Abstract
Purpose
The significant advantages of robotic surgery have expanded the scope of surgical procedures that can be performed through minimally invasive techniques. The aim of this study was to compare the perioperative outcomes between robotic and laparoscopic liver surgeries at a single center.
Methods
From July 2007 to October 2011, a total of 206 patients underwent laparoscopic or robotic liver surgery at the Asan Medical Center, Seoul, Korea. We compared the surgical outcomes between robotic liver surgery and laparoscopic liver surgery during the same period. Only patients who underwent left hemihepatectomy or left lateral sectionectomy were included in this study.
Results
The robotic group consisted of 13 patients who underwent robotic liver resection including 10 left lateral sectionectomies and three left hemihepatectomies. The laparoscopic group consisted of 17 patients who underwent laparoscopic liver resection during the same period including six left lateral sectionectomies and 11 left hemihepatectomies. The groups were similar with regard to age, gender, tumor type, and tumor size. There were no significant differences in perioperative outcome such as operative time, intraoperative blood loss, postoperative liver function tests, complication rate, and hospital stay between robotic liver resection and laparoscopic liver resection. However, the medical cost was higher in the robotic group.
Conclusions
Robotic liver resection is a safe and feasible option for liver resection in experienced hands. The authors suggest that since the robotic surgical system provides sophisticated advantages, the retrenchment of medical cost for the robotic system in addition to refining its liver transection tool may substantially increase its application in clinical practice in the near future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery of the liver has progressed tremendously because of a clearer understanding of its functional anatomy, enhanced knowledge of its regenerative capability, and its functional reserve [1]. Improved techniques to achieve vascular control and technological advancements have facilitated parenchymal transection, resulting in decreased mortality and morbidity due to liver surgery [1]. All the available knowledge and technology has been used to extend the scope of liver surgery to incorporate minimally invasive techniques (laparoscopic and robotic) to practically all types of hepatic resections [1, 2]. Over the past decade, although laparoscopic liver resection has been revealed to be feasible, due to the two-dimensional view and awkward laparoscopic instrumentation, there are still some limitations in terms of obtaining adequate visualization and meticulous manipulation of the tissues [3, 4]. Since the development of robotic surgical technology, these limitations are progressively being overcome [5]. The advantages of robotic surgery have expanded the scope of surgical procedures performed through minimally invasive techniques [1, 6]. However, to date, there have been only few studies, comparing the outcomes between robotic and laparoscopic liver surgeries. The aim of this preliminary study was to compare the perioperative outcomes between robotic and laparoscopic liver surgeries at a single center. In addition, the medical cost involved in both the techniques was also compared to determine the feasibility of robotic liver surgery for routine use in clinical practice.
Methods
From July 2007 to October 2011, a total of 206 patients underwent laparoscopic or robotic liver surgery at the Asan Medical Center, Seoul, Korea. Since robotic liver surgery was first performed in May 2010, the authors compared the surgical outcomes between robotic liver surgery and laparoscopic liver surgery during the same period. All robotic cases were performed in parallel with the laparoscopic resections. Because there were few patients who underwent robotic liver wedge resection and because robotic right hepatectomy has not been performed yet, to provide a more accurate analysis, only patients who underwent left hepatectomy or left lateral sectionectomy were included in this study. All the procedures were performed consecutively by a single surgeon. The selection of either approach depended on patient’s preference and the availability of equipments and familiarity of the surgeon with the robotic procedure. Furthermore, patient demographics, preoperative and postoperative liver function tests, tumor type and size, operative time, estimated blood loss (EBL), resection margin, complications, length of hospital stay, and medical cost were also documented. Data were collected into an institution review board-approved database. Specifically, data regarding postoperative complications were obtained and graded according to the Clavien-Dindo classification [7]. Operative time was defined as the time from skin incision to wound closure. Statistical analyses were performed using the Mann-Whitney U test for non-parametric ordinal variables and Χ 2 test for categorical variables. SPSS version 12.0 (SPSS Inc., Chicago, IL) was used for all the statistical analyses. A p value less than 0.05 was considered statistically significant.
