Abstract
Leishmaniasis is a neglected disease that affects millions of people, mostly in developing countries. Although this disease has a high impact on public health, there are few drug options to treat the different leishmaniasis forms. Additionally, these current therapies have various adverse effects, including gastrointestinal disturbances, headache, pancreatitis, and hepatotoxicity. Thus, it is essential to develop new drug prototypes to treat leishmaniasis. Accordingly, the present study aimed to evaluate the leishmanicidal activity of Morita-Baylis–Hillman adducts and their O-acetylates, carboxylic acid derivatives, and acid and ester derivatives of 2-methyl-phenylpropanoids against Leishmania chagasi. Initially, we evaluated the cytotoxicity of 16 derivatives (1-16G) against J774A.1 macrophages. Eight derivatives (2G, 4G, 5G, 7G, 9G, 10G, 13G, and 15G) showed no cytotoxicity at up to the maximum concentration tested (100 μM). When evaluated for antileishmanial effect against promastigote forms, 1G, 6G, 8G, 10G, 11G, 13G, 14G, 15G, and 16G displayed significant toxicity compared to the control (0.1% DMSO). Additionally, the compounds 1G, 5G, 7G, 9G, 11G, 13G, 14G, and 16G reduced macrophage infection by amastigotes. Thus, we conclude that these derivatives have antileishmanial effects, particularly 1G, which showed activity against promastigotes and amastigotes, and low toxicity against macrophages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neglected tropical diseases (NTDs) are a group of communicable diseases that affect 149 countries, mainly the poorest ones, prevailing in tropical and subtropical regions and causing social and economic damage. Despite reaching humans for centuries, they were considered neglected due to lack of funding, research, and concern of health authorities during the twentieth century (Engelman et al. 2016; WHO 2015).
Leishmaniasis, one of 17 neglected diseases, is endemic in 98 countries. Its various forms cause deep and permanent scars or destroy the mucous membranes of the nose, mouth, and throat. In the most severe form, if untreated, it can lead to death rapidly, as it mainly affects the liver and spleen (WHO 2013, 2015). This complex of diseases is classified as tegumentary or visceral and caused by different species of the genus Leishmania, obligate intracellular parasites. They are among the ten priority endemics of the World Health Organization (WHO) because of their significant impact on public health. It is estimated that around 20 to 40 thousand people die each year from leishmaniasis and that 400 million are at risk of contracting the disease (Alvar et al. 2012); WHO 2009, 2013).
Currently, pentavalent antimonials (Sb+5) are the drugs of choice for the treatment of all forms of leishmaniasis, followed by amphotericin B and pentamidine salts. As a second choice, if this treatment shows no response or if it cannot be applied, miltefosine and amphotericin B deoxycholate (antifungal antibiotic) are indicated. All these therapies have a high cost, adverse effects, and varied therapeutic response, which limits the patients’ access to quality treatment. Currently, there is no approved vaccine available for humans (Sabbaga Amato et al. 2007; MacHado et al. 2015; WHO 2010).
The search for new drugs of natural or synthetic origin is a challenge for researchers nowadays (Neri et al. 2020; Ghodsian et al. 2020; Hzounda Fokou et al. 2021; Maaroufi et al. 2021). In this context, Morita-Baylis–Hillman adducts (MBHA) and their derivatives have been studied as promising antiparasitic drugs, showing activity against promastigote forms of Leishmania brasiliensis, L. chagasi, and L. donovani. (Barbosa et al. 2011; Lima-Junior and Vasconcellos 2012; Silva et al. 2016a, b; Xavier et al. 2016; Souza et al. 2017). Likewise, the phenylpropanoids are described in the scientific literature for their antiparasitic potential against trypanosomatids (Abreu et al. 2020; Sulistyowaty et al. 2021), including the leishmanicidal activity (Abdel-Mageed et al. 2012; Costa-Silva et al. 2015; Chauhan et al. 2019). Therefore, the hypothesis of this study is that the production and biological evaluation of MBHA of phenylpropanoids as new leishmanicidal derivatives is a promising strategy for the development of useful therapeutic alternatives for this neglected disease.
The Morita-Baylis–Hillman reaction provides polyfunctional, simple, and versatile molecules through carbon–carbon bond formation with high atom-economy. This sustainable transformation provides highly substituted small molecules, which can be used as valuable starting materials for the synthesis of natural products, heterocyclic compounds, and drugs (Das et al. 2006; Basavaiah et al. 2007; Basavaiah and Naganaboina 2018; Luna-Freire et al. 2011, 2014).
The low cost and ready availability of the reagents make the reaction advantageous and economical since all atoms are incorporated into the product. Moreover, it is considered green chemistry or a sustainable reaction, since it can be performed in aqueous media and in the absence of some solvents (Sheldon 2005).
