Abstract
Background
An increasing number of studies have focused on the early diagnostic value of the methylation of RASSF1A and SHOX2 in lung cancer. However, the intricate cellular events related to RASSF1A and SHOX2 in lung cancer are still a mystery. For researchers and clinicians aiming to more profoundly understand the diagnostic value of methylated RASSF1A and SHOX2 in lung cancer, this review will provide deeper insights into the molecular events of RASSF1A and SHOX2 in lung cancer.
Methodology
We searched for relevant publications in the PubMed and Google Scholar databases using the keywords “RASSF1A”, “SHOX2” and “lung cancer” etc. First, we reviewed the RASSF1A and SHOX2 genes, from their family structures to the functions of their basic structural domains. Then we mainly focused on the roles of RASSF1A and SHOX2 in lung cancer, especially on their molecular events in recent decades. Finally, we compared the value of measuring RASSF1A and SHOX2 gene methylation with that of the common methods for the diagnosis of lung cancer patients.
Results
The RASSF1A and SHOX2 genes were confirmed to be regulators or effectors of multiple cancer signaling pathways, driving tumorigenesis and lung cancer progression. The detection of RASSF1A and SHOX2 gene methylation has higher sensitivity and specificity than other commonly used methods for diagnosing lung cancer, especially in the early stage.
Conclusions
The RASSF1A and SHOX2 genes are critical for the processes of tumorigenesis, development, metastasis, drug resistance, and recurrence in lung cancer. The combined detection of RASSF1A and SHOX2 gene methylation was identified as an excellent method for the screening and surveillance of lung cancer that exhibits high sensitivity and specificity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer contributes to the highest incidence of cancer-related mortality in the world (Bray et al. 2018). At present, the methods for treating lung cancer have continuously improved; such methods include early surgical resection, the first-line standard treatment of radiotherapy and chemotherapy, immunotherapy and targeted therapy for advanced lung cancer patients (Blumenthal et al. 2018). However, the effect of drug therapy is often unsatisfactory because of metastasis and the emergence of drug resistance, which could be derived by EGFR secondary mutations, such as EGFR T790M, and epigenetic modifications, such as DNA methylation (Lin and Shaw 2016; Mehta et al. 2015). The poor 5-year survival rate mainly results from delayed diagnosis and the presence of drug resistance and metastatic lesions (Dela Cruz et al. 2011). Therefore, the search for more specific and more sensitive detection strategies for the diagnosis of lung cancer in the early stage and for the monitoring of the response to therapies in the advanced stage is urgent.
Lung cancer is a heterogeneous disease based on different genetic and epigenetic molecular alterations. Genetic changes, including point mutations, deletions, translocations, and amplifications, are known as the drivers of lung cancer that lead to sequential progression from benign disease to cancer. Epigenetics focuses on the heritable alterations of gene expression while without changing the DNA sequence of genes (Deans and Maggert 2015). DNA methylation is one of the most thoroughly studied epigenetic modifications of genomic DNA. The functions of DNA modification by methylation include maintaining chromosome stability, inhibiting repetitive sequences, preventing foreign DNA integration, and controlling gene expression (Robertson 2005). DNA methylation has been considered closely associated with tumorigenesis and one of the earliest and most consistent molecular markers of human cancers (Abu-Remaileh et al. 2015; Heyn and Esteller 2012; Timp and Feinberg 2013). The genome of tumor cells shows global hypomethylation and regional hypermethylation, especially in promoter CpG islands of tumor suppressor genes (Heyn and Esteller 2012). Methylation of promoter CpG islands could transcriptionally silence the associated genes, most of which are tumor suppressor genes (TSGs), and contribute to oncogenesis (Laird 2003).
TSGs are normal genes that control normal cell division, repair DNA damage and promote apoptosis or programmed cell death of damaged cells. In addition, the proteins encoded by TSGs could regulate many other genes to maintain the stability of DNA. TSGs tend to be recessive that both alleles must be damaged contributing to cancer (Zhu et al. 2015). Once a TSG is hypermethylated or mutated, resulting in loss of its activity, cell division might proceed uncontrolled and contribute to tumorigenesis (Esteller 2002).
Recently, many prevalent studies have reported that TSGs, such as CDKN2A, APC, RARβ, MGMT, DAPK, F2RL3,and RASSF1A, were frequently hypermethylated and silenced in lung cancer (Duruisseaux and Esteller 2017; Feng et al. 2016; Niklinska et al. 2009). Ras association domain-containing protein 1A (RASSF1A), one of the most thoroughly studied TSGs, is functionally involved in cell proliferation, tumorigenesis, and migration (Malpeli et al. 2019). Short stature homeobox 2 (SHOX2), an oncogene, is a regulator of cell proliferation and apoptosis and an inducer of EMT (Marchini et al. 2016). In addition to its functions in the progression of cancer, SHOX2 is also critical for skeletal development, embryonic development, and cardiovascular system differentiation (Peng et al. 2019; Yi et al. 2017). RASSF1A and SHOX2 both are frequently hypermethylated in lung cancer tissue (Darwiche et al. 2013; Kneip et al. 2011; Zhang et al. 2017). Studies from several groups have shown that the combined detection of RASSF1A and SHOX2 methylation in various types of samples, including alveolar lavage fluid, serum, pleural effusion, ascites samples, cells, and lymph nodes, exhibited remarkably high sensitivity and specificity in lung cancer (Darwiche et al. 2013; Kneip et al. 2011; Ooki et al. 2017; Ren et al. 2017; Zhang et al. 2017). Evidence has strongly suggested that the methylation of RASSF1A and SHOX2 is a critical event in the tumorigenesis and progression of lung cancer, and these modified genes could serve as a potential pair of biomarkers for lung cancer screening at early or advanced stages (Alanazi et al. 2018; Niklinska et al. 2009; Peng et al. 2019; Zhang et al. 2017). Currently, an increasing number of studies have focused on the diagnostic value of RASSF1A and SHOX2 methylation in lung cancer. However, the inherent relationship between the epigenetic methylation and intricate cellular events of RASSF1A and SHOX2 in lung cancer is not well understood.
To more profoundly understand the diagnostic value of methylated RASSF1A and SHOX2 in lung cancer, this review will provide substantial insights into the molecular events of RASSF1A and SHOX2 in lung cancer.
Survey methodology
PubMed database (https://www.ncbi.nlm.nih.gov/pubmed) and Google scholar database (https://scholar.chongbuluo.com/) were mainly used for related publication search with the keywords “RASSF1A”, “RASSF1-A”, “RASSF-1A”, “SHOX2”, “SHOX”, “Shox2”, “OG12”, “SHOT”, “OG12X”, and “lung cancer”.
RASSF1A
RASSF1A gene function and related diseases
The RAS-association domain family (RASSF) comprises ten members from RASSF1 to RASSF10. These proteins are characterized by a putative Ras association (RA) domain that can be found on the C terminus (for example RASSF1-6, called C-RASSF proteins) or on the N terminus (for example RASSF7-10, called N-RASSF proteins) (Iwasa et al. 2018; Richter et al. 2009). RASSF1 and RASSF5 are widely and prominently studied members of this protein family, while few studies have provided data about the other members.
The RASSF1 gene contains eight exons (1α, 1β, 2αβ, 2γ, 3, 4, 5 and 6) and two promoters, in which there are two CpG islands. The RASSF1 proteins consist of eight variant isoforms (RASSF1A–RASSF1H) that are produced from alternative splice variants and alternative promoter usage (Richter et al. 2009). Recently, only RASSF1A and RASSF1C two isoforms were mainly focused and researched. Interestingly, RASSF1A and RASSF1C are ubiquitously expressed in normal tissue, and they localize microtubules and participate in growth regulation (Malpeli et al. 2019). Although harboring 60% amino acid identity, the two transcripts exhibit different biological functions (Volodko et al. 2014). The functions of RASSF1A and RASSF1C in cancer are almost opposite; the former plays a role in suppressing cancer, while the latter plays a pivotal role in carcinogenesis. RASSF1A and RASSF1C have three identical domains, including the RA domain, the ataxia telangiectasia mutated (ATM) phosphorylation site and the Salvador/rassf/Hippo (SARAH) domain, which suggests their overlapping functions in cells. The C1 domain (a protein kinase C (PKC) conserved region) is the main structural difference between the two isoforms, and it exists only at the N terminus of RASSF1A, which explains the opposing roles of these proteins in carcinogenesis in a certain (Dubois et al. 2019a). RASSF1A and RASSF1C balance cell survival events and malignant behavior. The hypermethylated transcriptional silencing of RASSF1A disrupts the balance and contributes to the overexpression of RASSF1C and the function of RASSF1C in carcinogenesis (Dubois et al. 2019a).
It is important to understand the functions of domains. RASSF1A is unique in its structures that it contains a cysteine-rich domain (CRD), known as an amino-terminal-conserved region one diacylglycerol-binding domain (C1/DAG), which is absent in RASSF1C and other RASSF family members except for RASSF5 (Donninger et al. 2007). Therefore, RASSF1A and RASSF5 form heterodimers with each other via the C1 domain (Ortizvega et al. 2002). The C1/DAG interaction can drive membrane translocation and mediate proximal signal transduction events, including the PKC/MAPK/ERK pathway, which is associated with cell growth (Johnson et al. 2007; Lucic et al. 2016). The RA domain is considered a Ras effector and interacts with Ras-related GTPases (Richter et al. 2009). However, the RA domain activity of RASSF1A is so weak that RASSF1A only acts as a scaffold linking members of the Ras family, such as k-ras, to the regulation of multiple pro-apoptotic signaling pathways (Schmidt et al. 2018). Adjacent to the RA domain is a C-terminal coiled-coil motif called the SARAH domain, which only exists in RASSF1-6 (Sherwood et al. 2009). The SARAH domain of RASSF1A (RASSF1-SARAH) binds RASSF1A to the RASSF isoforms to form a homodimer or heterdimer, and interacts with MST-SARAH to activate the Hippo pathway, which is an important pro-apoptotic signaling pathway (Iwasa et al. 2018). In addition, the ATM phosphorylation site is found only in RASSF1 isoforms A, C, D, E and H, and this site is not present in other RASSF family members. The ATM phosphorylation site contributes to modulating the phosphorylation of the effectors of DNA damage checkpoint pathways, which are involved in the regulation of genomic stability (Donninger et al. 2007). Figure 1 shows more clearly the structure and functional domain of RASSF1A as described.
