Abstract
Aconitine is a sodium channel opener, but its effects on the respiratory center are not well understood. We investigated the dose-dependent effects of aconitine on central respiratory activity in brainstem-spinal cord preparations isolated from newborn rats. Bath application of 0.5–5 μM aconitine caused an increase in respiratory rhythm and decrease in the inspiratory burst amplitude of the fourth cervical ventral root (C4). Separate application of aconitine revealed that medullary neurons were responsible for the respiratory rhythm increase, and neurons in both the medulla and spinal cord were involved in the decrease of C4 amplitude by aconitine. A local anesthetic, lidocaine (100 μM), or a voltage-dependent sodium channel blocker, tetrodotoxin (0.1 μM), partially antagonized the C4 amplitude decrease by aconitine. Tetrodotoxin treatment tentatively decreased the respiratory rhythm, but lidocaine tended to further increase the rhythm. Treatment with 100 μM riluzole or 100 μM flufenamic acid, which are known to inhibit respiratory pacemaker activity, did not reduce the respiratory rhythm enhanced by aconitine + lidocaine. The application of 1 μM aconitine depolarized the preinspiratory, expiratory, and inspiratory motor neurons. The facilitated burst rhythm of inspiratory neurons after aconitine disappeared in a low Ca2+/high Mg2+ synaptic blockade solution. We showed the dose-dependent effects of aconitine on respiratory activity. The antagonists reversed the depressive effects of aconitine in different manners, possibly due to their actions on different sites of sodium channels. The burst-generating pacemaker properties of neurons may not be involved in the generation of the facilitated rhythm after aconitine treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aconitine is a lipid-soluble cardiotoxin and neurotoxin found in Aconitum species [7, 28]. It targets the type 2 receptor site of sodium channels and, at the cellular level, induces a depolarizing shift of the resting membrane potential and causes repetitive firing of action potentials in excitable membranes [5, 28]. In clinical settings, aconitine is known to cause systemic paralysis and nausea and vomiting, followed by dizziness, palpitation, hypotension, arrhythmia, shock, dyspnea, and coma [1, 29]. However, aconitine is exclusively used as an ingredient in traditional medicine [28]. The intravenous administration of aconitine to rats leads to irregular respiratory activity, exophthalmia, Straub reaction, convulsions, disturbed locomotion activity, mydriasis, and loss of body weight. Higher doses can result in gasping for breath, convulsions of higher intensity and frequency, lacrimation, salivation, reduced locomotion, loss of orientation, ventral or ventro-lateral recumbency, and loss of different reflexes [9]. At the tissue level, aconitine is known to trigger ventricular arrhythmias in the heart and promote spontaneous transmitter release in ventral medial hypothalamic neurons [10, 29]. However, its effects on the respiratory center in the medulla are not well understood.
The voltage-dependent fast sodium channels and persistent sodium channels are involved in respiratory burst generation [13, 15, 17, 21, 27]. Moreover, sodium leak channels can affect the excitability of neurons in the respiratory center by influencing the resting membrane potential [24, 30]. Thus, we considered that analysis of the effects of aconitine on respiratory neuronal activity would be of help to understand the roles of sodium channels in respiratory modulation.
Brainstem-spinal cord preparation isolated from newborn rats preserves the neuron networks essential for respiratory rhythm generation and can produce respiratory activity for several hours under in vitro conditions [3, 12, 25]. This preparation has great advantages for pharmacological study of the respiratory center because it can be maintained in anesthetic-free conditions, and drugs can be applied by superfusion at known concentrations. Therefore, in the present study, we investigated the effects of aconitine on respiratory activity in isolated brainstem-spinal cord preparations from newborn rats.
Methods
Preparations and solutions
The experimental protocols were approved by the Animal Research Committee of Showa University (approval nos. 09049, 02022, 03066) in accordance with Law No. 105 for the care and use of laboratory animals of the Japanese Government. All efforts were made to minimize the number of animals used and their suffering.
Brainstems and spinal cords were isolated from Wistar rats at postnatal days 0–4 under deep anesthesia with isoflurane (approximately 0.13%). The specimens were cut slightly rostral to the level of the anterior inferior cerebellar artery and were continuously perfused at a rate of 2.5–3 ml/min with artificial cerebrospinal fluid (ACSF) [25] composed of (in mM): 124 NaCl, 5 KCl, 1.2 KH2PO4, 2.4 CaCl2, 1.3 MgCl2, 26 NaHCO3, 30 glucose, equilibrated with 95% O2 and 5% CO2, pH 7.4, at 25–26 °C. The respiratory activity was monitored by amplifying (× 10,000) the C4 activity through a glass capillary suction electrode and a 0.5 Hz high-pass filter (MEG-5200, Nihon Kohden, Tokyo, Japan). The electrical signals were digitized at 4 kHz (PowerLab, ADInstruments, Sydney, Australia) and stored on a personal computer using Lab Chart 7 Pro software program (ADInstruments). In some experiments, drugs were applied separately to the medulla or spinal cord [2, 12, 25]. Two thin plastic partitions were placed at the level of the medulla-spinal cord junction and C2 of the spinal cord. The solution was introduced from both ends of the perfusion chamber (i.e., the compartments of the medulla and the spinal cord) and sucked from the central compartment between the partitions.
