Abstract
Purpose
Adrenocortical carcinoma (A.C.C.) is a rare tumour, often discovered at an advanced stage and associated with a poor prognosis. Surgery is the treatment of choice. We aimed to review the different surgical approaches trying to compare their outcome.
Methods
This comprehensive review has been carried out according to the PRISMA statement. The literature search was performed in PubMed, Scopus, the Cochrane Library and Google Scholar.
Results
Among all studies identified, 18 were selected for the review. A total of 14,600 patients were included in the studies, of whom 4421 were treated by mini-invasive surgery (M.I.S.). Ten studies reported 531 conversions from M.I.S. to an open approach (OA) (12%). Differences were reported for operative times as well as for postoperative complications more often in favour of OA, whereas differences for hospitalization time in favour of M.I.S.
Some studies showed an R0 resection rate from 77 to 89% for A.C.C. treated by OA and 67 to 85% for tumours treated by M.I.S. The overall recurrence rate ranged from 24 to 29% for A.C.C. treated by OA and from 26 to 36% for tumours treated by M.I.S.
Conclusions
OA should still be considered the standard surgical management of A.C.C. Laparoscopic adrenalectomy has shown shorter hospital stays and faster recovery compared to open surgery. However, the laparoscopic approach resulted in the worst recurrence rate, time to recurrence and cancer-specific mortality in stages I–III ACC. The robotic approach had similar complications rate and hospital stays, but there are still scarce results about oncologic follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adrenocortical carcinoma (A.C.C.) is a rare and aggressive endocrine malignancy, with an annual incidence of approximately 1–2/1,000,000 people worldwide, accounting for 0.05–0.2% of all malignancies. In a recent Japanese nationwide survey, A.C.C.s accounted for 1.4% of many incidentalomas [1]. The age distribution is bimodal, with the first peak in childhood and a second higher peak in the fourth and fifth decade of life, with a slight female predominance [2]. Although most A.C.C.s are sporadic, many hereditary syndromes have been associated with this type of cancer, including Beckwith-Wideman syndrome, multiple endocrine neoplasia type 1, Li-Fraumeni, congenital adrenal hyperplasia, familial adenomatous polyposis and Lynch syndrome [3].
The diagnosis of A.C.C. is often presumptive based on imaging (C.T. or M.R.I.) and hormonal workup and is confirmed postoperatively on surgical pathology. Malignancy must be suspected when the tumour size ranges from 4 to 6 cm, with an increased risk of malignancy for masses larger than 4 cm. The literature defines giant adrenal tumours (G.A.T.) as adrenal masses larger than 6 cm. G.A.T. are considered rare, with an incidence ranging from 8.6 to 38.6% of all adrenal tumours [3]. In the literature, the size criteria remain the main subject to establish the indication for surgery. The size is an essential variable in predicting malignancy. If the lesions are smaller than 4 cm, the risk of malignancy is approximately 2%, while for lesions of 4–6 cm, the risk of malignancy is 6%, and for lesions of 6 cm, the risk of malignancy is 25% (10–53%) [4]. Moreover, an adrenal nodule increasing in size by more than 1 cm per year must be considered potentially malignant.
At the time of the first diagnosis, A.C.C. is often at an advanced stage, with distant metastases found in 20% of patients, with the prevalent location in the lungs and liver (45% and 40%, respectively). Thus, the prognosis of A.C.C. is often poor, with overall survival (O.S.) of 3.21 years from diagnosis [5].
In 2004, the World Health Organization (WHO) and Union for International Cancer Control (UICC) introduced the first Tumor, Node and Metastasis (T.N.M.) staging system for A.C.C. based on the traditional McFarlane classification, modified by Sullivan. This classification system has been recently challenged due to the failure to discriminate between the prognosis of patients classified as stages II and III. Rather, the newly introduced European Network for the Study of Adrenal Tumors (ENSAT) system has become more widely adopted due to its reliable stratification of patient outcomes. The ENSAT staging system defines A.C.C. disease into four stages. Stage I (< 5 cm) and stage II (> 5 cm) tumours are confined to the adrenal gland. Stage III tumours extend into the surrounding tissue (para-adrenal adipose tissue or adjacent organs) or involve locoregional lymph nodes. Stage IV includes distant metastases, including lung (40–80%), liver (40–90%) and bone (5–20%) [6]. Although prognosis is certainly dependent on an accurate diagnosis, survival of patients with A.C.C. is mainly associated with intraoperative findings and a radical surgical approach, with the R0 margin being one of the most important prognostic factors. When surgical excision is deemed complete, the 5-year survival ranges from 32 to 58%, but when incomplete, the median survival is generally < 1 year (range, 2–16 months). Unfortunately, even after an apparent complete resection, local or distant relapse occurs in nearly 80% of patients. Complete surgical excision with microscopically negative margins is, therefore, the standard of care for localized/locally advanced disease (ENSAT I–III), leading to palliation of symptoms for patients with functional A.C.C.s and an increased disease-free (D.F.S.) and overall survival (O.S.) [7].
