Abstract
Aims
To analyze the prevalence of depression, anxiety and their risk factors in German women with breast cancer (BC) in general and gynecological practices (GP, GYP).
Methods
Women initially diagnosed with BC between 2009 and 2013 were identified by 1202 general practitioners and 244 gynecologists in the IMS Disease Analyzer database. They were included only if they had not suffered from depression or an anxiety disorder within the 12 months prior to the index date. The main outcome was the first diagnosis of depression or an anxiety disorder within 5 years after index date. A multivariate Cox regression model was used to predict these diagnoses on the basis of patient characteristics.
Results
A total of 24,537 patients in GP were available for the study, as well as 20,018 patients in GYP. The mean age was 65.8 and 62.5 years in GP and GYP, respectively (p value <0.0001). The proportions of depressive or anxiety episodes in the past and the proportion of metastases were higher in GP than in GYP (7.9 vs. 3.6 %, and 10.1 vs. 8.6 %, p values <0.0001). Within 5 years of follow-up, 36.9 % of GP patients and 35.1 % of GYP patients had been diagnosed with depression or anxiety. There was a significantly higher risk of depression and/or anxiety in women in the age groups 51–60, 61–70 and >70 years than in women = <50 years (OR between 1.05 and 1.27, all p values lower than 0.0359). Patients with metastases or with previous episodes of depression/anxiety had a higher risk of depression/anxiety (OR = 1.21 and 1.97, p values <0.0001). Finally, women with private health insurance had a lower risk of depression and anxiety (OR = 0.45, p value <0.0001).
Conclusion
The present study indicates that levels of depression and anxiety increase in German women after diagnosis of BC and may be predicted on the basis of several demographic and clinical characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common cancer in women worldwide, with approximately 1.2 million new cases diagnosed in 2012 (World Cancer Research Fund International 2015). This number represents 25 and 12 % of all new cases of cancer in women and in the general population, respectively. Belgium, Denmark and France have the highest rates of BC in the world (111.9, 105.0 and 104.5 new diagnoses per 100,000 people), underlining the significant impact of this disease on health and on the economy in Europe. Although the incidence of the disease is slightly lower in Germany (91.6 new cases per 100,000 people), the burden of BC in the country is still considerable, with total related costs estimated at around 1956 million euros in 2008 (Jönsson and Wilking 2013).
Improvements in BC diagnosis and treatment have led to a decrease in patient mortality rates in recent decades (Bray et al. 2004; Giordano et al. 2004). Therefore, BC is now considered a chronic condition which requires particular management by physicians and other health professionals in order to maximize the quality of life of women suffering from the disease (Fann et al. 2008). This management is of particular importance, since patients frequently develop psychiatric disorders such as depression and abnormal anxiety after cancer diagnosis (Spiegel 1996; Hegel et al. 2006). Indeed, in 1983, Derogatis and colleagues (Derogatis et al. 1983) studied 215 patients with cancer and showed that 47 % of them had at least one psychiatric disorder. More recently, a 2005 study conducted in the UK demonstrated that almost 50 % of women with BC had suffered from depression and/or anxiety in the first year following diagnosis, 25 % in the second, third and fourth years, and 15 % in the fifth year (Burgess et al. 2005). The same study also showed that risk factors for longer-term depression and anxiety included previous psychological treatments, lack of an intimate relationship, younger age and stressful life experiences (Burgess et al. 2005). These results suggested that risk factors for depression and anxiety in women with BC are more closely related to the individual patient than to the disease itself or its treatment.
Although these findings emerged in several independent studies in different countries, they have only been confirmed once in Germany and most of them were obtained before 2008 or thereabouts (Burgess et al. 2005; Dean 1987; Fallowfield et al. 1990; Hopwood et al. 1991; Schwarz et al. 2008; So et al. 2010; Vahdaninia et al. 2010). Therefore, the goal of this work was to analyze the prevalence of depression, anxiety and their risk factors in women with BC in more recent cases treated in German general and gynecological practices.
Methods
Database
The Disease Analyzer database (IMS HEALTH) compiles drug prescriptions, diagnoses, basic medical and demographic data obtained directly and in anonymous format from computer systems used in the practices of general and gynecological practitioners (Becher et al. 2009). Diagnoses (ICD-10), prescriptions (Anatomical Therapeutic Chemical (ATC) classification system) and the quality of reported data are monitored by IMS based on a number of criteria (e.g., completeness of documentation, linkage between diagnoses and prescriptions).