Drugs
Aconitine was purchased from LKT Laboratories, Inc. (St. Paul, MN, USA) and was stocked as a 2.5 mM solution in 63% ethanol. Riluzole and lidocaine were purchased from Sigma-Aldrich (Tokyo, Japan) and were stocked as a 100 mM solution in dimethyl sulfoxide. Flufenamic acid was purchased from Sigma-Aldrich and was stocked as a 100 mM solution in 0.1 N NaOH. Tetrodotoxin (TTX) was purchased from Latoxan Laboratory (Portes lés Valence, France) and was stocked as a 1 mM solution. All stock solutions were stored at 4 °C.
Experimental protocols
-
1.
Dose-dependent effects of aconitine on C4 activity: As there were no similar previous studies on the concentration of aconitine and its dose dependence was unknown, we first conducted experiments with four concentration levels of aconitine (0.1, 0.5, 1.0, and 5.0 μM). The perfusion time for all drugs was 15 min. Activity after the washout of drugs was followed for a minimum of 15 min. Separate perfusion experiments were performed for 1.0 μM aconitine.
-
2.
Antagonistic effects of lidocaine or TTX on C4 activity after aconitine treatment: There are studies reporting that the effects of aconitine could be antagonized by a local anesthetic, lidocaine and a voltage-dependent sodium channel blocker, TTX [10, 20, 26]. Our previous study showed that lidocaine dose-dependently decreased the C4 burst rate, and 100 μM lidocaine induced an approximately 20% decrease in the burst rate [23]. We also examined the effects of various concentrations of TTX on C4 burst activity (Suppl. Figure 2 and Suppl. Table 1). On the basis of these results, we chose 100 μM lidocaine and 0.1 μM TTX for this protocol. First, 1 μM aconitine was applied for 15 min and then washed out. After 15 min of washout, 100 μM lidocaine or 0.1 μM TTX was applied for 15 min and then washed out.
-
3.
Effects of riluzole or flufenamic acid on C4 activity after aconitine + lidocaine treatment: To clarify the involvement of pacemaker properties in rhythm generation after aconitine + lidocaine treatment, the effects of riluzole or flufenamic acid which are known to inhibit respiratory pacemaker activity were examined. We previously reported that riluzole (10–100 μM) alone induced a dose-dependent decrease in the C4 burst rate without a noticeable change in burst amplitude [15]. The application of 100 μM riluzole induced an approximately 35% decrease in the burst rate. We also tested the effects of flufenamic acid because this drug inhibited Ca2+-dependent pacemaker activity [17, 21, 22], although this drug (100 μM) induced no significant effects on the C4 burst activity of brainstem-spinal cord preparations in the standard solution (unpublished observation). On the basis of these results, we chose 100 μM riluzole and 100 μM flufenamic acid for this protocol. First, 1 μM aconitine + 100 μM lidocaine was applied for 15 min. After 15-min washout, 100 μM riluzole or 100 μM flufenamic acid was applied for 15 min and then washed out.
-
4.
The involvement of pacemaker properties in rhythm generation after aconitine was also examined by perfusion with a low Ca2+/high Mg2+ (synaptic blockade) solution during monitoring firings of inspiratory neurons in the medulla because burst generation of neurons that have pacemaker properties could persist, even in the synaptic blockade solution [15, 18]. First, 1 μM aconitine was applied for 15 min. After 15 min of washout, the perfusate was changed to low Ca2+/high Mg2+ solution for 30–40 min. Then, the perfusate was changed to normal ACSF.
