with the movement disorders fellowship-trained clinician. Age, disease severity, as measured by the UPDRS, and disease duration were identified for each participant. Disease duration was defined as time since the onset of first PD symptoms.
Statistics
Intra- and interrater reliability was completed on 20 % of the measures of cough and PA scale score data. Receiver operator curves (ROC), sensitivity, and specificity measures were completed to quantify how accurate the disease-specific and cough parameters were at discriminating between patients with and without swallowing safety abnormalities. Separate analyses were conducted to compare: (1) participants with normal swallowing from those with abnormal swallowing (PA 1 vs. 2–8), (2) participants with normal to mild changes to those with more severe swallowing safety deficits (PA 1–3 vs. 4–8), and (3) participants with at least penetration to those who aspirated on the swallowing evaluation (PA 3–5 vs. 6–8). The sensitivity and specificity with the optimal cut-off value were derived from the analysis as a measure of validity. ROC curves and the corresponding areas under the curve (AUC) were calculated for continuous variables. Cross tabulation and Chi-Square analysis were used to measure association between the Cr2 response and the different PA groups. All statistical analyses were completed using SPSS IBM Statistics 21.0.
Results
Of the 64 participants with PD who were tested (44 male, 20 female), 25 (39.1 %) penetrated above the level of the vocal folds, 25 (39.1 %) penetrated to the level of the vocal folds, and 7 (10.9 %) aspirated during the three ounce sequential swallowing task. Participants’ average age was 65 years and average disease duration was 8.5 years (Fig. 1). The intra- and intermeasurer ratings for PA score were highly reliable (α = 0.917, p < .001 and α = 0.849, p < .001, respectively). The intra- and intermeasurer ratings for cough values were also reliable (α = 0.89, p = .003 and α = 0.712, p = .008, respectively).
No Penetration or Aspiration Versus Any Degree of Penetration or Aspiration (PA 1 Vs. PA 2–8)
ROC analysis compared outcomes for participants with PA scale score 1 (no penetration/aspiration) versus those with PA scale scores 2–8 (penetration or aspiration). Only disease duration significantly identified patients with no penetration/aspiration versus those in the penetrator/aspirator group [p = 0.035, area under the curve: 0.75, sensitivity: 82.5 %, specificity: 57.1 % for a cut-off of 4.5 years; Fig. 2]. None of the cough airflow variables were significantly predictive for the detection of penetration/aspiration in this model (Table 2).
Receiver operator curve (ROC) analysis for the significant variable disease duration (PA scale score 1 vs. PA scale scores 2–8) and UTC slope (PA scale scores 3–5 vs. PA scale scores 6–8). Disease duration significantly discriminated between patients with PA 1 versus all others (PA 2–8) (p = 0.027, sensitivity 71 %, specificity 55.4 %; (a). UTC sensitivity (log–log linear slope) was the only variable which significantly discriminated between patients with penetration versus aspiration (PA 3–5 vs. PA 6–8) (p = 0.017, sensitivity 85.7 %, specificity 73.2 %; (b)
Normal or Penetration Above the Vocal Folds Versus Penetration to the Level of the Vocal Folds or Below (Aspiration; PA 1–3 Vs. PA 4–8)
Chi-Square test showed a significant association between Cr2 response and the PA groups 1–3 versus 4–8 [p = 0.021]. Further cross tabulation analysis revealed a sensitivity of 70.97 % and a specificity of 57.58 % for the Cr2 response as the measure of cough threshold (Table 3).
Penetration Versus Aspiration (PA 3–5 Vs. PA 6–8)
ROC analysis compared outcomes for participants with PA scale scores 3–5 (penetration) versus PA scale scores 6–8 (aspiration). The reflex cough variable UTC slope was the only variable that significantly distinguished between patients with clinically significant penetration versus those patients who aspirated [p = 0.017, area under the curve: 0.78, sensitivity: 85.7 %, specificity: 73.2 % for a cut-off of 0.113; Fig. 2]. None of the voluntary cough airflow measures significantly discriminated between penetrators and aspirators (Table 2).
Discussion
The current study is the first to prospectively and directly compare the relationship between disease-specific factors such as disease duration and severity, along with both reflex and voluntary cough parameters, with the severity of swallowing dysfunction in patients with PD. It was initially hypothesized that measures of reflex cough would be the most robust indicators of swallowing dysfunction as compared to measures of voluntary cough airflow and disease-specific factors. The study’s results partially supported this hypothesis, with urge-to-cough (UTC) sensitivity being the only factor which significantly distinguished between those with mild dysphagia (penetration group; PA 3–5) and those with severe dysphagia (aspiration group; PA 6–8). Additionally, cough threshold (Cr2) was found to distinguish between participants with penetration above the level of the vocal folds (PA 2–3) to those with penetration to the folds or aspiration (PA 4–8). Disease duration was a significant factor in distinguishing those with no evidence of dysphagia (PA 1) from those with any degree of penetration or aspiration observed during the swallow study (PA 2–8).