The whole structure and functional domains of RASSF1A RASSF1 lie on 3p21.31 and is comprised of eight exons, three promotors with two CpG islands of which one belongs to RASSF1A and the other belongs to RASSF1C. RASS1A is generated from RASSF1 through alternative splicing. Untranslated region and exons are respectively showed by open boxes and black boxes, promoters by black arrows and CpG islands by grey bars. The protein of RASSF1A has four common domain whose functions were described as the above: conserved region 1 diacylglycerol-binding domain (C1/DAG) (red), putative ATM kinase phosphorylation consensus sequence motif (yellow), Ras association (RA) domain (green), Salvador/RASSF/Hippo (SARAH) domain (purple)
Based on the function of its domains, the basic function of RASSF1A is related to microtubule stabilization, motility, mitosis, DNA repair, genomic stability, apoptosis, and proliferation. Therefore, RASSF1A is so important that its deficiency is necessary for tumorigenesis, migration, and neoplastic transformation. Mutations of RASSF1A are rarely reported in tumors (Richter et al. 2009). Alleles of RASSF1A are mainly inactivated by hypermethylation of the CpG islands in their promoters and by heterozygous deletion; hypermethylation of the promoter is the dominant reason for RASSF1A deficiency in cancer tissues (Donninger et al. 2007).
Possible roles of RASSF1A in lung cancer
Inflammatory cytokines (including interleukin (IL)-6) are generated by precancerous cells or cancer cells and induce tissue damage, which ultimately results in chronic inflammation (Strzelak et al. 2018). Chronic inflammation plays an important role in driving the fundamental biological processes of cancer, including tumor angiogenesis, proliferation, metastasis, immune suppression, epithelial–mesenchymal transition (EMT), and cancer stem cell (CSC) generation (Markopoulos et al. 2019; Tan et al. 2013). The classic inflammatory cytokine signaling pathway is the TGF-β1/SMADS/AMPK/NF-κB pathway, which triggers a cascade that amplifies inflammatory events (Markopoulos et al. 2019). Interestingly, Marilyn Gordon et al. have shown that RASSF1A is strongly associated with the Toll-like receptor (TLR) components and results in inhibiting the TLR-driven activation of NF-κB (Gordon et al. 2013). In Rassf1a knockout mice, the failure of Rassf1a to inhibit NF-κB enhances inflammation-induced DNA damage and thereby promotes the tyrosine phosphorylation of Yes-associated protein (YAP) and the accumulation of p53 (Gordon et al. 2013). Therefore, RASSF1A deficiency could stimulate the NF-κB pathway, leading to enhanced inflammation and contributing to tumorigenesis. It was reported that IL-6 drove RASSF1A hypermethylation and decreased transcription by upregulating DNA methyltransferase 1 (DNMT1) in cancer cells (Braconi et al. 2010; Foran et al. 2010). Lee Schmidt et al. showed that RASSF1A-knockdown cells exhibited upregulated IL-6 and enhanced inflammation (Schmidt et al. 2018). Additionally, scientists demonstrated that Rassf1a-knockout mice with chemically induced colitis exhibited exacerbated inflammation and distinctly increased IL-6 production (Gordon et al. 2013; Schmidt et al. 2018). Therefore, there is a positive feedback loop between IL-6 and RASSF1A, which more obviously shows us the relationship between the silence of RASSF1A and inflammation. In cancer cells, overexpressed RASSF1A exhibited a dual function that suppressed cell proliferation by blocking the cell cycle through the downregulation of cyclin D1 and promoted invasiveness by upregulating p21 and vimentin through the activation of the IL-6/STAT3 pathway (Huang et al. 2016; Yi et al. 2018). Several elegant studies have directly demonstrated that IL-6 can promote lung tumorigenesis (Koyama et al. 2016; Qu et al. 2015; Tan et al. 2013). Obviously, RASSF1A epigenetic silencing and inflammatory signaling intricately cooperate in lung tumorigenesis and metastasis.
The Hippo signaling pathway not only promotes apoptosis but also induces stem cell differentiation during organ development and tissue regeneration. RASSF1A activates the Hippo pathway as a critical upstream regulator. Moreover, RASSF1A directly promotes cooperation between YAP1 and p73, which mediates the transcription of pro-apoptotic genes and differentiation genes by inhibiting the nuclear translocation of SMAD2 (Iwasa et al. 2018; Papaspyropoulos et al. 2018). RASSF1A overexpression inhibits lung cancer cell proliferation, invasion, and metastasis potentially by preventing YAP activation through the GEF-H1/RhoB pathway (Dubois et al. 2016). The deficiency in RASSF1A not only disrupts this critical pro-apoptotic pathway but also enhances cancer-related pathways. RASSF1A deficiency leading to YAP activation is a key reason that bronchial epithelial cells acquire a malignant phenotype, invasive and antiapoptotic properties, and finally transform into cancer cells (Dubois et al. 2016; Dubois et al. 2019b; Pefani et al. 2016). RASSF1A depletion increases YAP nuclear accumulation and activates YAP through the following main mechanisms: (i) inactivating the Hippo pathway: RASSF1A silencing fails to activate the MST2/LAST pathway, resulting in YAP dephosphorylation and reduced degradation; (ii) inhibiting the RASSF1A/NDR2/GEF-H1/RhoB/YAP pathway (Dubois et al. 2016; Keller et al. 2019): RASSF1A depletion causes NDR2 and GEF-H1/RhoB activation, and subsequently RhoB enhances the inhibition of YAP phosphorylation; (iii) promoting the YAP1/SMAD2 interaction: TGF-β stimulates RASSF1A degradation, which is required for YAP1/SMAD2 interaction and SMAD2 nuclear translocation, and YAP1 and SMAD2 cotranscribe many genes involved in invasion and metastasis (Pefani et al. 2016).
RASSF1A, as a RAS effector, not only crosslinks K-RAS to pro-apoptotic signaling pathways, such as the Bax and Hippo pathways but also facilitates the association of Ras with other signaling pathways, including inflammation, autophagy, DNA repair, protein acetylation, and ubiquitination (Donninger et al. 2016). For example, after K-RAS and RASSF1A form a complex, RASSF1A activates Bax by binding to MOAP-1 (Vos et al. 2006). Recently, Lee Schmidt and colleagues reported that RASSF1A deficiency enhances RAS-driven lung tumorigenesis, and the dysregulation of inflammatory pathways due to RASSF1A deficiency may also contribute to these processes (Schmidt et al. 2018). In conclusion, the frequent epigenetic loss of the RASSF1A gene undoubtedly affects the balance of many cellular events contributing to Ras-driven tumorigenesis, metastasis, and transformation.
RASSF1A competitively binds to MST2 from the RAF-1–MST2 inhibitory complex, which in turn enhances RAF-1 activity and enhances the MST2/LAST kinase cascade pro-apoptotic response (Romano et al. 2014). This observation suggests that the loss of RASSF1A inhibits the Ras-MAPK pathway. Thaler et al. (2012) reported a paradoxical regulatory relationship between RASSF1A and the Ras-MAPK pathway in breast cancer cells. RASSF1A represses estrogen receptor (ERα) expression and transiently suppresses ERα-induced Ras-MAPK activity upon E2 stimulation but later activates the Ras-MAPK pathway as a result of inhibited Akt1 activity (Thaler et al. 2012). The inhibited activity of Akt1 reduces the suppression of the Ras-MAPK pathway, resulting in its activation. Interestingly, some scientists reported an opposite result, namely that the loss of RASSF1A mediates the activation of the Raf-MAPK pathway in lung cancer cells (Huang et al. 2016; Kilili and Kyriakis 2010; Pallares et al. 2008; Thaler et al. 2009). RASSF1A deficiency activates extracellular signal-regulated kinase 1/2 (ERK1/2) by enhancing physical binding to MST2, which increases its activity (Ram et al. 2014). Mst2 and Raf not only inhibit each other's activity. In addition, Kilili GK demonstrated that Mst2 also positively regulates Raf-1 activity by maintaining the catalytic subunit of phosphatase-2A (PP2A-C) levels, which subsequently activate the Raf/ERK pathway (Kilili and Kyriakis 2010). In addition, this study showed that the Mst2 – > LATS1/2 pathway promotes mitogenic signaling. To date, there is little evidence regarding the mechanism by which RASSF1A cross-talks with components of the Raf-MAPK pathway. More evidence that validates the relationship between RASSF1A and the Ras-MAPK pathway might greatly contribute to the study of the mechanisms of lung cancer occurrence and progression.
