Abstract
Animal trypanosomosis is an important endemic and wasting disease in sub-Saharan Africa. Its control relies on chemotherapy, and resistance to trypanocides has been widely reported. The pathogenicity of drug-resistant canine trypanosomes is not clear with scanty information available. Thus, this study assessed the comparative pathogenicity of drug-resistant and drug-sensitive Trypanosoma brucei and Trypanosoma congolense infections in dogs. Twenty Nigerian local dogs were used and were randomly assigned into five groups (A–E) of four dogs each. Group A served as the uninfected-control group, while groups B and C were infected with 106 drug-sensitive T. congolense and T. brucei. Groups D and E were infected with 106 multidrug-resistant T. congolense and T. brucei, respectively. The pre-patent period (PPP), clinical signs, level of parasitaemia (LOP), rectal temperature, body weight, packed cell volume (PCV), red blood cell count (RBC), haemoglobin concentration (HbC), mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), mean corpuscular haemoglobin concentration (MCHC), total leucocyte count (TLC) and survivability were assessed. Groups D and E had longer (p < 0.05) mean PPP than groups B and C. Also, group E dogs had lower (p < 0.05) mean LOP, longer (p < 0.05) mean survivability, and higher (p < 0.05) mean body weight, PCV, HbC and RBC than group C dogs. The clinical signs were very severe in group C dogs, compared to group E dogs. However, these parameters did not differ statistically between groups B and D. Thus, multidrug-resistant T. brucei was of lower pathogenicity than drug-sensitive T. brucei, while multidrug-resistant and drug-sensitive T. congolense had comparable pathogenicity following infection in dogs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy is the most practical and widely applied method for controlling African animal trypanosomosis in sub-Saharan Africa (Giordani et al. 2016). Other trypanosomosis control methods involving trypanotolerant livestock, and tsetse control are sparingly utilized in Africa owing to their high cost and laborious nature (Obi et al. 2019). Despite the over-dependence on trypanocides for trypanosomosis control, with an estimated yearly utilization rate of about 50 million doses (McDermott et al. 2003), pharmaceutical companies are unwilling to fund the development and licensing of new animal trypanocides. There is also the problem of extensive abuse and poor quality of trypanocides (Tekle et al. 2018). The resultant effects are increased pressure on the few available old trypanocides and the occurrence of drug-resistant trypanosome strains.
Trypanocidal resistance has been reported in many African countries (Delespaux et al. 2008; Mulandane et al. 2017) and is increasingly recognized as a major threat to livestock production, pet rearing and the actualization of the sustainable development goals (SDGs) in Africa. The pathogenicity of drug-resistant trypanosomes is not clear (Geerts et al. 2001), though it is generally believed that resistance reduces the virulence and/or fitness of parasites in the absence of drugs (Coleman et al. 2000). Variations in the virulence and/or pathogenicity of trypanosomes species, strains and sub-groups have been reported (Motloang et al. 2014; Kabore et al. 2018). Conflicting reports abound on drug-resistant trypanosomes’ virulence and/or pathogenicity (Ihedioha et al. 2010; Ngumbi and Mnyone 2020). Also, paucity of information exists on the pathogenicity of drug-resistant trypanosomes in dogs despite reports of drug-resistant trypanosomes in dogs (Anene et al. 1999; Obi et al. 2022a, b). Thus, this study assessed the comparative pathogenicity of drug-resistant and drug-sensitive Trypanosoma brucei and Trypanosoma congolense infections in dogs.
Materials and methods
Experimental animals
Twenty male Nigerian local mongrel dogs aged between 12 and 24 months and weighing between 5.9 and 9.2 kg used in this study were housed in the Kennel Unit of the Laboratory Animal House of the Department of Veterinary Parasitology and Entomology, University of Nigeria, Nsukka. The dogs were identified by body markings and kept in groups of two dogs in clean metal cages. They were fed twice daily with commercial dog feed (Balance®, Balance Pet Food, Israel) and were given clean drinking water in stainless bowels ad libitum.
The dogs were acclimatized for 1 month within which they were screened and confirmed negative for trypanosomosis using wet blood film examination, examination of Giemsa-stained thin blood smear and buffy coat techniques. They were dewormed orally with albendazole (Albendazole®, GSK, UK) at a dose rate of 10 mg per kg body weight for 3 consecutive days. The dogs were treated against ectoparasites using ivermectin (Ivermectine®, Hebei Kexing Pharmaceutical, China) at a dose rate of 0.3 mg/kg body weight and vaccinated against rabies (Canvac®R, Dyntec, Czech Republic), canine distemper, hepatitis, leptospirosis, parvovirus and parainfluenza (Biocan® Novel Puppy, Bioveta, Czech Republic).