Open surgery has been recognized as the gold standard for A.C.C. because of the better achievement of R0 resection. Nevertheless, minimally invasive surgery (M.I.S.), which includes laparoscopic adrenalectomy (L.A.) and robotic adrenalectomy (R.A.), is increasingly considered a feasible approach for the resection of adrenal tumours. Indeed, in recent years, many studies in the literature have reported excellent results in terms of surgical and oncological outcomes with the minimally invasive approach to malignant adrenal tumours and G.A.T. [4].
This study aimed to review the current literature on the role of M.I.S. versus open technique in the surgical management of primary A.C.C. (ENSAT I–III) in adults. Since the oncological efficacy of surgery for A.C.C. is the most debated topic, this article has tried to critically evaluate which may be considered the best surgical approach depending on the ENSAT stage and to verify which are the most appropriate criteria for an oncologically adequate resection.
Method
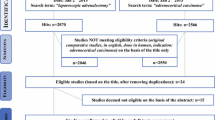
This comprehensive review was performed according to the methodological criteria reported in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (Fig. 1) [8]. The literature search was performed in PubMed, Scopus, Google Scholar and the Cochrane Library databases. The research was focused on the following issue: which kind of surgery should be proposed for which patients are affected by suspected/confirmed adrenocortical carcinoma, depending on the stage, size and other preoperative features? Which are the expected results of open, laparoscopic and/or robotic approaches? The search records were: ((surgery) OR (adrenalectomy)) AND (adrenocortical carcinoma). The research was limited to studies published after 2002, adult patients and papers written in English. The literature search was performed independently by two authors (AG and CB). Any discrepancies between the reviewers were discussed and solved by consensus. Quality studies were assessed for the level of evidence per the previously described methodology. Quality assessment of retrieved studies was performed with JADAD scores in the case of randomized clinical trials or MINORS scores for non-randomized studies. The risk of bias was assessed using the revised Cochrane risk-of-bias tool for non-randomized studies (ROBINS-I) [9].
Results
Studies included in our review article comparing minimally invasive surgical approaches to open adrenalectomy are reported in Table 1 [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Surgical and oncological outcomes and the differences in terms of overall survival (O.S.) and disease-free survival (D.F.S.) between the open and laparoscopic approaches are shown in Table 2. In Fig. 2, the evaluation of the risk of bias in the review articles is evaluated according to the revised Cochrane risk-of-bias tool for non-randomized studies (ROBINS-I).
Among all studies identified, 18 were selected for entering the review [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. A total of 14600 patients were included in the selected studies, of whom 4421 were treated by mini-invasive approaches, and 10179 patients were treated by open surgery. In three studies, M.I.S. included both a laparoscopic and a robotic approach [8, 10, 15]. Some authors suggested that LA should be only performed in high-volume referral centres [25]. Ten studies reported 531 conversions from M.I.S. to an open approach (12%) [8, 11,12,13,14,15,16,17,18,19]. Among all included studies, A.C.C. staging was performed based on ENSAT stage: three studies involved stage I–II ACC [12, 14, 19], and two studies involved patients with stage I–III and stage I–IV disease, respectively [16, 21]. Patients treated with open adrenalectomy (OA) had a median tumour size of 8.6 to 11.9 cm, whereas those with LA were from 7.1 to 8.5 cm. Some studies showed that LA is effective for A.C.C. when the tumour size is < 10 cm and showed no local invasion, enlarged lymph nodes or distant metastases (ENSAT stage I–II) [15, 20,21,22,23,24,25]. Differences were reported for operative times as well as for postoperative complications more often in favour of OA [18, 19, 21,22,23,24], whereas differences for hospitalization time in favour of LA [13,14,15,16,17,18,19, 21,22,23,24]. In particular, the overall average complication rate reported after OA was 25% while after LA was 29%, conversely, the mean postoperative hospital stay after M.I.S. was 3.7 days vs 6 days after OA. Conversely, LA was mostly performed in many centers with a percentage of 74.5% for the treatment of ACC [15,16,17,18,19,20,21,22,23,24,25], while in other centers OA represents the standard operative technique in over 53% of the procedures [17,18,19].