According to WHO (2010, 2015), access to free and well-designed essential medicines is one of the ways to improve access to health for the most disadvantaged populations. Considering the exposed scenario, the search for new treatment alternatives is needed, mainly with greater effectiveness, less adverse effects, and better dosage forms. Thus, the present study aimed to evaluate the leishmanicidal activity of MBHA adducts and their O-acetylates, carboxylic acid derivatives, and acid and ester derivatives of 2-methyl-phenylpropanoids in the search for new drug prototypes, since these compounds contain chemical fragments privileged in relation to this biological activity.
Material and methods
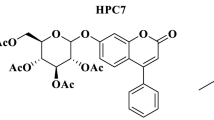
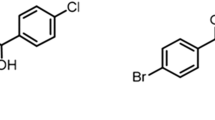
Synthesis of compounds
The compounds 1G–16G tested in this work (Fig. 1) were synthesized according to procedures described in previous works (Fig. 2) (Stork et al. 1978; Basavaiah et al. 1999; Amarante et al. 2010; Luna-Freire et al. 2011, 2014).
80% yield. Methyl 2-[(2-chloroquinolin-3-yl)(hydroxy)methyl]prop-2-enoate (1G)—FTIR (KBr, cm−1): 3537, 3216, 3062, 2992, 2955, 1702, 1619, 1490, 1138, 1033, 759. 1H NMR (250 MHz, CDCl3): δ (ppm) 3,8 (s, 3H); 5,65 (s, 1H); 6,1 (s, 1H); 6,40 (s, 1H); 7,5 (t, 1H); 7,75 (t, 1H); 7,8 (d, 1H), 8,0 (d, 1H); 8,4 (s, 1H). 13C RMN (62,5 MHz, CDCl3): δ (ppm) 52,51; 69,45; 127,40; 127,46; 127,97; 128,05; 128,37; 130,81; 132,89; 137,29; 140,42; 147,33; 149,49; 167,06.
92% yield. 2-[(2-Chloroquinolin-3-yl)(hydroxy)methyl]prop-2-enoic acid (2G)—FTIR (KBr, cm−1): 3271, 1702, 1655, 1421, 1276, 1038, 957, 760. 1H NMR (200 MHz, CD3OD): δ (ppm) 5,85 (d, 1H, J = 5,92 Hz); 6,35 (d, 1H, J = 5,90 Hz); 7,28 (dd, 1H, J = 7,85 e 15,52 Hz); 7,50 (m, 1H); 7,64 (d, 1H, J = 7,70 Hz); 7,92 (d, 1H, J = 3,01). 13C NMR (100 MHz, CD3OD): δ (ppm) 67,29; 121,20; 123,90; 126,37; 129,20; 131,60; 138,18; 139,21; 143,39; 143,74; 169,17.
83% yield. Methyl 2-[(acetyloxy)(2-chloroquinolin-3-yl)methyl]prop-2-enoate (3G)—FTIR (KBr, cm−1): 3079, 2949, 1726, 1623, 1435, 1246, 1053, 955, 750. 1H NMR (200 MHz, CDCl3): δ (ppm) 2,31 (s, 3H); 3,89 (s, 3H); 5,96 (m, 1H); 6,72 (m, 1H); 7,72 (m, 1H); 7,89 (ddd, 1H, J = 1,44; 6,96 e 8,46 Hz); 7,97 (m, 1H); 8,17 (m, 1H); 8,28 (s, 1H). 13C NMR (50 MHz, CDCl3): δ (ppm) 20,9; 52,37; 70,11; 126,93; 127,50; 127,84; 128,39; 128,60; 129,90; 131,08; 137,55; 137,66; 147,43; 149,86; 165,14; 169,16.
75% yield. Methyl (2E)-3-(2-chloroquinolin-3-yl)-2-methylprop-2-enoate (4G)—FTIR (KBr, cm−1): 3443, 2925, 2851, 1718, 1437, 1266, 1226, 1051, 750. 1H NMR (200 MHz, CDCl3): δ (ppm) 2,23 (s, 3H); 3,89 (s, 3H); 7,75 (d, 1H, J = 7,20 Hz); 7,93 (dd, 3H, J = 8,19 e 19,13 Hz); 8,19 (m, 1H); 8,28 (s, 1H). 13C NMR (50 MHz, CDCl3): δ (ppm) 52,36; 79,1; 126,75; 126,92; 127,86; 128,41; 128,58; 129,86; 131,13; 131,89; 134,24; 137,56; 138,88; 147,42; 149,88; 169,22.
95% yield. (2E)-3-(2-Chloroquinolin-3-yl)-2-methylprop-2-enoic acid (5G)—FTIR (KBr, cm−1):3476, 2961, 2924, 2871, 1690, 1624, 1268, 1056, 759. 1H NMR (200 MHz, CDCl3): δ (ppm) 2,04 (s, 3H); 8,20 (m, 1H,); 8,38 (m, 1H); 8,63 (m, 1H); 8,86 (m, 1H). 13C NMR (100 MHz, CD3OD) δ (ppm) 14,15; 128,28; 128,51; 128,81; 129,30; 129,84; 132,40; 133,79; 134,76; 140,59; 148,02; 151,14; 170,77.
