Abstract
Background
Tetraspanin KAI1/CD82, a tumor metastasis suppressor, has emerged as a promising molecular target for the management of metastatic disease. However, the peptide mimicking small extracellular ring domain (EC1) of CD82 has not been fully investigated for the function of inhibiting cell migration in vitro and tumor metastasis in vivo.
Methods
Different cancer cells were treated with EC1 mimic peptide in order to detect migration and invasion by the healing assay and transwell. Cell aggregation and adhesion assays were used to investigate the function of homotypic cell–cell aggregation and adhesion to tissue culture plates. Then, we established syngeneic and xenograft animal models to assess the metastasis inhibitory effect of EC1 mimic peptide in vivo.
Results
In vitro studies, the EC1 mimic peptide had been showed to promote homotypic cell–cell aggregation, suppress cell migration, invasion and adherence in multiple tumor cell types. In vivo metastasis assays, the EC1 mimic peptide could strongly inhibit the pulmonary metastasis of LCC in syngeneic mice model and SW620 and H1299 in xenograft mice model.
Conclusion
This novel finding will improve our understanding of the mechanism by which CD82 inhibits metastasis, and suggests that EC1 mimic peptide may be a promising candidate for developing anti-metastasis drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastasis is a complex, multi-step process which involves many molecular components, including adhesion molecules, cytoskeletal proteins, chemokines, protein kinases, signaling molecules and transcription factors (Robinson et al. 2004; Brabletz et al. 2013). Among these, a specific class of proteins that function as negative regulators of cancer metastasis, which frequently downregulated in many types of human cancers, is defined as tumor metastasis suppressors by their capacity to block metastasis without altering primary tumor growth (Kauffman et al. 2003; Yoshida et al. 2000). Thus far, more than 20 metastasis suppressor genes have been identified (Rinker-Schaeffer et al. 2006; Stafford et al. 2008). Metastasis suppressors may block metastatic process at different steps in the metastatic cascade. Reactivation of metastasis suppressor in metastatic tumor cell lines may reduce cancer invasion and metastasis. Therefore, the tumor metastasis suppressors have been considered as the potential targets for controlling tumor metastasis in clinic(Berger et al. 2005; Steeg et al. 2003).
In the past decades, several strategies have been developed to reactivate the metastasis suppressor functions. These strategies can be classified into three categories, including re-expression of metastasis suppressor gene by induction of the endogenous locus, restoration of gene function by liposome or viral-mediated gene therapy, direct administration of the productions of metastasis suppressor gene and targeting essential downstream pathways that are activated by loss of suppressor function (Smith and Theodorescu 2009). However, to date, none of the anti-metastasis agents targeting metastasis suppressor can be used in clinical metastasis therapy (Shoushtari et al. 2011).
Among the metastasis suppressors, KAI1/CD82 is one of the most extensively described metastasis suppressors. KAI1/CD82 was first identified as a prostate cancer metastasis suppressor through genetic screening (Dong et al. 1995). In the past two decades, the structure and function of CD82 in cancer metastasis had been well established (Tsai and Weissman 2011; Malik et al. 2009). Like other metastasis suppressors, the strategies, including gene therapy techniques or re-expression of endogenous KAI1 induced by etoposide, or genistein had been used to restore the CD82 function. However, to date, none of these strategies are yet in clinical routine application. CD82, as a transmembrane protein, cannot be directly applied to the clinic with the current drug delivery technology. However, the extracellular domain of KAI1/CD82 should be a key structure for CD82’s function and a potential target structure for the clinical interference with tumor metastasis. Thus, we focused primarily on the roles of extracellular domains of CD82. In our previous works, we found that the EC1 amino acid sequence mimic peptide of CD82 (CD82EC1-mP) could inhibit integrin-mediated tumor cell adhesion to extracellular matrix molecule (Luan et al. 2018). In this paper, we further studied the effects of CD82EC1-mP on the invasive behavior of cancer cells in vitro and tumor metastasis in vivo. To establish the generality of the conclusions, functional and biochemical studies were carried out using several different types of cell lines.