In Germany, the sampling methods used for the selection of physicians’ practices were appropriate to obtain a representative database of primary care and gynecological practices (Becher et al. 2009). Prescription statistics for several drugs were very similar to data available from pharmaceutical prescription reports (Becher et al. 2009). The age groups for given diagnoses in Disease Analyzer also agreed well with those in corresponding disease registries (Becher et al. 2009).
Study population
Women initially diagnosed with breast cancer (ICD 10: C50) between January 2009 and December 2013 (index date) were identified by 1202 general practitioners and 244 gynecologists in the IMS Disease Analyzer database. They were included only if they had not suffered from depression or an anxiety disorder within 12 months prior to index date. A total of 24,537 patients in general practices (GP) and 20,018 in gynecological practices (GYP) were available for analysis.
Study outcome
The main outcome measure was the first diagnosis of either depression (ICD 10: F32, F33) or anxiety (ICD 10: F41) disorder within 5 years after index date.
Independent variables
Demographic data included age and health insurance type (private or statutory). Patient histories of depressive or anxiety episodes in the past and the presence of potential metastases were also taken into account.
Statistical analyses
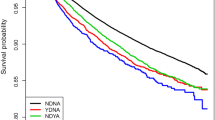
Descriptive analyses were obtained for demographic variables, depressive or anxiety episodes in the past, and metastases. Mean ± SD were calculated for age, while proportions were calculated for other variables. Time to depression diagnosis in newly diagnosed BC patients in GP and GYP was analyzed using Kaplan–Meier curves. A multivariate Cox regression model was used to predict depression or anxiety diagnosis on the basis of patient characteristics (age, health insurance, depressive or anxiety episodes in the past and metastases). P values <0.05 were considered statistically significant. Analyses were carried out using SAS version 9.3.
Results
Patient characteristics
Patient characteristics are shown in Table 1. A total of 24,537 and 20,018 women with BC were included in GP and GYP, respectively. The mean age was 65.8 years (SD = 13.0) in GP and 62.5 years (SD = 13.5) in GYP (p value <0.0001); 8.5 % of GP patients and 9.6 % of GYP patients had private health insurance (p value <0.0001). The proportion of depressive or anxiety episodes in the past was higher in GP than in GYP patients (7.9 vs. 3.6 %, p value <0.0001). Metastases were significantly more frequently documented in GP than in GYP (10.1–4.9 % bone and 7.1 % visceral metastases vs. 8.6–2.8 % and 7.4 %, p value <0.0001).
Depression and/or anxiety diagnosis
Kaplan–Meier curves for time to depression and/or anxiety diagnosis in newly diagnosed BC patients in GP and GYP are displayed in Fig. 1. After 1 year of follow-up, 17.4 % of BC patients in GP and 19.2 % in GYP had been diagnosed with depression and/or anxiety. Within 5 years of follow-up, 36.9 % of patients in GP and 35.1 % of patients in GYP had been diagnosed with depression and/or anxiety. Table 2 shows the results of the multivariate Cox regression model. There was a significantly higher risk of depression and/or anxiety in women in the age groups 51–60 (OR = 1.19, 95 % CI 1.13–1.26, p value <0.0001), 61–70 (OR = 1.27, 95 % CI 1.21–1.34, p value <0.0001) and >70 years (OR = 1.05, 95 % CI 1.00–1.11, p value = 0.0359) compared to women <=50 years. There was a higher risk of depression/anxiety in patients with metastatic breast cancer (OR = 1.21, 95 % CI 1.14–1.28, p value <0.0001) and patients who had suffered from depressive and/or anxiety episodes in the past (more than 1 year prior to breast cancer diagnosis) (OR = 1.97, 95 % CI 1.85–2.09, p value <0.0001). Private health insurance was associated with a significantly lower risk of depression/anxiety (OR = 0.45, 95 % CI 0.41–0.49, p value <0.0001).