Membrane potential recordings
We recorded the membrane potential of respiratory-related neurons, i.e., pre-inspiratory (Pre-I), expiratory (Exp), and inspiratory (Insp) neurons, at the level 0–400 μm caudal to the caudal end of the facial nucleus [4] in the ventrolateral region of the medulla where respiratory-related neurons were frequently found (i.e., respiratory regions) by a ventral approach. Pre-I neurons were characterized by firings that started preceding the Insp phase and continued during the post-Insp phase. Exp neurons showed tonic firings that were inhibited during the Insp phase (or Insp and pre- and post-I phases). Insp neurons showed firings that were limited during the Insp phase. Intracellular recordings were conducted using a blind whole-cell patch-clamp method [12, 19] with a high input impedance DC amplifier (CEZ-3100; Nihon Kohden). The electrical signals were amplified (× 10) and digitized at 4 kHz (PowerLab, ADInstruments), and then stored on a personal computer using the Lab Chart 7 Pro software program (ADInstruments). The electrodes were created by pulling thin-wall borosilicate glass (TW100F-4; World Precision Instruments, Inc., Sarasota, FL, USA) while heating. The inner tip diameter was 1.2–2.0 μm, and the resistance was 4–8 MΩ. The electrodes were filled with a pipette solution containing 130 mM K-gluconate, 10 mM EGTA, 10 mM HEPES, 2 mM Na2-ATP, 1 mM CaCl2, 1 mM MgCl2, and KOH at pH 7.2–7.3. The electrode tip was filled with a 0.5% solution of Lucifer Yellow (lithium salt, Sigma-Aldrich) dissolved in the same solution for the histological analysis of the recorded cells. In some experiments, we also recorded the membrane potential of Insp motor neurons at the C4 level. Insp motor neurons were identified by antidromic activation by C4 ventral root stimulation and the location of Lucifer yellow-stained cells in the ventral horn.
After the experiment, the preparations were fixed in 4% paraformaldehyde in 0.1 M phosphate buffer solution at 4 °C and stored for histological analysis. Transverse 50-μm slices were cut using a vibrating-blade tissue slicer (PR07, Dosaka EM CO. Ltd., Osaka, Japan). The locations of the cell bodies of the recorded neurons were confirmed after staining with NeuroTrace™ Nissl staining (435/455 blue or 530/615 red fluorescence, Invitrogen). Labeled neurons were photographed using a fluorescence microscope (BX60; Olympus Optical, Tokyo, Japan). The cell body locations of the recorded neurons were identified and plotted in a figure.
Data analysis
The initial data analysis was performed using the Lab Chart 7 Pro software program (ADInstruments). The burst rate was calculated as an average of 3–5 min. After passing the normality test by the method of Kolmogorov and Smirnov, the significance of the values was analyzed by a paired t-test or one-way repeated-measures ANOVA, followed by a Tukey–Kramer multiple comparisons test at a confidence level of P < 0.05 using the GraphPad Prism 6 software program (GraphPad Software Inc., La Jolla, CA, USA).
Results
Dose-dependent effects of aconitine on C4 activity
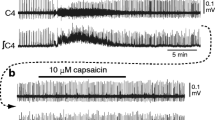
To examine the effects of aconitine, we perfused the preparation with 0.1, 0.5, 1.0, and 5 μM aconitine for 15 min, followed by a washout of at least 15 min (n = 5 in each experimental condition). The effects of aconitine were observed at concentrations of > 0.5 μM. Bath application of 0.5 or 1.0 μM aconitine caused an increase in respiratory rhythm and a decrease in amplitude (Fig. 1 A, B). The effects were sustained even after washout for > 15 min. The inspiratory burst duration was not significantly changed at these concentrations of aconitine (Fig. 1F). Bath application of 5 µM aconitine caused the disappearance of C4 activity without recovery after washout (Fig. 1C). A summary is shown in Fig. 1D-F, and detailed values are shown in Table 1.
Examples of C4 activity changes following the application of 0.5 μM aconitine (A), 1 μM aconitine (B), and 5 μM aconitine (C). a, Activity in control. b, Activity after 15-min application of aconitine. c, Activity after 15 min of washout. D-F, Summary of changes in the amplitude (D), burst rate (E), and burst duration (F) of C4 inspiratory activity, which are presented as relative values to the control (before the application of aconitine). Five samples were analyzed in each condition. Abscissa axis: a, activity in control; b, activity after 15-min application of aconitine; c, activity after 15-min washout. Dark blue, 0 μM; brown, 0.5 μM; light blue, 1 μM; yellow, 5 μM aconitine application. Note that the amplitude of the C4 inspiratory burst decreased extremely in association with the application of 0.5 or 1 μM aconitine and was not detectable after the application of 5 μM aconitine. Statistical significance was determined by a one-way repeated-measures ANOVA followed by Tukey–Kramer multiple comparisons test (*P < 0.05, **P < 0.01, ***P < 0.001) in comparison to the control values
Effects of separate perfusion of the medulla or spinal cord with aconitine on C4 activity
Next, we conducted an experiment to determine whether changes of respiratory activity induced by aconitine were attributable to effects in the medulla or spinal cord (n = 5 in each experimental condition). We perfused the preparation with 1 µM aconitine for 15–20 min on either the medullary or spinal side and then washed it out. Application to the medulla caused a decrease in C4 amplitude and an increase in respiratory rhythm. These effects persisted even after washout for > 15 min (Fig. 2A). In contrast, application to the spinal cord caused no significant change in inspiratory burst rate, but this resulted in a decrease in C4 amplitude (Fig. 2B). A summary is shown in Fig. 2C-E, and the detailed values are shown in Table 2.