Surgical procedure
Laparoscopic liver surgery
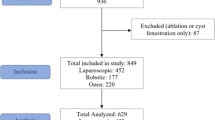
The patient was placed supine in the 30° reversed Trendelenburg position, with the surgeon standing between the patient’s legs. The authors inserted five trocars, and the middle trocar was used as a main working port as shown in Fig. 1a. A carbon dioxide pneumoperitoneum was established through a 10-mm umbilical port and was maintained at less than 12 mmHg to reduce the potential risk of air embolism. The authors employed a 30° laparoscope to inspect the liver surface, the porta hepatis surface, and the peritoneal surface. In patients with liver tumors, laparoscopic ultrasonography was used for precise tumor localization and to identify satellite nodules of hepatocellular carcinoma (HCC) and to demarcate an adequate liver resection margin. Vascular inflow was selectively controlled and the Pringle maneuver was not used. Although the superficial hepatic parenchyma was transected using a harmonic scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH), the parenchyma was mainly transected using a laparoscopic cavitron ultrasonic surgical aspirator (CUSA; Valleylab, Inc., Boulder, CO). During transection of the parenchyma, small Glissonian pedicles and hepatic vein branches were ligated using Hem-o-lok clips (Weck Closure System, Research Triangle Park, NC, USA) or titanium clips and were transected. During left lobectomy, the left hepatic artery and portal vein were individually dissected and ligated and the left hepatic vein was transected using an Endo-GIA stapler (Covidien, Mansfield, MA, USA). The resected specimen was inserted into a protective endobag and retrieved by making an additional suprapubic transverse incision. After specimen extraction, the suprapubic wound was closed and the abdominal cavity was reinsufflated with CO2 gas to examine for bleeding and bile leakage; furthermore, hemostasis and biliostasis were performed on the cut surface of the liver. Fibrin glue sealant (Greenplast, Green Cross Corp., Seoul, Korea) was sprayed over the resection surface to prevent bile leakage and postoperative bleeding. Two closed-suction drains were inserted to prevent fluid collection around the resection site.
Trocar positions for laparoscopic and robotic liver resections. a Laparoscopic liver resection. The solid arrow indicates the main working port of the surgical aspirator (cavitron ultrasonic surgical aspirator) and the dotted arrow represents the graft retrieval site. b Robotic liver resection. The solid arrow indicates the direction of the surgical cart and the dotted arrow represents the graft retrieval site
Robotic liver surgery
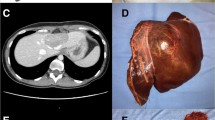
The patient was placed supine in the 15° reverse Trendelenburg position, with an assistant standing between the patient’s legs. A 12-mm trocar for the robotic camera was placed on either right or left side of the patient’s umbilicus depending on the procedure (left lateral sectionectomy vs. left hepatectomy). Carbon dioxide was insufflated, and pneumoperitoneum was maintained at 12 mmHg. Three 8-mm trocars were placed in the right subcostal, paramedian, and left subcostal areas. A 12-mm trocar for an assistant was placed in the right lower quadrant area. The surgical cart of the 4-arm da Vinci surgical system was placed and docked coming from the patient’s head towards the camera port, and the trocar for the robotic harmonic scalpel was placed along the target lesion (Fig. 1b). The surgeon moved towards the surgeon’s cart to control the robotic arms. The assistant stood between the patient’s legs to change the robotic instruments and perform clipping, stapling, suction, irrigation, and retraction through a 12-mm trocar placed at the right lower quadrant. The right subcostal port was used for liver retraction with the robotic arm. The left triangular and falciform ligaments were divided with the permanent cautery hook for mobilization of the left liver. Using a Maryland bipolar forceps, the left hepatic artery and portal vein were dissected and identified. These vessels were divided using metal or Hem-o-lok clips (Weck Closure System, Research Triangle Park, NC, USA) or ligated with the robotic needle holder (Fig. 2a, b). The parenchymal division was carried out along the demarcation line using the robotic harmonic scalpel (Fig. 2c). The larger Glissonian pedicles were ligated, clipped, and divided. The Pringle maneuver was not used during parenchymal division. The left hepatic duct and left hepatic vein were exposed after complete division of the remnant hepatic parenchyma and were divided using an Endo-GIA stapler (Covidien, Mansfield, MA, USA) (Fig. 2d). The specimen was placed in an endobag inserted through a 12-mm trocar and retrieved through a 10-cm suprapubic incision site. A closed suction drain was inserted to prevent fluid collection, and fibrin glue was applied to the resection site after hemostasis and biliostasis have been achieved.
