Abstract
Purpose
Research describes the existence of a relationship between cortical activity and the regulation of bulbar respiratory centers through the evaluation of the electroencephalographic (EEG) signal during respiratory challenges. For example, we found evidences of a reduction in the frequency of the EEG (alpha band) in both divers and non-divers during apnea tests. For instance, this reduction was more prominent in divers due to the greater physiological disturbance resulting from longer apnea time. However, little is known about EEG adaptations during tests of maximal apnea, a test that voluntarily stops breathing and induces dyspnea.
Results
Through this mini-review, we verified that a protocol of successive apneas triggers a significant increase in the maximum apnea time and we hypothesized that successive maximal apnea test could be a powerful model for the study of cortical activity during respiratory distress.
Conclusion
Dyspnea is a multifactorial symptom and we believe that performing a successive maximal apnea protocol is possible to understand some factors that determine the sensation of dyspnea through the EEG signal, especially in people not trained in apnea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The electroencephalographic signal (EEG) is a parameter obtained through the assessment of cortical brain activity (Muller-Putz 2020) which consists of brain electrical impulses, enabling its classification according to amplitude, frequency, and wave latency (Lee et al. 2015; Dimitriadis et al. 2018). Research has described the existence of a close relationship between cortex activity and the regulation of respiratory centers (Thayer and Lane 2009), and the possibility of evaluating the relationship between respiratory and cortical function through electroencephalography (Macefield and Gandevia 1991; Tort et al. 2018). Such interaction originates from the central autonomic network, an interconnected self-regulation system responsible for controlling behavioral, neurochemical, and visceromotor responses (Benarroch 1993), whose structures include the insular cortex, amygdaloid nucleus, hypothalamus, and solitary tract nucleus (NTS) in the medulla that connects with the spinal cord and afferent (sensory) and efferent (motor) neurons (Napadow et al. 2008).
Several assessment protocols have been used to detect changes in cortical activity through respiratory “challenges”, such as resistance inhalations and repeated voluntary nasal sniffs (Hudson et al. 2018). The voluntary apnea test is another example of a respiratory maneuver that consists of consciously suspending breathing (Elia et al. 2021). Its main performance parameters are the moment that the feeling of “air hunger” starts or more conveniently defined as the physiological breaking point (Agostoni 1963; Lin et al. 1974) and the maximum duration of the apnea. These outcomes may change under different conditions, for example: depending on the respiratory technique used before apnea, such as glosso-pharyngeal breathing (Lindholm and Nyrén 2005; Lemaître et al. 2010; Schipke et al. 2015), the level of partial or total lung insufflation at apnea start (Findley et al. 1983; Whitelaw et al. 1987; Flume et al. 1996; Andersson and Schagatay 1998), beta-1 adrenergic blockade (Hoiland et al. 2017), performing the technique in a dry environment or with one’s face submerged in water or during diving (Sterba and Lundgren 1988; Schagatay and Andersson 1998; Schagatay et al. 1999; Lemaître et al. 2007; Ratmanova et al. 2016; Elia et al. 2021), in individuals trained in apnea (Schagatay et al. 2000; Diniz et al. 2014), with different abilities to withstand the “urge to breathe” during apnea (Ferretti 2001; Menicucci et al. 2014), who experience psychological symptoms such as fear and anxiety (Rassovsky et al. 2006; Freire and Nardi 2012), with different intensities of dyspnea (Nishino 2011), or those who have pre-existing respiratory diseases (Nannini et al. 2007; Inoue et al. 2009; Viecili et al. 2011, 2012).
Based on evidence that successive apneas protocol increases the maximum apnea time (Heath and Irwin 1968; Bartlett 1977; Schagatay et al. 1999) and that the longer the maximum apnea time during breath-hold diving more significant are the reductions in the electroencephalographic signal (Steinberg et al. 2017), the hypothesis of this mini-review is that a successive apnea protocol is a promising model that can be used to take the electroencephalographic signal to lower frequencies and to understand the determinants of “air hunger” and dyspnea through comparison of the activity of the cerebral cortex between low and high physical fitness people or with comorbidities. This hypothesis study intends to suggest possibilities for future studies analyze mechanisms of dyspnea through the evaluation adaptations of the EEG signal during respiratory distress through of successive apneas protocol.
Connection between the cerebral cortex and the respiratory system
The central autonomic network is made up of billions of neurons that individually establish thousands of connections with different regions of the brain responsible for various vital functions. Among them is the NTS, a complex of nuclei capable of regulating various cognitive, neuroendocrine, and autonomic functions (Priovoulos et al. 2019). It is framed as a visceral sensorimotor nucleus located in the caudal and dorsomedial part of the medulla that receives, processes, and coordinates both respiratory and cardiovascular inputs through its connection with nerves and the spinal cord (Zoccal et al. 2014). It plays a key role in integrating and coupling the both respiratory and cardiovascular function through the neural network that it coordinates. This region of the central nervous system receives sensory informations via afferent pathways by means of the Glossopharyngeal and Vagus nerves, which comes from baroreceptor and chemoreceptors situated in the aortic and carotid bodies, which are responsible for capturing changes in O2 and CO2 pressure, in addition to systemic blood pressure (Guyenet et al. 2010). The Vagus nerve is also responsible for transmitting information from pulmonary and juxtacapillary stretch receptors that also influence respiratory control (Marek et al. 2008). Currently, several authors recognize the input of proprioceptive and chemical sensory information coming from the respiratory muscles (especially the diaphragm) through the phrenic nerve (Bordoni and Zanier 2013) and proprioceptive information coming from the joints and locomotor skeletal muscles (Parkes 2006). In addition to peripheral stimuli, the NTS is directly influenced by CO2 that move across the blood–brain barrier and stimulates the central H+ chemoreceptor and the respiratory centers of the bulb and triggers important respiratory responses (Nattie and Li 2012; Guyenet 2014). Sensory responses probably also reach higher cortical centers, influencing subjective respiratory sensation and voluntary respiratory command. Based on input from afferent (involuntary) and cortical (voluntary) information, the NTS is responsible for producing a respiratory motor response (central respiratory rhythm) that regulates the contraction of the respiratory muscles. Motor command starts at the bulbar inspiratory center and is prolonged when stimulated by the apneustic center or interrupted by the pneumotaxic center and reaches the respiratory muscles via the phrenic nerve.