81% yield. Methyl 2-[(4-fluorophenyl)(hydroxy)methyl]prop-2-enoate (6G)—FTIR (KBr, cm−1): 3452, 3003, 2954, 2901, 2848, 1713, 1604, 960, 834. 1H NMR (200 MHz, CDCl3): δ (ppm) 4,62 (s, 3H); 6,447 (s, 1H); 6,81 (s, 1H); 7,94 (t, 1H, J = 8,65 Hz); 8,26 (dd, 2H, J = 5,59 Hz, 8,36 Hz). 13C NMR (50 MHz, CDCl3): δ (ppm) 51,81; 72,08; 114,94; 115,37; 125,76; 128,24; 128,44; 137,21; 142,01; 159,76; 164,68; 166,61.
89% yield. 2-[(4-Fluorophenyl)(hydroxy)methyl]prop-2-enoic acid (7G)- FTIR (KBr, cm−1): 3358, 3878, 2547, 1689, 1605, 1511, 1235, 1028, 828. 1H NMR (200 MHz, CDCl3): δ (ppm) 6,34 (s, 1H); 6,72 (s, 1H); 7,83 (t, 2H, J = 8,38); 8,12 (m, 2H). 13C NMR (50 MHz, CDCl3): δ (ppm) 72,12; 115,21; 115,64; 128,45; 128,60; 136,58; 136,63; 141,37; 160,01; 164,9; 179,7.
78% yield. Methyl 2-[(4-chlorophenyl)(hydroxy)methyl]prop-2-enoate (8G)—FTIR (KBr, cm−1): 3359, 3102, 3018, 2959, 1718, 1635, 1437, 1275, 1037, 813, 744. 1H NMR (200 MHz CDCl3): δ (ppm) 3,71 (s, 3H); 5,5 (s, 1H); 5,83 (s, 1H); 6,33 (s, 1H), 7,30 (s, 4H). 13C NMR (50 MHz, CDCl3): δ (ppm) 52,17; 72,67; 126,43; 128,08; 128,65; 133,64; 139,89; 141,69; 166,70.
60% yield. Methyl 2-[hydroxy(4-methoxyphenyl)methyl]prop-2-enoate (9G)—FTIR (KBr, cm−1): 3358, 3001, 2952, 2833, 1717, 1512, 1259, 1023, 826, 579. 1H NMR (250 MHz, CDCl3): δ (ppm) 2,94 (d, 1H); 3,6 (s, 3H); 3,79 (s, 3H); 5,53 (d, 1H); 5,85 (s, 1H); 6,32 (s, 1H); 6,85 (d, 2H); 7,29 (d, 2H). 13C NMR (62,5 MHz, CDCl3): δ (ppm) 52,10; 55,45; 72,96; 114,03; 125,80; 128,09; 133,66; 142,38; 159,43; 166,99.
92% yield. 2-[Hydroxy(4-methoxyphenyl)methyl]prop-2-enoic acid (10G)—FTIR (KBr, cm−1): 3465, 2959, 2838, 1700, 1609, 1513, 1252, 1175, 1032, 829, 580. 1H NMR (450 MHz, MeOD): δ (ppm) 3,73(s, 3H), 5,08 (s, 1H); 5,84 (s, 1H), 6,27 (s, 1H); 6,84 (d, 2H, J = 9,5); 7,22 (d, 2H, J = 9,5). 13C NMR (112,5 MHz, MeOD): δ (ppm) 55,67, 81,76; 114,59; 130,00; 132,98; 136,63; 143,20; 145,91; 160,7; 173,42.
77% yield. Methyl 2-[(acetyloxy)(4-methoxyphenyl)methyl]prop-2-enoate (11G)—FTIR (KBr, cm−1): 3461, 3008, 2954, 2839, 1739, 1611, 1514, 1230, 1030, 828, 563. 1H NMR (200 MHz, CDCl3): δ (ppm) 2,71 (s, 3H); 4,32 (s, 3H); 4,41 (s, 3H); 6,50 (s, 1H); 7,00 (s, 1H); 7,49 (d, 2H, J = 8,73 Hz); 7,93 (d, 2H, J = 8,68 Hz). 13C NMR (50 MHz, CDCl3): δ (ppm) 21,25; 52,09; 55,34; 72,95; 113,03; 125,23; 129,27; 129,88; 139,79; 159,71; 165,56; 169,59.