Some authors state that LA for A.C.C. is associated with a high recurrence rate, particularly in peritoneal carcinomatosis [8, 12,13,14,15,16,17,18,19,20,21,22]. Other studies showed an R0 resection rate from 77 to 89% for A.C.C. treated by OA and 67 to 85% for tumours treated by mini-invasive surgery [22,23,24,25,26]. Some studies compared M.I.S. vs open lymph node (L.N.D.) dissection [14]. Several studies reported detailed follow-ups. The local recurrence rate ranged from 34 to 54% for A.C.C. treated by OA, and 44 to 51% for tumours treated by mini-invasive surgery [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. The overall recurrence rate ranged from 24 to 29% for A.C.C. treated by OA and from 26 to 36% for tumours treated by mini-invasive surgery [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. The median disease-free survival (D.F.S.) ranged from 26 to 38 months for A.C.C. treated by OA and from 21 to 32 months for tumours treated by mini-invasive surgery [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Time to recurrence and cancer-specific mortality were similar between LA and OA. The rates of positive margins in the LA group and OA were similar. In contrast, tumour spillage was demonstrated in 17% of patients in OA and 22% in LA. OA is considered the treatment of choice for A.C.C. according to most of the meta-analysis published [12, 14, 21]. They compared OA vs minimally invasive surgery (MIS). Although no significant differences were found for OS (HR 0.97, p = 0.801), cancer-specific survival (HR 1.4, p = 0.869) and recurrence/disease-free survival (HR 0.96, p = 0.791) between the two approaches, MIS was significantly associated with earlier recurrence (WMD 8.42, p = 0.048), positive surgical margin (RR 1.56, p = 0.018) and peritoneal recurrence (RR 2.63, p < 0.001).
Regardless of the surgical approach used, there is a general agreement about the rules of oncologic surgery: “R0 resection en bloc”, “complete excision”, “no tumour grasping or fragmentation or tumour capsule effraction”. The 5-year overall survival for R0 versus R1 resection was 33–68% (p < 0,001), and the 5-year recurrence-free survival for R0 and R1 resection was 28–34%. (p = 0,60), respectively [8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
The potential role of the robotic approach (RA) has been shown to have several theoretical advantages compared to LA [8, 11, 15]. To our knowledge, no specific or dedicated studies about RA performed for A.C.C. have been published. Data regarding adrenalectomy performed for A.C.C. with minimally invasive robotic techniques are extracted from more general studies and only a few articles report and compare RA to LA or OA in the management of A.C.C. Recent evidence suggests that robotic adrenalectomy can be performed safely and effectively with the potential advantages of a shorter hospital stay, less blood loss and lower postoperative complications [27] Different technical approaches are available such as robotic-assisted lateral or anterior transabdominal adrenalectomy and robotic-assisted posterior retroperitoneoscopic adrenalectomy. The transperitoneal approach is advisable for the larger working space, the easier orientation and the magnification of surrounding anatomical structures. The retroperitoneal approach mimics OA and should be preferred in the case of bilateral tumours or previous abdominal surgeries [28, 29].
Agcaoglu et al. [30] performed 62 adrenalectomies for tumours larger than 5 cm (24 robotic vs. 38 laparoscopic) showing significant shorter operative time (159.4 13.4 vs 187.2 8.3 min, p = 0.043), less conversion rate (4% vs. 11%, p = 0.43) and shorter hospital stay (1.4 0.2 vs. 1.9 0.1 days, p = 0.009), respectively, concluding that in large masses (> 6 cm), RA allowed one to shorten operative time providing less conversion rate compared to LA. Also, Nordenström et al. [31], in a series of 100 robotic-assisted laparoscopies, showed a conversion rate of 7%, but all converted cases were during the initial stage of the robotic approach. Although RA and LA showed similar operating times (p = 0.18), hospital stays were significantly lower for the RA group (W.M.D.: 0.52, p = 0.001). No significant differences in oncological efficacy (p = 0.81) and morbidity profile (p = 0.94) were reported, and the perioperative mortality rate was similar among the groups (p = 0.45). The above-mentioned pooled analysis showed the superiority of RA regarding conversion rate and hospital stay compared to LA. However, comparable results are provided for operating time, positive margin rate and postoperative morbidity and mortality.
In a recent study, Selvaraj et al. [32] analyzed peri- and post-operative data of 235 patients who underwent adrenalectomy (OA (n = 29), LA (n = 146) and RA (n = 60)) at three Institutions over a 7-year period. OA (n = 29) versus MIS (n = 206) showed significant differences in larger tumour size, cm (9.4 vs 5, (p = 0.0001)), longer operative time, mins (240 vs 100, (p = 0.0001)), longer hospital stay (8 vs 3 days,(p = .0001)), higher readmission rates (14% vs 1.9%), higher blood loss (400 vs 100 ml, (p = 0.0001)) requiring blood transfusion (14% vs 4.3%) (p = 0.03), higher intraoperative complication (21% vs 6%) (p = 0.0004) and post operative complications (17% vs 5.3%) (p = 0.01). Amongst the MIS (RA vs LA), RA appeared to have better outcomes in terms of shorter operative time, less blood loss and less intra operative complications with a p value <0.05. The postoperative complication rates were lowest with RA (3.3%) compared to OA (17%) and LA (6.1%).