The voluntary interruption of breathing triggers chemical processes that can result in the sensitization of peripheral CO2 (hypercapnia), O2 (hypoxemia), and central H+ (acidosis) chemoreceptors, and their afferent actions are essential for the homeostasis of blood gases and for stimulating ventilation and are considered crucial in determining the apnea breaking points (Lin 1982; Foster and Sheel 2005; Lindholm and Lundgren 2009; Guyenet et al. 2013; Fitz-Clarke 2018; Taboni et al. 2020). Non-chemical (mechanical) factors such as the degree of stretching of the lung parenchyma determined by the volume of air in the lungs and sensory feedback from the respiratory muscles, especially the diaphragm, also trigger ventilatory responses and the breaking point, namely involuntary interruption apnea (Parkes 2006; Nishino 2009). Agostoni's seminal study (1963) and subsequently other studies (Lin et al. 1974; Palada et al. 2008; Cross et al. 2013) confirmed the onset of diaphragmatic contractions to precede the volitional breaking point. Additionally, it was suggested that the onset of diaphragmatic contractions give origin to the final phase of the cardiovascular response to apnea, in which blood pressure increases and heart rate (HR) tends to decrease (Perini et al. 2008; 2010). Despite the importance of physiological factors (Ferretti et al. 1991; Delapille et al. 2001), the psychological factor is another parameter that can influence apnea performance. Although it is often overlooked, respiratory and cardiovascular signals that reach the brain are transmitted via the parabrachial subnuclei to different regions of the brain via the central autonomic network and converted into basic emotions related to respiratory distress and the urge to breathe. These sensations and feelings can limit apnea performance by participating in the control of breathing through the central autonomic network and supports the concept of a "wakefulness drive" that can have a profound impact on respiratory and cardiovascular control (Thornton et al. 2001; Martelli et al. 2013). In any case, from an integrative perspective, the time to the physiological breaking point should be directly proportional to the size of body oxygen stores (Fagoni et al. 2015; Taboni et al. 2018) and inversely proportional to the rate of body oxygen consumption (Sivieri et al. 2015), since the breath-hold duration was prolonged in hyperoxia (Klocke and Rahn 1959) and was shortened during hypoxia (Rahn et al. 1953). These adaptations are interpreted as an O2-conserving mechanism (Ferretti 2001).
Insufficient O2 can affect brain activity (Pearce 2018). It can result in cognitive deficits, such as attention deficit, mental confusion, memory loss, and syncope, and can cause psychomotor performance dysfunction such as hypomobility, weakness, loss of balance (Ando et al. 2020) and, in severe cases, seizures, coma, and brain death (Moral et al. 2019). Hypercapnia triggered by the ineffective pulmonary elimination of CO2 can lead to changes in brain activity, in addition to causing respiratory acidosis and functional impairments, such as a feeling of suffocation, dizziness, syncope, anxiety attacks, and headache (Romano et al. 2016). In such cases, electroencephalography has been employed to assess the severity of blood gas disturbances in patients hospitalized for acute respiratory failure (Papadelis et al. 2017). This is an example of clinical application of EEG assessment during respiratory disorders.
Respiratory maneuver and cortical responses assessed by EEG
Bulbar respiratory control is responsible for managing and coordinating respiratory functions through its direct connection with the spinal cord, cranial nerves, and its interaction with the central nervous system. However, due to its anatomical location within the brainstem, its electroencephalographic evaluation is not feasible. Thus, for a long time, the use of the EEG for the study of phenomena associated with breathing was redundant. However, research has demonstrated the possibility of evaluating respiratory function through electroencephalography by means of its connection with the cerebral cortex (Macefield and Gandevia 1991).
Several studies have transcribed reports of the capture of bioelectrical signals from electroencephalography during respiratory maneuvers. Macefield and Gandevia (1991) are pioneers in demonstrating that premotor potentials precede inspiration or expiration in rapid breaths or voluntary exhalations, that is, changes present in the EEG can be perceived through the activation of premotor potentials originating from simple tasks, such as speaking or conscious respiratory disturbances. During speech, we involuntarily perform an automatic control of breathing, as this occurs during the process of expiration and controlled inhibition of inspiration. Before speaking, unconscious pre-phonatory inspirations occur that precede the pronunciation, intonation, and rhythm of speech. In this act, breath control activities related to speech occur, modeling pre-phonatory breaths originating in the cortical premotor areas, which can be evidenced on the electroencephalogram (Tremoureux et al. 2014).