Trypanosomes
Trypanosomes used in this study were multidrug-resistant [resistant to both diminazene aceturate (DA) and isometamidium chloride (ISM)] and drug-sensitive Trypanosoma brucei and T. congolense. The trypanosomes were isolated from naturally infected dogs and molecularly identified via nested ITS-PCR following a cross-sectional study in Enugu North Senatorial Zone, Southeast Nigeria between January and August, 2016 (Obi et al. 2022a). The trypanosomes were also subjected to both single and multi-dose tests to determine their sensitivity to trypanocides and the dose required to cure 50% of the infected animals (CD50) [Obi et al. 2022b]. The trypanosomes were multidrug-resistant Trypanosoma brucei (DA CD50 = 34.19 mg/kg; ISM CD50 = 4.75 mg/kg), multidrug-resistant Trypanosoma congolense (DA CD50 = 30.61 mg/kg; ISM CD50 = 3.96 mg/kg), drug-sensitive Trypanosoma brucei (DA CD50 = 2.49 mg/kg; ISM CD50 = 0.19 mg/kg) and drug-sensitive Trypanosoma congolense (DA CD50 = 3.24 mg/kg; ISM CD50 = 0.16 mg/kg).
Experimental design
The dogs were randomly assigned to five groups (A–E) of four. Random numbers were generated using the standard = RAND() function in Google Sheets. Group A was the uninfected control group, while groups B and C were infected intraperitoneally (i.p) with 106 drug-sensitive T. congolense and T. brucei, respectively. Groups D and E were infected i.p with 106 multidrug-resistant T. congolense and T. brucei, respectively. Thereafter, blood samples were collected from the dogs and screened daily for parasitaemia using wet blood film examination and buffy coat techniques. The dogs were also clinically examined daily. The blood sampling and clinical examination period was between 7:30 am and 1:00 pm. The sampling, clinical examination and analysis order was randomized daily and/or weekly. To minimize pain, distress and animal suffering, minimal volume of blood was drawn from the experimental dogs at each blood sampling with food and water adequately provided. Also, experimental dogs showing severe/terminal signs of trypanosomosis and/or with a packed cell volume of < 20% were removed from the study and were humanely euthanized.
Parameters monitored for the comparative pathogenicity of multidrug-resistant Trypanosoma brucei and Trypanosoma congolense infections included the pre-patent period (PPP), clinical signs, first peak parasitaemia (FPP), days to first peak parasitaemia (DTFPP), daily level of parasitaemia (LOP), weekly body weight, rectal temperature, packed cell volume (PCV), haemoglobin concentration (HbC), red blood cell count (RBC), mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), mean corpuscular haemoglobin concentration (MCHC), total leucocyte count (TLC) and survivability. The rapid matching method of Herbert and Lumsden (1976) was used to assess the daily parasitaemia levels. About 10–20 microscope fields were examined when parasitaemia was detectable, but 40–50 microscope fields were examined when not detectable. Clinical signs were assessed by thorough monitoring, observation and palpation of the infected groups of dogs and the number of dogs per group exhibiting any observed clinical signs was duly recorded. The clinical signs were graded on a four-grade scale (0 = normal; 1 = mild; 2 = severe; 3 = very severe). The body weight and rectal temperature were determined weekly using a standard weighing balance (Avery, UK) and a digital thermometer. The haematological indices were assessed weekly using the standard methods and formulae described in Coles (1986).
Data analysis
Data generated from this study were subjected to normality distribution using Shapiro–Wilk test and analysed using one-way analysis of variance (ANOVA). Variant means were separated using the least significant difference. Subjective clinical sign scores of all the infected groups of dogs were subjected to Kruskall-Wallis H test and the mean ranks of the groups were compared. The level of significance was considered at p < 0.05. All statistical analyses were carried out in SPSS version 21 for windows.
Results
Parasitaemia
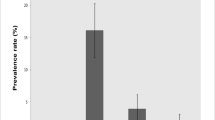
Parasitaemia was detected in the infected groups of dogs between days 4 and 11 post-infection (PI). The mean PPP and DFPP of the drug-sensitive trypanosome-infected groups B and C did not vary considerably but were significantly (p < 0.05) shorter than those of multidrug-resistant trypanosome-infected groups D and E (Fig. 1). Amongst the multidrug-resistant trypanosome-infected groups, group D dogs had significantly (p < 0.05) shorter mean PPP and DFPP than group E dogs. Dogs in groups B and C had significantly (p < 0.05) higher mean FPP, compared to the dogs in groups D and E (Fig. 2). Also, the mean FPP of group E dogs was significantly (p < 0.05) lower than that of group C dogs, while that of group B dogs did not differ statistically from those of groups D and E. The mean LOP of drug-sensitive T. brucei-infected group C dogs was significantly (p < 0.05) higher than the rest of the infected groups on days 3–6 and 8–10 PI, peaking on day 10 PI (Fig. 3). T. congolense-infected groups B and D also had significantly (p < 0.05) higher mean LOP than the multidrug-resistant T. brucei-infected group E except on day 20 PI.