Results
From May 2010 to June 2011, 13 patients underwent robotic liver resection including 10 left lateral sectionectomies and three left hepatectomies. These patients comprised the robotic group. The laparoscopic group consisted of 17 patients, who underwent laparoscopic liver resection during the same period including 11 left hepatectomies and six left lateral sectionectomies. The groups were similar with regard to age, gender, tumor type, and tumor size (Table 1). The performed procedures were similar in both the groups with the exception of the robotic group performing liver parenchymal transection using the harmonic scalpel due to the unavailability of the CUSA for robotic surgery. In addition, there were no significant differences in mean operative time (Robot vs. Lap; 291.5 ± 85.1 vs. 240.9 ± 68.6 min, p = 0.082) and mean estimated blood loss (Robot vs. Lap; 388.5 ± 65.0 vs. 342.6 ± 84.7 ml, p = 0.114) between the two groups (Table 2). Of the 13 patients who underwent robotic liver resection, there was no difference in terms of mean operative time between the last five robotic operations and the first five robotic operations.
Although there were more HCC patients in the robotic group, there were no significant differences in terms of tumor size and surgical margin (Table 3). In both groups, there was no patient who required conversion to an open operation. There were two complications in the laparoscopic group; all of which were retrieval site wound seromas. There were no postoperative complications in the robotic group. However, there was no significant difference regarding complication rates between the two groups (p = 0.208). Also, no mortality was present in either group. Although there was a tendency for a longer hospital stay in the laparoscopic group (p = 0.053), the total medical cost was significantly higher in the robotic group (Robot vs. Lap; 11,475 ± 2,174 vs. 6,762 ± 1,436 USD, p = 0.001) (Table 4). Of the 13 patients who underwent robotic liver resection, there was no difference in terms of total medical cost between the last five robotic operations and the first five robotic operations.
Discussion
Laparoscopic techniques for liver resection are gaining increased popularity. With increasing experience, laparoscopic liver resection has resulted in comparable and, in some aspects, more improved outcomes when compared to the cases undergoing open surgery [2, 5]. Although there are many technical differences in the laparoscopic approach as reported in the literature, laparoscopic liver resection is reported to have lower morbidity, intraoperative blood loss, blood transfusion rate, need for postoperative analgesic drugs, and shorter hospital stay when compared to open liver resection [4, 8, 9]. The first consensus meeting on laparoscopic liver surgery held in Louisville, KY concluded that laparoscopic liver surgery is a safe and effective approach for the management of surgical liver disease if performed by surgeons with experience in hepatobiliary and laparoscopic surgery [10]. Currently, indications for laparoscopic liver resection are patients with solitary lesions, 5 cm or less, located in liver segments 2 to 6. The laparoscopic approach for left lateral sectionectomy should be considered as a standard practice [6].
Robotic surgery has received increased attention as a result of advancements in its technology. Although introduced in the late 1990s, robotic surgery has generated enthusiasm outside the specialties of urology, gynecology, and cardiac surgery. With technology refinement, improved image quality, and smaller robotic systems, there has been a recent interest in using the robot for complex laparoscopic procedures such as complex hepatopancreatobiliary cases, rectal surgery, and thyroidectomy [11].