Examples of C4 activity changes following the separate application of 1 μM aconitine to the medulla (A) and spinal cord (B). a, Activity in control. b, Activity after 15-min application of aconitine. c, Activity after 15-min washout. C-E, Summary of changes in the amplitude (C), burst rate (D), and burst duration (E) of C4 inspiratory activity, which are presented as relative values to the control (before the application of aconitine). Five samples were analyzed in each condition. Abscissa axis: a, activity in control; b, activity after 15-min application of aconitine; c, activity after 15-min washout. Orange, Application to the medulla; green, application to the spinal cord. Note that the amplitude of the C4 inspiratory burst decreased extremely in association with the application of aconitine. Statistical significance was determined by a one-way repeated-measures ANOVA followed by Tukey–Kramer multiple comparisons test (**P < 0.01, ***P < 0.001) in comparison to the control values
Antagonistic effects of lidocaine or TTX on C4 activity after aconitine treatment
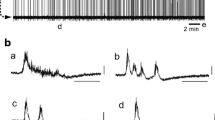
We examined the antagonistic effects of lidocaine or TTX on the effects of aconitine (n = 5 in each experimental condition). The preparation was perfused with 1 µM aconitine for 15–20 min and washed out. After 15-min washout of aconitine, 100 µM lidocaine or 100 nM TTX was perfused for 15–20 min. The application of lidocaine led to a partial recovery of C4 amplitude, a further increase in respiratory rhythm, and a decrease in inspiratory burst duration. These effects persisted after washout of lidocaine for > 15 min (Fig. 3A). Similarly, the application of TTX after aconitine treatment caused a partial recovery of C4 amplitude and a decrease in respiratory rhythm. The recovery of C4 amplitude was sustained even after washout of TTX for > 15 min (Fig. 3B). Bath application of TTX did not result in a significant difference in inspiratory burst duration. A summary is shown in Fig. 3C-E, and the detailed values are shown in Table 3.
Examples of C4 activity changes following the application of 100 μM lidocaine (A) and 0.1 μM tetrodotoxin (TTX) (B) after treatment with 1 μM aconitine. a, Activity in control. b, Activity after 15-min application of aconitine. c, Activity after 15-min washout of aconitine. d, Activity after 15-min application of 100 μM lidocaine (A’) or 0.1 μM TTX (B’). e, Activity after 15-min washout of lidocaine or TTX. C-E Summary of changes in the amplitude (C), burst rate (D), and burst duration (E) of C4 inspiratory activity, which are presented as relative values to the control (before the application of aconitine). Five samples were analyzed in each condition. Abscissa axis: a, activity in control; b, activity after 15-min application of aconitine; c, activity after 15-min washout of aconitine; d, activity after 15-min application of 100 μM lidocaine or 0.1 μM TTX; e, activity after 15-min washout of lidocaine or TTX. Orange, application of aconitine + lidocaine; blue, application of aconitine + TTX. Note that the amplitude of the C4 inspiratory burst decreased extremely in association with the application of aconitine and partially recovered after the application of lidocaine or TTX. Statistical significance was determined by a one-way repeated-measures ANOVA followed by Tukey–Kramer multiple comparisons test ($P < 0.05, $$P < 0.01, $$$P < 0.001) in comparison to values immediately before the application of lidocaine or TTX. See Table 3 for other detailed statistics
Effects of riluzole or flufenamic acid on C4 activity after aconitine + lidocaine treatment
Aconitine + lidocaine treatment induced a remarkable increase in the C4 burst rate. To investigate which mechanisms are involved in this increased respiratory rhythm, we examined the effects of riluzole or flufenamic acid, which are known to inhibit inspiratory pacemaker cells [22] (n = 5 in each experimental condition). The preparation was perfused with 1 µM aconitine plus 100 µM lidocaine for 15–20 min. After washout for > 15 min, 100 μM riluzole or 100 µM flufenamic acid was applied for 15–20 min. Application of riluzole after aconitine + lidocaine treatment induced an increase in C4 amplitude without change in the burst rate and duration (in comparison to values immediately before the application of riluzole) (Fig. 4 Ac-e). In contrast, the application of flufenamic acid after aconitine + lidocaine treatment induced a significant decrease in C4 amplitude without change in the burst rate and duration (compared to values immediately before flufenamic acid application) (Fig. 4 Bc-e). A summary is shown in Fig. 4C-E, and the detailed values are shown in Table 4.
