Abstract
Purpose
Adjuvant therapies for non-metastatic renal cell carcinoma (nmRCC) are being tested to improve outcomes in patients with high-risk (hR) nmRCC. The objective of the current study is to test the ability of three hR features to identify patients who are at the highest risk of cancer-specific mortality (CSM) after partial or radical nephrectomy.
Methods
Within the Surveillance Epidemiology and End Results (SEER) database (1988–2013), we identified 23,632 nm “clear cell” RCC partial or radical nephrectomy patients with hR features: Fuhrman grade (FG) 3 or 4 or pathological classifications T3a or T3b or lymph node invasion (LNI), or combination of these. Kaplan–Meier analyses (KM) and multivariable Cox’s regression models (CRM) evaluated the effect of hR features on CSM.
Results
Overall 11,568 (48.9%) patients harbored FG3-4, 5575 (23.6%) pT3a/b, 140 (0.6%) LNI, 5366 (22.7%) FG3-4 and pT3a/b, 183 (0.8%) LNI and pT3a/b, 203 (0.9%) LNI and FG3-4 and 597 (2.5%) LNI, FG3-4 and pT3a/b. Median CSM-free survival was 51, 58 and 22 months for LNI and pT3a/b, for LNI and FG3-4 and for LNI, FG3-4 and pT3a/b and was not reached for the other groups. These results remained unchanged in multivariable CRMs, where all hR features represented independent predictors.
Conclusions
Individuals with combination of LNI with FG3-4 or pT3a/b and patients with all three hR features are at highest risk of CSM. In consequence, these patients may represent ideal candidates for adjuvant therapy either in clinical practice or future prospective trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Of patients treated with partial or radical nephrectomy for non-metastatic renal cell carcinoma (nmRCC), 24–47% were considered high risk (hR) according to the authors of the CORONA study [1]. Within that study, hR was defined according to TNM classification, Fuhrman Grade (FG), histological subtype and tumor size. Others [2] defined hR features as tumor size > 5 cm, presence of necrosis and pathological classification > pT2. Regardless of the tumor classification used, hR nmRCC patients have invariably shown worse cancer control outcomes than their non-hR counterparts. However, the reported cancer control outcomes are highly variable according to hR feature type and/or combination of two or three concomitant hR features.
In consequence, the individual and/or combined effect of hR feature(s) on cancer-specific mortality (CSM) require a reappraisal, especially in the context of one contemporary randomized control trial that showed disease-free survival (DFS) benefit with the use of adjuvant sunitinib after nephrectomy relative to placebo [3]. Specifically, it may be hypothesized that one hR feature or a combination of multiple hR features may identify patients that could benefit the most of adjuvant therapy after nephrectomy. In consequence, the aim of this study was to quantify the absolute CSM rates for specific hR feature subgroups.
Materials and methods
The current study relied on the Surveillance Epidemiology and End Results (SEER) database. The SEER database approximately represents a 26% sample of the US population and approximates the United States in terms of demographic composition, as well as of cancer incidence and mortality [4].
In the SEER database, we focused on subjects over 18 years old, diagnosed between 1988 and 2013 with histologically confirmed RCC [International Classification of Disease for Oncology (ICD-O-3), site code C64.9]. All were treated with partial or radical nephrectomy. The hR pathological features were defined as FG3-4 or pathological classifications T3a/b, or LNI (pN1) or a combination of these. Only patients with clear cell histology were considered (histologic code 8310 and 8312) [5]. Exclusion criteria consisted of bilateral RCC, metastatic disease (M1), T3c/T4 classifications and unknown FG, lymph node status, T or M classifications. This resulted in 23,632 assessable patients. CSM was defined according to the SEER mortality code (code 29020).
Variable definition and statistical analyses
Data on age, American Joint Committee on Cancer (AJCC)-based T, N, and M stages [6] were acquired at the time of diagnosis. Additional variables consisted of race (African Americans, White and other), marital status (married, unmarried, unknown), gender and year of surgery. Medians and interquartile ranges, as well as frequencies and proportions were reported for continuous and categorical variables, respectively. The statistical significance of differences in medians and proportions was evaluated with the Kruskal–Wallis and Chi-square tests.