The da Vinci Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA, USA), a robotic surgical system approved by the US Food and Drug Administration for surgery, is the only commercially available therapeutic robotic system in the market, which allows surgeons to perform advanced laparoscopic procedures with greater ease. Similar to a human hand, the robotic articulating instruments translate the natural movements of the surgeon’s hand into precise movements inside the abdominal cavity. The system allows three-dimensional views of the operative field, has tremor filtration capacity, and permits 7° of freedom. Such properties allow surgeons to dexterously perform delicate dissections and precise intracorporeal suturing, thus leading to its potential to mimic open liver resection [1, 5]. In our experience, when performing left hepatectomy in a patient with intrahepatic duct stones, suturing the left main hepatic duct after opening the duct for additional stone removal was easier and less time consuming in the robotic method than in the conventional laparoscopic method. The indications for robotic liver resection are similar to those for laparoscopic liver resection [1, 12].
However, robotic surgery has several limitations including high cost, inadequate coverage by medical insurance, lack of tactile, lack of training systems, time-consuming setup, and difficulty in converting to open surgery [11, 13–15]. Furthermore, the da Vinci system is not attached to the operating table, and thus requires undocking to change table position. When perilous circumstances such as massive bleeding occur, the assistant can compress bleeding focus with laparoscopic instruments until conversion to open surgery [11]. Also, a “team approach” is necessary when using the robotic system for minimally invasive liver surgery. In particular, it is essential that there be an experienced assistant surgeon on the patient’s bedside. The role of this assistant in suctioning and retracting the tissue for optimal exposure and for safe stapling is crucial [12].
Contrary to the enthusiasm for robotic liver resection, there have been few reports comparing robotic liver resection with the conventional laparoscopic approach. In a study by Berber et al. which compared nine robotic liver resections with 23 laparoscopic liver resections and only included segmental resections and left lateral sectionectomies for liver tumors, it concluded that for selected liver lesions, a robotic approach provides similar perioperative outcomes when compared with laparoscopic liver resection [5]. One patient was converted to an open operation due to parenchymal bleeding after liver resection [5]. The complication rate after robotic and laparoscopic liver resections was 11 and 17 %, respectively and there were no cases of mortalities [5]. In addition, the patients were followed up for a mean of 14 months and disease-free survival (DFS) was found to be equivalent in both the groups. Although a case-by-case cost analysis was not carried out, medical cost was also a matter of concern in their study [5]. Despite a larger number of major liver resections in our study including 14 left hepatectomies (11 in the laparoscopic group and three in the robotic), the results of our study were similar in that there were no differences in perioperative outcome between robotic liver resection and laparoscopic liver resection including operative time, estimated blood loss, and complication rate. However, the authors believe that the availability of CUSA arm for robotic surgery would have shortened the operative time and reduced the estimated blood loss. The conversion rate in the laparoscopic group was 0 % which is lower than the 5 to 15 % conversion rate, as reported in the literatures for laparoscopic liver resection [4, 16–18]. Also, the conversion rate in the robotic group was lower than the 5.7 % conversion rate reported in the literature [12]. Although our 11.7 % complication rate after laparoscopic liver resection was similar to the study conducted by Berber et al. [5], there were no complications after robotic liver resection. The medical cost was also significantly higher in the robotic group.
However, there are some limitations in the present study. The small sample size due to the preliminary nature of this study and heterogeneity within the study groups (non-tumor lesions were also included) must be taken into account when interpreting the results. In addition, comparison of only left hepatectomies and left lateral sectionectomies might have resulted in the low complication rate in both the groups and low conversion rate in the robotic group so that the results of this study may not apply to other forms of liver resection including segmental resections or right hepatectomies. Also, the small sample size or less experience may have influenced the result that there was no difference in terms of mean operative time and total medical cost between the last five robotic operations and the first five robotic operations.