Currently, there is no valid, reliable, and efficient way for primary care clinicians or neurologists to screen patients with PD for swallowing dysfunction. The results of this study support the idea that has been previously reported in the literature stating that disease severity does not predict swallowing dysfunction. However, we found that disease duration does begin to separate patients with no swallowing disturbance from those who have or are beginning to demonstrate swallowing abnormalities. Specifically, at the cut-off point of 4.5 years post symptom onset, people with PD begin exhibiting symptoms of airway protective deficits. Based on these data, the 4.5-year duration marker may be the appropriate time for the neurologist or PCP to refer the patient for an initial swallowing evaluation. This proactive approach would facilitate implementation of programs targeting prevention of decline and maintenance of swallowing function. However, for determining the presence of severe versus mild airway protective deficits, disease duration was not an adequately specific predictor.
In order to better identify varying severities of airway protective deficits, it is necessary to include measures derived from reflex cough. The cough motor threshold (Cr2) was the most effective way to distinguish those with mild airway protective deficits from those exhibiting moderate to severe dysphagia with reduced sensitivity of the bolus in the airway. The cognitive perception of the cough-inducing stimulus (i.e., the UTC) was the best predictor of severe swallowing dysfunction, separating those who only penetrated liquids from those who were aspirating liquids. Taken together, these data show that if a patient requires a larger, or more intense, stimulus to trigger a cough response, they are more likely to have deep laryngeal penetration (PA 4, 5) or aspiration (PA 6–8) during swallowing. If the patient has a blunted perception of the strength of the cough stimulus (UTC), they are likely to be silently aspirating. These findings are supported by the shared sensorimotor control of swallowing and cough [16].
Both swallowing and cough consist of highly coordinated sequences of structural movements, require reconfiguration of the ventilatory breathing pattern, and share sensorimotor control (e.g., [17, 18]). For humans in the conscious state, higher-level processing is always involved in the production of swallowing and cough (e.g., [19–21]). This is an important distinction because traditional views of reflexive cough and swallowing consider only brainstem control of the behaviors. More recent studies have shown that stimulus perception at the cortical level occurs for both cough and swallowing, and this level of processing is necessary for normal execution and modulation of the behavior [16, 22, 23]. The volitional or behavioral control of reflex cough occurs because of the UTC, which precedes the cough. The UTC serves to engage the cognitive motivational system in response to a tussive stimulus [22, 24, 25]. In a recent study we found that participants with PD and dysphagia had higher reflex cough thresholds and reduced UTC ratings as compared to nondysphagic PD participants [8]. The reduced UTCs were especially blunted at subthreshold levels of capsaicin in the dysphagic PD participants [8]. This is particularly important because penetration and aspiration of even small amounts of swallowed material accumulates over time resulting in deleterious effects to pulmonary function and health. Improved airway protective outcomes are dependent upon timely awareness and response to subthreshold tussive stimuli and the results of the current study provide further support for the notion that properly screening a patient’s perception of cough stimuli is important for early identification of clinically significant airway protective deficits. The results of this study demonstrate that with worsening airway protective function comes reduced cough motor thresholds and blunted perception of a cough-inducing stimulus.
Interestingly, none of the voluntary cough airflow measures were significant predictors of swallowing dysfunction in these analyses. These findings are in contrast to the Pitts et al. [7] findings. The differences may be explained by variations in methodology. For example, the participants in Pitts et al. [7] completed voluntary single coughs, with instruction to cough hard, and did not complete sequential voluntary coughs or reflex coughs. The participants in Pitts et al. [7] also completed the cough measures with nose clips occluding nasal airflow during the cough maneuvers; whereas, a facemask was utilized in this study accounting for both nasal and oral airflow. Additionally, although disease severity was included as a possible predictor of swallowing dysfunction in the Pitts et al. [7] study, disease duration was not included. Thus, while the relationship between voluntary cough function and dysphagia has been well documented, the current study reveals that sensory measures of reflex cough are likely a better predictor of swallowing dysfunction. This may be related to the fact that reflex cough is a more ecologically valid measure with measurable sensory and motor components.