The outcome of interest was CSM. Kaplan–Meier analyses [7] evaluated CSM rates. Univariable and multivariable Cox regression models (CRM) tested for differences in CSM [8]. Covariates were age, ethnicity, gender and marital status. All statistical tests were two-sided with a level of significance set at p < 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.3.0; http://www.r-project.org/).
Results
Overall, we identified 23,632 patients with at least one hR feature and clear cell histology from among 40,374 patients with nmRCC treated with nephrectomy (Table 1). Median age at diagnosis was 62 years (range 53–70). Most were male (15,804; 66.9%), married (15,287; 64.7%) and Caucasian (20,042; 84.8%). Most underwent radical nephrectomy (20,165; 85.3%).
A single hR feature was reported in 17,283 (73.1%) patients: pT3a/b in 5575 (23.6%), FG3-4 in 11,568 (48.9%) and LNI in 140 (0.6%), respectively. A combination of two hR features was reported in 5752 (24.4%) of patients. Of these, 5366 (22.7%) harbored FG3-4 and pT3a/b, 183 (0.8%) LNI and pT3a/b and 203 (0.9%) LNI and FG3-4. The combination of the three hR features was reported in 597 (2.5%) patients.
Median CSM-free survival was 51, 58 and 22 months for patients with LNI and pT3a/b, LNI and FG3-4 and combination of LNI, FG3-4 and pT3a/b, respectively. Median CSM-free survival was not reached for all other groups (Fig. 1).
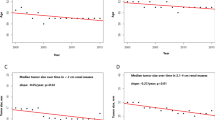
In univariable CRMs, all hR features reached statistical significance for prediction of CSM. In multivariable CRMs, all hR features reached independent predictor status (Table 2) and the three highest hazard ratios (HR) were recorded in patients with combination of LNI, pT3a/b and FG3-4 diseases (HR 9.88); LNI and FG3-4 (HR 5.27); and LNI and pT3-4 (HR 4.89), respectively. The third, second and lowest HRs were recorded in patients with the combination of pT3a/b and FG3-4 (HR 2.98), LNI only (HR 2.86) and pT3a/b only (HR 1.36), respectively. Unknown marital status and gender failed to reach the level of significance. Older age exerted a detrimental effect on CSM (HR 1.02). Conversely, more contemporary-treated patients exhibited lower CSM rates (HR 0.96). Finally, black and unmarried patients experienced worse CSM outcomes (HR 1.18/1.15).
Discussion
Nm clear cell RCC patients with one or several hR features are at highest risk of CSM after partial or radical nephrectomy. In that regard, adjuvant systemic strategies are being evaluated and four trials have been reported conflicting results. Specifically, the ASSURE (sunitinib or sorafenib vs. placebo) [9], the ARISER (girentuximab vs. placebo) [10] and the PROTECT (pazopanib vs. placebo) [11] trials reported negative DFS findings with respect to the addition of adjuvant therapy in the context of hR nmRCC treated with nephrectomy. Conversely, the S-TRAC trial [3] reported a DFS benefit with adjuvant sunitinib after nephrectomy. Some of the controversy surrounding these conflicting results originates from differences in agents tested, from differences in pathological characteristics of enrolled patients with associated CSM risk [12] and from differences in study designs. Specifically, patients enrolled in the ASSURE trial, as well in the S-TRAC and in the PROTECT trials received adjuvant vascular endothelial growth factor receptor-tyrosine kinase inhibitors (VEGFR-TKI: sunitinib, sorafenib or pazopanib) after PN or RN. Conversely, patients enrolled in the ARISER trial were treated with girentuximab, a monoclonal antibody of the carbonic anhydrase IX. Moreover, the number of patients enrolled in the four trials was also considerably different: 619 in the S-TRAC vs. 864 in the ARAISER vs. 1538 in the PROTECT vs. 1943 in the ASSURE trial, respectively. The four trials also differed regarding histology RCC sub-types. In particular, S-TRAC and PROTECT trials only included clear cell nmRCC. Conversly, ASSURE and ARISER trials also included 21 and 6% of non-clear cell nmRCC patients, respectively. Finally, S-TRAC trial only relied on central radiology review for disease-free status. Conversely, in the ASSURE, in the ARISER and in the PROTECT trials, this assessment was performed by investigators only.