As with phonation, other respiratory maneuvers can also produce changes in electroencephalographic signals, in addition to being a viable way to reduce artifacts during EEG collection. The practice of breathing techniques, such as diaphragmatic breathing, promotes the reduction of physiological responses linked to stress (Ma et al. 2017). For example, when taking a deep, slow inspiration, there is a synchronization of brain oscillations in the limbic network through the olfactory cortex. Stress and anxiety, on the other hand, cause respiratory disorders that result in short and rapid inspirations, thus causing a low level of cellular oxygenation due to reduced movement of the diaphragm muscles (Menicucci et al. 2014). Nasal breathing is closely related to the limbic system which is the area of the brain responsible for regulating emotions. The activity of chemoreceptors in detecting aromas during inspiration triggers impulses to the brain region of the olfactory cortex, where these signals are processed and associated with our memories and emotions (Laurent et al. 2001; Martin and Ravel 2014). Evidence demonstrated that cortical activity increased during nasal inspiration and dissipated when breathing was diverted from nose to mouth (Zelano et al. 2016). In this sense, breathing does not seem to serve only to supply oxygen to the body; it can also organize neuronal population activity across brain regions to orchestrate complex behaviors (Kleinfeld et al. 2014). This suggests a pathway by which nasal breathing could even shape rhythmic electrical activity in downstream limbic areas, with corresponding effects on cognitive functions (Zelano et al. 2016).
Apnea is another type of respiratory maneuver that provides interesting physiological and behavioral challenges for study with EEG. During a maximal apnea test, sensory impulses are produced by chemical factors such as increased arterial CO2 (PaCO2) levels. Hypoxaemia (reduced PaO2) can also be seen in longer duration apnea tests. Factors of non-chemical (mechanical) origin are also observed from lung tissue stretching and proprioceptive receptors of the respiratory muscles, especially the diaphragm (Delapille et al. 2001). Based on empirical definition, apnea has two phases: the first is called the easy phase and is characterized by less respiratory need, followed by the struggle phase which is characterized by respiratory distress and increasing electromyographic activity of the diaphragm and PaCO2. Based on both respiratory and cardiovascular perspective, apnea can be divided into three phases: phase I, HR reduction and blood pressure increase; phase II, maintenance of HR and blood pressure values; phase III, progressive reduction in HR and arterial oxygen saturation and blood pressure increase until breaking point (Perini et al. 2008). Subjects with high maximal breath-holding time present all three phases; however, subjects with reduced performance present only phases I and II. While the duration of the easy phase seems to be influenced more by PaCO2, the duration of the struggle phase is influenced by sensory stimuli produced by the respiratory muscles that maintain a tonic contraction, which is almost isometric, and is necessary to voluntarily maintain apnea (Nishino et al. 1996). Individuals not trained in apnea and/or diving have reduced maximum apnea time and both easy and struggle phases, while trained individuals have higher values. It is likely that the struggle phase is related to the III phase, in this sense, while subjects with lower performance end the apnea at the beginning of the III phase, subjects with higher performance endure the III phase for longer. The “urge to breathe” (distress) or “air hunger” during the struggle phase requires emotional endurance, motivation, and cognitive control to withstand discomfort. Apnea is a voluntary control event, and as time passes, sensory afferent signals increase the involuntary breathing stimulation until the breaking point, when the involuntary control interrupts the voluntary apnea stimulus. The prefrontal cortex is an area responsible for, among other functions, cognitive control (Miller and Cohen 2001), the mechanism of action and inhibition of cognitive response (Ridderinkhof et al. 2004), decision-making, performance monitoring, and learning, and, it seems, the voluntary control of apnea (Steinberg et al. 2017).
In this context, Ratmanova et al. (2016) raised the hypothesis that brain tissue hypoxia caused by voluntary apnea out of water could generate changes in the EEG and consequently in brain performance and attention span, especially in breath-hold divers. Despite the chronic changes observed in the EEG before the apnea test (professional divers showed a reduction in the alpha frequency approaching the theta band and an atypical spatial pattern of alpha amplitude when compared to non-divers), a few changes were observed in the EEG and in performance during apnea. The Direct Current potential (DC potential) suffered a small reduction from apnea but was stable until the end of the test in both divers and non-divers, with no significant differences between the groups. The total EEG spectrum amplitude during apnea did not differ from the pre-apnea situation nor between the groups. Contrary to the authors' expectations, attention deficit after breath-holding was not verified; on the contrary, the attention tests showed an increase, but with no difference between the groups regardless of the maximum apnea time (3 min for non-divers and 4.5 min for professional divers). Although apnea causes changes in the blood pressures of CO2 and O2, the results of this study refuted the hypothesis that hypoxia induces reduced brain activity, due to acute adaptations of the diving reflex aimed at centralizing blood circulation and reducing peripheral aerobic metabolism.