Examples of C4 activity changes following the application of 100 μM riluzole (A) and 100 μM flufenamic acid (FFA) (B) after treatment with 1 μM aconitine + 100 μM lidocaine (Lido). a, Activity in control. b, Activity after 15-min application of aconitine + lidocaine. c, Activity after 15-min washout of aconitine + lidocaine. d, Activity after 15-min application of 100 μM riluzole (A’) or 100 μM FFA (B’). e, Activity after 15-min washout of riluzole or FFA. C-E Summary of changes in the amplitude (C), burst rate (D), and burst duration (E) of C4 inspiratory activity, which are presented as relative values to the control (before the application of aconitine). Five samples were analyzed in each condition. Abscissa axis: a, activity in control; b, activity after 15-min application of aconitine + lidocaine; c, activity after 15-min washout of aconitine + lidocaine; d, activity after 15-min application of 100 μM riluzole or 100 μM FFA; e, activity after 15-min washout of riluzole or FFA. Orange, application of riluzole; blue, application of FFA. Note that the amplitude of the C4 inspiratory burst partially recovered after the application of riluzole, and the burst rate tended to increase after the application of riluzole or FFA. Statistical significance was determined by a one-way repeated-measures ANOVA followed by Tukey–Kramer multiple comparisons test ($P < 0.05) compared with values immediately before the application of riluzole or FFA. See Table 4 for other detailed statistics
Effects of aconitine on respiratory-related neurons in the medulla and spinal cord
We examined the effects of 1 μM aconitine on 7 Insp neurons, 6 Pre-I neurons, and 5 Exp neurons in the rostral ventrolateral medulla, as well as 5 Insp motor neurons in the spinal cord at the C4 level. The application of aconitine depolarized Pre-I neurons, Exp neurons, and Insp motor neurons, whereas no significant change was observed in the membrane potential of Insp neurons in the medulla (Figs. 5 and 6, Table 5). After aconitine treatment, the firing pattern of Pre-I neurons changed from a burst pattern to a tonic firing pattern, indicating the disappearance of burst activity (Fig. 5Bbc). Inspiratory motor neurons showed tonic firings during the interburst interval (i.e., Exp phase) (Fig. 6Abc). The above results of experiments with riluzole and flufenamic acid implied that the facilitated rhythm after treatment with aconitine (+ lidocaine) might be produced by independent mechanisms of burst-generating pacemaker properties of respiratory neurons [13, 15]. Intrinsic burst generation should be preserved in low Ca2+/high Mg2+ synaptic blockade solution [15, 18]. Therefore, we examined the effects of perfusion with a low Ca2+/high Mg2+ solution on the burst generation of medullary inspiratory neurons (n = 4) after treatment with 1 μM aconitine. After 30–40 min in the low Ca2+/high Mg2+ solution, C4 inspiratory activity and firings of inspiratory neurons disappeared, whereas excitatory postsynaptic potentials remained. This suppression was reversed when the perfusate was returned to the normal solution (Fig. 7). Figure 8 shows the location of the Lucifer yellow-stained medullary cells that were successively identified in the histological examination after the experiments. Recorded cells were located in the rostral ventrolateral medulla of the rostral part of the preBötzinger complex from the caudal part of the parafacial respiratory group [4].
Examples of membrane potential (Vm) and C4 activity changes following the application of 1 μM aconitine; inspiratory (Insp) neurons (A), pre-inspiratory (Pre-I) neurons (B), and expiratory (Exp) neurons (C). a, Activity in control. b, Activity after 15-min application of aconitine. c, Activity after 15-min washout. Note that after aconitine treatment, the firing pattern of Pre-I neurons changed from a burst pattern to a tonic firing pattern in association with membrane depolarization, indicating the disappearance of burst activity. d, A low magnification view of slices where recorded neurons were identified. e, A higher magnification view of the highlighted square in d. Arrows indicate the location of the recorded Lucifer yellow-labeled neuron. IO, inferior olivary nucleus
An example of membrane potential (Vm) changes in C4 inspiratory motor neurons and C4 activity changes following the application of 1 μM aconitine. a, Activity in control. b, Activity after 15-min application of aconitine. c, Activity after 15-min washout. Note the membrane depolarization and appearance of tonic firings during interburst phases. B, Antidromic action potential induced by C4 ventral root stimulation. C, Location of the Lucifer yellow-labeled neuron recorded in the ventral horn
Effects of low Ca2+/high Mg2+ synaptic blockade solution on the burst activity of inspiratory neurons after aconitine treatment. a, Activity in control. b, Activity after 15-min application of 1 μM aconitine. c, Activity after 15-min washout. d, Activity after 40 min low Ca2+/high Mg2+ solution. e, Activity after returning to normal ACSF. Note that after 40 min in low Ca2+/high Mg2+ solution, C4 inspiratory activity and firings of inspiratory neurons disappeared, whereas EPSPs remained. B-1, A low-magnification view of slices where the recorded neuron was identified; B-2, A higher-magnification view of the highlighted square in B-1. Arrows indicate the location of the Lucifer yellow-labeled neuron recorded. ACSF, artificial cerebrospinal fluid; EPSPs, excitatory postsynaptic potentials; IO, inferior olivary nucleus
Location of recorded neurons in the ventrolateral medulla. Neurons labeled with Lucifer yellow were distributed in the range of 0–450 μm caudal to the caudal end of the facial nucleus and were plotted in two sections (A and B). Closed circles, inspiratory neurons; open circles, pre-inspiratory neurons; and closed triangles, expiratory neurons. NA, nucleus ambiguus; CST, corticospinal tract; IO, inferior olivary nucleus; XII, hypoglossal nucleus
Discussion
The application of aconitine to brainstem-spinal cord preparations of neonatal rats resulted in a dose-dependent depression of the Insp burst amplitude and an increase in the burst rate (rhythm-facilitating effect). Separate perfusion experiments showed that application of aconitine to the medulla led to a rhythm-facilitating effect and an amplitude-suppressing effect. Conversely, the application of aconitine to the spinal cord only produced an amplitude-suppressing effect. Thus, the amplitude decrease in Insp burst was attributable to the effects of aconitine on motor neurons in the spinal cord as well as on medullary neurons, including interneurons and premotor neurons, whereas the rhythm-facilitating effect was due to aconitine effects on medullary neurons. The effects of aconitine persisted after washout. This could be explained by the characteristics of aconitine, which is a lipophilic substance that binds to site 2 of sodium channels with strong affinity [28].