Based on this controversy we decided to analyze the effect of hR features on CSM in order to individualize the best candidates to adjuvant therapy. We hypothesized that hR nmRCC patients treated with nephrectomy may display a large array of phenotypes with respect to CSM risk and that one of these three characteristics or one of their combinations may emerge as a predictor of particularly elevated CSM after nephrectomy.
Several noteworthy findings emerged. First, patients with a combination of all three hR features, namely pT3a/b, FG3-4, and LNI, exhibited the highest CSM (median 22 months). They may represent ideal candidates for adjuvant therapy, if such therapy is selected. Alternatively, such individuals represent ideal candidates for inclusion in future adjuvant clinical trials. Inclusion of such hR patients would maximize the potential of such studies to not only demonstrate DFS benefits but also maximize the potential for reporting overall survival benefits. However, such individuals accounted for only 2.5% of hR patients and for even lower proportion of all nephrectomies when non-hR patients are also included. This emphasizes their rarity in every day clinical practice even at high volume tertiary care centers. For example, when approximatively 200 nephrectomies are performed annually, individuals with all three features would account for 2.5% or 5 cases annually if all nephrectomies were performed for hR RCC. In the CORONA study, up to 47% of nephrectomies were performed for hR RCC. This implies that at most 3 of 200 nephrectomy patients were harbored hR features [1].
Second, we identified patients with the combination of two hR features (LNI and FG3-4 or pT3a/b). These individuals exhibited lower, nonetheless highly appreciable risk of CSM after nephrectomy (median 58 and 51 months, respectively). Despite the fact that these values were half as elevated as in the previous highest risk group, these individuals also represent ideal targets for adjuvant therapy and very good candidates for potential inclusion in future trials examining adjuvant therapy after nephrectomy. However, just like their counterparts with all three hR criteria, they account for very few of examined patients: only 1.7% of the hR population.
The combined inclusion of individuals with all three features or of individuals with LNI and a second hR feature (pT3a/b or FG3-4)) only resulted in 4.2% of the hR study cohort. With this in mind, such trials would, therefore, invariably require multi-institutional and/or international involvement of the urological community. Based on the same consideration, the opportunity for clinical use of adjuvant sunitinib outside of protocol setting may also represent a rare opportunity.
Third, it may be postulated that the rarity of patients harboring LNI was largely attributable to decreased rate of lymph node dissection (LND) for nmRCC patients. Kates et al. [13] demonstrated a gradual decline in LND from 1988 in a SEER population. The rate of patients who had > 5 lymph nodes (LN) removed decreased from 10% in 1988 to less than 5% in more contemporary patients. This implies that LNI is frequently underestimated considering the decrease in LND rate and thus increase in pNx status [14]. This is of paramount importance if we consider that in pT3a/b and FG3-4 patient the prevalence of LNI is > 20%, when European cohorts with a higher rate of LND are considered [15]. These evidences may explain why only 4.8% of hR cohort harbored LNI at the time of surgery, as well as why only 4.2% of patients presented all three features or LNI and a second hR feature (pT3a/b or FG3-4).
Fourth, our study of hR individuals treated with nephrectomy shows that the vast majority of such individuals enjoy lengthy CSM-free survival. Specifically, all individuals who did not fall into the two previously discussed hR categories enjoyed median CSM-free survival in excess of 10 years. In consequence, it is difficult to conceptualize the use of adjuvant targeted therapy, with accompanying toxicity that provides at best a 25% reduction in DFS, without overall survival improvement.
To the best of our knowledge, this is the first study that specifically examined pathological hR features and their effect on CSM after nephrectomy, in patients with nmRCC. Nonetheless other studies examined similar endpoints to identify patients at highest risk of CSM. For example, investigators from the University of California in Los Angeles relied on the integrated staging system (UISS) [16, 17] for prediction of CSM in patients with nmRCC using T and N classifications, Fuhrman grade and ECOG-PS. In their analysis, hR nmRCC patients harbored pT3 classification, FG ≥ 2, LNI and had on ECOG ≥ 1. This classification could not be replicated in the current study. ECOG performance status is unavailable in the SEER database and in other similar population databases (NIS [18], NCDB [19]). Similarly, investigators from the Mayo Clinic developed the SSIGN score [2]. Here, hR nmRCC patients harbored tumor size > 5 cm, pT ≥ 2, FG ≥ 3, presence of necrosis and LNI. This classification also could not directly be applied in the current study. Tumor necrosis is unavailable in the SEER database or other population-based datasets. Other hR classification tools were also not applicable for the same reasons [20,21,22].