77% yield. Methyl 2-[hydroxy(3,4,5-trimethoxyphenyl)methyl]prop-2-enoate (12G)—FTIR (KBr, cm−1): 3491, 2997, 2943, 2839, 1716, 1126, 1003, 838, 683. 1H NMR (250 MHz, CDCl3): δ (ppm) 3,14 (s, 1H); 3,74 (s, 3H); 3,83 (s, 9H); 5,50 (s, 1H); 5,82 (s, 1H); 6,32 (s, 1H); 6,58 (s, 2H). 13C NMR (62,5 MHz, CDCl3): δ (ppm) 52,14; 56,19; 60,89; 73,31; 103,69; 126,29; 136,98; 137,55; 141,97; 153,31; 166,97.
71% yield. 2-[Hydroxy(3,4,5-trimethoxyphenyl)methyl]prop-2-enoic acid (13G)—FTIV (KBr, cm−1): 3458; 3371; 2974; 2941; 2841; 2561; 1709; 822; 685; 667. 1H NMR (250 MHz, CDCl3): δ (ppm) 3,83 (s, 9H); 5,50 (s, 1H); 5,90 (s, 1H); 6,45 (s, 1H); 6,57 (s, 2H). 13C NMR (62,5 MHz, CDCl3): δ (ppm) 56,24; 60,95; 73,01; 103,81; 128,44; 136,73; 141,57; 153,37; 170,75.
90% yield. Methyl 2-[hydroxy(4-nitrophenyl)methyl]prop-2-enoate (14G)—FTIR (KBr, cm−1): 3511, 3104, 2958, 1708, 1529, 1348, 1146, 1044, 984, 751. 1H NMR (250 MHz, CDCl3): δ (ppm) 3,29 (d, 1H); 3,75 (s, 3H); 5,65 (d, 1H); 5,87 (s, 1H); 6,40 (s, 1H); 7,58 (d, 2H); 8,25 (d, 2H); 13C NMR (62,5 MHz, CDCl3): δ (ppm) 52,20; 72,8; 123,6; 127,3; 140,9; 147,4; 148,6; 166,4.
98% yield. 2-[Hydroxy(4-nitrophenyl)methyl]prop-2-enoic acid (15G)—FTIR (KBr, cm−1): 3568, 3456, 2917, 2848, 1690, 1513, 1350, 1038, 752. 1H NMR (200 MHz, CDCl3): δ (ppm) 5,53 (s,1H); 5,84 (s, 1H); 6,30 (s, 1H); 7,5 (d, 2H); 8,04 (d, 2H). 13C NMR (50 MHz, CDCl3): δ (ppm) 71,72; 123,30; 126,52; 127,5; 141,91; 147,03; 149,73; 167,76.
85% yield. Methyl 2-[(3,4-dichlorophenyl)(hydroxy)methyl]prop-2-enoate (16G)—FTIR (KBr, cm−1):1432, 2952, 2867, 1719, 1629, 1469, 1151, 1031, 961, 820. 1H NMR (200 MHz, CDCl3): δ (ppm) 4,63 (s, 3H); 6,38 (s, 1H); 6,78 (s, 1H); 8,10 (d, 1H, J = 8,19 Hz); 8,32 (m, 2H). 13C NMR (50 MHz, CDCl3): δ (ppm) 52,17; 71,82; 128,04; 128,66; 128,64; 130,30; 131,63; 132,40; 141,60; 141,73; 166,40.
In vitro pharmacological tests
Promastigote culture
The parasite of the Gonçalo Moniz—Fiocruz—BA Research Center, provided by Dr. Valéria de Matos Borges (MCAN/BR/89/BA262), was used to culture the L. chagasi promastigotes. These promastigotes were maintained in vitro in Schneider’s medium supplemented with 10% fetal bovine serum (FBS) and 2% male human urine at 27 °C in a biochemical oxygen demand (BOD) incubator. For the experiments, the parasites were placed in Falcon tubes and centrifuged at 3500 rpm for 10 min. The supernatant was then discarded, and the pellet was resuspended in Schneider’s medium. The parasites were then counted in a Neubauer chamber for plating and thus the subsequent assays.
Macrophage culture
J774.A1 macrophages were maintained in culture flasks containing 10 mL of RPMI medium supplemented with 10% FBS, 2 mM L-glutamine, non-essential amino acids, and pyruvate. For the experiments, the cells were counted, adjusted in RPMI medium supplemented with 10% FBS, and then plated on a culture dish.