This study is not without limitations. Although the data were collected prospectively, it was analyzed retrospectively. There is always the possibility that there are other factors which are also salient in identifying patients with airway protective deficits, but this is the first study to include a robust amount of both airway protective and disease-specific predictors to understand dysphagia in PD. Although there was an adequate distribution of disease severity, duration, and airway protective outcomes; a prospective study with the goal of recruiting a larger distribution of swallowing performance and disease duration/severity would help expand and strengthen this body of literature.
Clinical Implications
Deficits of airway protection result in adverse effects to health outcomes, decreased quality of life, and increased health care costs making them an issue of substantial public health concern. This is of particular interest in people with PD in whom aspiration pneumonia secondary to airway protective deficits is a leading cause of death [1–3]. Airway protection is functionally complex and includes a continuum of behaviors with cough and swallowing at either end of that continuum. More specifically, effective swallowing prevents material from entering the airway and effective coughing ejects the aspirate material when airway compromise occurs. There is strong evidence that both swallowing and cough function are impaired in PD (e.g., [8, 26, 27]). In fact, one study identified voluntary cough outcomes as predictive of swallowing safety [7]. However, the results of this study showed that reflex cough sensitivity and perception of cough-inducing stimuli are better predictors of swallowing safety, than measures of voluntary cough airflow. This supports the notion that decreasing the incidence of aspiration pneumonia in PD should target both sensory and motor aspects of cough and swallowing. Recent work by our group and others has identified the utility of bedside reflex cough screening devices for the early identification and management of airway protective deficits (e.g., [28]). The current study helps inform these efforts with identification of specific factors that are predictive of swallowing outcomes. The long-term goal of this research is the development of an easy screening method for airway protective deficits to be used by clinicians in neurology, speech-language pathology, primary medicine, and other clinics.
References
Fernandez HH, Lapane KL. Predictors of mortality among nursing home residents with a diagnosis of Parkinson’s disease. Med Sci Monit. 2002;8(4):CR241–6.
Fall PA, Saleh A, Fredrickson M, Olsson JE, Granerus AK. Survival time, mortality, and cause of death in elderly patients with Parkinson’s disease: a 9-year follow-up. Mov Disord. 2003;18(11):1312–6.
D’Amelio M, Ragonese P, Morgante L, Reggio A, Callari G, Salemi G, Savettieri G. Long-term survival of Parkinson’s disease: a population-based study. J Neurol. 2006;253(1):33–7.
Gorell JM, Johnson CC, Rybicki BA. Parkinson’s disease and its comorbid disorders: an analysis of Michigan mortality data, 1970 to 1990. Neurology. 1994;4(10):1865–8.
Miller N, Noble E, Jones D, Burn D. Hard to swallow: dysphagia in Parkinson’s disease. Age Ageing. 2006;35(6):614–8.
Pitts T, Bosler DC, Rosenbeck JC, Troche MS, Sapienza C. Voluntary cough production and swallow dysfunction in Parkinson’s disease. Dysphagia. 2008;23(3):297–301.
Pitts T, Troche MS, Mann G, Rosenbeck JC, Okun MS, Sapienza C. Using voluntary cough to detect penetration and aspiration during oropharyngeal swallowing in patients with Parkinson disease. Chest. 2010;138(6):1426–31.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson’s disease. Chest. 2014;146(5):1294–9.
Smith Hammond CA, Goldstein LB, Zajac DJ, Gray L, Davenport PW, Bolser DC. Assessment of aspiration risk in stroke patients with quantification of voluntary cough. Neurology. 2001;56(4):502–6.
Smith Hammond CA, Goldstein LB, Horner RD, Ying J, Gray L, Gonzalez-Rothi DC, Bolser DC. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009;135(3):769–77.
Hegland KW, Okun MS, Troche MS. Sequential voluntary cough and aspiration or aspiration risk in Parkinson’s disease. Lung. 2014;192(4):601–8.
Wheeler Hegland K, Troche MS, Brandimore AE, Davenport PW, Okun MS. Comparison of voluntary and reflex cough effectiveness in Parkinson’s disease. Parkinsonism Relat Disord. 2014;20(11):1226–30.
Vovk A, Bolser DC, Hey JA, Danzig M, Vickroy T, Berry R, Martin AD, Davenport PW. Capsaicin exposure elicits complex airway defensive motor patterns in normal humans in a concentration-dependent manner. Pulm Pharmacol Ther. 2007;20(4):423–32.
Hegland KW, Troche MS, Davenport PW. Cough expired volume and airflow rates during sequential induced cough. Front Physiol. 2013;4:167.
Rosenbeck JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Troche MS, Brandimore AE, Godoy J, Hegland KW. A framework for understanding shared substrates of airway protection. J Appl Oral Sci. 2014;22(4):251–60.