Clinical findings
The clinical signs observed following infection of the experimental animals are itemized in Table 1. Most of these clinical signs were more severe in groups B, C and D dogs than in group E. The multidrug-resistant trypanosome-infected groups D and E had significantly lower mean rectal temperature at weeks 3 and 1–2 PI, respectively, compared to the drug-sensitive trypanosome-infected groups B and C (Fig. 4).
There was a significant decrease (p < 0.05) in the mean body weight of all the dogs in the infected groups (Fig. 5). However, group B had significantly lower (p < 0.05) body weight changes than groups C, D and E.
Haematological parameters
A significant (p < 0.05) decline in the mean PCV of the infected groups was observed from week 2 PI, compared to the uninfected control group (Fig. 6). The drug-sensitive T. brucei-infected group C dogs had significantly (p < 0.05) lower mean PCV than the multidrug-resistant T. brucei-infected group E dogs at weeks 2 and 3 PI. The mean PCV value of the T. congolense-infected groups B and D were decreased but did not differ significantly (p > 0.05).
The mean HbC values of the group C dogs were significantly (p < 0.05) lower than that of group E dogs at weeks 1–3 PI (Fig. 7). Groups B and D had comparable mean HbC values, except at week 2 PI, where group B had significantly (p < 0.05) lower HbC values. The mean RBC count of group E dogs did not differ (p > 0.05) from that of group A till week 2 PI and was significantly (p < 0.05) higher than that of group C dogs between weeks 1 and 3 PI (Fig. 8). Group D dogs had significantly (p < 0.05) higher mean RBC count values at weeks 2 and 3 PI than the dogs in group B, while group B dogs had significantly (p < 0.05) higher mean RBC count than group C and D at week 1 PI. A significant decline was observed in the mean TLC of the infected groups of dogs, compared to the uninfected control group A from week 2–3 PI (Fig. 9). At week 3 PI, the mean TLC of group C dogs was significantly (p < 0.05) higher when compared with the other infected groups.
Group B dogs had significantly higher (p < 0.05) mean MCV values than group C dogs at week 1 PI (Table 2). The mean MCH and MCHC of the experimental dogs did not significantly differ (p > 0.05) from each other between weeks 0–3 PI (Table 2). Beyond week 3 PI, the MCHC of group E dogs was significantly lower than that of the uninfected control group A.
Survivability
The mean post-infection survival times of the infected dogs were 20.25 ± 2.32, 19.25 ± 2.32, 24.50 ± 2.75 and 30.25 ± 3.86 days for groups B, C, D and E, respectively (Fig. 10). Multidrug-resistant T. brucei-infected group E dogs had significantly (p < 0.05) longer mean post-infection survival time than those of groups B and C but did not differ significantly (p > 0.05) from that of group D. The mean post-infection survival time of group D dogs did not also vary significantly (p > 0.05) from those of groups B and C.
Discussion
This study sought to determine the pathogenicity of multidrug-resistant and drug-sensitive Trypanosoma brucei and T. congolense in Nigerian local dogs. Field strains of multidrug-resistant and drug-sensitive Trypanosoma brucei and T. congolense were used with few passages in mice. The drug-sensitive T. brucei and T. congolense isolates had significantly shorter mean PPP than their multidrug-resistant counterparts. Similar findings of significantly shorter mean PPP in drug-sensitive isolates compared to drug-resistant isolates have been reported in T. congolense (Burudi et al. 1994; Coleman et al. 2000; Tesfaye et al. 2012) and T. brucei (Egbe-Nwiyi et al. 2005; Ihedioha et al. 2010) infected animals. However, in mice infected with drug-sensitive and resistant T. congolense (Ngumbi and Mnyone 2020), their mean PPP did not vary significantly. Ngumbi and Mnyone (2020) also reported shorter PPP in drug-resistant T. congolense-infected steer than the drug-sensitive T. congolense-infected steer. The differences in the mean PPP may be attributed to the varying levels of sensitivity of trypanosomes to trypanocides, differences in trypanosome species and strains, varying infective doses, number of passages of trypanosome stock, and the different animal species utilized.