The clinical implications of our findings are severalfold. First, they provide proof of concept for future studies of adjuvant therapy, since we identified a subset of patients that benefit the most from such treatment. Our findings provide clinicians with CSM estimates that might be used to optimize patient selection for adjuvant therapy outside of clinical trials. Last but not least, our findings might affect study design in future clinical trials.
On the other hand, it should also be noted that patients with hR features after partial or radical nephrectomy and those who can benefit most from adjuvant therapy, do not necessarily overlap. Administration of adjuvant agents has not exclusively based on hR features. Conversely, other considerations such as comorbidities, protocol adherence, or other tumor characteristics (i.e., genomics) might also be considered. Additionally, adjuvant agents should be only ideally considered based on net OS benefit. The latter was not confirmed in S-TRAC, ASSURE, ARISER and PROTECT trial. In consequence, the European Association of Urology does not recommend adjuvant therapy for nmRCC after nephrectomy [12]. Furthermore, it is not known whether earlier treatment with adjuvant targeted therapy will even modify the clinical course of disease compared to treat only recurrent or metastatic disease [23]. In this context, future studies are required to void this lack.
Our study is not devoid of limitations. First, the SEER database is devoid of variables such as ECOG performance status, detailed histological information such as tumor necrosis or detailed pathological information, such as positive surgical margin status. Second, the observed number of patients with one, two or three hR features might underestimate the actual proportion of patients with hR in clinical practice due to exclusion from analysis of individuals with unknown hR features. Third, adjuvant and/or salvage treatment regimens also cannot be ascertained. Fourth, ideally hypothesis generated study such as the current ones should be followed by confirmatory phase 3 trials. The reverse order related to other findings might add to existing uncertainties about adjuvant therapy. These and other limitations are shared with other large-scale population-based studies.
Conclusions
Individuals with combination of LNI with FG3-4 or pT3a/b and patients with all three hR features are at highest risk of CSM. In consequence, these patients may represent ideal candidates for adjuvant therapy either in clinical practice or future prospective trials.
References
Wolff I, May M, Hoschke B et al (2016) Do we need new high-risk criteria for surgically treated renal cancer patients to improve the outcome of future clinical trials in the adjuvant setting? Results of a comprehensive analysis based on the multicenter CORONA database. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 42:744–750. doi:10.1016/j.ejso.2016.01.009
Frank I, Blute ML, Cheville JC et al (2002) An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol 168:2395–2400. doi:10.1097/01.ju.0000035885.91935.d5
Ravaud A, Motzer RJ, Pandha HS et al (2016) Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med 375:2246–2254. doi:10.1056/NEJMoa1611406
Noone A-M, Cronin KA, Altekruse SF et al (2017) Cancer Incidence and Survival Trends by Subtype Using Data from the Surveillance Epidemiology and End Results Program, 1992–2013. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 26:632–641. doi:10.1158/1055-9965.EPI-16-0520
Scoll BJ, Wong Y-N, Egleston BL et al (2009) Age, tumor size and relative survival of patients with localized renal cell carcinoma: a surveillance, epidemiology and end results analysis. J Urol 181:506–511. doi:10.1016/j.juro.2008.10.026
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474. doi:10.1245/s10434-010-0985-4
Dinse GE, Lagakos SW (1982) Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics 38:921–932
Gill R (1982) Understanding Cox’s regression model. Exp Suppl 41:187–199