Macrophage viability assay
For the study of cell viability of macrophages exposed to acyloxymethyl derivatives, we performed the MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) reduction assay (Mosmann 1983; Hussain et al. 1993). J774A.1 macrophages were seeded in 96-well plates for 1 h in (5 × 104/well) and exposed to different concentrations of the diluted test compounds in supplemented RPMI medium (0.1, 1, 10, and 100 μM) for 24 h in a 37 °C incubator with a humid 5% CO2 atmosphere. Control wells contained cells with only culture medium or cells exposed to the diluent (0.1% DMSO). After incubation, the supernatant was discarded and 100 μL of the MTT solution (5 mg/10 mL) was then added. The plates were incubated again for 1 h in a 37 °C incubator with a 5% CO2 atmosphere. After removing the supernatant, 100 μL of DMSO was added and the plate read with a spectrophotometer at 550 nm. The cell viability of the wells treated with the synthesized compounds was compared to that of the death standard in the control cultures.
Promastigote viability assay
Promastigote forms of L. chagasi at a density of 1 × 106 parasites/well in a volume of 100 μL were grown in triplicate in 96-well plates using Scnheider’s medium supplemented with 10% FBS, 2 mM L-glutamine, and 2% human urine. Different concentrations (0.1, 1, 10, and 100 μM) of the derivatives and controls (pentamidine, glucantime, RPMI medium, and 0.1% DMSO) were added to the wells containing the promastigote forms up to a final volume of 200 μL. The plate was incubated in a BOD incubator at 27 °C for 48 h. Afterwards, 20 μL of MTT solution was added to the wells, and the plates were placed in a CO2 incubator for 2 h. The MTT solution was then removed, and isopropyl alcohol was added to the wells to dissolve the formazan product. The plates were then read in a spectrophotometer at 550 nm. Cell viability of the wells treated with the synthesized compounds was compared to the death standard obtained in the control cultures.
Macrophage infection with L. chagasi assay
J774.A1 macrophages were seeded at a density of 5 × 104 cells/well in 24-well plates with coverslips for 1 h with supplemented RPMI medium. Macrophages were incubated overnight and subsequently infected with L. chagasi promastigotes, at a proportion of 10 parasites:1 macrophage. The plate was incubated for 6 h at 37 °C in a humid 5% CO2 atmosphere. Six hours after infection, the macrophages were washed with phosphate-buffered saline (PBS, pH 7.2), to remove the non-internalized parasites. Macrophages were cultured with RPMI supplemented with 10% FBS, 2 mM L-glutamine, 2 mM non-essential amino acids, and 2 mM sodium pyruvate, in the presence or absence of derivatives at a concentration of 10 μM, and were kept in a 37 °C incubator with a humid 5% CO2 atmosphere for 24 h. Afterwards, the wells containing the coverslips were washed with PBS, and the cells were fixed with methanol, stained with May-Grünwald-Giemsa, and mounted on slides. The number of infected macrophages and the number of amastigotes in 100 macrophages were evaluated using a light microscope with 100 × oil-immersion objective (Nunes et al. 2005).
Statistical analysis
All data are expressed as the mean ± SEM and were analyzed by GraphPad Prism 8.0 software using one-way analysis of variance (ANOVA) followed by Dunnett’s test. Differences were considered statistically significant when p < 0.05.
Results and discussion
Leishmaniasis is a complex of diseases in which the cells of the mononuclear phagocytic system serve as host and replication site for the parasite as well. The parasite in turn resists lysis by the lysosomes and resides mainly in macrophages in the spleen and liver. It is important to note that the use of pentavalent antimonials is the first choice for the treatment of leishmaniasis in Brazil. However, they have a high cost and are hepatotoxic and nephrotoxic as well, which justifies the search for new therapeutic options (Ayres et al. 2007; Jain and Jain 2013).
The Morita-Baylis–Hillman reaction has proved to be effective, is low cost, and provides highly functional derivatives. Morita-Baylis–Hillman derivatives have been studied since 1999 from a pharmacological point of view. They have a range of activities, including antifungal, antimalarial, antineoplastic, molluscicide, antileishmanial, and antichagasic action (Lima-Junior and Vasconcellos 2012).
First, the compounds synthesized were evaluated for their effect on cell viability of J774A.1 macrophages using the MTT assay. The results showed that only the derivatives 2G, 4G, 5G, 7G, 9G, 10G, 13G, and 15G were not cytotoxic at up to the maximum concentration tested (100 μM). The other compounds (1G, 3G, 6G, 8G, 11G, 12G, 14G, and 16G) were cytotoxic when compared to the control (0.1% DMSO). When cytotoxicity was determined at a concentration of 10 μM, only 9G, 11G, 14G, and 16G showed a significant cytotoxic effect against macrophages (Table 1). As expected, 0.1% DMSO had no deleterious effect when compared to the negative control (RPMI culture medium). A similar assay was used by Silva et al. 2011 in evaluating the cytotoxicity of MBHA in peritoneal murine macrophages.
After determination of cytotoxicity in macrophages, the viability of promastigote forms treated with the derivatives and controls was evaluated by the MTT reduction assay. The results showed that the 1G, 6G, 8G, 10G, 11G, 13G, 14G, 15G, and 16G derivatives had a significant cytotoxic effect compared to the control (0.1% DMSO) (Table 2).
