Abstract
Background
Breast cancer (BC) and genital organ cancers (GOC) are known to have a major impact on the quality of life of patients. The aim of this study was to analyze the risk of depression, anxiety, and adjustment disorders in women in Germany with a suspected but unconfirmed diagnosis of BC or GOC in their medical history.
Methods
This study included women who received a suspected diagnosis of BC or GOC and were followed between 2007 and 2015 (index date). These women were matched (1:1:1) by age to women with a confirmed diagnosis of BC or GOC and women without a cancer diagnosis. The main outcome measure of the study was the rate of depression, anxiety, and adjustment disorder diagnoses within 3 years of the index date.
Results
The present analysis included a total of 4,842 patients (mean age = 49.3 years). Within 3 years of the index date, 23.5% of women with a confirmed diagnosis of BC or GOC, 14.1% of those with a suspected diagnosis of BC or GOC, and 10.5% of those without a cancer diagnosis developed depression, anxiety, or an adjustment disorder (log-rank p value <0.001). Women with a suspected diagnosis of cancer were at a higher risk for these psychiatric conditions than those without a cancer diagnosis (BC and GOC: HR 1.32; BC: HR 1.21; GOC: HR 1.50).
Conclusion
A suspected diagnosis of BC or GOC in a woman’s medical history is associated with an increased risk of developing depression, anxiety, and adjustment disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) and genital organ cancers (GOC) are very common cancers in women around the world. In 2012, around 1.7 million patients were diagnosed with BC, which represented 25% of all new cases of cancer in women [1]. With an age-standardized rate of 91.6 new diagnoses per 100,000 individuals for BC and 10.2 for ovarian cancer, Germany has among the highest incidences of BC and GOC in the world [1, 2]. Therefore, these cancers are associated with an important health and economic burden in this country [3,4,5].
BC and GOC are known to have a major impact on patients’ quality of life [6, 7]. In a 2016 German study, researchers discovered that the incidence of depression and anxiety was 8.8 per 100 person-years in women with BC and 5.9 in those with GOC [7]. Another work including more than 24,500 individuals with BC showed that more than one patient of three developed depression within 5 years of a cancer diagnosis [6]. Interestingly, few authors have studied the risk of developing psychiatric disorders in patients with a suspected diagnosis of BC or GOC. In 2001, Lampic et al. showed that approximately 46% of women recalled after a suspicious screening mammogram were anxious, and 11% were depressed, with a wait time of approximately 1 week [8]. Later, in 2008, Liao and colleagues estimated that women with suspected BC displayed moderate to high uncertainty and anxiety levels during the diagnostic period, which was estimated to be almost 9 days [9]. More recently, a 2010 study discovered that 56% of individuals with a possible ovarian cancer diagnosis were potentially anxious prior to clinical investigations [10]. Finally, in 2015, a significant interaction between wait time for BC surgery and chronic life stress was found, with women displaying such stress being at a higher risk for anxiety [11].
Although these previous works are of great importance, most of them included only small numbers of patients and were not conducted in Europe. Furthermore, none of these studies focused on the development of psychiatric disorders in the years following the suspected diagnosis of BC or GOC. Therefore, the purpose of the present study was to analyze the risk of developing depression, anxiety, and adjustment disorders in women in Germany with a suspected but unconfirmed diagnosis of BC or GOC in their medical history.
Methods
Database
This study is based on data from the Disease Analyzer database (QuintilesIMS), which compiles drug prescriptions, diagnoses, and basic medical and demographic data obtained directly and in anonymous format from computer systems used in physicians’ practices [12]. Diagnoses (ICD-10), prescriptions (Anatomical Therapeutic Chemical [ATC] Classification System), and the quality of reported data have been monitored by QuintilesIMS based on a number of criteria (e.g., completeness of documentation and linkage between diagnoses and prescriptions).
In Germany, the sampling methods used for the selection of physicians’ practices were appropriate for obtaining a representative database of physicians [12]. Finally, the database has already been used in several studies focusing on BC and GOC [6, 7].