The multidrug-resistant T. brucei-infected group E dogs had significantly lower mean LOP, FPP and longer mean DTFPP, compared to the drug-sensitive T. brucei-infected group C dogs, indicating low virulence and the ability of the immune system to control the parasite, while the higher parasitaemia observed in the groups B, C and D dogs suggest that these parasites were more virulent. Multidrug-resistant T. congolense-infected group D also had longer mean DTFPP than group B. These findings were similar to the reports of Egbe-Nwiyi et al. (2005) and Ihedioha et al. (2010) in rats. Hugo (2011) observed no significant differences in the mean LOP of melarsoprol-resistant and sensitive T. brucei rhodesiense in mice, while Tesfaye et al. (2012) observed significantly low LOP in goats infected with drug-resistant T. congolense. Lower FPP and longer DTFPP have also observed in melarsoprol-resistant T. brucei rhodesiense-infected mice (Hugo 2011).
In the current study, beyond week 3 PI, most dogs either died or showed terminal clinical signs of trypanosomosis and were humanely euthanized. Therefore, evaluating the clinical and haematological parameters amongst the different infected groups of dogs was not possible. Consequently, the comparison was made between weeks 0 and 3 PI. The observed clinical signs following infection of dogs were usual of canine trypanosomosis and were akin to the reports of Ezeokonkwo et al. (2010) and Obi et al. (2013). The severity of the clinical signs observed in groups B, C and D dogs could be related to the persistently high level of parasitaemia observed in such dogs. Bloody diarrhoea was previously reported by Ezeokonkwo et al. (2010) in T. congolense-infected dogs. In the present study, it was observed in both drug-sensitive T. brucei and T. congolense-infected dogs and was believed to have stemmed from intestinal intussusceptions observed in some bloody diarrheic dogs at necropsy.
Pyrexia was observed in this study amongst the trypanosome-infected dogs, with the multidrug-resistant trypanosome-infected groups having significantly lower mean rectal temperature than the drug-sensitive trypanosome-infected groups at some weeks post-infection. Increased rectal temperature in trypanosome infected dogs was also reported by some authors (Ezeokonkwo et al. 2010; Obi et al. 2013). Tesfaye et al. (2012) reported diminazene-sensitive T. congolense-infected goats having higher rectal temperatures than the diminazene-resistant infected group. Pyrexia in trypanosomosis is hypothesized to arise from the metabolism of tryptophan to tryptophol by trypanosomes (Taylor and Authie 2004), which tends to exert its effects on the thermoregulatory centre of the hypothalamus so that the thermostatic level of the body is raised.
The weight loss evident in the infected dogs compared to the uninfected dogs could be attributed to anorexia, dehydration and emaciation observed in the infected dogs. The multidrug-resistant T. brucei-infected dogs lost the least body weight, compared to the other infected groups of dogs and this could be associated with the low LOP and mild anorexia, emaciation and dehydration observed in the multidrug-resistant T. brucei-infected group E dogs. Otavio et al. (2016) reported a positive correlation between weight loss and the number of circulating Trypanosoma sp. A similar finding of reduced weight loss was reported by Odette (2011) in mice infected with melarsoprol-resistant Trypanosoma brucei rhodesiense compared to its sensitive counterpart, while Ihedioha et al. (2010) and Hugo (2011) observed no significant differences in the mean body weights of drug-sensitive and resistant trypanosome-infected animals.
The low levels of packed cell volume, haemoglobin concentration and red blood cell counts detected in the infected groups of dogs indicate anaemia, manifested by the pallor of the mucous membranes. Anaemia is the most prominent feature of trypanosomosis and has been reported in several trypanosome-infected animals (Ezeokonkwo et al. 2010; Obi et al. 2013; 2019). The pathophysiology of anaemia in trypanosomosis is variable and has been variously reviewed by researchers (Taylor and Authie 2004; Mbaya et al. 2012).
The anaemia in multidrug-resistant T. brucei-infected group E dogs was mild, compared to that of the other infected groups of dogs. Also, multidrug-resistant T. congolense-infected group D had less severe anaemia than the drug-sensitive T. congolense-infected group B. This may indicate that the drug sensitivity of Trypanosoma species may have some impact on the pathogenicity of the trypanosomal infection in animals. The mild anaemia observed in the group E dogs could be due to the low LOP, low virulence of the parasite and possibly the role of the host’s immune response. The onset and severity of anaemia in trypanosomosis are directly related to the appearance of the parasite in the blood and the level of parasitaemia (Murray 1979). Mild anaemia in drug-resistant trypanosome infections depicted by considerably higher packed cell volume than that of the drug-sensitive trypanosome infections has also been reported in diminazene-resistant T. brucei-infected rats (Egbe-Nwiyi et al. 2005; Ihedioha et al. 2010) and diminazene-resistant T. congolense-infected goats (Tesfaye et al. 2012). Nonetheless, Hugo (2011) and Odette (2011) reported no differences in the severity of anaemia induced by drug-resistant and sensitive T. brucei rhodesiense in mice.