Discussion
An appropriate surgical resection is a mandatory step in the therapeutic management of A.C.C.: a complete resection with negative margins and an intact adrenal capsule is necessary for curative intent [33]. Considering the fragility of A.C.C., surgeons must choose an appropriate approach that provides adequate exposure and access to the surrounding tissues and structures.
Although surgery remains the treatment of choice for A.C.C., the role of M.I.S. is still debated regarding oncological outcomes. In early 2000, the First International Adrenal Cancer Symposium defined open adrenalectomy (OA) as the gold standard for A.C.C. [34]. According to these recommendations, OA represents the treatment of choice to secure oncological principles, such as complete R0 “en bloc” resection and lymphadenectomy, as also confirmed by the last guidelines [35].
LA is today considered the gold standard treatment for benign adrenal tumours. Over the decades, there has been a radical change in the management of adrenal masses because minimally invasive adrenalectomy has been shown to decrease the length of hospital stay, reduce healthcare costs, reduce wound complications and blood loss and improve the patient’s outcome with earlier patient mobility and faster return to regular activity [30]. The basic principle of LA is to perform gentle and elegant dissection of the surrounding tissues away from the adrenal mass, avoiding tumour rupture or excessive manipulation. Even so, the main concern in LA is the risk of capsule rupture and intraperitoneal tumour spread. Current guidelines from ESMO-EURACAN [35] suggest performing LA in patients with unilateral adrenal masses with radiological findings suspicious of malignancy and a diameter ≤ 6 cm but with no evidence of local invasion (ENSAT stage I/II). Due to the lack of literature concerning the approach for ENSAT stage III, OA remains recommended for unilateral adrenal masses with radiological findings suspicious of malignancy, including signs of local invasion [31].
Furthermore, there is no consensus on the role of LAfor tumours > 6 cm and local invasion. The size is an essential variable in predicting malignancy, if the lesions are smaller than 4 cm, the risk of malignancy is approximately 2%, while for lesions of 4–6 cm, the risk of malignancy is 6%, and for lesions of 6 cm, the risk of malignancy is 25% (10–53%) [3]. No evidence suggests that a laparoscopic approach is contraindicated for G.A.T. because the size is only a predictor factor of malignancy [4]. In a recent metanalysis, Hue et al. [36] demonstrate that minimally invasive resections are being performed for tumours of all sizes. The authors performed an analysis stratified by tumour size and highlighted several important points. First, increasing tumour size and right-sided tumours were associated with an increased likelihood of conversion from M.I.S. to OA. Second, operations that required conversion to open and tumours with evidence of local invasion were associated with an increased likelihood of a positive surgical margin, however, tumour size was not an independent predictor of margin status. Third, positive margins, local invasion and operations that required conversion to open were all associated with poor survival, however, tumour size was not an independent predictor of survival. These collective data suggest that evidence of local invasion and operative technique play a significant role in treating patients with A.C.C. However, tumour size by itself may not be the most critical metric. This analysis adds granularity to the existing literature regarding the most important factors when determining the operative approach. M.I.S. may be cautiously considered in tumours with a relatively low risk of conversion (small size left-sided) and with no evidence of local invasion preoperatively. Otherwise, OA should remain the standard of care.
It is mandatory to consider the surgeon’s experience and hospital volume. The last guidelines stated that adrenal cancer surgery should be performed only in centres performing at least six adrenalectomies per year (but with a preference for > 20 surgeries per year) [35] and by surgeons with expertise in both open and laparoscopic surgery [19].
In their meta-analysis, Autorino et al. [21] have not found differences in most relevant oncological outcomes between LA and OA, namely the overall recurrence rate (p = 0.53), time to recurrence (p = 0.11) and cancer-specific mortality (p = 0.08). However, there was a higher risk of development of peritoneal carcinomatosis at the time of recurrence for LA (RR 2.39, CI 1.41, 4.04, p = 0.001). This finding is in line with the study by Leboulleux et al. [37], who found the surgical approach to be related to the risk of peritoneal carcinomatosis observed in 5 of the 6 patients (83%) who underwent laparoscopic resection of A.C.C. in their series. Considering that patients with A.C.C. recurrence seem to have higher survival rates if amenable to complete surgical resection and the presence of peritoneal recurrence is likely to compromise a salvage surgery, these findings support the concept that a complete oncological resection, possibly involving adjacent organs and avoiding the rupture of the adrenal capsule, remains the key factor and it should not be compromised by the implementation of M.I.S.