It was reported that the LD50 value of aconitine was approximately 0.1 mg/kg in mice [9]. On the basis of this value, we calculated the concentration in the plasma as approximately 2 μM, if this substance moved into the plasma. This concentration was comparable to the concentrations of the present study, which produced obvious effects on respiratory activity.
Both lidocaine and TTX showed a recovery of C4 amplitude that was decreased by aconitine treatment, but they exhibited different antagonistic effects on respiratory rhythm. Lidocaine further facilitated respiratory rhythm, whereas TTX temporarily reversed it. Lidocaine binds to the local anesthetic binding site of sodium channels, whereas TTX binds to site 1 of sodium channels [28]. These differences in binding sites might have contributed to the changes observed in respiratory rhythm.
Treatment with aconitine and subsequent lidocaine induced a rhythm-facilitating effect that persisted after washout with a burst rate that was approximately four times that of the control group. We investigated whether pacemaker properties are involved in the generation of this facilitated rhythm. This rhythm generation was not suppressed by the administration of riluzole or flufenamic acid, which are known to inhibit respiratory pacemaker activity [17, 21, 22]. Thus, these results suggest that pacemaker properties were not involved in the generation of facilitated rhythm after treatment with aconitine followed by lidocaine.
Membrane potential changes in respiratory-related neurons following 1 μM aconitine treatment differed in neuronal subtypes: depolarization in Pre-I, Exp, and spinal motor neurons but no significant change in the Insp neurons in the medulla. In particular, burst generation in Pre-I neurons was depressed, and tonic firings appeared after aconitine treatment. It is well known that the voltage-dependent sodium channels are the target site of aconitine. However, this mechanism seemed to be not straightforward in understanding why changes of resting membrane potentials after aconitine treatment differed in neuronal subtypes. Recently, it was reported that a channel that generates “leak” sodium currents could regulate the excitability of neurons [16, 24] and influence the resting membrane potential of respiratory neurons [30]. Although there have been no reports indicating that aconitine affects the “leak” sodium channel, this may be considered as a possible additional mechanism. Our findings suggest that sodium channels could work as one of factors modulating respiratory activity.
Previous studies have suggested that some Pre-I neurons express persistent sodium currents (i.e., riluzole-sensitive negative slope conductance), which are essential to produce intrinsic burst generation [14, 15, 23]. This burst-generating pacemaker property of Pre-I neurons was not involved in generation of the facilitated rhythm, which was resistant to riluzole after aconitine. Alternatively, sustained inactivation of the persistent sodium current might occur after aconitine because the burst generation of Pre-I neurons disappeared. It was also reported that some Insp neurons have intrinsic burst-generating properties [11]. Intrinsic burst generation should be retained in low Ca2+/high Mg2+ synaptic blockade solution [15, 18]. However, the burst activity in Insp neurons disappeared after perfusion with the synaptic blockade solution. This result was also consistent with the above suggestion that the pacemaker property is not involved in the facilitated rhythm after aconitine and further suggested that mutual excitatory synaptic connections are important in fast rhythm generation. This mechanism coincides with a model of rhythm generation by the group pacemaker [8, 21]. Under standard experimental conditions, the synaptic activities of Insp neurons were almost completely silenced in low Ca2+/high Mg2+ solution [18]. However, after aconitine treatment, some synaptic activities in Insp neurons remained in the low Ca2+/high Mg2+ solution. We speculated that Ca2+-independent transmitter release [6] might be involved in this synaptic activity.