Study population
This study included women who received a suspected diagnosis of BC or GOC (ICD-10: C50–C59) and were followed in 262 German gynecological practices between January 2007 and December 2015 (index date). Follow-up ended in December 2016. Inclusion criteria were as follows: (i) absence of a confirmed diagnosis of breast or genital cancer within 3 years of the index date; (ii) absence of any other cancer diagnosis (C00-C49, C60-C99) prior to the index date; (iii) follow-up of at least 365 days prior to the index date; and (iv) absence of a diagnosis of depression, anxiety, or adjustment disorder prior to the index date. After applying these inclusion criteria, except for the first one, these women were matched (1:1:1) by age to women with a confirmed diagnosis of BC or GOC (C50-C59) and women without cancer. No other variables were used for matching the patients included in the three different groups.
Study outcome
The main outcome measure of the study was the rate of depression (F32, F33), anxiety (F41), and adjustment disorder (F43) diagnoses within 3 years of the index date.
Statistical analysis
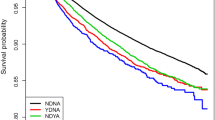
Kaplan–Meier analyses were performed to study the development of depression, anxiety, and adjustment disorders in women with suspected BC or GOC, those with a confirmed diagnosis of BC or GOC, and those without cancer within 3 years of the index date. Cox proportional hazards regression models were used to estimate the relationship between a suspected cancer diagnosis, confirmed cancer diagnosis, and the subsequent diagnosis of these three psychiatric conditions. A p value <0.05 was considered statistically significant. All analyses were carried out using SAS 9.3 (SAS Institute, Cary, USA) (Fig. 1).
Results
Patient characteristics are shown in Table 1. The present analysis included a total of 4,842 patients. The mean age was 49.3 years (SD 16.5 years), and 55.6% of the population were 50 years or younger. Figure 2 displays Kaplan–Meier curves for the time to diagnosis of depression, anxiety, or an adjustment disorder in the three different groups. Within 3 years of the index date, 23.5% of women with a confirmed diagnosis of BC or GOC, 14.1% of those with a suspected diagnosis of BC or GOC, and 10.5% of those without a cancer diagnosis developed at least one of these psychiatric conditions (log-rank p value <0.001). The results of the Cox regression models are shown in Table 2. Women with a suspected diagnosis of cancer were at a higher risk of depression, anxiety, and adjustment disorders than those without a cancer diagnosis [BC and GOC: hazard ratio (HR) 1.32, 95% confidence interval (CI) 1.09–1.59; BC: HR = 1.21, 95% CI 1.01–1.42; GOC: HR 1.50, 95% CI 1.18–1.91]. Such risk was also significantly increased in the group with a confirmed diagnosis of cancer when compared to the group without a cancer diagnosis (HRs ranging from 2.01 to 2.58).
Discussion
The present retrospective study including approximately 4,800 women found that almost 15% of women with a suspected diagnosis of BC or GOC developed depression, anxiety, or an adjustment disorder within 3 years of the diagnosis. It was further discovered that a suspected diagnosis of BC or GOC was associated with a significant increase in the risk of being subsequently diagnosed with one of these psychiatric diseases. Finally, women with a confirmed diagnosis of cancer exhibited a higher risk of developing these conditions than those without a diagnosis of cancer.
Although the association between a confirmed diagnosis of BC or GOC and mental health has been analyzed in depth by several authors in the past [6, 7, 13,14,15,16,17,18], little is known about the impact of a suspected diagnosis of one of these female cancers on the development of psychiatric disorders. In 2001, Lampic and colleagues examined the psychological effects of clinical investigations after BC screening in almost 800 women from Sweden [8]. They showed that approximately one out of two women reported anxiety and one out of ten reported depression prior to the recall visit. Anxiety and depression were further found to decrease a few days after the visit in women with normal or benign results. In individuals who were referred to a surgeon for a subsequent biopsy, psychological distress remained high for as long as 12 months.