Beyond the surgical approach, resection should be extended, in the case of extra-adrenal invasion, to include en bloc resection of macroscopically invaded surrounding organs [25]. In the early 1990s, Icard et al. [38] advocated for en bloc removal of the ipsilateral kidney, including peri-hilar lymph nodes and other adjacent structures, to obtain wide operative margins with a low risk of surgical tumour infringement. Thirteen patients (32%) underwent extensive resections over 12 years, including one partial pancreatectomy, four nephrectomies, three right hepatectomies and three bowel resections, all for apparent invasion. Additionally, 11 patients underwent en-bloc nephrectomy without evident tumour invasion. No improvement in the outcome was observed. However, the authors argued that an “en bloc resection” allowed R0 surgery. Kidney involvement is rare, and there is no evidence that nephrectomy may positively influence the oncologic outcome. It is suggested to remove an adjacent organ case-by-case basis, considering preoperative imaging and overall inspection during surgery.
There is no consensus on the role of lymph-node dissection (L.N.D.) in adrenal tumours. The adrenal gland has two main lymphatic drain flows: the first to the inferior vena cava and right/left edge of the aorta and the second one to the lomboaortic nodes and interaorticocaval space. Adrenal lymphatic drainage patterns are complex, so the extent of lymphadenectomy in A.C.C. resection remains unclear [27]. Last ESMO-EURACAN guidelines [35] advise that locoregional lymphadenectomy improved tumour staging leading to a better oncological outcome. Moreover, the E.S.E. guidelines suggest performing a locoregional lymphadenectomy in highly suspected or proven A.C.C cases. In the studies regarding L.N.D. in A.C.C., the German A.C.C. Registry analyzed 283 patients: 47 cases underwent adrenalectomy with L.N.D., and 236 patients underwent adrenalectomy with no L.N.D. [39]. Multivariate analysis indicated a reduced risk of tumour recurrence (hazard ratio [H.R.] 50.65, P5.42) and disease-related death (HR 50.54, P5.049) for the L.N.D. group 2. In a recent study, Deschner et al. demonstrated that L.N.D. is not associated with an increased survival rate [40]. Lymph node metastasis is associated with advanced tumours (p = 0.4). Median overall survival was incrementally worse with an increasing number of positive lymph nodes (88.2 months for N0, 34.9 months for 1–3 positive nodes and 15.6 months for ≥ 4 positive nodes, p < 0.001). The optimal extent of lymphadenectomy in A.C.C. is still not known.
In the absence of clear-cut evidence of any benefits in the oncologic outcome, extended resection should be performed in selected cases when lymph node involvement is detected on preoperative imaging or intraoperatively. It remains controversial as an essential part of the surgical management for A.C.C. and deserves further investigation in a more extensive, prospective study. However, regional L.N.D. should still be considered for staging and prognostic purposes and to standardize surgical care [41, 42].
Therefore, from all the studies that we have cited, M.I.S. approaches might have a comparable oncologic outcome compared with OA for patients with localized (ENSAT I–II) or resectable A.C.C. (ENSAT I–III) if the principle of surgical oncology was respected. However, most studies were retrospective and involved a small number of patients. Hence, bias may exist. As a result, surgeons should carefully evaluate the condition of the patients and choose the surgical approach conducted in an oncologically appropriate manner to minimize the risk of recurrence and improve survival. Furthermore, more well-conducted studies with a large sample size are required to verify our findings.
The limitations of this study and the difficulty in concluding the evaluated studies are due to multiple confounding factors. First, all the studies analyzed were retrospective. They included a few cases due to the overall rarity of A.C.C. with inherent bias, which may affect our results and partially explain the heterogeneity among studies. Additionally, several factors may impact the results, such as adjuvant therapies, surgical volume, duration of follow-up and others. Over the years, radiological imaging techniques have improved and changed as well as surgical approaches with an increase in minimally invasive surgery, which may affect patient outcomes. L.N.D. and complete resection confer better oncologic outcomes, but they are not standardized and depend on the presentation stage and surgeons’ expertise.
On the other hand, many patients included in the previous studies were operated at low-volume centres. Furthermore, it would have been helpful to compare surgical management by grouping tumours by size, hormonal profile or other clinical characteristics. However, these data are poorly available and inhomogeneous among the studies. Lastly, to our knowledge, no studies about RA performed for only A.C.C. have been published yet. Thus, clear indications and unambiguous management of A.C.C. patients are still lacking. Further investigations, with patient randomization according to staging and surgical treatment, are needed.