The direct leishmanicidal activity of MBHA has been previously described. Barbosa et al. (2011) evaluated the in vitro leishmanicidal activity of MBHA compounds in promastigotes of L. chagasi and L. amazonesis, using the molecular hybridization strategy, but without evaluating cytotoxicity in macrophages. Additionally, it was previously observed that others MBHA had an antileishmanial effect against promastigote forms of L. chagasi after 72 h of treatment (Junior et al. 2010).
After cytotoxicity evaluation in macrophages and promastigote forms, the derivatives were evaluated for leishmanicidal activity in amastigote forms of L. chagasi at a concentration of 10 μM. The results obtained demonstrated that the test compounds 1G, 5G, 7G, 9G, 11G, 10G, 13G, 14G, and 16G caused a significant reduction in the number of amastigotes in 100 macrophages. On the other hand, the derivatives 2G, 3G, 4G, 6G, 8G, 12G, and 15G did not display leishmanicidal activity against intracellular parasites (Fig. 3).
Sandes et al. 2014 evaluated the effect of an MBHA on epimastigote forms of Trypanosoma cruzi. The group found that the 3-hydroxy-2-methylene-3-(4-nitrophenylpropanenitrile) adduct induced parasite cell death by necrosis, in a mitochondria-dependent manner. A range of therapeutic targets for the treatment of leishmaniasis has been emerging (Sundar and Singh 2018; Raj et al. 2020). The exact mechanism of action MBHA in Leishmania targets remains to be elucidated. However, it is possible that MBHA acts inhibiting Leishmania proteases (da Silva et al. 2016a, b), which are virulence factors related to the pathogenesis of this protozoan (Machado et al. 2019).
The compounds 1G, 11G, 13G, 14G, and 16G present antileishmanial activity against both amastigotes and promastigotes forms. However, 11G, 14G, and 15G derivatives showed significant cytotoxicity against macrophages, being 1G and 13G derivatives safer for mammalian cells based on this preliminary assay. Thus, in molecular prospecting for leishmanicidal compounds, this study demonstrates that derivative 1G is the most promising for drug development, since the compound was highly active against promastigotes, with IC50 lower than standard drugs and 13G derivative, and amastigotes of L. chagasi. In addition, it showed low toxicity against macrophages.
Considering that MBHA compounds are easy to synthesize and readily available, their use becomes an advantage when compared to the currently available drugs, since leishmaniosis is a neglected diseases and affects less fortunate populations (WHO 2010, 2015).
Conclusion
On the basis of the results obtained, it can be concluded that some MBHA compounds, their O-acetylates, carboxylic acid derivatives, and acid and ester derivatives of 2-methyl-phenylpropanoids possess leishmanicidal activity in vitro against promastigotes and amastigotes of L. chagasi. Derivative 1G, which was active against promastigotes and amastigotes, showed low toxicity against the macrophage cell line J774A.1. Thus, it is a strong candidate for further pharmacological studies aimed at the treatment of leishmaniasis.
References
Abdel-Mageed WM, Backheet EY, Khalifa AA et al (2012) Antiparasitic antioxidant phenylpropanoids and iridoid glycosides from Tecoma mollis. Fitoterapia 83:500–507. https://doi.org/10.1016/j.fitote.2011.12.025
Abreu LS, do Nascimento YM, do Espirito-Santo RF et al (2020) Phenylpropanoids from Croton velutinus with cytotoxic, trypanocidal and anti-inflammatory activities. Fitoterapia 145:104632. https://doi.org/10.1016/j.fitote.2020.104632
Alvar J, Vélez ID, Bern C et al (2012) Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 7:e35671. https://doi.org/10.1371/journal.pone.0035671
Amarante GW, Cavallaro M, Coelho F (2010) Highly diastereoselective total synthesis of the anti-tumoral agent (±)-Spisulosine (ES285) from a Morita-Baylis-Hillman adduct. Tetrahedron Lett 51:2597–2599. https://doi.org/10.1016/j.tetlet.2010.02.169
Ayres DC, Marcucci MC, Giorgio S (2007) Effects of Brazilian propolis on Leishmania amazonensis. Mem Inst Oswaldo Cruz 102:215–220. https://doi.org/10.1590/S0074-02762007005000020
Barbosa TP, Sousa SCO, Amorim FM et al (2011) Design, synthesis and antileishmanial in vitro activity of new series of chalcones-like compounds: a molecular hybridization approach. Bioorganic Med Chem 19:4250–4256. https://doi.org/10.1016/j.bmc.2011.05.055