The scientists (Volodko et al. 2016) found that RASSF1A methylation frequency and expression were indirectly regulated by p53/death-associated protein 6 (DAXX) signaling. These authors reported that P53 binds to the promoter of RASSF1A and then recruits DAXX and DNMT1, which finally results in the methylation and inactivation of RASSF1A. Moreover, studies demonstrated that the DAXX expression levels (and not the p53 expression levels) directly affected the rates of RASSF1A methylation. However, RASSF1A-knockout mice tend to exhibit spontaneous tumorigenesis and can enhance p53- or K-RAS-mediated tumor susceptibility (Schmidt et al. 2018; Tommasi et al. 2011). Rassf1a−/− p53−/− double-knockout mice were remarkably susceptible to tumor formation and died due to malignancies significantly faster than their single-knockout littermates (Tommasi et al. 2011); these results indicated that p53 and RASSF1A have a unique relationship with each other. The loss of RASSF1A disrupts the normal mechanisms by which mitosis causes genomic instability, such as cytokinesis failure, tetraploidization, and p53-dependent tetraploidy checkpoint activation (Tommasi et al. 2011). Therefore, RASSF1A epigenetic silencing and p53 also potentially cooperate in lung tumorigenesis. Further basic molecular research and clinical studies must be carried out to prove the effect of the p53 mutation status on RASSF1A promoter-specific methylation. Interestingly, Licchesi et al. (2008) confirmed that the level of RASSF1A hypermethylation significantly increased in the progression from normal tissues to precancerous lesions and then to lung cancer. Interestingly, it has been demonstrated that RASSF1A directly antagonizes RhoA, which is a factor that is directly related to tumor cell invasion and metastasis; this is an indispensable process for tumor inhibition (Lee et al. 2016). In addition, RASSF1A deficiency reduces the expression of β-catenin and E-cadherin, which facilitate malignant cell adhesion to the extracellular matrix (ECM), migration and invasion (Bao et al. 2019). The loss of RASSF1A meditates dedifferentiation to pluripotency in embryonic stem cells (ESCs) via WNT/Hippo pathway transcription factor competition (Papaspyropoulos et al. 2018). Pankova et al. reported that lung adenocarcinoma cells with hypermethylated RASSF1A exhibit increased expression of prolyl 4-hydroxylase alpha-2 (P4HA2), resulting in collagen deposition and a rigid ECM that trigger cancer stem cell-like programming and metastatic dissemination (Pankova et al. 2019). Therefore, the deficiency of RASSF1A in lung cancer is involved in lower differentiation grade and enhanced stem cell characteristics, which are essential for EGFR-TKI resistance, reoccurrence, and metastasis in lung cancer.
According to the present data, the frequency of RASSF1A promoter methylation is reported to be as high as 88% in lung cancer compared with hardly any methylation in the normal surrounding tissue; the frequency of RASSF1A promoter methylation reaches almost 100% in small cell lung cancer (SCLC) and 65% in non-small cell lung cancer (NSCLC) (Burbee et al. 2001; Grawenda and O'neill 2015). Epigenetic loss in RASSF1A is considered a common event in lung tumors, and this loss is very important for the occurrence, invasion and metastasis of lung cancer. However, Swati Dabral et al. (Dabral et al. 2019) reported a novel finding that in some tumors, RASSF1A was highly expressed instead of epigenetically or genetically silenced. Under hypoxia, RASSF1A-HIF-1α signaling forms a positive feedback loop that results in the accumulation of RASSF1A and then facilitates the regulation of hypoxia-driven genes, the Warburg effect, and proliferation in a nonmalignant, hypoxia-induced prototype disease and in lung cancer (Dabral et al. 2019).
Furthermore, microRNAs (miRNAs) are involved in the regulation of RASSF1A. Recently, two miRNAs (miR-602 and miR-181a/b) have been proven to directly target and negatively control the expression of RASSF1A in many types of cancer cells (Bräuer-Hartmann et al. 2015; Yang et al. 2010; Yu et al. 2018). The research team of Daniela Bräuer-Hartmann demonstrated that the process of mir-181 a/b targeting and inhibiting RASSF1A demonstrates a very specific PML/RARα dependency in acute promyelocytic leukemia (APL) (Bräuer-Hartmann et al. 2015). Therefore, these authors first thought that RASSF1A might be a member of the retinoic acid-induced differentiation network in APL (Bräuer-Hartmann et al. 2015). Moreover, many miRNAs, including miR-148a, miR-152 and miR-342, also downregulate RASSF1A expression but first target DNMT1 and then silence RASSF1A by hypermethylation (Braconi et al. 2010; Wang et al. 2011). Interestingly, RASSF1A induces miR-711 to downregulate CDK4 expression, resulting in cell cycle arrest at the G1 phase (Liao et al. 2016). Therefore, miRNA-induced suppression of RASSF1A might be necessary for tumorigenesis and progression of cancer.
Based on the information described above, we aim to provide a deeper understanding of the molecular events of RASSF1A in lung cancer. In the past several decades, scholars have reported that RASSF1A plays a vital role in lung cancer tumorigenesis and metastasis. The link between RASSF1A and key cancer pathways, including the IL-6/JAK/STAT3 (Yi et al. 2018), Hippo (Chen et al. 2017; Oh and Lockwood 2017), Ras/PI3K/AKT, Ras/RAF/MEK/ERK, RhoA/TGF-β (Lee et al. 2016), K-RAS and p53 signaling pathways, is discussed above and is summarized in Fig. 2. In all of these scenarios, RASSF1A or methylated RASSF1A could be a promising and practical biomarker for the early diagnosis, stage evaluation, histopathological typing, and monitoring the chemotherapy/targeted drug response and progression of lung cancer.
Possible roles of RASSF1A in lung cancer. Inflammatory stimulation induces the production of inflammatory cytokines, such as IL6. IL-6 and micro RNAs epigenetically silence RASSF1A through DNMT1 and DNA methyltransferase 3B (DNMT3B). RASSF1A is a pivotal regulator of the hippo pathway promoting apoptosis. RASSF1A activates MST1/2, LATS1/2 and YAP/TAZ by phosphorylating their proteins one by one and in turn, promotes pro-apoptotic genes transcription. The epigenetic silence of RASSF1A fails to activate the Hippo pathway resulting in YAP dephosphorylation and degradation of reducing. RASSF1A depletion causes NDR2 and GEF-H1/RhoB activation, and subsequently RhoB enhances the inhibition of YAP phosphorylation. It leads to more nuclear accumulation of dephosphorylation of YAP/TAZ. RASSF1A cross-talks with TFG-β by negatively regulating SMAD2/3 and RhoA. What’s more, the loss of RASSF1A could activate Ras/Raf/MAPK/ERK and Ras/PI3K/AKT pathway. The RASSF1A loss-drived processes could result in lung cancer cell proliferation, anti-apoptosis, inflammation, angiogenesis, resistance, stemness, EMT, metastasis, and invasion
SHOX2
SHOX2 gene function and related diseases
Short stature homeobox (SHOX) is a member of the paired homeobox gene family and lies on the pseudoautosomal quarter 1 (PAR1) of the sex chromosomes in humans. The SHOX2 gene, located on chr3q25.32 in humans, is known as SHOX, SHOT, OG12, and OG12X in humans, as Shox2 or Og12x in mice, and as paired family homeodomain protein (Prx3) in rats (Blaschke et al. 1998; De Baere et al. 1998; Hu et al. 2018; Semina et al. 1998; Van Schaick et al. 1997). SHOX2 is orthologous to murine Shox2 (sharing 99% identity at the amino acid level) and is highly homologous to SHOX (sharing 83% identity) with identical functional domains, so their functions are considered to partly overlap (Clement-Jones et al. 2000; Marchini et al. 2016; Semina et al. 1998). This observation suggests that studies of SHOX and Shox2 might provide certain clues regarding the role of SHOX2 in fundamental biological processes. The SHOX2 gene includes seven exons and yields three transcripts, namely SHOX2a, SHOX2b, and SHOX2c, about which there is little known to date (Hu et al. 2018). The proteins encoded by this gene contain a homeodomain, an SH3-binding domain, a P-loop cyclic nucleotide-binding site and an OAR domain (Blaschke et al. 1998; Rovescalli et al. 1996). The homeobox family proteins all contain a homeodomain, which is a characteristic 60-amino acid DNA-binding domain. The homeodomain is essential for the development of the early embryonic body structure and the cardiac autonomic rhythm system by regulating cellular proliferation and differentiation (Boncinelli 1997; Gehring et al. 1994). Some publications have identified the role of SHOX2 in physical development (Aza-Carmona et al. 2014; Blaschke et al. 1998; Bobick and Cobb 2012; Clement-Jones et al. 2000). SH3 domains mainly function by mediating intracellular protein–protein interactions through the recognition of proline-rich sequence motifs on cellular proteins (Weng et al. 1995). The OAR sequence is required for the transactivation activity of the human SHOX protein (Sawada et al. 2015). All the structural and functional domains of SHOX2 can be seen more clearly in Fig. 3.