In another study, oscillations and asymmetries in the amplitude of the alpha band were verified during an out-of-water apnea test when comparing professional divers with non-divers (Steinberg et al. 2017). Initially, the authors found an increase in alpha amplitude in professional divers in the first two minutes of apnea in the central and parietal regions of the brain and a reduction in the non-diver group. After 2 min, the group of professional divers showed a significant decrease in the amplitude of alpha waves until the end of the apnea (four minutes of duration). This reduction was greater than that seen in the group of non-professionals (apnea lasting 2 min). The increase in alpha amplitude in the initial minutes in the group of professional divers was attributed to the ventilatory maneuvers and concentration techniques performed before the apnea test, leading to the conclusion that these pre-apnea techniques possibly contributed to a delay in the drop in alpha amplitude. The physiological adaptations provided by a longer apnea time produced a significant reduction in the frequency of alpha waves when compared to the pre-apnea situation only in the group of professional divers. Professional divers also showed an alpha-lateralized pattern (greater frontal activity on the left than on the right), possibly related to the psychophysiological process triggered by apnea (air hunger, resistance, motivation, emotional regulation, and cognitive control). In general, the reduction in the frequency of alpha waves is related to the reduction in cognitive performance, as it is associated with information processing speed and memory (Klimesch 2009). The effect of apnea on the reduction of the EEG frequency (alpha waves) seems to be an adaptive response to a lower cognitive need and an increase in attention for the person who is performing a certain task during apnea (Sinha et al. 2020).
Later, the same group published a study with the objective of verifying whether cognitive and psychological responses could be affected by the reduction in the frequency of the alpha band during out-of-water apnea. The performance of trained apnea divers was assessed using chess and visual activities during a pre-determined 4 min apnea period (Steinberg and Doppelmayr 2019). No significant changes were found in the responses of neurocognitive markers VEP and P300. The authors concluded that the short air retention time previously determined in 4 min was not sufficient to produce a reduction in brain activity. Despite the significant reduction in the alpha band frequency seen earlier during a 4 min apnea test (Steinberg et al. 2017), this study failed to find changes in cognitive and psychological performance for the same period. These results were similar to the study carried out by Ratmanova et al. (2016), and according to the authors, a longer apnea time may be necessary to produce greater hypoxaemia and detect such changes.
Elite apnea divers can hold their breath for up to 11 min and thus produce hypoxaemia (Arce-Álvarez et al. 2021; Elia et al. 2021). The afferent stimuli triggered by hypercapnia and by proprioceptors of the respiratory muscles and lung tissue are delayed in these divers due to the adaptations provided by apnea training, allowing for longer duration apnea and, consequently, greater hypoxaemia. These divers have greater lung oxygen stores due to higher total lung capacity that non-diving individuals (Lindholm and Nyren 2005; Loring et al. 2007; Walterspacher et al. 2011; Ferretti et al. 2012; Patrician et al. 2021). Blood oxygen stores are dictated by blood hemoglobin concentration. This can increase only in case of red blood cell delivery into blood by spleen contraction. Some authors have suggested this possibility (Schagatay et al. 2001; Espersen et al. 2002; Baković et al. 2003). These adaptations ascribed to the mammalian diving reflex, e.g., sympathetically mediated peripheral vasoconstriction and vagally mediated bradycardia, are necessary for oxygen conservation to maintain cerebral functioning (Bain et al. 2018; Ferretti 2001; Elia et al. 2021). In defense of maintaining global cerebral oxygen delivery during prolonged breath holds, the cerebral blood flow may increase by ∼100% from resting values (Elia et al. 2021). Furthermore, these divers also have greater emotional tolerance toward the desire to breathe and to resist the feeling of shortness of breath. Adaptations such as these affect NTS activity, which in turn is connected with the prefrontal cortex and limbic system through the central autonomic network. For this reason, exposure to acute levels of stress, such as during apnea, triggers emotions and feelings, which can also alter cognitive abilities. Constant exposure to these stimuli is likely to provide chronic psychophysiological adaptations such as those observed in elite divers (Diniz et al. 2014). In addition, performing pre-apnea breathing techniques that induce well-being and relaxation (Perciavalle et al. 2017) and reduce anxiety (Malathi and Damodaran 1999) and stress (Berger and Owen 1988; Netz and Lidor 2017) also contribute to greater performance and greater resistance to psychophysiological stress during apnea in elite divers (Steinberg et al. 2017). Thus, greater support for apnea is made possible by both previous physiological adaptations and pre-apnea preparation, such as a successive apnea protocol, which triggers greater physiological and psychological changes that can be observed through changes in cortical activity (Perciavalle et al. 2017).
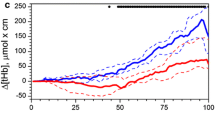
Individuals not trained in apnea have very limited performance in this activity. The literature recognizes that performing successive apneas in the same session provides acute breaking point delay and a significant increase in maximum apnea time (Heath and Irwin 1968; Bartlett 1977; Schagatay et al. 1999), as well as in the struggle duration phase (Nishino et al. 1996). As the duration of the struggle phase is mainly influenced by the proprioceptive activity of the respiratory muscles, its prolongation seems to be related to some type of habituation or reduced sensitivity of this proprioceptive stimulus or of the hypercapnic or hypoxic ventilatory response, caused by the increase in endogenous opioids in the central nervous system, or decreased anxiety, or some other mechanism (Nishino et al. 1996). In any case, the cause of the increase in maximal breath-holding time in successive apnea protocols is unknown and may contribute to understanding the mechanisms of “air hunger” or other types of respiratory distress such as dyspnea (Nishino 2009, 2011). Therefore, we hypothesized that the protocol-induced increase in performance of successive apneas could significantly reduce the amplitude of the beta and alpha bands especially in individuals not trained in apnea or with respiratory distress (Fig. 1). In addition, a protocol of successive apneas seems to be promising for understanding the neural mechanisms of respiratory distress and dyspnea.