Conclusion
We found that aconitine has the dose-dependent effects of depressing C4 amplitude and increasing respiratory rhythm. The amplitude decrease could be caused by effects on spinal motor neurons and medullary (premotor and inter) neurons, whereas effects on medullary neurons facilitated respiratory rhythm. Lidocaine and TTX reversed the effects of aconitine in different ways, likely because they target different sites on sodium channels. Pacemaker properties might not be involved in the facilitation of rhythm generation after aconitine treatment. The results of synaptic blockade experiments are consistent with the facilitation of rhythm generation by the group pacemaker mechanism. Overall, our findings shed light on the effects of aconitine on respiratory activity and provide new insights into a role of sodium channels involved in respiratory rhythm modulation.
Data availability
The datasets generated and analyzed during the current study will be made available by the corresponding author on reasonable request.
Change history
25 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00424-023-02861-5
References
Ameri A (1998) The effects of Aconitum alkaloids on the central nervous system. Prog Neurobiol 56:211–235. https://doi.org/10.1016/s0301-0082(98)00037-9
Arata A, Onimaru H, Homma I (1998) The adrenergic modulation of firings of respiratory rhythm-generating neurons in medulla-spinal cord preparation from newborn rat. Exp Brain Res 119:399–408. https://doi.org/10.1007/s002210050355
Ballanyi K, Onimaru H, Homma I (1999) Respiratory network function in the isolated brainstem-spinal cord of newborn rats. Prog Neurobiol 59:583–634
Ballanyi K, Ruangkittisakul A, Onimaru H (2009) Opioids prolong and anoxia shortens delay between onset of preinspiratory (pFRG) and inspiratory (preBotC) network bursting in newborn rat brainstems. Pflugers Arch 458:571–587
Catterall WA (1980) Neurotoxins that act on voltage-sensitive sodium channels in excitable membranes. Annu Rev Pharmacol Toxicol 20:15–43. https://doi.org/10.1146/annurev.pa.20.040180.000311
Chai Z, Wang C, Huang R, Wang Y, Zhang X, Wu Q, Wang Y, Wu X, Zheng L, Zhang C, Guo W, Xiong W, Ding J, Zhu F, Zhou Z (2017) Ca(V)2.2 Gates Calcium-Independent but Voltage-Dependent Secretion in Mammalian Sensory Neurons. Neuron 96:1317–1326. https://doi.org/10.1016/j.neuron.2017.10.028
Chan TY (2009) Aconite poisoning. Clin Toxicol (Phila) 47:279–285. https://doi.org/10.1080/15563650902904407
Feldman JL, Del Negro CA (2006) Looking for inspiration: new perspectives on respiratory rhythm. Nat Rev Neurosci 7:232–242. https://doi.org/10.1038/nrn1871
Friese J, Gleitz J, Gutser UT, Heubach JF, Matthiesen T, Wilffert B, Selve N (1997) Aconitum sp. alkaloids: the modulation of voltage-dependent Na+ channels, toxicity and antinociceptive properties. Eur J Pharmacol 337:165–174. https://doi.org/10.1016/s0014-2999(97)01268-5
Hong B, He J, Le Q, Bai K, Chen Y, Huang W (2019) Combination Formulation of Tetrodotoxin and Lidocaine as a Potential Therapy for Severe Arrhythmias. Mar Drugs 17:685. https://doi.org/10.3390/md17120685
Johnson SM, Smith JC, Funk GD, Feldman JL (1994) Pacemaker behavior of respiratory neurons in medullary slices from neonatal rat. J Neurophysiol 72:2598–2608. https://doi.org/10.1152/jn.1994.72.6.2598
Katsuki S, Ikeda K, Onimaru H, Dohi K, Izumizaki M (2021) Effects of acetylcholine on hypoglossal and C4 nerve activity in brainstem-spinal cord preparations from newborn rat. Respir Physiol Neurobiol 293:103737. https://doi.org/10.1016/j.resp.2021.103737
Koizumi H, Smith JC (2008) Persistent Na+ and K+-dominated leak currents contribute to respiratory rhythm generation in the pre-Botzinger complex in vitro. J Neurosci 28:1773–1785. https://doi.org/10.1523/JNEUROSCI.3916-07.2008
Kotani S, Irie S, Izumizaki M, Onimaru H (2018) Effects of eugenol on respiratory burst generation in newborn rat brainstem-spinal cord preparations. Pflugers Arch 470:385–394. https://doi.org/10.1007/s00424-017-2074-z
Lin ST, Onimaru H (2015) Effects of riluzole on respiratory rhythm generation in the brainstem-spinal cord preparation from newborn rat. Neurosci Res 94:28–36. https://doi.org/10.1016/j.neures.2014.12.001
Lutas A, Lahmann C, Soumillon M, Yellen G (2016) The leak channel NALCN controls tonic firing and glycolytic sensitivity of substantia nigra pars reticulata neurons. Elife 5:e15271. https://doi.org/10.7554/eLife.15271