Materials and methods
Cell culture
SW620 (L-15 medium, Macgene), MDA-MB-231, LLC and Hepg2 (DMEM medium, Gibco), PC3 and H1299 (RPMI 1640 medium, Gibco), all the cell lines were cultured in a specific medium supplied with 10% fetal bovine serum (Gibco), at 37 °C, 5% CO2.
Reagents
CD82EC1-mP used in this paper was synthesized by Xinghao biological co. Ltd. (Wuhan,China) according to EC1 amino acid sequence of CD82 (CD82Asp37-Tyr58) and modified by addition of 4 lysine residues at the N terminal.
Amino acid sequence of CD82EC1-mP is KKKKDKSSFISVLQTSSSLRMGAY.
Cell migration assay
Cell motility was determined by wound healing assay. SW620, MDA-MB-231, PC3 and H1299 cells were seeded in 12-well plates in a specific medium supplemented with 10% fetal bovine serum. When the cells were grown to 85–90% confluence, the cell monolayers were then carefully scratched using 200 μl sterile pipette tips. Cell debris was removed by washing with PBS. The wounded monolayers were maintained in medium with increased doses of CD82EC1-mP for an additional 72 h and photographs were taken under an inverted light microscope. The effects of CD82EC1-mP on cell migration are displayed as relative healing area.
Cell invasion assay
Cell invasion was determined by transwell analysis. SW620, MDA-MB- 231, PC3 and H1299 cells (1 × 104) suspended in 100 μl L15 medium with increased doses of CD82EC1-mP and plated on the upper side of a 0.45 μm polycarbonate membrane separating two chambers of transwell culture plates (Corning) and 600 μl of 10% FBS medium were placed in the bottom chamber. After incubation 24 h at 37 ℃ in 5% CO2, the cells on the top membrane surface were scraped using a cotton swab and the cells that migrated to the bottom side of the membrane were fixed and stained with 0.1% crystal violet (Beyotime). Photographs were taken and stained cells were counted under a microscope. The data were expressed as the average number of cells from five randomly selected fields.
Cell aggregation assays
SW620, MDA-MB-231, PC3, H1299 and LLC cells were plated in 12-well plates and incubated in a specific culture medium with or without (control) 50 μg/ml of CD82EC1-mP for 12 h. Cell aggregation was photographed under an inverted light microscope (Olympus).
Cell adhesion assays
SW620, MDA-MB-231, PC3, H1299 and Hpeg2 cells were plated in 12-well plates and incubated in a specific medium supplemented with 10% fetal bovine serum (Gibco) and with or without (control) 50 μg/ml of CD82EC1-mP for 24 h. Unattached cells were removed by two washes with a culture medium and photographs were taken under an inverted light microscope.
Experimental metastasis assay
Both syngeneic and xenograft animal models have been employed to assess the in vivo effects of CD82EC1-mP.
First, mouse lung cancer LLC cell syngeneic mice model was constructed. In brief, a total of 40 ICR mice (6-week-old, 20 g) were assigned to a control group and three treatment groups (10 mice per group). For control group, the cells (1 × 106 cells in 0.1 ml PBS) were injected into each mouse through the tail vein. The treatment groups were divided into groupI, groupII and groupIII according to the time of administration of the drug. For groupI, the cells (1 × 106 cells in 0.1 ml PBS with 100 μg CD82EC1-mP) were injected into each mouse through tail vein. For groupII, first, the mice were treated with 100 μg CD82EC1-mP in 0.1 ml PBS via tail vein, 2 h later, the cells (1 × 106 cells in 0.1 ml PBS) were injected into each mouse through the tail vein. For groupIII, the mouse was injected firstly with the cells, 2 h later, the mouse were injected with 100 μg CD82EC1-mP in 0.1 ml PBS via the tail vein. After 35 days of injection, the mice were sacrificed and the metastatic foci on the lung surface were detected. Lung metastasis positive mice were defined by the formation of one or more visible metastatic nodules on the lung surface of tumor-bearing mice and numbered with “+”.