Haas NB, Manola J, Uzzo RG et al (2016) Adjuvant sunitinib or sorafenib for high-risk, non-metastatic renal-cell carcinoma (ECOG-ACRIN E2805): a double-blind, placebo-controlled, randomised, phase 3 trial. Lancet Lond Engl 387:2008–2016. doi:10.1016/S0140-6736(16)00559-6
Chamie K, Donin NM, Klöpfer P et al (2017) Adjuvant weekly girentuximab following nephrectomy for high-risk renal cell carcinoma: the ARISER randomized clinical trial. JAMA Oncol 3:913–920. doi:10.1001/jamaoncol.2016.4419
Randomized Phase III trial of adjuvant pazopanib versus placebo after nephrectomy in patients with locally advanced renal cell carcinoma (RCC) (PROTECT): J Clin Oncol 35(15). http://ascopubs.org/doi/abs/10.1200/JCO.2017.35.15_suppl.4507. Accessed 20 July 2017
Bex A, Albiges L, Ljungberg B et al (2017) Updated European Association of Urology guidelines regarding adjuvant therapy for renal cell carcinoma. Eur Urol 71:719–722. doi:10.1016/j.eururo.2016.11.034
Kates M, Lavery HJ, Brajtbord J et al (2012) Decreasing rates of lymph node dissection during radical nephrectomy for renal cell carcinoma. Ann Surg Oncol 19:2693–2699. doi:10.1245/s10434-012-2330-6
Capitanio U, Becker F, Blute ML et al (2011) Lymph node dissection in renal cell carcinoma. Eur Urol 60:1212–1220. doi:10.1016/j.eururo.2011.09.003
Capitanio U, Jeldres C, Patard J-J et al (2009) Stage-specific effect of nodal metastases on survival in patients with non-metastatic renal cell carcinoma. BJU Int 103:33–37. doi:10.1111/j.1464-410X.2008.08014.x
Zisman A, Pantuck AJ, Wieder J et al (2002) Risk group assessment and clinical outcome algorithm to predict the natural history of patients with surgically resected renal cell carcinoma. J Clin Oncol Off J Am Soc Clin Oncol 20:4559–4566. doi:10.1200/JCO.2002.05.111
Patard J-J, Kim HL, Lam JS et al (2004) Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: an international multicenter study. J Clin Oncol Off J Am Soc Clin Oncol 22:3316–3322. doi:10.1200/JCO.2004.09.104
HCUP-US NIS Overview. https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 20 July 2017
National Cancer Database. In: American College of Surgeons. https://www.facs.org/quality%20programs/cancer/ncdb. Accessed 20 July 2017
Frank I, Blute ML, Cheville JC et al (2003) A multifactorial postoperative surveillance model for patients with surgically treated clear cell renal cell carcinoma. J Urol 170:2225–2232. doi:10.1097/01.ju.0000095541.10333.a7
Thompson RH, Leibovich BC, Lohse CM et al (2007) Dynamic outcome prediction in patients with clear cell renal cell carcinoma treated with radical nephrectomy: the D-SSIGN score. J Urol 177:477–480. doi:10.1016/j.juro.2006.09.057
Sun M, Shariat SF, Cheng C et al (2011) Prognostic factors and predictive models in renal cell carcinoma: a contemporary review. Eur Urol 60:644–661. doi:10.1016/j.eururo.2011.06.041
Rini BI, Dorff TB, Elson P et al (2016) Active surveillance in metastatic renal-cell carcinoma: a prospective, phase 2 trial. Lancet Oncol 17:1317–1324. doi:10.1016/S1470-2045(16)30196-6
Acknowledgements
The authors have none to declare.
Author information
Authors and Affiliations
Contributions
MB: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. AS, MM, UC: Manuscript writing/editing. EZ, FKC: Data analysis. RP: Data collection or management. AK, SFS: Data collection or management. FM, AB: Protocol/project development. PIK: Manuscript writing/editing, Protocol/project development.
Corresponding author
Ethics declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. None conflict of interest.
Research involving human participants and/or animals
None to declare.
Informed consent
None to declare.
Rights and permissions
About this article
Cite this article
Bandini, M., Smith, A., Zaffuto, E. et al. Effect of pathological high-risk features on cancer-specific mortality in non-metastatic clear cell renal cell carcinoma: a tool for optimizing patient selection for adjuvant therapy. World J Urol 36, 51–57 (2018). https://doi.org/10.1007/s00345-017-2093-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-017-2093-6