The whole structure and functional domains of SHOX2. The SHOX2 gene lay on 3q25.32 and consisted of seven exons, three promoters and three CpG islands, one of which is on gene body and two of which are on promoters. Untranslated region and exons are, respectively, shown by open boxes and black boxes, promoters by black arrows, and CpG islands by grey bars. The amino acid sequence and common homology domains between the SHOX, Shox2, and SHOX2 genes show high similarity. The protein of SHOX2 has four domains whose functions were described as above: homeodomain (red), SH3-binding domain (green), P-loop cyclic nucleotide-binding site (yellow), and OAR domain (blue)
The role of SHOX2 in lung cancer. MiR-375 targets and represses SHOX2 through regulation of DNMT3B expression. MiR-375 is down-regulated in many cancers, which leads to the up-regulation of SHOX2. High expression of SHOX2 enhances the inhibition of Bmp4 and results in RUNX2 increase. RUNX2 plays a pivotal role in bone metastasis processes, including the up-regulation of MMPs and VEGFs, the activation of TGF-β and Wnt/β-catenin pathway, promoting the binding of Runx2–Smad complex and Runx2–cJun complex. Besides, SHOX2 and TβR-I or FGFR3 have interactions with each other. TβR-I and FGFR3 activate downstream signaling pathways, respectively. SHOX2 inhibits anti-apoptosis ability and activates NF-κB pathway through increasing RUNX2 to repress the activity of p53. Through these biological processes, the overexpression of SHOX2 in lung cancer cells is critial for tumor cell proliferation, inflammation, tumorigenesis, invasion, cell-skeleton reconstruction, EMT, bone metastasis, and drug resistance
The SHOX proteins are mainly enriched in the mid-portion and relatively distal regions of the limb skeleton, heart, nose, gill arches, nervous system, and human embryonic reproductive nodules (Clement-Jones et al. 2000). However, SHOX2 is relatively proximal to the limbs (Song et al. 2015). In addition, SHOX2 is also expressed in the nasal process, CNS basal plate, dorsal root ganglia, cardiac inflow tract, third pharyngeal arch, and derived structures (Clement-Jones et al. 2000). The SHOX gene mainly regulates the development of the early embryonic body structure and the cardiac autonomic rhythm system (Marchini et al. 2016; Mortensen et al. 2012). The alteration of the SHOX gene, such as by mutation, generally leads to a lack of expression that causes short stature syndrome (Marchini et al. 2016). Haploinsufficiency or mutation of the SHOX gene occurs in some skeletal dysplasia, such as Leri–Weill dyschondrosteosis, Turner syndrome, and Langer mesomelic dysplasia (Bonafe et al. 2015). Abnormal expression of SHOX2 causes cardiac rhythm system disorders, impaired cerebellar development, and motor coordination deficits (Ionta et al. 2015; Rosin et al. 2015). However, whether genetic alteration of the SHOX2 gene may lead to short stature syndrome diseases has not yet been determined (Aza-Carmona et al. 2014). In healthy, normal individuals and idiopathic short stature (ISS) and Leri–Weill dyschondrosteosis (LWD) patients with pseudoautosomal CNVs, the promoter CpG islands of SHOX were minimally methylated (Ogushi et al. 2019). This observation suggests that SHOX2 might be in a demethylation state in normal people and majority of ISS/LWD patients, which needs to be investigated.
SHOX interacts with chondrogenic transcription factors (SOX5/SOX6 and SOX9) and then activates the Agc1 enhancer, which is essential for chondrogenesis and skeletal development (Aza-Carmona et al. 2011). Interestingly, Miriam Aza-Carmona and Veronica Barca-Tierno et al. (Aza-Carmona et al. 2014) demonstrated that SHOX2 regulates two SHOX transcription targets using the same cofactors (SOX5, SOX6 and SOX9); one target is the natriuretic peptide precursor B gene (NPPB), and the other target is Aggrecan (ACAN). These authors showed that there was no genetic alteration of SHOX2 in a cohort of 83 LWD patients. In addition, these authors postulated a time- and tissue-specific functional redundancy between SHOX and SHOX2. SHOX has a dual regulatory function because it could not only be a transcriptional activator but also a transcriptional repressor, temporally and spatially regulating the expression of downstream genes (Hristov et al. 2014). Interestingly, similar to human SHOX, mouse Shox2 functions in bidirectional transcriptional regulation in different cell types, depending on the cell type-specific cofactors (Puskaric et al. 2010; Yu et al. 2007). Thus, we speculate that SHOX2 may also be a bidirectional transcription regulator.
There are three CpG islands in the SHOX2 gene (Ogushi et al. 2019; Song et al. 2015), and the methylation of these CpG islands could profoundly affect the SHOX2 gene itself and the expression of other related genes. Interestingly, the CpG islands of the SHOX2 gene are frequently hypermethylated and exhibit elevated expression in cancer tissue and cells, such as in lung cancer, breast cancer, esophageal squamous cell carcinoma, and hepatocellular carcinoma (Leiro et al. 2019; Yang et al. 2013; Yi et al. 2017). We can conclude that SHOX2 not only is critical for skeletal development, embryonic development, and cardiovascular system differentiation but also functions in the progression of cancer by promoting phenotypic transformation and migration (Peng et al. 2019; Yi et al. 2017).
Possible roles of SHOX2 in lung cancer
DNA methylation is important for regulating fundamental biological processes and human diseases (Robertson 2005). Aberrant DNA methylation is a biomarker of tumors. The differential methylation of certain genes, such as SHOX2, in tumor tissues and normal tissues indicates that these genes play an important role in tumorigenesis and tumor invasion and metastasis (Peng et al. 2019). In the last decade, the methylation of SHOX2 was considered a valuable auxiliary diagnostic biomarker for lung cancer. Nevertheless, there are currently just a few papers focused on the relevant pathophysiological molecular mechanisms of SHOX2 in carcinogenesis.
Shox2 directly interacts with and targets the bone morphogenic protein 4 (Bmp4) gene, which is a member of the TGF-β superfamily (Puskaric et al. 2010). Interestingly, Shox2 can facilitate the transcription of Bmp4 in Xenopus embryos while repressing the transcription of Bmp4 in limb development (Puskaric et al. 2010). This evidence certainly supports Ling Yu's conjecture that Shox2 can repress the expression of Bmp4 during limb development in normal mice (Yu et al. 2007). In addition, Ling Yu and her colleagues demonstrated that the overexpression of Bmp4 indirectly represses the expression of runt-related transcription factor 2 (Runx2) in the proximal limb of Shox2-deficient mice (Yu et al. 2007). Runx2 has been identified as a mesenchymal stem marker for various types of cancer, especially those with bone metastases, including lung cancer, and as a determinant regulator of bone metastases that is involved in bone remodeling and skeletal integrity (Valenti et al. 2016). Runx2 plays a crucial role in the osteogenic differentiation process of mesenchymal stem cells, which includes transforming growth factor-β 1/2 (TGF-β), vascular endothelial growth factors (VEGFs) and the Wnt/β-catenin pathway (Dalle Carbonare et al. 2012; Valenti et al. 2016). The high expression of Runx2 in prostate cancer cells is associated with the increased expression of metastasis-related factors, including matrix metalloproteinases (MMPs), pro-angiogenic factors and adhesion proteins, which are truly pivotal for tumorigenesis and metastasis (Baniwal et al. 2010). Moreover, TGF-β1 independently induces the Runx2–Smad and Runx2–cJun complexes to increase the expression of IL-11 and Runx2 in metastatic cells, which contribute to the progression of cancer-induced bone disease (Zhang et al. 2015a, b). In addition, it was reported that Runx2 regulates the processes of cell proliferation, epithelial–mesenchymal transition (EMT), apoptosis, metastasis, and resistance in lung cancer (Hsu et al. 2011; Huang et al. 2019a; Valenti et al. 2016; Xie et al. 2016). In response to DNA damage, RUNX2 forms a complex with P53 in the nucleus and binds to the p53-target promoter with the assistance of histone deacetylase 6 (HDAC6) (Ozaki et al. 2013) (35). Then RUNX2 negatively regulates the transcription and anti-apoptotic functions of the P53 target genes in the H1299 lung adenocarcinoma cell line (Ozaki et al. 2013). The knockdown of RUNX2 recovers the chemosensitivity of p53-null/p53-mutated cancer cells through activating the TAp73/TAp63-dependent cell death pathway (Ozaki et al. 2018). The downregulation of p53 activates NF-κB to promote tumorigenesis and leads to drug resistance by dysregulating cell cycle progression and inhibiting apoptosis in lung cancer cells (Yang et al. 2015). Therefore, SHOX2 inhibits anti-apoptosis and activates NF-κB pathway through increasing RUNX2 to repress the activity of p53, which results in the occurrence of carcinogenic biological processes. According to the completely orthologous relationship of mouse Shox2 and human SHOX2, we can strongly speculate that SHOX2 may act through the same mechanism (as we can see in Fig. 4). Therefore, SHOX2 promotes tumorigenesis, EMT, bone metastasis, and resistance in lung cancer through its downstream target genes.
Recently, SHOX2 was identified to be targeted and inhibited by certain microRNAs, such as miR-223-3p, miR-503, and miR-375, which ultimately suppresses cancer-related biological behavior (proliferation, EMT, and metastasis) in several different tumors (Hong et al. 2014; Huang et al. 2019b; Sun et al. 2019; Yi et al. 2017). Hong and his colleagues demonstrated that miR-375 directly targets SHOX2 and inhibits its protein and mRNA expression in breast cancer cells (Hong et al. 2014). Surprisingly, Laixi Bi and his colleagues demonstrated that miR-375 is too low to inhibit homeobox B3 (HOXB3) expression, leading to more DNMT3B promoting pre-miR-375 hypermethylation that represses miR-375 again in acute myeloid leukemia (Bi et al. 2018). The most classic function of DNMT3B is to cause DNA methylation of gene promoter CpG islands, especially of CpG islands in TSG promoters, resulting in transcriptional repression (Gagliardi et al. 2018). In addition, DNMT3B that lacks catalytic activity promotes the methylation of the bodies of transcribed genes and then causes high expression of these genes (Baubec et al. 2015; Duymich et al. 2016; Yang et al. 2014). Interestingly, SHOX2, which is considered an oncogene, is hypermethylated and overexpressed in cancer (Hong et al. 2014; Schneider et al. 2011; Yang et al. 2013; Yi et al. 2017). Furthermore, a publication demonstrated that HOXB3-activated DNMT3B represses TSG RASSF1A (Braconi et al. 2010). Therefore, we can boldly speculate that DNMT3B hypermethylates the oncogene SHOX2 and the TSG RASSF1A in lung cancer.