For xenograft studies, two human cancer cell lines, colon SW620 and lung H1299 were used in the experiments. The cells (1 × 106 cells in 0.1 ml PBS, with or without 100 μg CD82EC1-mP) were injected into tail vein of male nude mice (BALB/cA-nu/nu, seven per group). After 45 days of injection, the mice were sacrificed and the metastatic foci on the lung surface were detected. Experiments were conducted according to the guidelines for the ethical use of animals of Dalian Medical University under an approved protocol by the Ethics Committees of Dalian Medical University (No. AEE18014).
Statistic analysis
All experiments in vitro were performed at least three times independently. Data were analyzed by the student’s t test. Results are expressed as mean ± standard error of the mean. Statistical significance was determined. *P < 0.05, **P < 0.01, ***P < 0.001.
Results
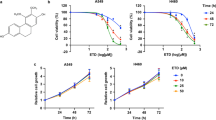
CD82EC1-mP inhibits the cancer cells migration
Cell adhesion and migration play an essential role during cancer metastasis. It is well documented that CD82 suppresses tumor metastasis primarily via regulating cell adhesion and migration (Lee et al. 2011; Hemler 2003). To investigate the role of CD82EC1-mP on the invasive behavior of cancer cells, we first tested the effect of CD82EC1-mP on the migration of cancer cells in vitro using wound healing assay analysis. The results showed that the CD82EC1-mP strongly inhibited the migration in all four cancer cell lines, including SW620, MDA-MB-231, PC3, H1299 cells. The inhibitory effect was dose-dependent. At the concentration of 60 μg/ml CD82EC1-mP, cell migration was almost completely inhibited. When the concentration of CD82EC1-mP is higher than 50, its effect no longer increases or even decreases (Fig. 1).
CD82EC1-mP suppresses cell migration. SW620, MDA-MB- 231, PC3 and H1299 cells were seeded in 12-well plates in a specific medium supplemented with 10% fetal bovine serum and treated with increased doses of CD82EC1-mP. Cell migration was examined by the scratch wound-healing assay. Photographs were taken under an inverted light microscope and the effects of CD82EC1-mP on cell migration are displayed as relative healing area
CD82EC1-mP inhibits the cancer cells invasion
Tumor cell metastasis is closely related to its invasion ability. Next, the effect of CD82EC1-mP on the invasive ability of cancer cells was determined using transwell assay. As showing in Fig. 2 the results showed that the CD82EC1-mP strongly inhibited the tumor cell invasion in all the tested cancer cell lines. The inhibitory effect was dose-dependent. At the concentration of 60 μg/ml CD82EC1-mP, When the concentration of CD82EC1-mP is higher than 50, its effect no longer increases or even decreases.
CD82EC1-mP suppresses cancer cell invasion. SW620, MDA-MB- 231, PC3 and H1299 cells were seeded in 12-well plates in a specific medium supplemented with 10% fetal bovine serum and treated with increased doses of CD82EC1-mP. Cell invasion was examined by transwell assay. Photographs were taken under an inverted light microscope. The data were expressed as the average number of cells from five randomly selected fields
CD82EC1-mP promotes the homotypic cell–cell aggregation
The first step of metastasis is the tumor cell dissociation from the primary tumor nest. In this process, tumor cells are required to loosen their homophilic cell adhesion, enabling tumor cells to escape from the tumor nest. Overexpression of CD82 had been found to increase cell homotypic adhesion and induce cell aggregation, which inhibited the initiation of the metastatic process (Abe et al. 2008; Jee et al. 2003). Furthermore, we examined the influence of CD82EC1-mP on cell homotypic aggregation. As shown in Fig. 3, after treatment with 50 μg/ml of CD82EC1-mP, all the cells tested were clustered together to form large multi-cellular clusters. The result indicated that CD82EC1-mP could promote homotypic cell–cell aggregation.