Discussion
This study confirmed the findings of other works, which had shown that depression and anxiety occur frequently in women with BC. However, to date, the association between BC and these psychiatric disorders has only been investigated once in Germany by Schwarz et al. (2008), who analyzed the impact of treatments in hospital on depression in patients with different stages of BC. Our work demonstrated that the number of patients with depression and/or anxiety increased after BC diagnosis. Furthermore, we showed that age over 50 years, statutory health insurance, patient history of depressive/anxiety episodes and the presence of metastases were linked to a significant extent with a higher risk of depression and/or anxiety.
BC is one of the most common cancers in the world, particularly in Europe, where its incidence and the related mortality rates remain significant (World Cancer Research Fund International 2015). Nonetheless, the diagnosis, management and treatment of women with BC have resulted in an increase in the number of survivors. Therefore, one of the major goals of physicians, nurses and other health key players is to improve the life of BC patients who are facing important changes after diagnosis and are at a high risk of developing psychiatric disorders, such as depression and anxiety (Brennan 2001; Reich et al. 2008). Indeed, women with cancer frequently have concerns regarding death, daily life, body image or sexuality, and these concerns may have a strong impact on their mental health, even several years after diagnosis (Spiegel 1997; Baucom et al. 2005).
A number of authors have studied the prevalence of mood disorders in women with early and late BC (Derogatis et al. 1983; Fulton 1997; Burgess et al. 2005; Grabsch et al. 2006; Reich et al. 2008). Recently, Burgess and his colleagues demonstrated that 50 % of patients display the symptoms of depression during the first year following BC diagnosis (Burgess et al. 2005). Furthermore, another study, which was conducted in Australia and included 227 women from Melbourne in the late stages of BC, showed that 35.7 % of them had either depression or anxiety (Grabsch et al. 2006). Interestingly, when all stages of BC are considered, one out of four patients is found to suffer from depression. This number tends to increase with the duration of the disease, reaching 50 % in women in the late stages of the disease (Fulton 1997). Therefore, our data are in line with the literature, as we observed an increase in the number of depressed and anxious patients during the 5 years following cancer diagnosis. This increase may be related to the initial diagnosis itself, but also to the diagnosis of metastases, the dependency associated with treatments and their numerous side effects (i.e., fatigue, pain and nausea).
The association between BC and depression and/or anxiety may be even more significant, since major psychological and psychiatric outcomes are usually underestimated, underrated and undertreated in patients with cancer (Somerset et al. 2004). First, one has to remember that the diagnosis of depression and anxiety is not always obvious and is based on different nosological systems, for example DSM-V and ICD-10. Moreover, given the rapid evolution of psychological disorders in cancer patients, the time of evaluation is an important factor (Reich et al. 2008). Apart from these considerations, there are two main hypotheses that may explain the underestimation of depression and anxiety frequently observed in women with BC (Somerset et al. 2004). The first is that women usually do not report these diseases to the physician and do not want to admit that they are anxious or depressed (Maguire et al. 1978). It is also possible that health professionals, and in particular GPs and gynecologists, do not document potential episodes of depression or anxiety (Greenberg 2004).
In order to reduce the prevalence of depression and anxiety in patients with BC, it is important to understand the nature of the relationship between these psychological conditions and cancer. Although the link has been studied by several authors in the past, its exact nature is not perfectly understood (Reich et al. 2008). In 1999, McKenna et al. (1999) analyzed 46 studies and demonstrated that specific psychological factors led to a modest increase in the occurrence of BC. More recently, Duijts and colleagues (Duijts et al. 2003) examined the relationship between BC and stressful life events in several studies conducted between 1966 and 2002 and showed that the death of a spouse and the death of a relative or friend slightly increased the risk of developing BC. The main hypothesis that could explain the effects of psychological disorders and stressful life episodes on BC occurrence is a disruption to the immune system, potentially leading to the proliferation of oncogenic cells (Ollonen et al. 2005; Reich et al. 2008). To add further complexity, several demographic and clinical characteristics of women with BC are also known to be predictors of depression and/or anxiety. Indeed, in 2005, a Japanese study showed that the risk of developing psychiatric diseases, including major depressive and generalized anxiety disorders, was 16 times higher in BC patients with a history of depression than in women without previous episodes of depression (Okamura et al. 2005). Furthermore, other authors have demonstrated that the lack of an intimate relationship, neuroticism and low incomes correlates with depression in women with BC (Golden-Kreutz and Andersen 2004; Ell et al. 2005; Den et al. 2009). All these results suggest that depression and anxiety are predicted mainly on the basis of the demographic and clinical characteristics of BC patients. Since we found in our study that the prevalence of depression was higher in patients with a history of psychiatric disorders and in women with statutory health insurance, which is an indicator of low income, our work corroborates these findings.