Notably, miR-375 also targets YAP1, TEA domain family 4 (TEAD4) and connective tissue growth factor (CTGF) (Kang et al. 2018), which are important effectors of the Hippo signaling pathway. As we conclude, miR-375 is a super controller of the Hippo pathway. SHOX2 may cross-talk with the Hippo signaling pathway through miR-375 to induce tumorigenesis and metastasis. More cellular studies are needed to explore the association between microRNAs and SHOX2 methylation.
EMT is defined as the transformation from epithelial phenotypes to mesenchymal phenotypes, and this transformation is essential for the invasion ability of cancer cells. Some reports have indicated that the SHOX2 gene is a novel EMT inducer. One study showed that ectopic SHOX2 expression promotes the expression of growth factor-beta receptor I (TβR-I), which suggests that transforming growth factor-beta (TGF-β) signaling is essential for the process of SHOX2-induced EMT in mesenchymal breast cancer cells (Hong et al. 2014). Another report demonstrated that ectopic SHOX2 expression reverses the mRNA and protein expression of EMT-related genes, including β-catenin, N-cadherin, E-cadherin, and Vimentin, and induces the proliferation and metastasis of carcinoma in vitro and in vivo (Yi et al. 2017). Furthermore, Lukas Balek et al. (Balek et al. 2018) proved that FGFR3 interacts with the transcriptional regulator SHOX2. The SHOX2 gene is involved in FGF-regulated pathways/events, including the RAS/ERK and PI3K/AKT pathways, stem cell pluripotency relevant signaling pathways, EGFR tyrosine kinase inhibitors resistance, cell proliferation, migration, differentiation and cell phenotypes. The role of SHOX2 in tumors is discussed above and is summarized in Fig. 4.
The clinical application of RASSF1A and SHOX2 in lung cancer auxiliary diagnosis
Since the methylation of the RASSF1A and SHOX2 genes is described as an early and frequent event in tumorigenesis, RASSF1A and SHOX2 could be a pair of valuable biomarkers in lung cancer screening, including NSCLC and SCLC (Burbee et al. 2001; Schmidt et al. 2015). An analysis of current research progress showed that lung tumor patients who exhibit hypermethylation of RASSF1A and SHOX2 showed poor tissue differentiation, more advanced stages, susceptibility to local recurrence, and significantly shortened overall survival and disease-free survival (Bao et al. 2019; Dubois et al. 2016; Grawenda and O'neill 2015; Hong et al. 2014; Malpeli et al. 2019; Peng et al. 2019; Yang et al. 2013; Zhao et al. 2015). Moreover, it has been confirmed that the detection of RASSF1A and SHOX2 methylation is useful for the surveillance of chemotherapy responses in advanced lung cancer patients (De Fraipont et al. 2012; Schmidt et al. 2015). Therefore, we concluded that the methylated RASSF1A and SHOX2 genes may be a powerful pair of biomarkers for tracking tumorigenesis and metastasis in lung cancer.
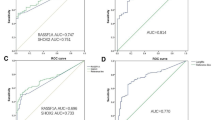
The RASSF1A and SHOX2 methylation assay is a reliable technique for the diagnosis of lung cancer patients whose diagnoses are unclear based on cytological examination or chest CT (Ilse et al. 2014). Recently, the detection of RASSF1A and SHOX2 methylation has been clinically available for the auxiliary diagnosis of lung cancer by alveolar lavage fluid samples. Other types of samples, such as plasma, bronchoalveolar lavage fluid, pleural effusion, lymph node, and tumor tissue of lung cancer patients, are also under investigation (Ren et al. 2017; Zhang et al. 2017; Zhao et al. 2015). The sensitivity and specificity of methylated RASSF1A for lung cancer diagnosis from serum or sputum samples were just 45% (95% CI: 0.41–0.48) (random effects) and as high as 99% (95% CI: 0.98–1.00) (fixed effects) (Zhang et al. 2019). A meta-analysis (Zhao et al. 2015) reported that SHOX2 methylation has a moderate sensitivity of 70% (95% CI: 0.46–0.87) but with unexceptionable specificity of 96% (95% CI: 0.91–0.99) (AUC = 0.96), supporting its value for confirming benignity for negative results. The low diagnostic sensitivity of testing methylated RASSF1A or SHOX2 separately limited the application to lung cancer screening. However, the combined detection of RASSF1A and SHOX2 methylation sharply increased the sensitivity to 81.0% and almost maintained the original high specificity (AUC = 0.892) (Zhang et al. 2017). Interestingly, the combination of methylation detection and cytology detection further increased the sensitivity to 93.0% (Zhang et al. 2017). In addition, based on all the types of samples listed above, the SHOX2 and RASSF1A methylation assay has remarkably higher sensitivity than the traditional serum-based biomarkers, CT and positron emission tomography/computed tomography (PET–CT) for diagnosing lung cancer in the early stage. The most common serum-based biomarkers, including CEA, CYFRA 21–1, SCC, and NSE, had sensitivities of 47.5%, 47.5%, 49%, and 39.7%, respectively (Chu et al. 2011), pulmonary nodules detected by screening with low-dose computed tomography (LDCT) displayed a low lung cancer prevalence of 5.5% (Mcwilliams et al. 2013), and the PET–CT in lung cancer in lung disease patients was 93.5% (Feng et al. 2017). PET–CT is an invasive, radiative, and expensive diagnostic technique, so it is not suitable for early screening for lung cancer. However, the detection of SHOX2 and RASSF1A methylation did not have the disadvantages of the detection methods described above.
Therefore, by comparing these validations with the above data, the SHOX2 and RASSF1A methylation assays might be an excellent option for auxiliary lung cancer diagnosis or screening.
Conclusions and perspective
In various cancers, including lung cancer, esophageal cancer, gastric carcinoma, prostatic cancer, APL, breast cancer, hepatocellular carcinoma, and colorectal cancer, RASSF1A is a TSG that is widely silenced by hypermethylation, while SHOX2 is an oncogene that is broadly overexpressed and hypermethylated (Bräuer-Hartmann et al. 2015; Byun et al. 2001; Fernandes et al. 2013; Li et al. 2018; Li et al. 2012; Ren et al. 2017; Yang et al. 2010). The loss of RASSF1A and the high expression of SHOX2 play important roles in the regulation of the occurrence, apoptosis, and transformation of lung cancer cells. Numerous studies have shown that these two genes act as regulators or effectors of multiple cancer signaling pathways, driving cancer progression. RASSF1A is a key regulator of the Hippo pathway and couples this pathway to the TNF-α, NF-κB, and TGF-β signaling pathways. In the synergistic action of the inflammatory cytokines, P53 and K-RAS, the epigenetic loss of RASSF1A crosslinks a series of important cancer signaling pathways and plays an essential role in carcinogenesis and metastasis. SHOX2, due to its complex relationship with certain microRNAs, may cross-talk with the Hippo, EMT, RAS/ERK MAPK and PI3K/AKT pathways, which are critical for tumorigenesis, metastasis, and occurrence of lung cancer. The combined detection of RASSF1A and SHOX2 methylation, with its high sensitivity and specificity, may provide an unexceptionable biomarker pair for lung cancer screening and progression monitoring.
SHOX2 is capable of binding to the TGF receptor and cross-talk with the NF-κB pathway, suggesting a mutual regulatory relationship with RASSF1A. The close relationship between RASSF1A and SHOX2 and the Hippo, NF-kB, and TGF-β pathways may provide new insights into how we can interfere with these pathways or factors to produce benefits. Further study on the crosstalk and crossover between these two genes and cancer signaling pathways is very important for a better understanding of their functional implications and therapeutic effects in lung cancer. As described above, more scientists are necessary to conduct clinical and basic research to further understand the biological functions of RASSF1A and SHOX2 and to improve the methods of their detection. It is expected that these markers can increase the accuracy of screening lung cancer patients to improve the 5-year survival rate and guide personalized clinical medication in a timely manner.