CD82EC1-mP promotes the homotypic cell–cell aggregation. SW620, MDA-MB- 231, PC3, H1299 and LLC cells were seeded in 12-well plates in a specific medium supplemented with 10% fetal bovine serum with or without (control) 50 μg/ml of CD82EC1-mP for 12 h. The cell aggregation was photographed under an inverted light microscope
CD82EC1-mP inhibits cancer cell adhesion
Cell adhesion to extracellular matrix is essential for motility and invasion. It was reported that CD82 attenuated the cancer cell adherent to the extracellular matrix, such as FN, LN, or non-coated tissue culture plates (Hemler et al. 1996; He et al. 2005). We next examined the effect of CD82EC1-mP on cell adhesion. As shown in Fig. 4, treatment with 50 μg/ml CD82EC1-mP almost completely blocked the cell adhesion to tissue culture plates. Taken together, all the results from above indicated that CD82EC1-mP could promote homotypic cell aggregation, inhibit cell migration and adhesion. In addition to the cell lines used above, the same results were also obtained using other cell lines, including A549, HepG2, 4T1, SW480 (results were not shown because of space limitations). This suggested that the action of CD82EC1-mP on tumor cells has no tissue specificity.
CD82EC1-mP blockes the cell adhesion to tissue culture plates. SW620, MDA-MB- 231, PC3, H1299 and HepG2 cells were seeded in 12-well plates in a specific medium supplemented with 10% fetal bovine serum and treated with or without (control) 50 μg/ml of CD82EC1-mP for 24 h. Cell adhesiveness was photographed under an inverted light microscope
CD82EC1-mP abrogates the lung metastases in animal models
In the cell-based assays, we found that CD82EC1-mP was able to promote homotypic cell–cell aggregation, inhibit cell migration and adhesion. Hence, CD82EC1-mP would be expected to exert the role of metastasis inhibition in vivo. To test this, we examined the effect of CD82EC1-mP on the tumor metastasis in vivo using both syngeneic and xenograft animal models.
First, we prepared the mouse lung cancer LLC cell syngeneic mice models by injecting LLC cell into ICR mice via tail vein. To mimic a clinical therapeutic situation (For example, CD82EC1-mP were administrated at preoperative, postoperative, or intraoperative of surgical resection of primary tumor foci to prevent the spread and metastasis of tumor cells), we designed three treated groups according to the time of administration of the drug. After 35 days of injection, the mice were sacrificed and the metastatic foci on the lung surface were detected. As shown in Fig. 5, the lung metastasis was dramatically reduced in all three treated groups, comparing with the control group. The lung metastasis positive rates were 90% (9/10) in control mice, and 10% (1/10), 40% (4/10) and 30% (3/10) in groupI, II and III, respectively. These data indicated that CD82EC1-mP strongly inhibited LLC cell pulmonary metastasis.
For xenograft studies, two human cancer cell lines, colon SW620 and lung H1299 were used in the experimental metastasis assays. As shown in Fig. 6, the lung metastasis was markedly reduced by CD82EC1-mP in all the tumor cell line xenograft modles. The lung metastasis positive rates in treated group mice versus control group mice were 14% (1/7) and 86% (6/7) for SW620, and 14% (1/7) and 100% (7/7) for H1299, respectively. The results from xenograft study demanstrated that CD82EC1-mP had a broad anti-metastasis activity (Figs. 5 and 6).