By contrast, we discovered that older patients had a higher risk of developing depression or anxiety than patients under 50. This result may be intriguing, as younger age is known to be a predictor of long-term depression and anxiety in women with BC (Burgess et al. 2005). Nonetheless, quality of life steadily decreases with age in general population, leading to an increase in the occurrence of depression (Blazer et al. 1991). To add more complexity, a recent study conducted by Vahdaninia et al. (2010) found no association between age and depression in BC patients. Nonetheless, one has to keep in mind that it only included 167 patients from Tehran, whereas we analyzed more than 40,000 German women with BC.
Interestingly, we also found that the presence of metastases was a predictor for depression and anxiety. This last result may be explained by the fact that metastases decrease the quality of life of women with BC, as they increase pain, are associated with more severe treatments and shorten life, causing fear of death (Spiegel and Bloom 1983). Our work also showed that, in Germany, depressive and anxiety episodes are better documented by gynecologists than by GPs, underlining the fact that gynecologists are more commonly responsible for the support of German women with BC.
This study was subject to several limitations. First of all, diagnoses were only established by primary care physicians and gynecologists. Secondly, the database contained no information on TNM classification. Finally, data on socioeconomic status and quality of life are not available (i.e., marital status, alcohol/drug abuse and stressful experiences), although socioeconomic factors may also be predictors of depression and anxiety.
Overall, the present study indicates that the levels of depression and anxiety increase after diagnosis of BC in German women. This increase is predicted by several factors, such as age, health insurance, a history of anxiety and depressive episodes, and the presence of metastases. Therefore, there is a need to improve psychological management and intervention for women with BC. Such therapies must be established as soon as possible in both general and gynecological practices, in order to improve the quality of life of patients and indirectly prevent depression. In return, women may display better adherence and persistence to their anti-oncogenic treatment, which may maximize clinical responses.
References
Baucom DH, Porter LS, Kirby JS, Gremore TM, Keefe FJ (2005) Psychosocial issues confronting young women with breast cancer. Breast Dis 23:103–113
Becher H, Kostev K, Schröder-Bernhardi D (2009) Validity and representativeness of the “disease analyzer” patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther 47:617–626
Blazer D, Burchett B, Service C, George LK (1991) The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol 46:M210–M215. doi:10.1093/geronj/46.6.M210
Bray F, McCarron P, Parkin DM (2004) The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res BCR 6:229–239. doi:10.1186/bcr932
Brennan J (2001) Adjustment to cancer—coping or personal transition? Psychooncology 10:1–18
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702. doi:10.1136/bmj.38343.670868.D3
Dean C (1987) Psychiatric morbidity following mastectomy: preoperative predictors and types of illness. J Psychosom Res 31:385–392
Den Oudsten BL, Van Heck GL, Van der Steeg AFW, Roukema JA, De Vries J (2009) Predictors of depressive symptoms 12 months after surgical treatment of early-stage breast cancer. Psycho-oncology 18:1230–1237. doi:10.1002/pon.1518
Derogatis LR, Morrow GR, Fetting J, Penman D, Piasetsky S, Schmale AM, Henrichs M, Carnicke CL (1983) The prevalence of psychiatric disorders among cancer patients. JAMA 249:751–757
Duijts SF, Zeegers MP, Borne BV (2003) The association between stressful life events and breast cancer risk: a meta-analysis. Int J Cancer 107:1023–1029. doi:10.1002/ijc.11504
Ell K, Sanchez K, Vourlekis B, Lee P-J, Dwight-Johnson M, Lagomasino I, Muderspach L, Russell C (2005) Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. J Clin Oncol 23:3052–3060. doi:10.1200/JCO.2005.08.041