In 2008, Liao et al. estimated in 127 women who had a suspected BC diagnosis and were followed in a teaching hospital in northern Taiwan that uncertainty and anxiety were higher before than after diagnosis [9]. The same work showed that these levels were more pronounced in participants ultimately diagnosed with malignant tumors than in those diagnosed with benign tumors. Finally, a positive correlation was found between uncertainty and anxiety. More recently, in 2010, Gonçalves et al. showed that around 33% of a population of 30 women undergoing clinical investigations for possible ovarian cancer were anxious and 7% were depressed prior to the confirmation of the cancer diagnosis [10]. In line with previous studies, the rates of these two psychiatric disorders decreased to approximately 18 and 5%, respectively, a few months after the final cancer diagnosis was made. In contrast, no significant difference was found in this work in the levels of anxiety and depression between women with a subsequent cancer diagnosis and those with a benign result. This lack of a difference in anxiety and depression patterns may potentially be explained by the small number of patients included, as well as by the fact that diagnoses were made using questionnaires, potentially leading to a decrease in the study’s statistical power. Even if such results are of great importance, this analysis only considered the impact of wait time and not the impact of a suspected cancer diagnosis in the medical history on the risk of being subsequently affected by psychiatric conditions. Except for the study by Gonçalves and colleagues [10], no recent work has focused on the potential impact of a suspected diagnosis of GOC on the subsequent risk of developing psychiatric diseases.
Uncertainty about biopsy results is known to be associated with an increase in biochemical stress levels [11, 19]. In 2009, Lang et al. discovered in 150 women undergoing large-core breast biopsies that the mean cortisol slope was significantly flatter in the group with an uncertain diagnosis when compared to the group with a benign diagnosis [19]. In contrast, this slope was similar between women with a suspected cancer diagnosis and those with a confirmed cancer diagnosis. Although no such work has been performed in women affected by other female organ cancers, uncertainty about cervical biopsies may also be associated with an important increase in biological stress levels. In 2015, Hayes Balmadrid et al. aimed to analyze the relationship between psychosocial factors and the length of time from breast biopsy recommendation to biopsy procedure [11]. In this American study, which included 140 women and was based on questionnaires, the authors found that the anxiety levels were clinically important regardless of wait time.
In line with these various works, the present German study showed that women with a suspected diagnosis of BC or GOC in their medical history exhibited an increased risk of being diagnosed with anxiety, depression, or adjustment disorders. Furthermore, it is worth noting that this risk was slightly higher than half the risk of women with a confirmed diagnosis of BC or GOC. Taken together with the findings of Hayes Balmadrid et al. [11], such data indicate that a suspected diagnosis of cancer, and not just the wait time between the initial and the confirmation diagnosis, is itself a risk factor for the subsequent development of psychiatric conditions. Therefore, a suspected diagnosis of BC or GOC is associated with both short- and long-term risks of being affected by anxiety, depression, and adjustment disorders.
This study was subject to three major limitations. Firstly, diagnoses relied solely on ICD-10 codes. Secondly, data on socioeconomic status and quality of life were not available (i.e., marital status, alcohol/drug abuse, and stressful experiences), although socioeconomic factors may also be predictors of depression and anxiety. Finally, the study cohorts were matched by age only, as no other relevant variables were available. For example, no information on family history of cancer was available, although a family history of BC may lead to a greater degree of distress and may be associated with a higher risk of receiving an unconfirmed cancer diagnosis.
Overall, a suspected diagnosis of BC or GOC in the medical history of a woman is associated with an increased risk of developing depression, anxiety, or an adjustment disorder. Therefore, women with a suspected diagnosis of cancer should be intensively screened for anxiety and other psychiatric conditions in the months following their initial diagnosis.