Bolser DC, Poliacek J, Jakus J, Fuller DD, Davenport PW. Neurogenesis of cough, other airway defensive behaviors and breathing: a holarchical system. Respir Physiol Neurobiol. 2006;152(3):255–65.
Davenport PW, Bolser DC, Morris KF. Swallow remodeling of respiratory neural networks. Head Neck. 2013;33(Suppl 1):S8–13.
Mazzone SB, McGovern AE, Yang SK, Woo A, Phipps S, Ando A, Leech J, Farrel MJ. Sensorimotor circuitry involved in the higher brain control of coughing. Cough. 2013;9(1):7.
Mazzone SB, Cole LJ, Ando A, Egan GF, Farrel MJ. Investigation of the neural control of cough and cough suppression in humans using functional brain imaging. J Neurosci. 2011;31(8):2948–58.
Simonyan K, Saad ZS, Loucks TM, Poletto CJ, Ludlow CL. Functional neuroanatomy of human voluntary cough and sniff production. Neuroimage. 2007;37(2):401–9.
Davenport PW. Clinical cough I: the urge-to-cough: a respiratory sensation. Handb Exp Pharmacol. 2009;187:263–76.
Theurer JA, Bihari F, Barr AM, Martin RE. Oropharyngeal stimulation with air-pulse trains increases swallowing frequency in healthy adults. Dysphagia. 2005;20(4):254–60.
Davenport PW, Sapienza CS, Bolser D. Psychophysical assessment of the urge-to-cough. Eur Respir J. 2002;12(85):249–53.
Davenport PW, Bolser DC, Vickroy T, Berry RB, Martin AD, Hey JA, Danzig M. The effect of codeine on the urge-to-cough response to inhaled capsaicin. Pulm Pharmacol Ther. 2007;20(4):338–46.
Ebihara S, Saito H, Kanda A, Nakajoh M, Takahashi H, Arai H, Sasaki H. Impaired efficacy of cough in patients with Parkinson disease. Chest. 2003;124(3):1009–15.
Fontana GA, Pantaleo T, Lavorini F, Benvenuti F, Gangemi S. Defective motor control of coughing in Parkinson’s disease. Am J Respir Crit Care Med. 1998;158(2):458–64.
Hegland KW, Troche MS, Brandimore AE, Okun MS, Davenport PW. Comparison of two methods for inducing reflex cough in patients with Parkinson’s disease, with and without dysphagia. Dysphagia. 2016;31(1):66–73.
Acknowledgments
We would like to first acknowledge the participants and caregivers who so generously gave of their time to participate in this study. We also acknowledge the support of the National Parkinson Foundation Center of Excellence at the University of Florida and of the NIH (NCATS) CTSA through the University of Florida (UL1TR000064 and KL2TR000065) awarded to Dr. Michelle S. Troche.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Troche’s work was supported in part by an NIH (NCATS) CTSA through the University of Florida (UL1TR000064 and KL2TR000065). She has no other disclosures or conflicts of interest to report. Ms. Schumann has no financial disclosures to report. Dr. Brandimore’s work was supported in part by a predoctoral fellowship through the Department of Veterans Affairs. Dr. Okun serves as a consultant for the National Parkinson Foundation, and has received research grants from NIH, NPF, the Michael J. Fox Foundation, the Parkinson Alliance, Smallwood Foundation, the Bachmann-Strauss Foundation, the Tourette Syndrome Association, and the UF Foundation. Dr. Okun has previously received honoraria, but in the past >36 months has received no support from industry. Dr. Okun has received royalties for publications with Demos, Manson, Amazon, and Cambridge (movement disorders books). Dr. Okun is an associate editor for New England Journal of Medicine Journal Watch Neurology. Dr. Okun has participated in CME activities on movement disorders in the last 36 months sponsored by PeerView, Prime, and by Vanderbilt University. The institution and not Dr. Okun receives grants from Medtronic and ANS/St. Jude, and the PI has no financial interest in these grants. Dr. Okun has participated as a site PI and/or co-I for several NIH, foundation, and industry sponsored trials over the years but has not received honoraria. Dr. Hegland’s work is supported in part by the American Heart Association, National Institutes of Health and BAE defense systems.
Rights and permissions
About this article
Cite this article
Troche, M.S., Schumann, B., Brandimore, A.E. et al. Reflex Cough and Disease Duration as Predictors of Swallowing Dysfunction in Parkinson’s Disease. Dysphagia 31, 757–764 (2016). https://doi.org/10.1007/s00455-016-9734-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9734-6