The anaemia type reported in this study’s infected groups was microcytic normochromic anaemia. Similar findings have been reported in T. evansi-infected dogs and horses (Silva et al. 1995) and T. brucei rhodesiense-infected vervet monkeys (Thuita et al. 2008). Dacie et al. (2001) associated microcytic hypochromic anaemia with iron deficiency. Thus, the inability of iron to be integrated into red cell precursors even in the presence of sufficient iron reserve or weak recovery of iron from the phagocytized RBCs in the infected dogs may have occasioned the occurrence of this type of anaemia. In this case, quantifying the levels of iron reserve in the dogs could be crucial.
Leucopenia was observed in the infected groups of dogs. However, in the drug-sensitive and resistant T. brucei-infected groups of dogs, there was a subsequent rise in the total leucocyte counts. A similar pattern has been reported by Otavio et al. (2016) in T. vivax-infected cattle. The observed leucopenia may be attributed to the immunosuppressive effect of trypanosome infections and trypanosome-induced alterations in the spleen, the major lymphoid organ. Immunosuppression in animal trypanosomosis has been severally reported (Taylor and Authie 2004) with a resultant low-grade response to vaccines and/or the diminished ability of infected animals to mount a primary humoral immune response to non-trypanosome antigens (Ezeokonkwo et al. 2010).
Dogs infected with multidrug-resistant T. brucei survived longer than their drug-sensitive counterparts, while there was no statistical difference in the mean survival times of the T. congolense-infected groups B and D dogs. Some researchers have reported that drug-resistant trypanosome-infected animals have longer survival time than their drug-sensitive counterparts (Egbe-Nwiyi et al. 2005; Ihedioha et al. 2010; Hugo 2011; Odette 2011). However, Mutangala (2011) and Ngumbi and Mnyone (2020) reported a longer mean survival time in mice infected with isometamidium-sensitive T. congolense than isometamidium-resistant T. congolense-infected mice. The preponderance of the stumpy T. brucei forms in infected animals has been reported to increase the chances of parasite transmission and lengthens host survival time (MacGregor et al. 2012). Though the parasitaemia of T. brucei-infected dogs was not characterized into the different forms in this study, the extended survival time observed in the multidrug-resistant T. brucei-infected group E dogs might be due to the dominance of stumpy forms in addition to the low virulence of the parasite strain.
The pre-patent period, level of parasitaemia, first peak parasitaemia, days to first peak parasitaemia and survivability are recognized chief indicators of trypanosome virulence and/or pathogenicity (Bengaly et al. 2002; Egbe-Nwiyi et al. 2005; Taylor and Authie 2004; Ihedioha et al. 2010; Motloang et al. 2014). Trypanosome isolates with short mean PPP, high LOP and short survival time were reportedly very virulent/pathogenic (Bengaly et al. 2002; Masumu et al. 2006; Perrone et al. 2018). Thus, the longer PPP, DTFPP, survival time and lower LOP and FPP of the resistant isolates principally the multidrug-resistant T. brucei-infected group E dogs are indicators of reduced/low virulence and/or pathogenicity. Genetic variations induced by mutations of specific genes and gene transfer have been established in trypanosomes and may be responsible for acquired drug resistance (Geerts and Holmes 1998; Delespaux et al. 2008). As such, drug-sensitive trypanosomes may vary in the manifestation of some phenotypic features and macromolecules related to virulence and pathogenicity from the drug-resistant trypanosomes.
The multidrug-resistant T. brucei-infected group E dogs exhibited low level of parasitaemia, low first peak parasitaemia, long pre-patent period and survival time; mild clinical signs, anaemia and improved haematological parameters, compared to the drug-sensitive T. brucei-infected group C dogs. This denotes low pathogenicity of the multidrug-resistant T. brucei isolate. The observed low pathogenicity of the multidrug-resistant T. brucei in this study may be attributed to the sensitivity of the trypanosome to trypanocide, in addition to the strain of the parasite, as the sensitivity of trypanosomes to trypanocides was hypothesized to influence the virulence and/or pathogenicity of trypanosomes (Geerts and Holmes 1998; Geerts et al. 2001).
Drug resistance comes at a cost as studies have severally shown that drug-resistant parasite strains were likely to be less fit than the wild-type strains (Giha et al. 2006; Schneider et al. 2012). However, Levin et al. (2000) and Giha et al. (2006) reported the ability of drug-resistant parasites in the absence of drugs to develop a compensatory mechanism to recover the cost and to ensure their survival. This, in addition to the strain of T. congolense used, could be responsible for the seemingly comparable pathogenicity of the multidrug-resistant and drug-sensitive T. congolense-infected dogs. These findings were akin to the report of Coleman et al. (2000), who observed no difference in the pathogenicity of isometamidium-resistant and sensitive T. congolense-infected animals, except for the longer pre-patent period of the resistant T. congolense-infected animals.