References
Abu-Remaileh M et al (2015) Chronic inflammation induces a novel epigenetic program that is conserved in intestinal adenomas and in colorectal cancer. Cancer Res 75:2120–2130. https://doi.org/10.1158/0008-5472.CAN-14-3295
Alanazi IO, AlYahya SA, Ebrahimie E, Mohammadi-Dehcheshmeh M (2018) Computational systems biology analysis of biomarkers in lung cancer; unravelling genomic regions which frequently encode biomarkers, enriched pathways, and new candidates. Gene 659:29–36. https://doi.org/10.1016/j.gene.2018.03.038
Aza-Carmona M et al (2011) SHOX interacts with the chondrogenic transcription factors SOX5 and SOX6 to activate the aggrecan enhancer. Hum Mol Genet 20:1547–1559. https://doi.org/10.1093/hmg/ddr032
Aza-Carmona M et al (2014) NPPB and ACAN, two novel SHOX2 transcription targets implicated in skeletal development. PLoS ONE 9:e83104. https://doi.org/10.1371/journal.pone.0083104
Balek L et al (2018) Proteomic analyses of signalling complexes associated with receptor tyrosine kinase identify novel members of fibroblast growth factor receptor 3 interactome. Cell Signal 42:144–154. https://doi.org/10.1016/j.cellsig.2017.10.003
Baniwal SK et al (2010) Runx2 transcriptome of prostate cancer cells: insights into invasiveness and bone metastasis. Mol Cancer 9:258. https://doi.org/10.1186/1476-4598-9-258
Bao Y, Liu X, Liu Y, Wang S, Wu B (2019) Ras-association domain family 1 (RASSF1A) gene regulates progression, migration and invasion of bladder cancer. Surg Oncol Oxf 30:63–71
Baubec T et al (2015) Genomic profiling of DNA methyltransferases reveals a role for DNMT3B in genic methylation. Nature 520:243–247. https://doi.org/10.1038/nature14176
Bi L et al (2018) A novel miR-375-HOXB3-CDCA3/DNMT3B regulatory circuitry contributes to leukemogenesis in acute myeloid leukemia. BMC Cancer 18:182. https://doi.org/10.1186/s12885-018-4097-z
Blaschke RJ et al (1998) SHOT, a SHOX-related homeobox gene, is implicated in craniofacial, brain, heart, and limb development. Proc Natl Acad Sci USA 95:2406–2411
Blumenthal GM et al (2018) Current status and future perspectives on neoadjuvant therapy in lung cancer. J Thorac Oncol 13:1818–1831. https://doi.org/10.1016/j.jtho.2018.09.017
Bobick BE, Cobb J (2012) Shox2 regulates progression through chondrogenesis in the mouse proximal limb. J Cell Sci 125:6071–6083. https://doi.org/10.1242/jcs.111997
Bonafe L et al (2015) Nosology and classification of genetic skeletal disorders: 2015 revision. Am J Med Genet A 167A:2869–2892. https://doi.org/10.1002/ajmg.a.37365
Boncinelli E (1997) Homeobox genes and disease. Curr Opin Genet Dev 7:331–337. https://doi.org/10.1016/s0959-437x(97)80146-3
Braconi C, Huang N, Patel T (2010) MicroRNA-dependent regulation of DNA methyltransferase-1 and tumor suppressor gene expression by interleukin-6 in human malignant cholangiocytes. Hepatology 51:881–890. https://doi.org/10.1002/hep.23381
Bräuer-Hartmann D et al (2015) PML/RARα-regulated miR-181a/b cluster targets the tumor suppressor RASSF1A in acute promyelocytic leukemia. Cancer Res 75:3411–3424
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Burbee DG et al (2001) Epigenetic inactivation of RASSF1A in lung and breast cancers and malignant phenotype suppression. J Natl Cancer Inst 93:691–699
Byun D, Lee M, Chae KS, Ryu B, Chi SJCR (2001) Frequent epigenetic inactivation of RASSF1A by aberrant promoter hypermethylation in human gastric. Adenocarcinoma 61:7034–7038
Chen T, Sun Z, Liu F, Wang Q (2017) RASSF1A and SIRT6 in non-small cell lung cancer: Relationship with clinical outcome. Oncol Lett 14:5759–5764. https://doi.org/10.3892/ol.2017.6172
Chu X, Hou X, Song W, Xue Z, Wang B, Zhang LJCB, Therapy (2011) Diagnostic values of SCC, CEA, Cyfra21–1 and NSE for lung cancer in patients with suspicious pulmonary masses: a single center analysis 11:995–1000
Clement-Jones M et al (2000) The short stature homeobox gene SHOX is involved in skeletal abnormalities in turner syndrome. Hum Mol Genet 9:695–702
Dabral S et al (2019) A RASSF1A-HIF1alpha loop drives Warburg effect in cancer and pulmonary hypertension. Nat Commun 10:2130. https://doi.org/10.1038/s41467-019-10044-z
Dalle Carbonare L, Innamorati G, Valenti MT (2012) Transcription factor Runx2 and its application to bone tissue engineering. Stem Cell Rev Rep 8:891–897. https://doi.org/10.1007/s12015-011-9337-4
Darwiche K et al (2013) Assessment of SHOX2 methylation in EBUS-TBNA specimen improves accuracy in lung cancer staging. Ann Oncol 24:2866–2870
Deans CA, Maggert KAJG (2015) What do you mean, “Epigenetic”? 199:887–896
Dela Cruz CS, Tanoue LT, Matthay RA (2011) Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med 32:605–644. https://doi.org/10.1016/j.ccm.2011.09.001
De Baere E, Speleman F, Van Roy N, De Paepe A, Messiaen LJC, Research G (1998) Assignment of SHOX2 (alias OG12X and SHOT) to human chromosome bands 3q25 -%3e q26.1 by in situ hybridization 82:228–229
De Fraipont F et al (2012) An apoptosis methylation prognostic signature for early lung cancer in the IFCT-0002. Trial 18:2976–2986
Donninger H, Vos MD, Clark GJ (2007) The RASSF1A tumor suppressor. J Cell Sci 120:3163–3172. https://doi.org/10.1242/jcs.010389
Donninger H, Schmidt ML, Mezzanotte J, Barnoud T, Clark GJ (2016) Ras signaling through RASSF proteins. Semin Cell Dev Biol 58:86–95. https://doi.org/10.1016/j.semcdb.2016.06.007
Dubois F et al. (2016) RASSF1A Suppresses the Invasion and metastatic potential of human non–small cell lung cancer cells by inhibiting YAP activation through the GEF-H1/RhoB pathway 76:1627–1640
Dubois F et al (2019) Role of the YAP-1 transcriptional target cIAP2 in the differential susceptibility to chemotherapy of non-small-cell lung cancer (NSCLC) patients with tumor RASSF1A gene methylation from the phase 3 IFCT-0002 trial. Cancers (Basel). https://doi.org/10.3390/cancers11121835
Dubois F, Bergot E, Levallet G (2019) Cancer and RASSF1A/RASSF1C, the two faces of Janus. Trends Cancer 5:662–665. https://doi.org/10.1016/j.trecan.2019.10.001
Duruisseaux M (2017) Esteller MJSiCB. Lung cancer epigenetics: From knowledge to applications 51:116–128
Duymich CE, Charlet J, Yang X, Jones PA, Liang G (2016) DNMT3B isoforms without catalytic activity stimulate gene body methylation as accessory proteins in somatic cells. Nat Commun 7:11453. https://doi.org/10.1038/ncomms11453
Esteller MJO (2002) CpG island hypermethylation and tumor suppressor genes: a booming present, a brighter future 21:5427–5440
Feng H, Zhang Z, Qing X, Wang X, Liang C, Liu DJE, Pathology M (2016) Promoter methylation of APC and RAR-β genes as prognostic markers in non-small cell lung cancer (NSCLC). EXP Mol Biol 100:109–113
Feng M, Yang X, Ma Q, He YJM (2017) Retrospective analysis for the false positive diagnosis of PET-CT scan in lung cancer patients 96
Fernandes MS, Carneiro F, Oliveira C, Seruca R (2013) Colorectal cancer and RASSF family–a special emphasis on RASSF1A. Int J Cancer 132:251–258. https://doi.org/10.1002/ijc.27696
Foran E, Garrity-Park MM, Mureau C, Newell J, Smyrk TC, Limburg PJ, Egan LJ (2010) Upregulation of DNA methyltransferase-mediated gene silencing, anchorage-independent growth, and migration of colon cancer cells by interleukin-6. Mol Cancer Res 8:471–481. https://doi.org/10.1158/1541-7786.MCR-09-0496
Gagliardi M, Strazzullo M, Matarazzo MR (2018) DNMT3B functions: novel insights from human disease. Front Cell Dev Biol 6:140. https://doi.org/10.3389/fcell.2018.00140
Gehring WJ, Affolter M, Burglin T (1994) Homeodomain proteins. Annu Rev Biochem 63:487–526. https://doi.org/10.1146/annurev.bi.63.070194.002415
Gordon M et al. (2013) The tumor suppressor gene, RASSF1A, is essential for protection against inflammation-induced injury. PloS one 8
Grawenda A, O'neill E (2015) Clinical utility of RASSF1A methylation in human malignancies. Br J Ccancer 113:372–381
Heyn H, Esteller M (2012) DNA methylation profiling in the clinic: applications and challenges. Nat Rev Genet 13:679–692. https://doi.org/10.1038/nrg3270
Hong S et al (2014) SHOX2 is a direct miR-375 target and a novel epithelial-to-mesenchymal transition inducer in breast cancer cells. Neoplasia 16(279–290):e275
Hristov G, Marttila T, Durand C, Niesler B, Rappold G, Marchini AJHMG (2014) SHOX triggers the lysosomal pathway of apoptosis via oxidative. Stress 23:1619–1630
Hsu YL, Huang MS, Yang CJ, Hung JY, Wu LY, Kuo PL (2011) Lung tumor-associated osteoblast-derived bone morphogenetic protein-2 increased epithelial-to-mesenchymal transition of cancer by Runx2/Snail signaling pathway. J Biol Chem 286:37335–37346. https://doi.org/10.1074/jbc.M111.256156