Basavaiah D, Krishnamacharyulu M, Hyma RS et al (1999) A facile one-pot conversion of acetates of the Baylis-Hillman adducts to [E]-α-methylcinnamic acids. J Org Chem 64:1197–1200. https://doi.org/10.1021/jo981761b
Basavaiah D, Rao KV, Reddy RJ (2007) The Baylis-Hillman reaction: a novel source of attraction, opportunities, and challenges in synthetic chemistry. Chem Soc Rev 36:1581–1588. https://doi.org/10.1039/b613741p
Basavaiah D, Naganaboina RT (2018) The Baylis-Hillman reaction: a new continent in organic chemistry - our philosophy, vision and over three decades of research. New J Chem 42:14036–14066
Chauhan K, Kaur G, Kaur S (2019) Evaluation of antileishmanial efficacy of Salidroside against the SSG-sensitive and resistant strain of Leishmania donovani. Parasitol Int 72:101928. https://doi.org/10.1016/j.parint.2019.101928
Da Costa-Silva TA, Grecco SS, De Sousa FS et al (2015) Immunomodulatory and antileishmanial activity of phenylpropanoid dimers isolated from Nectandra leucantha. J Nat Prod 78:653–657. https://doi.org/10.1021/np500809a
da Silva WAV, Rodrigues DC, de Oliveira RG et al (2016a) Synthesis and activity of novel homodimers of Morita–Baylis–Hillman adducts against Leishmania donovani: a twin drug approach. Bioorganic Med Chem Lett 26:4523–4526. https://doi.org/10.1016/j.bmcl.2016.07.022
Das B, Banerjee J, Chowdhury N, Majhi A (2006) Synthetic applications of Baylis-Hillman chemistry: an efficient and solely stereoselective synthesis of (E)-α-methylcinnamic acids and potent hypolipidemic agent LK-903 from unmodified Baylis-Hillman adducts. Chem Pharm Bull 54:1725–1727. https://doi.org/10.1248/cpb.54.1725
Engelman D, Fuller LC, Solomon AW et al (2016) Opportunities for integrated control of neglected tropical diseases that affect the skin. Trends Parasitol 32:843–854. https://doi.org/10.1016/j.pt.2016.08.005
Ghodsian S, Taghipour N, Deravi N et al (2020) Recent researches in effective antileishmanial herbal compounds: narrative review. Parasitol Res 119:3929–3946. https://doi.org/10.1007/s00436-020-06787-0
Hussain RF, Nouri AME, Oliver RTD (1993) A new approach for measurement of cytotoxicity using colorimetric assay. J Immunol Methods 160:89–96. https://doi.org/10.1016/0022-1759(93)90012-V
Hzounda Fokou JB, Dize D, Etame Loe GM et al (2021) Anti-leishmanial and anti-trypanosomal natural products from endophytes. Parasitol Res 1–12. https://doi.org/10.1007/s00436-020-07035-1
Jain K, Jain NK (2013) Novel therapeutic strategies for treatment of visceral leishmaniasis. Drug Discov Today 18:1272–1281. https://doi.org/10.1016/j.drudis.2013.08.005
Junior CGL, De Assis PAC, Silva FPL et al (2010) Efficient synthesis of 16 aromatic Morita-Baylis-Hillman adducts: biological evaluation on Leishmania amazonensis and Leishmania chagasi. Bioorg Chem 38:279–284. https://doi.org/10.1016/j.bioorg.2010.08.002
Lima-Junior CG, Vasconcellos MLAA (2012) Morita-Baylis-Hillman adducts: biological activities and potentialities to the discovery of new cheaper drugs. Bioorganic Med Chem 20:3954–3971. https://doi.org/10.1016/j.bmc.2012.04.061
Luna-Freire KR, Scaramal JPS, Resende JALC et al (2014) An asymmetric substrate-controlled Morita-Baylis-Hillman reaction as approach for the synthesis of pyrrolizidinones and pyrrolizidines. Tetrahedron 70:3319–3326. https://doi.org/10.1016/j.tet.2013.10.050
Luna-Freire KR, Tormena CF, Coelho F (2011) Heck reaction on morita-baylis-hillman adducts: diastereoselective synthesis of pyrrolizidinones and pyrrolizidines. Synlett 2011:2059–2063. https://doi.org/10.1055/s-0030-1261161
Maaroufi Z, Cojean S, Loiseau PM et al (2021) In vitro antileishmanial potentialities of essential oils from Citrus limon and Pistacia lentiscus harvested in Tunisia. Parasitol Res 1–15. https://doi.org/10.1007/s00436-020-06952-5
Machado P, Carneiro M, Sousa-Batista A et al (2019) Leishmanicidal therapy targeted to parasite proteases. Life Sci 219:163–181. https://doi.org/10.1016/J.LFS.2019.01.015
MacHado PRL, Rosa MEA, Guimarães LH et al (2015) Treatment of disseminated leishmaniasis with liposomal amphotericin B. Clin Infect Dis 61:945–949. https://doi.org/10.1093/cid/civ416
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63. https://doi.org/10.1016/0022-1759(83)90303-4