The use of field strains of multidrug-resistant and drug-sensitive Trypanosoma brucei and T. congolense is a limitation in this study. The field Trypanosoma specie may consist of different strains of the Trypanosoma specie, thus, presence of mixed Trypanosoma strain infections cannot be ruled out. However, the field trypanosome strains were deliberately not cloned as cloning in rodents may introduce selection bias (Masumu et al. 2006; Kabore et al. 2018). Regrettably, unbiased techniques for isolating trypanosomes in adequate quantities are currently non-existent.
In conclusion, this study has shown that drug-sensitive T. brucei is more pathogenic than multidrug-resistant T. brucei, following infection in Nigerian local dogs, while the multidrug-resistant and drug-sensitive T. congolense had comparable pathogenicity.
Data availability
All additional data associated with this study can be obtained from the corresponding author on reasonable request.
References
Anene BM, Chukwu CC, Anika SM (1999) Sensitivity to diminazene aceturate and isometamidium chloride of trypanosomes isolated from dogs in Nsukka area, Nigeria. Revue Élev Méd Vét Pays Trop 52(2):129–131
Bengaly Z, Sidibe I, Ganaba R, Desquesnes M, Boly H, Sawadogo L (2002) Comparative pathogenicity of three genetically distinct types of Trypanosoma congolense in cattle: clinical observations and haematological changes. Vet Parasitol 108:1–19. https://doi.org/10.1016/S0304-4017(02)00164-4
Burudi EM, Peregrine AS, Mejia PO, Mbiuki SM, Murphy NB (1994) Response of diminazine aceturate resistant and diminazine aceturate susceptible Trypanosoma congolense to treatment with Diminazine when occurring together as a mixed infection. Ann Tropl Med Parasitol 88(6):595–606. https://doi.org/10.1080/00034983.1994.11812910
Coleman PG, Eisler MC, McDermott JJ, Murphy NB, Majiwa PAO, Peregrine AS (2000) Relative fitness in laboratory mice of drug-resistant and drug-sensitive field isolates of Trypanosoma congolense. Australasian e-Library of Veterinary & Animal Science. https://www.sciquest.org.nz/browse/publications/article/71162. Accessed 15 Feb 2022
Coles EH (1986) Veterinary clinical pathology, 4th edn. WB Saunders, Philadelphia
Dacie J, Bain B, Imelda B, Lewis M (2001) Practical haematology, 9th edn. Churchill Livingstone, London, pp 34–35
Delespaux V, Geysen D, Van den Bossche P, Geerts S (2008) Molecular tools for the rapid detection of drug resistance in animal trypanosomes. Trends Parasitol 24:236–242. https://doi.org/10.1016/j.pt.2008.02.006
Egbe-Nwiyi TN, Igbokwe IO, Onyeyili PA (2005) Diminzene aceturate resistance on the virulence of Trypanosoma brucei for rats. J Comp Path 133:286–288. https://doi.org/10.1016/j.jcpa.2005.05.002
Ezeokonkwo RC, Ezeh IO, Onukwu JI, Obi PO, Onyenwe IW, Agu WE (2010) Comparative haematological study of single and mixed infections of mongrel dogs Trypanosoma congolense and Trypanosoma brucei brucei. Vet Parasitol 173:48–54. https://doi.org/10.1016/j.vetpar.2010.06.020
Geerts S, Holmes PH, Diall O, Eisler MC (2001) African bovine trypanosomiasis. the problem of drug resistance. Trends Parasitol 17:25–28. https://doi.org/10.1016/S1471-4922(00)01827-4
Geerts S, Holmes PH (1998) Drug management and parasite resistance in bovine trypanosomosis in Africa. Program against African Trypanosomes (PAAT). Technical and scientific series 1. Food Agric Org U N (FAO) Rome, 25:1–3.