Diagram representing the hypothesis of this study where the successive apnea protocol is seen on the left, with an increase in the performance in the apnea time (seconds) and the consequent reduction in the frequency in the EEG signal (right). In patients with respiratory distress, performance and adaptations in the EEG signal (alpha band) would be lower
In this sense, interesting questions could be raised knowing that the easy phase duration does not change sharply after successive apneas (Nishino et al. 1996), for example: what results would be produced by EEG when the struggle phase time was increased? What would the activity of the prefrontal cortex and sensory cortex be like under conditions of respiratory distress, given that the prolongation of diaphragm activity influences the increase in voluntary activity sustaining the apnea up to its breaking point? What would EEG activity be like when we compare healthy individuals with respiratory restriction triggered by some apparatus or individuals with respiratory disorders, such as obstructive, restrictive, and neurological diseases under conditions of a prolonged struggle phase and respiratory distress? In addition to answering these questions, the successive maximal apnea test protocol associated with the use of electroencephalography could be used to assess cortical brain waves under conditions of irritability and anxiety triggered by exposure to the respiratory stress of air deprivation.
Conclusion
Based on the evidence in the literature, we propose that the prolongation of the maximal apnea time through a successive maximal apnea protocol is a useful method for the study of EEG adaptations under conditions of air deprivation. In addition, it expands the field of study of the determinants of dyspnea and respiratory distress based on the analysis of cortical activity.
Availability of data and materials
All data generated or analyzed are included in this publication.
References
Agostoni E (1963) Diaphragm activity during breath holding: factors related to its onset. J Appl Physiol 18:30–36
Andersson J, Schagatay E (1998) Effects of lung volume and involuntary breathing movements on the human diving response. Eur J Appl Physiol Occup Physiol 77(1–2):19–24
Ando S, Komiyama T, Sudo M, Higaki Y, Ishida K, Costello JT, Katayama K (2020) The interactive effects of acute exercise and hypoxia on cognitive performance: a narrative review. Scand J Med Sci Sports 30(3):384–398
Arce-Álvarez A, Veliz C, Vazquez-Muñoz M, von Igel M, Alvares C, Ramirez-Campillo R, Izquierdo M, Millet GP, Del Rio R, Andrade DC (2021) Hypoxic respiratory chemoreflex control in young trained swimmers. Front Physiol 26(12):632603
Bain AR, Drvis I, Dujic Z, MacLeod DB, Ainslie PN (2018) Physiology of static breath holding in elite apneists. Exp Physiol 103(5):635–651
Baković D, Valic Z, Eterović D, Vukovic I, Obad A, Marinović-Terzić I, Dujić Z (2003) Spleen volume and blood flow response to repeated breath-hold apneas. J Appl Physiol 95(4):1460–1466
Bartlett DJ (1977) Effects of Valsalva and Mueller maneuvers on breath-holding time. J Appl Physiol Respir Environ Exerc Physiol 42(5):717–721
Benarroch EE (1993) The central autonomic network: functional organization, dysfunction, and perspective. Mayo Clin Proc 68(10):988–1001
Berger BG, Owen DR (1988) Stress reduction and mood enhancement in four exercise modes: swimming, body conditioning, Hatha yoga, and fencing. Res Quart Exer Sport 59(2):148–159
Bordoni B, Zanier E (2013) Anatomic connections of the diaphragm: influence of respiration on the body system. J Multidiscip Healthc 25(6):281–291
Cross TJ, Breskovic T, Sabapathy S, Zubin Maslov P, Johnson BD, Dujic Z (2013) Respiratory muscle pressure development during breath holding in apnea divers. Med Sci Sports Exerc 45(1):93–101
Delapille P, Verin E, Tourny-Chollet C, Pasquis P (2001) Breath-holding time: effects of non-chemical factors in divers and non-divers. Pflugers Arch 442(4):588–594
Dimitriadis SI, Brindley L, Evans LH, Linden DE, Singh KD (2018) A novel, fast, reliable, and data-driven method for simultaneous single-trial mining and amplitude-latency estimation based on proximity graphs and network analysis. Front Neuroinform 19(12):59
Diniz CM, Farias TL, Pereira MC, Pires CB, Gonçalves LS, Coertjens PC, Coertjens M (2014) Chronic adaptations of lung function in breath-hold diving fishermen. Int J Occup Med Environ Health 27(2):216–223
Elia A, Gennser M, Harlow PS, Lees MJ (2021) Physiology, pathophysiology and (mal)adaptations to chronic apnoeic training: a state-of-the-art review. Eur J Appl Physiol 121(6):1543–1566
Espersen K, Frandsen H, Lorentzen T, Kanstrup IL, Christensen NJ (2002) The human spleen as an erythrocyte reservoir in diving-related interventions. J Appl Physiol 92(5):2071–2079