References
World Cancer Research Fund International (2015) Breast cancer statistics. http://www.wcrf.org, http://www.wcrf.org/int/cancer-facts-figures/data-specific-cancers/breast-cancer-statistics
International Agency for Research on Cancer (2017) Ovarian cancer—estimated incidence, mortality & prevalence, 2012. http://eco.iarc.fr/eucan/CancerOne.aspx?Cancer=27&Gender=2
Hampl M, Huppertz E, Schulz-Holstege O, Kok P, Schmitter S (2011) Economic burden of vulvar and vaginal intraepithelial neoplasia: retrospective cost study at a German dysplasia centre. BMC Infect Dis 11:73
Jönsson B, Wilking N (2013) Prevention and the economic burden of breast cancer. GE Healthcare. http://gehc.s3.amazonaws.com/Newsroom%20stories/BreastCancer%202013/Final%20Breast%20Cancer%20White%20Paper.pdf. Accessed 19 Jul 2015
Schrauder MG, Brunel-Geuder L, Häberle L, Wunderle M, Hoyer J, Reis A et al (2017) Cost-effectiveness of risk-reducing surgeries in preventing hereditary breast and ovarian cancer. Breast Edinb Scotl 32:186–191
Jacob L, Bleicher L, Kostev K, Kalder M (2015) Prevalence of depression, anxiety and their risk factors in German women with breast cancer in general and gynecological practices. J Cancer Res Clin Oncol 142:447
Jacob L, Kalder M, Kostev K (2016) Incidence of depression and anxiety among women newly diagnosed with breast or genital organ cancer in Germany. Psychooncology
Lampic C, Thurfjell E, Bergh J, Sjödén PO (2001) Short- and long-term anxiety and depression in women recalled after breast cancer screening. Eur J Cancer Oxf Engl 37(4):463–469
Liao M-N, Chen M-F, Chen S-C, Chen P-L (2008) Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nurs 31(4):274–283
Gonçalves V, Jayson G, Tarrier N (2010) A longitudinal investigation of psychological disorders in patients prior and subsequent to a diagnosis of ovarian cancer. J Clin Psychol Med Settings 17(2):167–173
Hayes Balmadrid MA, Shelby RA, Wren AA, Miller LS, Yoon SC, Baker JA et al (2015) Anxiety prior to breast biopsy: relationships with length of time from breast biopsy recommendation to biopsy procedure and psychosocial factors. J Health Psychol 30:1359105315607828
Becher H, Kostev K, Schröder-Bernhardi D (2009) Validity and representativeness of the “Disease Analyzer” patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther 47(10):617–626
Chochinov HM (2001) Depression in cancer patients. Lancet Oncol 2(8):499–505
Ollonen P, Lehtonen J, Eskelinen M (2005) Stressful and adverse life experiences in patients with breast symptoms; a prospective case-control study in Kuopio, Finland. Anticancer Res 25(1B):531–536
Ollonen P, Lehtonen J, Eskelinen M (2005) Anxiety, depression, and the history of psychiatric symptoms in patients with breast disease: a prospective case-control study in Kuopio, Finland. Anticancer Res 25(3c):2527–2533
Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL et al (2006) Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107(12):2924–2931
Eskelinen M, Ollonen P (2009) Psychosocial risk scale (PRS) for breast cancer in patients with breast disease: a prospective case-control study in Kuopio, Finland. Anticancer Res 29(11):4765–4770
Watts S, Prescott P, Mason J, McLeod N, Lewith G (2015) Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 5(11):e007618
Lang EV, Berbaum KS, Lutgendorf SK (2009) Large-core breast biopsy: abnormal salivary cortisol profiles associated with uncertainty of diagnosis. Radiology 250(3):631–637
Funding
The authors have received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KK, LJ, and MK have declared that they have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Kostev, K., Jacob, L. & Kalder, M. Risk of depression, anxiety, and adjustment disorders in women with a suspected but unconfirmed diagnosis of breast or genital organ cancer in Germany. Cancer Causes Control 28, 1021–1026 (2017). https://doi.org/10.1007/s10552-017-0948-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-017-0948-1