Giha HA, Elbashir MI, A-Elbasit IE, A-Elgadir TME, El-Ghazali GE, Mackinnon MJ, Babiker HA (2006) Drug resistance–virulence relationship in Plasmodium falciparum causing severe malaria in an area of seasonal and unstable transmission. Acta Trop 97:181–187. https://doi.org/10.1016/j.actatropica.2005.10.004
Giordani F, Morrison LJ, Rowan TG, De Koning HP, Barrett MP (2016) The animal trypanosomiases and their chemotherapy: a review. Parasitol 143(14):1862–1889. https://doi.org/10.1017/S0031182016001268
Herbert WJ, Lumsden WH (1976) Trypanosoma brucei: a rapid “Matching” method for estimating the host’s parasitaemia. Exp Parasitol 40:427–431. https://doi.org/10.1016/0014-4894(76)90110-7
Hugo KM (2011) Molecular characterization and pathogenicity of melarsoprol resistant and sensitive Trypanosoma brucei rhodesiense isolates from Uganda. Dissertation, Egerton University
Ihedioha JI, Onuma CJ, Okorie-Kanu CO, Ihedioha TE (2010) Changes in the pathogenicity of relapsed diminazene aceturate (DA)-resistant Trypanosoma brucei brucei as the trypanosomes are transmitted from DA-treated hosts to another set of animals. Comp Clin Pathol 19:481–486. https://doi.org/10.1007/s00580-009-0893-9
Kaboré J, Camara O, Koffi M, Sanou D, Ilboudo H, Sakandé H, Camara M, De Meeûs T, Ravel S, Belem AMG, MacLeod A, Bucheton B, Jamonneau V, Thévenon S (2018) Differences in pathogenicity and virulence of Trypanosoma brucei gambiense field isolates in experimentally infected Balb/C mice. Infect Genet Evol 63:269–276. https://doi.org/10.1016/j.meegid.2018.05.018
Levin BR, Perrot V, Walker N (2000) Compensatory mutations, antibiotic resistance and the population genetics of adaptive evolution in bacteria. Genet 154:985–997. https://doi.org/10.1093/genetics/154.3.985
MacGregor P, Szöoõr B, Savill NJ, Matthews KR (2012) Trypanosomal immune evasion, chronicity and transmission: an elegant balancing act. Nat Rev Microbiol 10(6):431–438. https://doi.org/10.1038/nrmicro2779
Masumu J, Marcotty T, Geysen D, Geerts S, Vercruysse J, Dorny P, den Bossche PV (2006) Comparison of the virulence of Trypanosoma congolense strains isolated from cattle in a trypanosomiasis endemic area of eastern Zambia. Int J Parasitol 36:497–501. https://doi.org/10.1016/j.ijpara.2006.01.003
Mbaya A, Kumshe H, Nwosu CO (2012) The mechanisms of anaemia in trypanosomosis: a review. In: Silverberg D (ed) Anaemia, InTechopen. https://doi.org/10.5772/29530
McDermott J, Woitag T, Sidibe I, Bauer B, Diarra B, Oue´draogo D, Kamuanga M, Peregrine A, Eisler M, Zessin K-H, Mehlitz D, Clausen P-H (2003) Field studies of drug-resistant cattle trypanosomes in Ke´ne´dougou Province, Burkina Faso. Acta Trop 86:93–103. https://doi.org/10.1016/S0001-706X(03)00019-6
Motloang MY, Masumu J, Mans BJ, Latif AA (2014) Virulence of Trypanosoma congolense strains isolated from cattle and African buffaloes (Synceru scaffer) in KwaZulu-Natal. South Africa Onderstepoort J Vet Res 81:679. https://doi.org/10.4102/ojvr.v81i1.679
Mulandane FC, Fafetine J, Van Den Abbeele J, Clausen P-H, Hoppenheit A, Cecchi G, Oosthuizen M, Delespaux V, Neves L (2017) Resistance to trypanocidal drugs in cattle populations of Zambezia Province, Mozambique. Parasitol Res https://doi.org/10.1007/s00436-017-5718-1
Murray M (1979) The anaemia of bovine African trypanosomiasis: an overview. In: Losos G, Chouinard A (eds) Pathogenicity of Trypanosomes. IDRC, Ottawa, pp 121–127
Mutangala NW (2011) Transmisibility and virulence study of drug sensitive and resistant Trypanosoma congolense in mice. Dissertation, Egerton University
Ngumbi A, Mnyone L (2020) Pathogenicity of trypanosomes in relation to 1 drug sensitivity: comparative studies between a drug-sensitive and drug-resistant Trypanosoma congolense strain in murine-and bovine model. Preprint, https://doi.org/10.21203/rs.3.rs-17414/v1
Obi CF, Obidike IR, Ezeh IO, Omoja VU, Iheagwam CN, Idika IK, Ezeokonkwo RC (2013) Effects of Trypanosoma brucei infection and diminazene aceturate therapy on testicular morphology and function of Nigerian local dogs. Vet Parasitol 196(3):283–288. https://doi.org/10.1016/j.vetpar.2013.03.023