Conclusion
A.C.C. is a highly malignant tumour of the adrenal cortex necessitating complete surgical excision with microscopically negative margins. The suspicions of A.C.C. for an adrenal lesion are driven by tumour size (> 6 cm), radiological signs of malignancy, presence of local invasion or distant metastases and typical hormonal secretions. Surgery is the treatment of choice for A.C.C. (Stage I–III), whereas, for stage IV, ACC surgery may be of more palliative intent. During the last years, surgical approaches have changed. Initially, OA has defined as the gold standard for confirmed or suspicious A.C.C. LA has gained more consensus for its indications and efficacy. LA appears to be equivalent to the open method for localized/locally advanced primary A.C.C. (ENSAT I–III) in terms of R0 resection rate, overall recurrence rate, time to recurrence and cancer-specific mortality, therefore, suggesting that the extent of surgery with adequate tumour resection is the predominant endpoint, rather than the surgical approach itself. Theoretically, robotic adrenalectomy has been shown to have several advantages compared to L.A., but there is still a lack of documentation of RA on malignant adrenal lesions. Thus, no direct conclusion about RA in A.C.C. can be inferred. The importance of R0 resection is emphasized by several studies, with en bloc removal of adjacent involved tissues or organs for locally advanced lesions. Current guidelines state that locoregional lymphadenectomy improves tumour staging and a better oncological outcome can be reached, while there is no consensus about the extent of lymphadenectomy. An appropriate surgical resection is a mandatory step in the therapeutic management of A.C.C. Although RA represents the future perspective, the role of minimally invasive surgery still needs further investigation. Multicenter randomized controlled trials with long follow-up periods exploring the long-term oncological outcomes are required to determine the benefits of the laparoscopic over the open approach in A.C.C.
References
Kostiainen I, Hakaste L, Kejo P, Parviainen H, Laine T, Löyttyniemi E, Pennanen M, Arola J, Haglund C, Heiskanen I et al (2019) Adrenocortical carcinoma: presentation and outcome of a contemporary patient series. Endocrine 65:166–174
Mihai R (2015) Diagnosis, treatment and outcome of adrenocortical cancer. Br J Surg 102:291–306
Ichijo T, Ueshiba H, Nawata H, Yanase T (2020) A nationwide survey of adrenal incidentalomas in Japan: the first report of clinical and epidemiological features. Endocr J 67:141–152
Giordano A, Alemanno G, Bergamini C, C, Valeri A, Prosperi P. (2021) Laparoscopic adrenalectomy for giant adrenal tumours: technical considerations and surgical outcome. J Minim Access Surg 17(1):76–80. https://doi.org/10.4103/jmas.JMAS_266_19
Ayala-Ramirez M, Jasim S, Feng L, Ejaz S, Deniz F, Busaidy N, Waguespack SG, Naing A, Sircar K, Wood CG et al (2013) Adrenocortical carcinoma: clinical outcomes and prognosis of 330 patients at a tertiary care center. Eur J Endocrinol 169:891–899
Scollo C, Russo M, Trovato MA et al (2016) Prognostic factors for adrenocortical carcinoma outcomes. Front Endocrinol 7:99
Huynh KT, Lee DY, Lau BJ, Flaherty DC, Lee J, Goldfarb M (2016) Impact of laparoscopic adrenalectomy on overall survival in patients with nonmetastatic adrenocortical carcinoma. J Am Coll Surg 223:485–492
Ball MW, Hemal AK, Allaf ME (2017) International consultation on urological diseases and european association of urology international consultation on minimally invasive surgery in urology: laparoscopic and robotic adrenalectomy. B.J.U Int. 119(1):13–21. https://doi.org/10.1111/bju.13592
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Machado NO, Al Qadhi H, Al Wahaibi K, Rizvi SG (2015) Laparoscopic adrenalectomy for large adrenocortical carcinoma. JSLS 19(3):e2015.00036. https://doi.org/10.4293/JSLS.2015.00036
Calcatera NA, Hsiung-Wang C, Suss NR, Winchester DJ, Moo-Young TA, Prinz RA (2018) Minimally invasive adrenalectomy for adrenocortical carcinoma: five-year trends and predictors of conversion. World J Surg 42(2):473–481. https://doi.org/10.1007/s00268-017-4290-2
Sgourakis G, Lanitis S, Kouloura A, Zaphiriadou P, Karkoulias K, Raptis D, Anagnostara A, Caraliotas C (2015) Laparoscopic versus open adrenalectomy for stage I/II adrenocortical carcinoma: meta-analysis of outcomes. J Invest Surg 28(3):145–152. https://doi.org/10.3109/08941939.2014.987886