CD82EC1-mP blocked the pulmonary metastasis of mouse lung cancer LLC cell in syngeneic mice model. The mouse lung cancer LLC cell syngeneic mice models were prepared by injecting LLC cell into ICR mice via tail vein. According to the time of administration of drug, the treated groups were divided into three groups: groupI, cells and CD82EC1-mP were injected at the same time; groupII, CD82EC1-mP was administrated 2 h before cell inoculation; groupIII, CD82EC1-mP was administrated 2 h after cell inoculation. Lung metastasis positive mice were defined by the formation of one or more visible metastatic nodules on the lung surface of tumor-bearing mice and labeled with “+”. The non-metastatic samples were labeled with “−”. The Lung metastatic nodules were indicated with arrows
CD82EC1-mP blocked the pulmonary metastasis of tumor cells in xenograft mice models. Human colon SW620 and lung H1299 cells xenograft mice models were constructed by injecting these cells into BALB/cA-nu/nu via tail vein. Lung metastasis positive mice were defined by the formation of one or more visible metastatic nodules on the lung surface of tumor-bearing mice and labeled with “+”, The non-metastatic samples were labeled with “−”. The Lung metastatic nodules were indicated with arrows
Discussion
At present, except for EC1, the corresponding function of each of the domain of CD82 was basically clear (Kovalenko et al. 2005; Stipp et al. 2003). In this paper, we focused our attention on the EC1 domain CD82. We synthesized the peptide according to the EC1 amino acid sequence of CD82 by means of chemical synthesis, and then examined these peptides roles in the invasive behavior of tumor cells. In the cell-based assays, we found that CD82EC1-mP was able to promote homotypic cell–cell aggregation, inhibit cell migration and adhesion, and its action was more powerful than that of full CD82 molecules compared to the data reported by others. In the tested cell lines, cell migration and cell adherence were completely inhibited at a concentration of 50 μg/ml CD82EC1-mP. These findings suggested that CD82CE1-mP alone is sufficient for the function of CD82 inhibit cell invasion and migration.
Since CD82EC1-mP can strongly inhibit tumor cell invasion and migration in vitro, it would be expected to exert the role of metastasis inhibition in vivo. Next, we investigated the influence of CD82EC1-mP on the lung metastasis capability of different tumor cell lines by injecting the tumor cell into the tail veil of syngeneic mice or nude mice. Our results showed that CD82EC1-mP treatment significantly reduced the pulmonary metastasis in multiple types of tumor cells both in syngeneic and xenograft mice models. These results indicated that EC1 mimic peptide will be very promising to be used in clinical metastasis therapy.
Of the three treated groups in syngeneic mice models, groupI showed a maximum inhibition in lung metastases formation (1/10). Other two treated groups, group II and group III showed a lower lung metastasis inhibition rate than that of groupI. The reason may be that the concentration of CD82EC1-mP in vivo was decreased through enzymolysis or binding with plasma proteins. Especially in group II, when the cells were inoculated 2 h after administration of CD82EC1-mP, the concentration of CD82EC1-mP in vivo will greatly reduce. Therefore, we believe that further increase of CD82EC1-mP concentration will increase the inhibition rate of lung metastasis.
To sum up, this novel finding has important theoretical and clinical significance. Theoretically, the novel finding will improve our understanding of the mechanism by which CD82 inhibits metastasis. Therapeutically, with current technology, all the strategies, including gene therapy, induction of gene re-expression or direct administration of CD82 intact molecule cannot be used in clinical metastasis therapy. Our result offers a new strategy for the design of anti-metastasis agents targeting CD82. CD82 is widely expressed in normal tissue cell, so EC1 mimic peptide is a natural peptide and has no immunogenicity(Stipp et al. 2003). CD82EC1-mP exerts its function outside the cells, thus, can be used directly in the clinic, not requiring complicated gene transfer or drug delivery technology. The CD82EC1-mP can abrogate multiple types of tumor metastasis, so that has no tissue cell specificity.
The main biological function of CD82 is to regulate cell adhesion and migration, which involved in tumor metastasis, development, immune response, virus binding and growth of stem cells. Therefore, in addition to inhibiting tumor metastasis, the EC1 mimic peptide should have a broader role.