Although laparoscopic liver resection has demonstrated its safety in resections for malignancy, only a limited number of robotic liver surgeries have been reported in the literature and only preliminary experience exists for robotic liver resection [8–10, 19]. Since the first robotic liver resection at our center was performed in May 2010, the follow-up period in our study was relatively short and comparison of recurrence or survival with the laparoscopic method was not possible. Furthermore, this study was limited due to its non-randomized design. The authors believe that future prospective randomized studies with larger numbers of patients, more diverse liver resections, and longer follow-up are warranted to precisely compare robotic liver resection and laparoscopic liver resection.
Conclusion
Robotic liver resection is a safe and feasible option for liver resection in experienced hands. Although the medical cost was higher in the robotic group, there were no significant differences regarding perioperative outcome between robotic liver resection and laparoscopic liver resection. The authors further suggest that since the robotic surgical system provides sophisticated advantages such as three-dimensional image and a 360° rotating endowrist comfortable for suture enabling robotic surgery to further expand the application of the minimally invasive approach to liver surgery, the retrenchment of medical cost for the robotic system in addition to refining its liver transection tool by incorporating a CUSA arm may substantially increase its application in clinical practice in the near future.
References
Idrees K, Bartlett DL (2010) Robotic liver surgery. Surg Clin North Am 90(4):761–774
Kim KH, Jung DH, Park KM, Lee YJ, Kim DY, Kim KM, Lee SG (2011) Comparison of open and laparoscopic live donor left lateral sectionectomy. Br J Surg 98(9):1302–1308. doi:10.1002/bjs.7601
Pilgrim CH, To H, Usatoff V, Evans PM (2009) Laparoscopic hepatectomy is a safe procedure for cancer patients. HPB (Oxford) 11(3):247–251. doi:10.1111/j.1477-2574.2009.00045.x
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery 141(2):203–211
Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J (2010) Robotic versus laparoscopic resection of liver tumours. HPB (Oxford) 12(8):583–586. doi:10.1111/j.1477-2574.2010.00234.x
Lai EC, Tang CN, Li MK (2012) Robot-assisted laparoscopic hemi-hepatectomy: technique and surgical outcomes. Int J Surg 10(1):11–15
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Walsh MR, Vogt D, Fung J, Berber E (2009) Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc 23(4):847–853. doi:10.1007/s00464-008-0262-9
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246(3):385–392. doi:10.1097/SLA.0b013e318146996c
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 250(5):825–830
Choi SB, Park JS, Kim JK, Hyung WJ, Kim KS, Yoon DS, Lee WJ, Kim BR (2008) Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J 49(4):632–638
Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E (2011) Robotic liver surgery: results for 70 resections. Surgery 149(1):29–39. doi:10.1016/j.surg.2010.04.002
Vidovszky TJ, Smith W, Ghosh J, Ali MR (2006) Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res 136(2):172–178. doi:10.1016/j.jss.2006.03.021
Hashizume M, Tsugawa K (2004) Robotic surgery and cancer: the present state, problems and future vision. Jpn J Clin Oncol 34(5):227–237
Nguyen MM, Das S (2004) The evolution of robotic urologic surgery. Urol Clin North Am 31(4):653–658. doi:10.1016/j.ucl.2004.06.002, vii
Dagher I, Proske JM, Carloni A, Richa H, Tranchart H, Franco D (2007) Laparoscopic liver resection: results for 70 patients. Surg Endosc 21(4):619–624. doi:10.1007/s00464-006-9137-0
Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B (2006) Laparoscopic liver resection. Br J Surg 93(1):67–72. doi:10.1002/bjs.5150
Bryant R, Laurent A, Tayar C, Cherqui D (2009) Laparoscopic liver resection-understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg 250(1):103–111. doi:10.1097/SLA.0b013e3181ad6660
Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, Brock G, McMasters KM (2008) Experience with more than 500 minimally invasive hepatic procedures. Ann Surg 248(3):475–486. doi:10.1097/SLA.0b013e318185e
Conflicts of interest
All authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, YD., Kim, KH., Jung, DH. et al. Robotic versus laparoscopic liver resection: a comparative study from a single center. Langenbecks Arch Surg 399, 1039–1045 (2014). https://doi.org/10.1007/s00423-014-1238-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1238-y