Winoker JS, Ahlborn DT, Omidele OO, Fernandez-Ranvier G, Derweesh IH, Mehrazin R (2018) Minimally invasive adrenal surgery: virtue or vice? Future Oncol 14(3):267–276. https://doi.org/10.2217/fon-2017-0420
Hendricks A, Müller S, Fassnacht M, Germer CT, Wiegering VA, Wiegering A, Reibetanz J (2022) Impact of lymphadenectomy on the oncologic outcome of patients with adrenocortical carcinoma-a systematic review and meta-analysis. Cancers (Basel) 14(2):291. https://doi.org/10.3390/cancers14020291
Cavallaro G, Tarallo M, Chiappini A, Crocetti D, Polistena A, Petramala L, Sibio S, De Toma G, Fiori E, Letizia C (2021) Surgical management of adrenocortical carcinoma: current highlights. Biomedicines 9(8):909. https://doi.org/10.3390/biomedicines9080909
Buller DM, Hennessey AM, Ristau BT (2021) Open versus minimally invasive surgery for suspected adrenocortical carcinoma. Transl Androl Urol 10(5):2246–2263. https://doi.org/10.21037/tau.2020.01.11
Maurice MJ, Bream MJ, Kim SP, Abouassaly R (2017) Surgical quality of minimally invasive adrenalectomy for adrenocortical carcinoma: a contemporary analysis using the National Cancer Database. B.J.U Int 119(3):436–443. https://doi.org/10.1111/bju.13618
Kastelan D, Knezevic N, Zibar Tomsic K, Alduk AM, Kakarigi L, Kastelan M, Coric M, Skoric-Polovina T, Solak M, Kraljevic I, Balasko A, Gnjidic M, Dusek T (2020) Open vs laparoscopic adrenalectomy for localized adrenocortical carcinoma. Clin Endocrinol (Oxf) 93(4):404–408. https://doi.org/10.1111/cen.14251
Hue JJ, Bingmer K, Zhao H, Ammori JB, Wilhelm SM, Towe CW, Rothermel LD (2021) Reassessing the impact of tumor size on operative approach in adrenocortical carcinoma. J Surg Oncol 123(5):1238–1245. https://doi.org/10.1002/jso.26418
Mpaili E, Moris D, Tsilimigras DI, Oikonomou D, Pawlik TM, Schizas D, Papalampros A, Felekouras E, Dimitroulis D (2018) Laparoscopic versus open adrenalectomy for localized/locally advanced primary adrenocortical carcinoma (ENSAT I-III) in adults: is margin-free resection the key surgical factor that dictates outcome? A Review of the Literature. J Laparoendosc Adv Surg Tech A 28(4):408–414. https://doi.org/10.1089/lap.2017.0546
Autorino R, Bove P, De Sio M, Miano R, Micali S, Cindolo L, Greco F, Nicholas J, Fiori C, Bianchi G, Kim FJ, Porpiglia F (2016) Open versus laparoscopic adrenalectomy for adrenocortical carcinoma: a meta-analysis of surgical and oncological outcomes. Ann Surg Oncol 23(4):1195–1202. https://doi.org/10.1245/s10434-015-4900-x
Delozier OM, Stiles ZE, Deschner BW, Drake JA, Deneve JL, Glazer ES, Tsao MW, Yakoub D, Dickson PV (2021) Implications of conversion during attempted minimally invasive adrenalectomy for adrenocortical carcinoma. Ann Surg Oncol 28(1):492–501. https://doi.org/10.1245/s10434-020-08824-9
Gonzalez RJ, Shapiro S, Sarlis N, Vassilopoulou-Sellin R, Perrier ND, Evans DB, Lee JE (2005) Laparoscopic resection of adrenal cortical carcinoma: a cautionary note. Surgery 138(6):1078–1085. https://doi.org/10.1016/j.surg.2005.09.012
Zheng GY, Li HZ, Deng JH, Zhang XB, Wu XC (2018) Open adrenalectomy versus laparoscopic adrenalectomy for adrenocortical carcinoma: a retrospective comparative study on short-term oncologic prognosis. Onco Targets Ther 21(11):1625–1632. https://doi.org/10.2147/OTT.S157518
Wu K, Liu Z, Liang J, Tang Y, Zou Z, Zhou C, Zhang F, Lu Y (2018) Laparoscopic versus open adrenalectomy for localized (stage 1/2) adrenocortical carcinoma: experience at a single, high-volumecenter. Surgery. 164(6):1325–1329. https://doi.org/10.1016/j.surg.2018.07.026
Lee CW, Salem AI, Schneider DF, Leverson GE, Tran TB, Poultsides GA, Postlewait LM, Maithel SK, Wang TS, Hatzaras I, Shenoy R, Phay JE, Shirley L, Fields RC, Jin LX, Pawlik TM, Prescott JD, Sicklick JK, Gad S et al (2017) Minimally invasive resection of adrenocortical carcinoma: a multi-institutional study of 201 patients. J Gastrointest Surg 21(2):352–362. https://doi.org/10.1007/s11605-016-3262-4
Mirallié E, Blanchard C, Caillard C, Rodien P, Briet C, Mucci S, Drui D, Hamy A (2019) Adrenocortical carcinoma: impact of surgical treatment. Ann Endocrinol 80:308–313
Ji C, Qun L, Chen W, Zhang F, Ji H, Zhang S, Zhao X, Li X, Zhang G, Guo H (2020) Retrospective comparison of three minimally invasive approaches for adrenal tumors: perioperative outcomes of transperitoneal laparoscopic, retroperitoneal laparoscopic and robot-assisted laparoscopic adrenalectomy. BMC Urol 20(1):66. https://doi.org/10.1186/s12894-020-00637-y