Fagoni N, Sivieri A, Antonutto G, Moia C, Taboni A, Bringard A, Ferretti G (2015) Cardiovascular responses to dry resting apnoeas in elite divers while breathing pure oxygen. Respir Physiol Neurobiol 219:1–8
Ferretti G (2001) Extreme human breath-hold diving. J Appl Physiol 84(4):254–271
Ferretti G, Costa M, Ferrigno M, Grassi B, Marconi C, Lundgren CE, Cerretelli P (1991) Alveolar gas composition and exchange during deep breath-hold diving and dry breath holds in elite divers. J Appl Physiol 70(4):794–802
Ferretti G, Costa M, Moroni R, Ranieri P, Butti F, Sponsiello N (2012) Lung volumes of extreme breath-hold divers. Sport Sci Health 7:55–59
Findley LJ, Ries AL, Tisi GM, Wagner PD (1983) Hypoxemia during apnea in normal subjects: mechanisms and impact of lung volume. J Appl Physiol Respir Environ Exerc Physiol 55(6):1777–1783
Fitz-Clarke JR (2018) Breath-hold diving. Compr Physiol 8(2):585–630
Flume PA, Eldridge FL, Edwards LJ, Mattison LE (1996) Relief of the “air hunger” of breathholding. A role for pulmonary stretch receptors. Respir Physiol 103:221–232
Foster GE, Sheel AW (2005) The human diving response, its function, and its control. Scand J Med Sci Sports 15(1):3–12
Freire RC, Nardi AE (2012) Panic disorder and the respiratory system: clinical subtype and challenge tests. Braz J Psychiatry 34(1):32–34
Guyenet PG (2014) Regulation of breathing and autonomic outflows by chemoreceptors. Compr Physiol 4(4):1511–1562
Guyenet PG, Stornetta RL, Bayliss DA (2010) Central respiratory chemoreception. J Comp Neurol 518(19):3883–3906
Guyenet PG, Abbott SB, Stornetta RL (2013) The respiratory chemoreception conundrum: light at the end of the tunnel? Brain Res 20(1511):126–137
Heath JR, Irwin CJ (1968) An increase in breath-hold time appearing after breath-holding. Respir Physiol 4:73–77
Hoiland RL, Ainslie PN, Bain AR, MacLeod DB, Stembridge M, Drvis I, Madden D, Barak O, MacLeod DM, Dujic Z (2017) β1-Blockade increases maximal apnea duration in elite breath-hold divers. J Appl Physiol 122(4):899–906
Hudson AL, Raux M, Similowski T, Niérat M (2018) The relationship between respiratory-related premotor potentials and small perturbations in ventilation. Front Physiol 9:621
Inoue H, Yamauchi K, Kobayashi H, Shikanai T, Nakamura Y, Satoh J, Kohno N, Mishima M, Sasaki H, Hildebrandt J (2009) A new breath-holding test may noninvasively reveal early lung abnormalities caused by smoking and/or obesity. Chest 136(2):545–553
Kleinfeld D, Deschênes M, Wang F, Moore JD (2014) More than a rhythm of life: breathing as a binder of orofacial sensation. Nat Neurosci 17(5):647–651
Klimesch W (2009) EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain Res Brain Res Rev 29(2–3):169–195
Klocke FJ, Rahn H (1959) Breath holding after breathing of oxygen. J Appl Physiol 14:689–693
Laurent G, Stopfer M, Friedrich RW, Rabinovich MI, Volkovskii A, Abarbanel HD (2001) Odor encoding as an active, dynamical process: experiments, computation, and theory. Annu Rev Neurosci 24:263–297
Lee SA, Lee SH, Jung BK (2015) Analysis of cortical activation during three types of therapeutic activity. J Phys Ther Sci 27(4):1219–1222
Lemaître F, Polin D, Joulia F, Boutry A, Le Pessot D, Chollet D, Tourny-Chollet C (2007) Physiological responses to repeated apneas in underwater hockey players and controls. Undersea Hyperb Med 34(6):407–414
Lemaître F, Clua E, Andréani B, Castres I, Chollet D (2010) Ventilatory function in breath-hold divers: effect of glossopharyngeal insufflation. Eur J Appl Physiol 108(4):741–747
Lin YC (1982) Breath-hold diving in terrestrial mammals. Exerc Sport Sci Rev 10:270–307
Lin YC, Lally DA, Moore TO, Hong SK (1974) Physiological and conventional breath-hold breaking points. J Appl Physiol 37(3):291–296
Lindholm P, Lundgren CE (2009) The physiology and pathophysiology of human breath-hold diving. J Appl Physiol 106(1):284–292
Lindholm P, Nyrén S (2005) Studies on inspiratory and expiratory glossopharyngeal breathing in breath-hold divers employing magnetic resonance imaging and spirometry. Eur J Appl Physiol 94(5–6):646–651
Loring SH, O’Donnell CR, Butler JP, Lindholm P, Jacobson F, Ferrigno M (2007) Transpulmonary pressures and lung mechanics with glossopharyngeal insufflation and exsufflation beyond normal lung volumes in competitive breath-hold divers. J Appl Physiol 102(3):841–846
Ma X, Yue ZQ, Gong ZQ, Zhang H, Duan NY, Shi YT, Wei GX, Li YF (2017) The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Front Psychol 8:874
Macefield G, Gandevia SC (1991) The cortical drive to human respiratory muscles in the awake state assessed by premotor cerebral potentials. J Physiol 439:545–558
Malathi A, Damodaran A (1999) Stress due to exams in medical students—role of yoga. Indian J Physiol Pharmacol 43(2):218–224