Fallowfield LJ, Hall A, Maguire GP, Baum M (1990) Psychological outcomes of different treatment policies in women with early breast cancer outside a clinical trial. BMJ 301:575–580
Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J (2008) Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 30:112–126. doi:10.1016/j.genhosppsych.2007.10.008
Fulton CL (1997) The physical and psychological symptoms experienced by patients with metastatic breast cancer before death. Eur J Cancer Care 6:262–266
Giordano SH, Buzdar AU, Smith TL, Kau S-W, Yang Y, Hortobagyi GN (2004) Is breast cancer survival improving? Cancer 100:44–52. doi:10.1002/cncr.11859
Golden-Kreutz DM, Andersen BL (2004) Depressive symptoms after breast cancer surgery: relationships with global, cancer-related, and life event stress. Psycho-oncol 13:211–220. doi:10.1002/pon.736
Grabsch B, Clarke DM, Love A, McKenzie DP, Snyder RD, Bloch S, Smith G, Kissane DW (2006) Psychological morbidity and quality of life in women with advanced breast cancer: a cross-sectional survey. Palliat Support Care 4:47–56
Greenberg DB (2004) Barriers to the treatment of depression in cancer patients. J Natl Cancer Inst Monogr. doi:10.1093/jncimonographs/lgh019
Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL, Clay KF, Ahles TA (2006) Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107:2924–2931. doi:10.1002/cncr.22335
Hopwood P, Howell A, Maguire P (1991) Psychiatric morbidity in patients with advanced cancer of the breast: prevalence measured by two self-rating questionnaires. Br J Cancer 64:349–352
Jönsson B, Wilking N (2013) Prevention and the economic burden of breast cancer. GE Healthcare. http://gehc.s3.amazonaws.com/Newsroom%20stories/BreastCancer%202013/Final%20Breast%20Cancer%20White%20Paper.pdf
Maguire GP, Lee EG, Bevington DJ, Küchemann CS, Crabtree RJ, Cornell CE (1978) Psychiatric problems in the first year after mastectomy. Br Med J 1:963–965
McKenna MC, Zevon MA, Corn B, Rounds J (1999) Psychosocial factors and the development of breast cancer: a meta-analysis. Health Psychol 18:520–531
Okamura M, Yamawaki S, Akechi T, Taniguchi K, Uchitomi Y (2005) Psychiatric disorders following first breast cancer recurrence: prevalence, associated factors and relationship to quality of life. Jpn J Clin Oncol 35:302–309. doi:10.1093/jjco/hyi097
Ollonen P, Lehtonen J, Eskelinen M (2005) Stressful and adverse life experiences in patients with breast symptoms; a prospective case-control study in Kuopio Finland. Anticancer Res 25:531–536
Reich M, Lesur A, Perdrizet-Chevallier C (2008) Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat 110:9–17. doi:10.1007/s10549-007-9706-5
Schwarz R, Krauss O, Höckel M, Meyer A, Zenger M, Hinz A (2008) The course of anxiety and depression in patients with breast cancer and gynaecological cancer. Breast Care 3:417–422. doi:10.1159/000177654
So WKW, Marsh G, Ling WM, Leung FY, Lo JCK, Yeung M, Li GKH (2010) Anxiety, depression and quality of life among Chinese breast cancer patients during adjuvant therapy. Eur J Oncol Nurs 14:17–22. doi:10.1016/j.ejon.2009.07.005
Somerset W, Stout SC, Miller AH, Musselman D (2004) Breast cancer and depression. Oncol (Williston Park NY) 18:1021–1034 (discussion 1035–1036, 1047–1048)
Spiegel D (1996) Cancer and depression. Psychiatry, Suppl
Spiegel D (1997) Psychosocial aspects of breast cancer treatment. Semin Oncol 24:S1–36–S1–47
Spiegel D, Bloom JR (1983) Pain in metastatic breast cancer. Cancer 52:341–345
Vahdaninia M, Omidvari S, Montazeri A (2010) What do predict anxiety and depression in breast cancer patients? A follow-up study. Soc Psychiatry Psychiatr Epidemiol 45:355–361. doi:10.1007/s00127-009-0068-7
World Cancer Research Fund International (2015) Breast cancer statistics. http://www.wcrf.org. Accessed on 07/19/15
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Jacob, Bleicher, Hadji, Kalder and Kostev declare that they have no conflict of interest.
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Jacob, L., Bleicher, L., Kostev, K. et al. Prevalence of depression, anxiety and their risk factors in German women with breast cancer in general and gynecological practices. J Cancer Res Clin Oncol 142, 447–452 (2016). https://doi.org/10.1007/s00432-015-2048-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-2048-5