Sforza S, Minervini A, Tellini R, Ji C, Bergamini C, Giordano A, Lu Q, Chen W, Zhang F, Ji H, Di Maida F, Prosperi P, Masieri L, Carini M, Valeri A, Guo H (2020) Perioperative outcomes of robotic and laparoscopic adrenalectomy: a large international multicenter experience. Surg Endosc. https://doi.org/10.1007/s00464-020-07578-5
Agcaoglu O, Aliyev S, Karabulut K, Mitchell J, Siperstein A, Berber E (2012) Robotic versus laparoscopic resection of large adrenal tumors. Ann Surg Oncol 19(7):2288–2294. https://doi.org/10.1245/s10434-012-2296-4
Nordenström E, Westerdahl J, Hallgrimsson P, Bergenfelz A (2011) A prospective study of 100 roboticallyassisted laparoscopic adrenalectomies. J Robot Surg 5(2):127–131. https://doi.org/10.1007/s11701-011-0243-1
Selvaraj N, Pooleri GK, Addla SK, Raghavan D, Govindaswamy TG, Balakrishnan AK, Sivaraman A, Jain N, Kandasamy SG, Ragavan N (2022) Robot assisted laparoscopic adrenalectomy: should this be the new standard? Urologia 89(3):430–436. https://doi.org/10.1177/03915603221097166
Mir MC, Klink JC, Guillotreau J, Long JA, Miocinovic R, Kaouk JH, Simmons MN, Klein E, Krishnamurthi V, Campbell SC, Fergany AF, Reynolds J, Stephenson AJ, Haber GP (2013) Comparative outcomes of laparoscopic and open adrenalectomy for adrenocortical carcinoma: single, high-volume center experience. Ann Surg Oncol 20(5):1456–1461. https://doi.org/10.1245/s10434-012-2760-1
Schteingart DE, Doherty G, Gauger PG, Giordano T, Hammer GD, Korobkin M, Worden FP (2005) Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr Relat Cancer 12:667–680
Fassnacht M, Assie G, Baudin E, Eisenhofer G, de la Fouchardiere C, Haak HR, de Krijger R, Porpiglia F, Terzolo M, Berruti A (2020) Adrenocortical carcinomas and malignant phaeochromocytomas: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 31:1476–1490
Hu X, Yang WX, Shao YX, Dou WC, Xiong SC, Li X (2020) Minimally invasive versus open adrenalectomy in patients with adrenocortical carcinoma: a meta-analysis. Ann Surg Oncol 27(10):3858–3869. https://doi.org/10.1245/s10434-020-08454-1
Leboulleux S, Deandreis D, Al Ghuzlan A, Aupérin A, Goéré D, Dromain C, Elias D, Caillou B, Travagli JP, De Baere T, Lumbroso J, Young J, Schlumberger M, Baudin E (2010) Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur J Endocrinol 162(6):1147–1153. https://doi.org/10.1530/EJE-09-1096
Icard P, Louvel A, Chapuis Y (1992) Survival rates and prognostic factors in adrenocortical carcinoma. World J Surg 16:753–758
Brix D, Allolio B, Fenske W, Agha A, Dralle H, Jurowich C, Langer P, Mussack T, Nies C, Riedmiller H, Spahn M, Weismann D, Hahner S, Fassnacht M, German Adrenocortical Carcinoma Registry Group (2010) Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur Urol 58(4):609–615. https://doi.org/10.1016/j.eururo.2010.06.024
Deschner BW, Do ZES, DeLozier OM, Drake JA, Tsao M, Glazer ES, Do JLD, Yakoub D (2020) Dickson PV (2020) Critical analysis of lymph node examination in patients undergoing curative-intent resection for adrenocortical carcinoma. J Surg Oncol 122(6):1152–1162. https://doi.org/10.1002/jso.26138
Saade N, Sadler C, Goldfarb M (2015) Impact of regional lymph node dissection on disease specific survival in adrenal cortical carcinoma. Horm Metab Res 47(11):820–825. https://doi.org/10.1055/s-0035-1549877
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. B.M.J. (Clinical Research Ed.) 372:n71. https://doi.org/10.1136/bmj.n71
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work. Alessio Giordano and Carlo Bergamini collected all the records and supervised the drafting of the article.
Corresponding author
Ethics declarations
Authors state that the work described has not been published previously, that it is not under consideration for publication elsewhere and that all authors approve its publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Authors state that the work described has not been published previously, that it is not under consideration for publication elsewhere and that all authors approve its publication.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giordano, A., Feroci, F., Podda, M. et al. Minimally invasive versus open adrenalectomy for adrenocortical carcinoma: the keys surgical factors influencing the outcomes—a collective overview. Langenbecks Arch Surg 408, 256 (2023). https://doi.org/10.1007/s00423-023-02997-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02997-z