Hu W, Xin Y, Zhao Y, Hu J (2018) Shox2: the role in differentiation and development of cardiac conduction system Tohoku. J Exp Med 244:177–186. https://doi.org/10.1620/tjem.244.177
Huang X et al (2016) Decitabine and 5-azacitidine both alleviate LPS induced ARDS through anti-inflammatory/antioxidant activity and protection of glycocalyx and inhibition of MAPK pathways in mice. Biomed Pharmacother 84:447–453. https://doi.org/10.1016/j.biopha.2016.09.072
Huang J, Chen YX, Zhang B (2019) IGF2-AS affects the prognosis and metastasis of gastric adenocarcinoma via acting as a ceRNA of miR-503 to regulate SHOX2. Gastric Cancer. https://doi.org/10.1007/s10120-019-00976-2
Huang J et al (2019) Enhanced osteopontin splicing regulated by RUNX2 is HDAC-dependent and induces invasive phenotypes in NSCLC cells. Cancer Cell Int 19:306. https://doi.org/10.1186/s12935-019-1033-5
Ilse P, Biesterfeld S, Pomjanski N, Wrobel C, Schramm MJCG, Proteomics (2014) Analysis of SHOX2 methylation as an aid to cytology in lung cancer. Diagnosis 11:251–258
Ionta V, Liang W, Kim EH, Rafie R, Giacomello A, Marban E, Cho HC (2015) SHOX2 overexpression favors differentiation of embryonic stem cells into cardiac pacemaker cells, improving biological pacing ability. Stem Cell Rep 4:129–142. https://doi.org/10.1016/j.stemcr.2014.11.004
Iwasa H, Hossain S, Hata Y (2018) Tumor suppressor C-RASSF proteins. Cell Mol Life Sci 75:1773–1787. https://doi.org/10.1007/s00018-018-2756-5
Johnson JE et al (2007) Differential membrane binding and diacylglycerol recognition by C1 domains of RasGRPs. Biochem J 406:223–236. https://doi.org/10.1042/BJ20070294
Kang W et al (2018) miR-375 is involved in Hippo pathway by targeting YAP1/TEAD4-CTGF axis in gastric carcinogenesis. Cell Death Dis 9:92. https://doi.org/10.1038/s41419-017-0134-0
Keller M et al (2019) NDR2 kinase contributes to cell invasion and cytokinesis defects induced by the inactivation of RASSF1A tumor-suppressor gene in lung cancer cells. J Exp Clin Cancer Res 38:158. https://doi.org/10.1186/s13046-019-1145-8
Kilili GK, Kyriakis JMJJBC (2010) Mammalian Ste20-like kinase (Mst2) indirectly supports Raf-1/ERK pathway activity Via maintenance of protein phosphatase-2A catalytic subunit levels and consequent suppression of inhibitory Raf-1. Phosphorylation 285:15076–15087
Kneip C et al (2011) SHOX2 DNA methylation is a biomarker for the diagnosis of lung cancer in plasma 6:1632–1638
Koyama S et al (2016) STK11/LKB1 deficiency promotes neutrophil recruitment and proinflammatory cytokine production to suppress T-cell activity in the lung tumor microenvironment. Cancer Res 76:999–1008. https://doi.org/10.1158/0008-5472.CAN-15-1439
Laird PW (2003) The power and the promise of DNA methylation markers. Nat Rev Cancer 3:253–266. https://doi.org/10.1038/nrc1045
Lee MG et al (2016) RASSF1A directly antagonizes RhoA activity through the assembly of a Smurf1-mediated destruction complex to suppress tumorigenesis. Cancer Res 76:1847–1859. https://doi.org/10.1158/0008-5472.CAN-15-1752
Leiro V, De Chiara L, Rodriguez-Girondo M, Botana-Rial M, Valverde D, Nunez-Delgado M, Fernandez-Villar A (2019) Methylation assessment for the prediction of malignancy in mediastinal adenopathies obtained by endobronchial ultrasound-guided transbronchial needle aspiration in patients with lung cancer. Cancers (Basel). https://doi.org/10.3390/cancers11101408
Li Q, Zhu F, Chen PJB, Communications BR (2012) miR-7 and miR-218 epigenetically control tumor suppressor genes RASSF1A and Claudin-6 by targeting HoxB3 in breast. Cancer 424:28–33
Li L et al (2018) Epigenomic characterization of a p53-regulated 3p22.2 tumor suppressor that inhibits STAT3 phosphorylation via protein docking and is frequently methylated in esophageal and other. Carcinomas 8:61–77
Liao A, Tan G, Chen L, Zhou W, Hu HJO (2016) RASSF1A inhibits gastric cancer cell proliferation by miR-711- mediated downregulation of CDK4 expression 7:5842–5851
Licchesi JD, Westra WH, Hooker CM, Herman JG (2008) Promoter hypermethylation of hallmark cancer genes in atypical adenomatous hyperplasia of the lung. Clin Cancer Res 14:2570–2578. https://doi.org/10.1158/1078-0432.CCR-07-2033
Lin JJ, Shaw AT (2016) Resisting resistance: targeted therapies in lung cancer trends. Cancer 2:350–364. https://doi.org/10.1016/j.trecan.2016.05.010
Lucic I, Truebestein L, Leonard TA (2016) Novel features of DAG-activated PKC isozymes reveal a conserved 3-D architecture. J Mol Biol 428:121–141. https://doi.org/10.1016/j.jmb.2015.11.001
Malpeli G et al (2019) Methylation dynamics of RASSF1A and its impact on cancer. Cancers 11:959
Marchini A, Ogata T, Rappold GA (2016) A track record on SHOX: from basic research to complex models and therapy. Endocr Rev 37:417–448
Markopoulos GS, Roupakia E, Marcu KB, Kolettas E (2019) Epigenetic regulation of inflammatory cytokine-induced epithelial-to-mesenchymal cell transition and cancer. Stem Cell Gen Cell. https://doi.org/10.3390/cells8101143
Mcwilliams A et al (2013) Probability of cancer in pulmonary nodules detected on first screening CT. Cancer 369:910–919
Mehta A, Dobersch S, Romero-Olmedo AJ, Barreto G (2015) Epigenetics in lung cancer diagnosis and therapy. Cancer Metastasis Rev 34:229–241. https://doi.org/10.1007/s10555-015-9563-3
Mortensen KH, Andersen NH, Gravholt CHJER (2012) Cardiovascular phenotype in turner syndrome—integrating cardiology. Gene Endocrinol 33:677–714
Niklinska W, Naumnik W, Sulewska A, Kozłowski M, Pankiewicz W, Milewski R (2009) Prognostic significance of DAPK and RASSF1A promoter hypermethylation in non-small cell lung cancer (NSCLC). Folia histochemica et cytobiologica 47:275–280
Ogushi K et al (2019) DNA Methylation Status of SHOX-Flanking CpG Islands in Healthy Individuals and Short Stature Patients with Pseudoautosomal Copy Number Variations Cytogenetic and genome research 158:56–62
Oh MH, Lockwood WW (2017) RASSF1A methylation, YAP1 activation and metastasis: a new role for an old foe in lung cancer. J Thoracic Dis 9:1165–1167. https://doi.org/10.21037/jtd.2017.04.16
Ooki A et al (2017) A panel of novel detection and prognostic methylated DNA markers in primary non-small cell lung cancer and serum DNA. Clin Cancer Res 23:7141–7152. https://doi.org/10.1158/1078-0432.CCR-17-1222
Ortizvega S, Khokhlatchev A, Nedwidek M, Zhang X, Dammann R, Pfeifer GP, Avruch JJO (2002) The putative tumor suppressor RASSF1A homodimerizes and heterodimerizes with the Ras-GTP binding protein Nore1 21:1381–1390
Ozaki T, Wu D, Sugimoto H, Nagase H, Nakagawara A (2013) Runt-related transcription factor 2 (RUNX2) inhibits p53-dependent apoptosis through the collaboration with HDAC6 in response to DNA damage. Cell Death Dis 4:e610. https://doi.org/10.1038/cddis.2013.127
Ozaki T, Yu M, Yin D, Sun D, Zhu Y, Bu Y, Sang M (2018) Impact of RUNX2 on drug-resistant human pancreatic cancer cells with p53 mutations. BMC Cancer 18:309. https://doi.org/10.1186/s12885-018-4217-9
Pallares J et al (2008) Promoter hypermethylation and reduced expression of RASSF1A are frequent molecular alterations of endometrial carcinoma. Mod Pathol 21:691–699. https://doi.org/10.1038/modpathol.2008.38
Pankova D et al (2019) RASSF1A controls tissue stiffness and cancer stem-like cells in lung adenocarcinoma. EMBO J 38:e100532. https://doi.org/10.15252/embj.2018100532
Papaspyropoulos A et al (2018) RASSF1A uncouples Wnt from Hippo signalling and promotes YAP mediated differentiation via p73. Nat Commun 9:424. https://doi.org/10.1038/s41467-017-02786-5
Pefani DE, Pankova D, Abraham AG, Grawenda AM, Vlahov N, Scrace SEON (2016) TGF-beta targets the hippo pathway scaffold RASSF1A to facilitate YAP/SMAD2 nuclear translocation. Mol Cell 63:156–166. https://doi.org/10.1016/j.molcel.2016.05.012
Peng X, Liu X, Xu L, Li Y, Wang H, Song L, Xiao W (2019) The mSHOX2 is capable of assessing the therapeutic effect and predicting the prognosis of stage IV lung cancer. J Thoracic Dis 11:2458
Puskaric S et al (2010) Shox2 mediates Tbx5 activity by regulating Bmp4 in the pacemaker region of the developing heart. Hum Mol Genet 19:4625–4633. https://doi.org/10.1093/hmg/ddq393
Qu Z, Sun F, Zhou J, Li L, Shapiro SD, Xiao G (2015) Interleukin-6 prevents the initiation but enhances the progression of lung cancer. Cancer Res 75:3209–3215. https://doi.org/10.1158/0008-5472.CAN-14-3042
Ram R, Mendiratta S, Bodemann BO, Torres MJ, Eskiocak U, White MAJM, Biology C (2014) RASSF1A inactivation unleashes a tumor suppressor/oncogene cascade with context-dependent consequences on cell cycle progression 34:2350–2358