Del Negro CA, Morgado-Valle C, Hayes JA, Mackay DD, Pace RW, Crowder EA, Feldman JL (2005) Sodium and calcium current-mediated pacemaker neurons and respiratory rhythm generation. J Neurosci 25:446–453. https://doi.org/10.1523/JNEUROSCI.2237-04.2005
Onimaru H, Arata A, Homma I (1995) Intrinsic burst generation of preinspiratory neurons in the medulla of brainstem-spinal cord preparations isolated from newborn rats. Exp Brain Res 106:57–68
Onimaru H, Homma I (1992) Whole cell recordings from respiratory neurons in the medulla of brainstem-spinal cord preparations isolated from newborn rats. Pflugers Arch 420:399–406
Ono T, Hayashida M, Tezuka A, Hayakawa H, Ohno Y (2013) Antagonistic effects of tetrodotoxin on aconitine-induced cardiac toxicity. J Nippon Med Sch 80:350–361. https://doi.org/10.1272/jnms.80.350
Pace RW, Mackay DD, Feldman JL, Del Negro CA (2007) Inspiratory bursts in the preBotzinger complex depend on a calcium-activated non-specific cation current linked to glutamate receptors in neonatal mice. J Physiol 582:113–125. https://doi.org/10.1113/jphysiol.2007.133660
Peña F, Parkis MA, Tryba AK, Ramirez JM (2004) Differential contribution of pacemaker properties to the generation of respiratory rhythms during normoxia and hypoxia. Neuron 43:105–117. https://doi.org/10.1016/j.neuron.2004.06.023
Shakuo T, Lin ST, Onimaru H (2016) The effects of lidocaine on central respiratory neuron activity and nociceptive-related responses in the brainstem-spinal cord preparation of the newborn rat. Anesth Analg 122:1586–1593. https://doi.org/10.1213/ANE.0000000000001205
Shi Y, Abe C, Holloway BB, Shu S, Kumar NN, Weaver JL, Sen J, Perez-Reyes E, Stornetta RL, Guyenet PG, Bayliss DA (2016) Nalcn Is a “Leak” Sodium Channel That Regulates Excitability of Brainstem Chemosensory Neurons and Breathing. J Neurosci 36:8174–8187. https://doi.org/10.1523/JNEUROSCI.1096-16.2016
Suzue T (1984) Respiratory rhythm generation in the in vitro brain stem-spinal cord preparation of the neonatal rat. J Physiol 354:173–183
Tanaka K, Sakai S (1953) Modification of the cardiovascular-respiratory action of aconitin by intravenously injected procaine in rabbits. Jpn J Pharmacol 2:144–148. https://doi.org/10.1254/jjp.2.144
Thoby-Brisson M, Karlen M, Wu N, Charnay P, Champagnat J, Fortin G (2009) Genetic identification of an embryonic parafacial oscillator coupling to the preBotzinger complex. Nat Neurosci 12:1028–1035. https://doi.org/10.1038/nn.2354
Wang SY, Wang GK (2003) Voltage-gated sodium channels as primary targets of diverse lipid-soluble neurotoxins. Cell Signal 15:151–159. https://doi.org/10.1016/s0898-6568(02)00085-2
Yamanaka H, Doi A, Ishibashi H, Akaike N (2002) Aconitine facilitates spontaneous transmitter release at rat ventromedial hypothalamic neurons. Br J Pharmacol 135:816–822. https://doi.org/10.1038/sj.bjp.0704517
Yeh SY, Huang WH, Wang W, Ward CS, Chao ES, Wu Z, Tang B, Tang J, Sun JJ, Esther van der Heijden M, Gray PA, Xue M, Ray RS, Ren D, Zoghbi HY (2017) Respiratory Network Stability and Modulatory Response to Substance P Require Nalcn. Neuron 94:294–303. https://doi.org/10.1016/j.neuron.2017.03.024
Funding
This work was partially supported by JSPS KAKENHI (grant no. 19K06946).
Author information
Authors and Affiliations
Contributions
S.Y. and H.O. designed and performed the experiments, analyzed the data, performed the histological analysis, and wrote the manuscript. M.I. helped draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The experimental protocols were approved by the Animal Research Committee of Showa University (approval nos. 09049, 02022, 03066) in accordance with Law No. 105 for the care and use of laboratory animals of the Japanese Government.
Human and animal ethics
This study was performed with animal experiments. All efforts were made to minimize the number of animals used and their suffering.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare no commercial or financial conflicts of interest in association with the present study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original article published with corrections in Table 2. The presentation of the entries in Table 2 has been changed and modified.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoda, S., Onimaru, H. & Izumizaki, M. Effects of aconitine on the respiratory activity of brainstem-spinal cord preparations isolated from newborn rats. Pflugers Arch - Eur J Physiol 475, 1301–1314 (2023). https://doi.org/10.1007/s00424-023-02857-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02857-1