Marek W, Muckenhoff K, Prabhakar NR (2008) Significance of pulmonary vagal afferents for respiratory muscle activity in the cat. J Physiol Pharmacol 6:407
Martelli D, Stanić D, Dutschmann M (2013) The emerging role of the parabrachial complex in the generation of wakefulness drive and its implication for respiratory control. Respir Physiol Neurobiol 188(3):318–323
Martin C, Ravel N (2014) Beta and gamma oscillatory activities associated with olfactory memory tasks: different rhythms for different functional networks? Front Behav Neurosci 23(8):218
Menicucci D, Artoni F, Bedini R, Pingitore A, Passera M, Landi A, L’Abbate A, Sebastiani L, Gemignani A (2014) Brain responses to emotional stimuli during breath holding and hypoxia: an approach based on the independent component analysis. Brain Topogr 27(6):771–785
Miller EK, Cohen JD (2001) An integrative theory of prefrontal cortex function. Annu Rev Neurosci 24:167–202
Moral Y, Robertson NJ, Goni-de-Cerio F, Alonso-Alconada D (2019) Neonatal hypoxia-ischemia: cellular and molecular brain damage and therapeutic modulation of neurogenesis. Rev Neurol 68(1):23–36
Muller-Putz GR (2020) Electroencephalography. Handb Clin Neurol 168:249–252
Nannini LJ, Zaietta GA, Guerrera AJ, Varela JA, Fernández OM, Flores DM (2007) Breath-holding test in subjects with near-fatal asthma. A new index for dyspnea perception. Respir Med 101(2):246–253
Napadow V, Dhond R, Conti G, Makris N, Bronw EN, Barbieri R (2008) Brain correlates of autonomic modulation: combining heart rate variability with FMRI. Neuroimage 42(1):169–177
Nattie E, Li A (2012) Central chemoreceptors: locations and functions. Compr Physiol 2(1):221–254
Netz Y, Lidor R (2017) Mood alterations in mindful versus aerobic exercise modes. J Psychol 137(5):405–419
Nishino T (2009) Pathophysiology of dyspnea evaluated by breath-holding test: studies of furosemide treatment. Respir Physiol Neurobiol 167(1):20–25
Nishino T (2011) Dyspnoea: underlying mechanisms and treatment. Br J Anaesth 106(4):463–474
Nishino T, Sugimori K, Ishikawa T (1996) Changes in the period of no respiratory sensation and total breath-holding time in successive breath-holding trials. Clin Sci 91(6):755–761
Palada I, Bakovic D, Valic Z, Obad A, Ivancev V, Eterovic D, Shoemaker JK, Dujic Z (2008) Restoration of hemodynamics in apnea struggle phase in association with involuntary breathing movements. Respir Physiol Neurobiol 161(2):174–181
Papadelis C, Kourtidou-Papadeli C, Bamidis PD, Maglaveras N, Pappas K (2017) The effect of hypobaric hypoxia on multichannel EEG signal complexity. Clin Neurophysiol 18(1):31–52
Parkes MJ (2006) Breath-holding and its breakpoint. Exp Physiol 91(1):1–15
Patrician A, Gasho C, Spajić B, Caldwell HG, Baković-Kramaric D, Barak O, Drviš I, Dujić Ž, Ainslie PN (2021) Breath-hold diving beyond 100 meters-cardiopulmonary responses in world-champion divers. J Appl Physiol 130(5):1345–1350
Pearce WJ (2018) Fetal cerebrovascular maturation: effects of hypoxia. Semin Pediatr Neurol 28:17–28
Perciavalle V, Blandini M, Fecarotta P, Buscemi A, Di Corrado D, Bertolo L, Fichera F, Coco M (2017) The role of deep breathing on stress. Neurol Sci 38(3):451–458
Perini R, Tironi A, Gheza A, Butti F, Moia C, Ferretti G (2008) Heart rate and blood pressure time courses during prolonged dry apnoea in breath-hold divers. Eur J Appl Physiol 104(1):1–7
Perini R, Gheza A, Moia C, Sponsiello N, Ferretti G (2010) Cardiovascular time courses during prolonged immersed static apnoea. Eur J Appl Physiol 110(2):277–283
Priovoulos N, Poser BA, Ivanov D, Verhey FRJ, Jacobs HIL (2019) In vivo imaging of the nucleus of the solitary tract with Magnetization Transfer at 7 Tesla. Neuroimage 1(201):116071
Rahn H, Bahnson HT, Muxworthy JF, Hagen JM (1953) Adaptation to high altitude: changes in breath-holding time. J Appl Physiol 6(3):154–157
Rassovsky Y, Abrams K, Kushner MG (2006) Suffocation and respiratory responses to carbon dioxide and breath holding challenges in individuals with panic disorder. J Psychosom Res 60(3):291–298
Ratmanova P, Semenyuk R, Popov D, Kuznetsov S, Zelenkova I, Napalkov D, Vinogradova O (2016) Prolonged dry apnoea: effects on brain activity and physiological functions in breath-hold divers and non-divers. Eur J Appl Physiol 116(7):1367–1377
Ridderinkhof KR, Van Den Wildenberg WP, Segalowitz SJ, Carter CS (2004) Neurocognitive mechanisms of cognitive control: the role of prefrontal cortex in action selection, response inhibition, performance monitoring, and reward-based learning. Brain Cogn 56(2):29–40
Romano TG, Correia MD, Mendes PV, Zampieri FG, Maciel AT, Park M (2016) Metabolic acid-base adaptation triggered by acute persistent hypercapnia in mechanically ventilated patients with acute respiratory distress syndrome. Rev Bras Ter Intensiva 28(1):19–26