Ren M, Wang C, Sheng D, Shi Y, Jin M, Xu S (2017) Methylation analysis of SHOX2 and RASSF1A in bronchoalveolar lavage fluid for early lung cancer diagnosis. Ann Diagn Pathol 27:57–61
Richter AM, Pfeifer GP, Dammann RH (2009) The RASSF proteins in cancer; from epigenetic silencing to functional characterization. Biochim Biophys Acta 1796:114–128. https://doi.org/10.1016/j.bbcan.2009.03.004
Robertson KD (2005) DNA methylation and human disease. Nat Rev Genet 6:597–610. https://doi.org/10.1038/nrg1655
Romano D, Nguyen LK, Matallanas D, Halasz M, Doherty C, Kholodenko BN, Kolch W (2014) Protein interaction switches coordinate Raf-1 and MST2/Hippo signalling. Nat Cell Biol 16:673–684. https://doi.org/10.1038/ncb2986
Rosin JM, McAllister BB, Dyck RH, Percival CJ, Kurrasch DM, Cobb J (2015) Mice lacking the transcription factor SHOX2 display impaired cerebellar development and deficits in motor coordination. Dev Biol 399:54–67. https://doi.org/10.1016/j.ydbio.2014.12.013
Rovescalli A, Asoh S, Nirenberg MW (1996) Cloning and characterization of four murine homeobox genes. Proc Natl Acad Sci USA 93:10691–10696
Sawada R, Kamei H, Hakuno F, Takahashi S, Shimizu TJDD (2015) In vivo loss of function study reveals the short stature homeobox-containing (shox) gene plays indispensable roles in early embryonic growth and bone formation in zebrafish 244:146–156
Schmidt B, Beyer J, Dietrich D, Bork I, Liebenberg V, Fleischhacker M (2015) Quantification of cell-free mSHOX2 plasma DNA for therapy monitoring in advanced stage non-small cell (NSCLC) and small-cell lung cancer (SCLC) patients. PLoS One 10
Schmidt ML, Hobbing KR, Donninger H, Clark GJ (2018) RASSF1A deficiency enhances RAS-driven lung tumorigenesis. Cancer Res 78:2614–2623. https://doi.org/10.1158/0008-5472.CAN-17-2466
Schneider KU et al (2011) Correlation of SHOX2 gene amplification and DNA methylation in lung cancer. Tumors 11:102–102
Semina EV, Reiter RS, Murray JCJHMG (1998) A new human homeobox gene OGI2X is a member of the most conserved homeobox gene family and is expressed during heart development in mouse 7:415–422
Sherwood V, Recino A, Jeffries A, Ward A, Chalmers AD (2009) The N-terminal RASSF family: a new group of Ras-association-domain-containing proteins, with emerging links to cancer formation. Biochem J 425:303–311. https://doi.org/10.1042/BJ20091318
Song L, Yu H, Li Y (2015) Diagnosis of lung cancer by SHOX2 gene methylation assay. Mol Diagn Ther 19:159–167. https://doi.org/10.1007/s40291-015-0144-5
Strzelak A, Ratajczak A, Adamiec A, Feleszko W (2018) Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: a mechanistic review. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15051033
Sun C, Liu XH, Sun YR (2019) MiR-223–3p inhibits proliferation and metastasis of oral squamous cell carcinoma by targeting SHOX2. Eur Rev Med Pharmacol Sci 23:6927–6934. https://doi.org/10.26355/eurrev_201908_18732
Tan X et al (2013) Loss of p53 attenuates the contribution of IL-6 deletion on suppressed tumor progression and extended survival in Kras-driven murine lung cancer. PLoS ONE 8:e80885. https://doi.org/10.1371/journal.pone.0080885
Thaler S, Hahnel PS, Schad A, Dammann R, Schuler M (2009) RASSF1A mediates p21Cip1/Waf1-dependent cell cycle arrest and senescence through modulation of the Raf-MEK-ERK pathway and inhibition of Akt. Cancer Res 69:1748–1757. https://doi.org/10.1158/0008-5472.CAN-08-1377
Thaler S, Schmidt M, Schad A, Sleeman JP (2012) RASSF1A inhibits estrogen receptor alpha expression and estrogen-independent signalling: implications for breast cancer development. Oncogene 31:4912–4922. https://doi.org/10.1038/onc.2011.658
Timp W, Feinberg AP (2013) Cancer as a dysregulated epigenome allowing cellular growth advantage at the expense of the host. Nat Rev Cancer 13:497–510. https://doi.org/10.1038/nrc3486
Tommasi S, Besaratinia A, Wilczynski SP, Pfeifer GPJO (2011) Loss of Rassf1a enhances p53-mediated tumor predisposition and accelerates progression to aneuploidy 30:690–700
Van Schaick HSA et al. (1997) Homeobox gene Prx3 expression in rodent brain and extraneural tissues 94:12993–12998
Valenti MT, Serafini P, Innamorati G, Gili A, Cheri S, Bassi C, Dalle Carbonare L (2016) Runx2 expression: a mesenchymal stem marker for cancer. Oncol Lett 12:4167–4172. https://doi.org/10.3892/ol.2016.5182
Volodko N, Gordon M, Salla M, Ghazaleh HA, Baksh S (2014) RASSF tumor suppressor gene family: biological functions and regulation. FEBS Lett 588:2671–2684. https://doi.org/10.1016/j.febslet.2014.02.041
Volodko N et al (2016) RASSF1A site-specific methylation hotspots in cancer and correlation with RASSF1C and MOAP-1. Cancers (Basel). https://doi.org/10.3390/cancers8060055
Vos MD et al (2006) The RASSF1A tumor suppressor activates Bax via MOAP-1. J Biol Chem 281:4557–4563. https://doi.org/10.1074/jbc.M512128200
Wang H et al (2011) MicroRNA-342 inhibits colorectal cancer cell proliferation and invasion by directly targeting DNA methyltransferase 1. Carcinogenesis 32:1033–1042. https://doi.org/10.1093/carcin/bgr081
Weng Z et al. (1995) Structure-function analysis of SH3 domains: SH3 binding specificity altered by single amino acid substitutions 15:5627–5634
Xie J, Yu F, Li D, Zhu X, Zhang X, Lv Z (2016) MicroRNA-218 regulates cisplatin (DPP) chemosensitivity in non-small cell lung cancer by targeting RUNX2. Tumour Biol 37:1197–1204. https://doi.org/10.1007/s13277-015-3831-2
Yang L, Ma Z, Wang D, Zhao W, Chen L, Wang G (2010) MicroRNA-602 regulating tumor suppressive gene RASSF1A is overexpressed in hepatitis B virus-infected liver and hepatocellular carcinoma. Cancer Biol Ther 9:803–808. https://doi.org/10.4161/cbt.9.10.11440
Yang T et al (2013) Elevated SHOX2 expression is associated with tumor recurrence of hepatocellular carcinoma. Ann Surg Oncol 20:644–649
Yang X, Han H, De Carvalho DD, Lay FD, Jones PA, Liang G (2014) Gene body methylation can alter gene expression and is a therapeutic target in cancer. Cancer Cell 26:577–590. https://doi.org/10.1016/j.ccr.2014.07.028
Yang L et al (2015) Mutations of p53 and KRAS activate NF-kappaB to promote chemoresistance and tumorigenesis via dysregulation of cell cycle and suppression of apoptosis in lung cancer cells. Cancer Lett 357:520–526. https://doi.org/10.1016/j.canlet.2014.12.003
Yi J, Jin L, Chen J, Feng B, He Z, Chen L, Song H (2017) MiR-375 suppresses invasion and metastasis by direct targeting of SHOX2 in esophageal squamous cell carcinoma. Acta Biochim Biophys Sin (Shanghai) 49:159–169. https://doi.org/10.1093/abbs/gmw131
Yi M et al (2018) Dual-functionality of RASSF1A overexpression in A375 cells is mediated by activation of IL-6/STAT3 regulatory loop. Mol Biol Rep 45:1277–1287. https://doi.org/10.1007/s11033-018-4288-3
Yu L, Liu H, Yan M, Yang J, Long F, Muneoka K, Chen Y (2007) Shox2 is required for chondrocyte proliferation and maturation in proximal limb skeleton. Dev Biol 306:549–559. https://doi.org/10.1016/j.ydbio.2007.03.518
Yu J et al (2018) MicroRNA181a promotes cell proliferation and inhibits apoptosis in gastric cancer by targeting RASSF1A. Oncol Rep 40:1959–1970. https://doi.org/10.3892/or.2018.6632
Zhang X et al (2015a) Runx2-Smad signaling impacts the progression of tumor-induced bone disease. Int J Cancer 136:1321–1332. https://doi.org/10.1002/ijc.29094
Zhang X et al (2015b) Expression of the IL-11 gene in metastatic cells is supported by Runx2-Smad and Runx2-cJun complexes induced by TGFbeta1. J Cell Biochem 116:2098–2108. https://doi.org/10.1002/jcb.25167
Zhang C et al (2017) DNA methylation analysis of the SHOX2 and RASSF1A panel in bronchoalveolar lavage fluid for lung cancer diagnosis. J Cancer 8:3585
Zhang Z, Yan S, Cui H, Chen H, Liu JJMSM (2019) Correlation BETWEEN RASSF1A gene promoter hypermethylation in serum or sputum and non-small cell lung cancer (NSCLC): a meta-analysis 25:5518–5524
Zhao Q et al (2015) Diagnostic value of SHOX2 DNA methylation in lung cancer: a meta-analysis 8:3433–3439
Zhu KW, Liu Q, Zhou Y, Tao C, Zhao Z, Sun J, Xu HJBG (2015) Oncogenes and tumor suppressor genes: comparative genomics and network perspectives 16:1–11
Funding
The work was supported by the National Natural Science Foundation of China (81572610) and the "Yangfan Plan" for Outstanding Scholars in Guangdong Province (4YF16002G).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, N., Zeng, Y. & Huang, J. Signaling pathways and clinical application of RASSF1A and SHOX2 in lung cancer. J Cancer Res Clin Oncol 146, 1379–1393 (2020). https://doi.org/10.1007/s00432-020-03188-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03188-9