Neri FSM, Júnior DBC, Froes TQ et al (2020) Antileishmanial activity evaluation of thiazolidine-2,4-dione against Leishmania infantum and Leishmania braziliensis. Parasitol Res 119:2263–2274. https://doi.org/10.1007/s00436-020-06706-3
Nunes MP, Cysne-Finkelstein L, Monteiro BC et al (2005) CD40 signaling induces reciprocal outcomes in Leishmania-infected macrophages; roles of host genotype and cytokine milieu. Microbes Infect 7:78–85. https://doi.org/10.1016/j.micinf.2004.08.022
Raj S, Sasidharan S, Balaji S, Saudagar P (2020) An overview of biochemically characterized drug targets in metabolic pathways of Leishmania parasite. Parasitol Res 119:2025–2037. https://doi.org/10.1007/S00436-020-06736-X
Sabbaga Amato V, Francisco Tuon F, Machado Siqueira A et al (2007) Treatment of mucosal leishmaniasis in Latin America: systematic review. Am J Trop Med Hyg 77:266–274
Sandes JM, Fontes A, Regis-da-Silva CG et al (2014) Trypanosoma cruzi cell death induced by the Morita-Baylis-Hillman adduct 3-hydroxy-2-methylene-3-(4-nitrophenylpropanenitrile). PLoS ONE 9:e93936. https://doi.org/10.1371/journal.pone.0093936
Sheldon RA (2005) Green solvents for sustainable organic synthesis: state of the art. Green Chem 7:267–278. https://doi.org/10.1039/b418069k
Silva FPL, De Assis PAC, Junior CGL et al (2011) Synthesis, evaluation against Leishmania amazonensis and cytotoxicity assays in macrophages of sixteen new congeners Morita-Baylis-Hillman adducts. Eur J Med Chem 46:4295–4301. https://doi.org/10.1016/j.ejmech.2011.06.036
Silva WAV, Rodrigues DC, Oliveira RG et al (2016b) Synthesis and activity of novel homodimers of Morita–Baylis–Hillman adducts against Leishmania donovani: a twin drug approach. Bioorg Med Chem Lett 26:4523–4526. https://doi.org/10.1016/j.bmcl.2016.07.022
Souza SCO, Rocha JC, Keesen TSL et al (2017) Synthesis of 16 new hybrids from tetrahydropyrans derivatives and Morita-Baylis-Hillman adducts: in vitro screening against Leishmania donovani. Molecules 22:207/1-207/14
Stork G, Takahashi T, Kawamoto I, Suzuki T (1978) Total synthesis of prostaglandin F2α by chirality transfer from D-glucose1,2. J Am Chem Soc 100:8272–8273. https://doi.org/10.1021/ja00494a045
Sulistyowaty MI, Uyen NH, Suganuma K et al (2021) Six new phenylpropanoid derivatives from chemically converted extract of alpinia galanga (L.) and their antiparasitic activities. Molecules 26:1756. https://doi.org/10.3390/molecules26061756
Sundar S, Singh B (2018) Emerging therapeutic targets for treatment of leishmaniasis. Expert Opin Ther Targets 22:467–486
WHO UNICEF/UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases & World Health Organization (2009). Research to support the elimination of visceral leishmaniasis: annual report 2008. World Health Organization. https://apps.who.int/iris/handle/10665/70112
WHO Expert Committee on the Control of the Leishmaniases & World Health Organization (2010). Control of the leishmaniases: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010. World Health Organization. https://apps.who.int/iris/handle/10665/44412
WHO/Department of control of neglected tropical diseases Sustaining the drive to overcome the global impact of neglected tropical diseases: Second WHO report on neglected tropical diseases. 2013. https://www.who.int/neglected_diseases/9789241564540/en/
WHO Investing to overcome the global impact of neglected tropical diseases: third WHO report on neglected diseases 2015. World Health Organization. https://apps.who.int/iris/handle/10665/152781
Xavier FJS, Rodrigues KAF, Oliveira RG et al (2016) Synthesis and in vitro anti Leishmania amazonenses biological screening of Morita-Baylis-Hillman adducts prepared from eugenol, thymol and carvacrol. Molecules 21:1483/1-1483/12
Acknowledgements
Dr. A. Leyva (USA) helped with English editing of the manuscript.
Funding
The authors thank the Universidade Federal de Alagoas (UFAL), the foundations Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), and the Instituto Nacional de Ciência e Tecnologia em Fármacos e Medicamentos (INCT-INOFAR) for funding this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Section Editor: Nawal Hijjawi
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vieira, A.C.S., da Silva Santos, M., Leite, A.B. et al. Leishmanicidal activity of Morita-Baylis–Hillman adducts. Parasitol Res 121, 751–762 (2022). https://doi.org/10.1007/s00436-021-07421-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-021-07421-3