Obi CF, Nzeakor TA, Okpala MI, Ezeh IO, Nwobi LG, Omeje MO, Ezeokonkwo RC (2019) Evaluation of antitrypanosomal activity of Pterocarpus santalinoides L’H’erit ex DC hydroethanol leaf extract in rats experimentally infected with Trypanosoma brucei. J Ethnopharmacol 243:112085. https://doi.org/10.1016/j.jep.2019.112085
Obi CF, Ezeh IO, Okpala MI, Agina A, Umeakuana PU, Essuman GAA, Gwira TM, Ezeokonkwo RC (2022a) Prevalence and molecular identification of trypanosomes in dogs in Enugu North Senatorial Zone. South East Nigeria. Acta Parasitol 67(1):391–402. https://doi.org/10.1007/s11686-021-00475-4
Obi CF, Okpala MI, Ezeh IO, Onyeabo A, Ezeokonkwo RC (2022b) Drug-resistant trypanosome isolates populations in dogs in Enugu North Senatorial Zone. Southeastern Nigeria. Parasitol Res 121(1):423–431. https://doi.org/10.1007/s00436-021-07362-x
Odette AE (2011) Transmissibility and virulence of drug sensitive and resistant Trypanosoma brucei rhodesiense isolates from Kenya. Dissertation, Egerton University
Otavio LFJ, Sampaio PH, Machado RZ, André MR, Marques LC, Cadioli FA (2016) Evaluation of clinical signs, parasitemia, hematologic and biochemical changes in cattle experimentally infected with Trypanosoma vivax. Rev Bras Parasitol Vet 25(1). https://doi.org/10.1590/S1984-29612016013
Perrone T, Aso PM, Mijares A, Holzmuller P, Gonzatti M, Parra N (2018) Comparison of infectivity and virulence of clones of Trypanosoma evansi and Trypanosoma equiperdum Venezuelan strains in mice. Vet Parasitol 253:60–64. https://doi.org/10.1016/j.vetpar.2018.02.024
Schneider P, Bell AS, Sim DG, O’Donnell AJ, Blanford S, Paaijmans KP, Read AF, Reece SE (2012) Virulence, drug sensitivity and transmission success in the rodent malaria Plasmodium Chabaudi. Proc Biol Sci 279:4677–4685. https://doi.org/10.1098/rspb.2012.1792
Silva RAMS, Arosemena NAE, Herrera HM, Sahib CA, Ferreira MSJ (1995) Outbreak of trypanosomosis due to Trypanosoma evansi in horses of pantanal Mato-grossense, Brazil. Vet Parasitol 60:167–171. https://doi.org/10.1016/0304-4017(94)00757-4
Taylor K, Authie EML (2004) Pathogenesis of animal trypanosomosis. In: Maudin I, Holmes PH, Miles MA (eds) The trypanosomiasis. CAB International, UK, pp 331–353
Tekle T, Terefe G, Cherenet T, Ashenafi H, Akoda KG, Teko-Agbo A, van den Abbeele J, Gari G, Clausen P-H, Hoppenheit A, Mattioli RC, Peter R, Marcotty T, Cecchi G, Delespaux V (2018) Aberrant use and poor quality of trypanocides: a risk for drug resistance in south western Ethiopia. BMC Vet Res 14:4. https://doi.org/10.1186/s12917-017-1327-6
Tesfaye B, Getachew A, Hagos A, Yacob HT (2012) Comparative study on the pathogenic effects of Diminazine aceturate sensitive and resistant isolates of Trypanosoma congolense in goats. Ethiop Vet J 16(1):59–69. https://doi.org/10.4314/evj.v16i1.5
Thuita JK, Kagira JM, Mwangangi D, Matovu E, Turner CM, Masiga D (2008) Trypanosoma brucei rhodesiense transmitted by a single tsetse fly bite in vervet monkeys as a model of human African trypanosomiasis. PLoS Negl Trop Dis 2(5):e238. https://doi.org/10.1371/journal.pntd.0000238
Funding
This study was supported by the Nigerian Tertiary Education Trust Fund (TETFUND) through the TETFUND Institution Based Research (IBR) intervention (TETFUND/ DESS/UNI/NSUKKA/2018/RP/VOL.1).
Author information
Authors and Affiliations
Contributions
RCE, IOE and CFO contributed to the study design and conception; RCE secured funding; CFO, MIO, DCA, AO and IOE performed the experiment; CFO conducted the statistical analysis of the data and wrote the first draft of the manuscript; RCE, IOE and CFO reviewed and edited the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Valid ethical clearance (FVM-UNN-IACUC-2019–0922) was gotten from the University of Nigeria Faculty of Veterinary Medicine Institutional Animal Care and Use Committee. More so, the University of Nigeria, national and international guidelines for the ethical care and use of animals were fully observed.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Handling Editor: Una Ryan
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obi, C.F., Okpala, M.I., Anyogu, D.C. et al. Comparative pathogenicity of drug-resistant and drug-sensitive Trypanosoma brucei and Trypanosoma congolense infections in Nigerian local dogs. Parasitol Res 122, 49–60 (2023). https://doi.org/10.1007/s00436-022-07688-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-022-07688-0