Change history
05 May 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00432-021-03649-9
References
Abe M, Sugiura T, Takahashi M et al (2008) A novel function of CD82/KAI-1 on E-cadherin-mediated homophilic cellular adhesion of cancer cells. Cancer Lett 266:163–170
Berger JC, Vander Griend DJ, Robinson VL et al (2005) Metastasis suppressor genes: from gene identification to protein function and regulation. Cancer Biol Ther 4:805–812
Brabletz T, Lyden D, Steeg PS et al (2013) Roadblocks to translational advances on metastasis research. Nat Med 19:1104–1109
Dong JT, Lamb PW, Rinker-Schaeffer CW (1995) KAI1, a metastasis suppressor gene for prostate cancer on human chromosome 11p11.2. Science 268:884–886
He B, Liu L, Cook GA et al (2005) Tetraspanin CD82 attenuates cellular morphogenesis through down-regulating integrin alpha6-mediated cell adhesion. J Biol Chem 280:3346–3354
Hemler ME (2003) Tetraspanin proteins mediate cellular penetration, invasion, and fusion events and define a novel type of membrane microdomain. Annu Rev Cell Dev Biol 19:397–422
Hemler ME, Mannion BA, Berditchevski F (1996) Association of TM4SF proteins with integrins: relevance to cancer. Biochim Biophys Acta 1287:67–71
Jee B, Jin K, Hahn JH et al (2003) Metastasis suppressor KAI1/CD82 induces homotypic aggregation of human prostate cells through Src-dependent pathway. Exp Mol Med 35:30–37
Kauffman EC, Robinson VL, Stadler WM et al (2003) Metastasis suppression: the evolving role of metastasis suppressor genes for regulating cancer cell growth at the secondary site. J Urol 169:1122–1133
Kovalenko OV, Metcalf DG, DeGrado WF, Hemler ME (2005) Structural organization and interactions of transmembrane domains in tetraspanin proteins. BMC Struct Biol 5:11
Lee HA, Park I, Byun HJ et al (2011) Metastasis suppressor KAI1/CD82 attenuates the matrix adhesion of human prostate cancer cells by suppressing fibronectin expression and β1 integrin activation. Cell Physiol Biochem 27:575–586
Luan MC, He X, Huang XH et al (2018) The peptide mimicking small extracellular loop domain of CD82 inhibits tumor cell migration, adhesion and induces apoptosis by inhibiting integrin mediated signaling. Biochem Biophys Res Commun 503:2206–2211
Malik FA, Sanders AJ, Jiang WG (2009) KAI-1/CD82, the molecule and clinical implication in cancer and cancer metastasis. Histol Histopathol 24:519–530
Rinker-Schaeffer CW, O’Keefe JP, Welch DR et al (2006) Metastasis suppressor proteins: discovery, molecular mechanisms, and clinical application. Clin Cancer Res 12:3882–3889
Robinson VL, Kauffman EC, Sokoloff MH et al (2004) The basic biology of metastasis. Cancer Treat Res 118:1–21
Shoushtari AN, Szmulewitz RZ, Rinker-Schaeffer CW (2011) Metastasis-suppressor genes in clinical practice: lost in translation? Nat Rev Clin Oncol 8:333–342
Smith SC, Theodorescu D (2009) Learning therapeutic lessons from metastasis suppressor proteins. Nat Rev Cancer 9:253–264
Stafford LJ, Vaidya KS, Welch DR (2008) Metastasis suppressors genes in cancer. Int J Biochem Cell Biol 40:874–891
Steeg PS, Ouatas T, Halverson D et al (2003) Metastasis suppressor genes: basic biology and potential clinical use. Clin Breast Cancer 4:51–62
Stipp CS, Kolesnikova TV, Hemler ME (2003) Functional domains in tetraspanin proteins. Trends Biochem Sci 28:106–112
Tsai YC, Weissman AM (2011) Dissecting the diverse functions of the metastasis suppressor CD82/KAI1. FEBS Lett 585:3166–3173
Yoshida BA, Sokoloff MM, Welch DR et al (2000) Metastasis-suppressor genes: a review and perspective on an emerging field. J Natl Cancer Inst 92:1717–1730
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81472716) and Dalian Technology and Innovation Fund (No. 2019J13SN94).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the changes in the figure citations.
Rights and permissions
About this article
Cite this article
He, X., Ma, X., Wang, C. et al. The peptide mimicking small extracellular ring domain of CD82 inhibits tumor cell migration in vitro and metastasis in vivo. J Cancer Res Clin Oncol 147, 1927–1934 (2021). https://doi.org/10.1007/s00432-021-03595-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03595-6