Schagatay E, Andersson J (1998) Diving response and apneic time in humans. Undersea Hyperb Med 25(1):13–19
Schagatay E, Van Kampen M, Andersson J (1999) Effects of repeated apneas on apneic time and diving response in non-divers. Undersea Hyperb Med 26:143–149
Schagatay E, Van Kampen M, Emanuelsson S, Holm B (2000) Effects of physical and apnea training on apneic time and the diving response in humans. Eur J Appl Physiol 82(3):161–169
Schagatay E, Andersson JP, Hallén M, Pålsson B (2001) Selected contribution: role of spleen emptying in prolonging apneas in humans. J Appl Physiol 90(4):1623–1629
Schipke JD, Kelm M, Siegmund K, Muth T, Sievers B, Steiner S (2015) “Lung packing” in breath hold-diving: an impressive case of pulmo-cardiac interaction. Respir Med Case Rep 16(16):120–121
Sinha M, Sinha R, Ghate J, Sarnik G (2020) Impact of altered breathing patterns on interaction of EEG and heart rate variability. Ann Neurosci 27(2):67–77
Sivieri A, Fagoni N, Bringard A, Capogrosso M, Perini R, Ferretti G (2015) A beat-by-beat analysis of cardiovascular responses to dry resting and exercise apnoeas in elite divers. Eur J Appl Physiol 115(1):119–128
Steinberg F, Doppelmayr M (2019) Neurocognitive markers during prolonged breath-holding in freedivers: an event-related EEG study. Front Physiol 10:69
Steinberg F, Pixa NH, Doppelmayr M (2017) Electroencephalographic alpha activity modulations induced by breath-holding in apnea divers and non-divers. Physiol Behav 179(1):2–26
Sterba JA, Lundgren CE (1988) Breath-hold duration in man and the diving response induced by face immersion. Undersea Biomed Res 15(5):361–375
Taboni A, Vinetti G, Bruseghini P, Camelio S, D’Elia M, Moia C, Ferretti G, Fagoni N (2018) Cardiovascular responses to dry apnoeas at exercise in air and in pure oxygen. Respir Physiol Neurobiol 255:17–21
Taboni A, Fagoni N, Fontolliet T, Grasso GS, Moia C, Vinetti G, Ferretti G (2020) Breath holding as an example of extreme hypoventilation: experimental testing of a new model describing alveolar gas pathways. Exp Physiol 105(12):2216–2225
Thayer JF, Lane RD (2009) Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev 33(2):81–88
Thornton JM, Guz A, Murphy K, Griffith AR, Pedersen DL, Kardos A, Leff A, Adams L, Casadei B, Paterson DJ (2001) Identification of higher brain centres that may encode the cardiorespiratory response to exercise in humans. J Physiol 533(Pt 3):823–836
Tort ABL, Brankack J, Draguhn A (2018) Respiration-entrained brain rhythms are global but often overlooked. Trends Neurosci 41(4):186–197
Tremoureux L, Raux M, Ranohavimparany A, Morélot-Panzini C, Pouget P, Similowski T (2014) Electroencephalographic evidence for a respiratory-related cortical activity specific of the preparation of prephonatory breaths. Respir Physiol Neurobiol 1(204):64–70
Viecili RB, Sanches PR, Silva DR, Silva DP, Muller AF, Barreto SS (2011) Bronchodilator effect on maximal breath-hold time in patients with obstructive lung disease. J Bras Pneumol 37(6):745–751
Viecili RB, Silva DR, Sanches PRS, Müller AF, Silva DP, Barreto SSM (2012) Real-time measurement of maximal voluntary breath-holding time in patients with obstructive ventilatory defects and normal controls. J Pulmon Resp Med 2:5
Walterspacher S, Scholz T, Tetzlaff K, Sorichter S (2011) Breath-hold diving: respiratory function on the longer term. Med Sci Sports Exerc 43(7):1214–1219
Whitelaw WA, McBride B, Ford GT (1987) Effect of lung volume on breath holding. J Appl Physiol 62(5):1962–1969
Zelano C, Jiang H, Zhou G, Arora N, Schuele S, Rosenow J, Gottfried JA (2016) Nasal respiration entrains human limbic oscillations and modulates cognitive function. J Neurosci 36(49):12448–12467
Zoccal DB, Furuya WI, Bassi M, Colombari DS, Colombari E (2014) The nucleus of the solitary tract and the coordination of respiratory and sympathetic activities. Front Physiol 25(5):238
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, LJAR and MC; methodology, LJAR and MC; investigation, LJAR and MC; resources, LJAR and MC; data curation, LJAR, MC, and VHVB; writing—original draft preparation, LJAR, MC, and VHVB; writing—review and editing, LJAR, MC, and VHVB; visualization, MC and VHVB; supervision, MC and VHVB; project administration, MC and VHVB. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has conflicts of interest to declare.
Consent for publication
No personal data are published.
Additional information
Communicated by Michael I Lindinger.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro, L.d.A., Bastos, V.H.d. & Coertjens, M. Breath-holding as model for the evaluation of EEG signal during respiratory distress. Eur J Appl Physiol 124, 753–760 (2024). https://doi.org/10.1007/s00421-023-05379-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-023-05379-x