Abstract
Purpose
Sickle cell trait is characterized by the presence of both normal and abnormal haemoglobin in red blood cells. The rate of exertional collapse is increased in athletes and military recruits who carry the trait, particularly in stressful environmental conditions. The aim of the present study was to investigate microvascular function and its determinants in response to intense exercise at control and warm environmental temperatures in carriers (AS) and non-carriers (AA) of sickle cell trait.
Methods
Nine AS and 11 AA, all healthy physically active young men, randomly participated in four experimental sessions (rest at 21 °C and 31 °C and cycling at 21 °C and 31 °C). All participants performed three exercises bouts as follows: 18-min submaximal exercise; an incremental test to exhaustion; and three 30-s sprints spaced with 20-s resting intervals.
Results
Skin Blood Flow (SkBF) was similar at rest between AA and AS. SkBF for all participants was higher at 31 °C than 21 °C. It was significantly higher in the AS group compared to the AA group immediately after exercise, regardless of the environmental conditions. No significant differences in hemorheological parameters, muscle damage or cardiac injury biomarkers were observed between the two groups. Our data also suggest higher oxidative stress for the AS group, with high superoxide dismutase (P = 0.044 main group effect).
Conclusion
A specific profile is identified in the AS population, with increased microvascular reactivity after maximal exercise in stressful environment and slight pro-/antioxidant imbalance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sickle cell trait (SCT) is the heterozygous form of sickle cell anaemia characterized by the presence of normal haemoglobin A (HbA) and about 40% of abnormal haemoglobin S (HbS). It is usually considered an asymptomatic and benign condition. However, epidemiological studies on cohorts of U.S. army youth (Harmon et al. 2012; Kark et al. 1987; Nelson et al. 2018; Quattrone et al. 2015; Singer et al. 2018) and young athletes (Key et al. 2015; O’Connor et al. 2012) have reported serious events such as exertional rhabdomyolysis, sometimes resulting in death immediately after exercise in SCTs. Numerous case studies indicate high exercise intensity may present major risks of exercise collapse in the context of SCT (Hedreville et al. 2009; Quattrone et al. 2015; Singer et al. 2018). Particular attention should be paid to hot environmental conditions. Hemorheological disturbances may be accentuated by the effect of dehydration in these conditions.
Nevertheless, the mechanisms underlying these complications have not been clearly defined. Increased blood viscosity and slightly decreased red blood cell (RBC) deformability have been reported after exercise in SCT carriers in comparison with non-SCT carriers and it has been suggested that this specific blood rheological profile may impair blood flow through the microcirculation. Blood viscosity has been found to be further increased in SCT carriers when they exercise in hot conditions with water deprivation(Diaw et al. 2014; Tripette et al. 2010a,b) the contributions of enhanced coagulation activity, oxidative stress and inflammation have also been suspected in exertional collapse in SCT (Chirico et al. 2016). However, no direct evidence links the pathogenesis of exercise-related death to microvascular obstruction by rigid RBCs and/or highly viscous blood (Connes et al. 2006; Tripette et al. 2010a,b). Despite clear evidence of vascular alterations noted post-mortem in humans, no study has investigated the microvascular specificity of SCT carriers both at rest and after intense exercise, and more particularly in various ambient environmental temperatures. The aim of the present study was to compare the microvascular function and its determinants in response to intense exercise conducted in either control or warm environment between SCT carriers (AS) and controls (AA). The secondary purpose was to compare blood rheological, circulating muscle and cardiac damage biomarkers, and oxidative stress responses to exercise and environmental stress between the two groups.
Materials and methods
Participants
Twenty young men participated in this study after giving their informed consent: 9 SCT carriers (AS group, 21 ± 3 years, 182 ± 6 cm, 76.2 ± 6.9 kg, 23.1 ± 1.9 kg/m2) and 11 control participants (AA group, 21 ± 2 years, 181 ± 7 cm, 73.8 ± 9.5 kg, 22.4 ± 2.4 kg/m2). All participants were acclimated to tropical climate. To participate in this study, they had to have lived in the West Indies for at least 6 months. They regularly practiced athletic activities (12.0 ± 2.1 h/week). The exclusion criteria included any known chronic disease. They were informed of the study aims, requirements and risks before providing written informed consent. In this study, only men were selected as female and male hormones may be associated with differentiated skin blood flow responses (Charkoudian and Stachenfeld 2014; Reminy et al. 2020).
Protocol
Study design
All participants completed four experimental sessions in randomized order with each session performed > 1 week apart. Experimental sessions consisted of two resting control sessions and two exercise sessions. Exercise and resting sessions were performed in both environmental temperatures. Blood samples were obtained exclusively during exercise sessions (warm and control). Participants were instructed to refrain from physical activity, alcohol, and caffeine for 24 h before each experimental session and were asked to replicate their dietary intake for 24 h before each session. We had data loss for some variables.
Pre-experimental procedures
All participants completed a familiarization session to the equipment’s and the exercise protocol. For this session, they arrived in fasting state and anthropometric data were collected.
Exercise session
Exercise was performed on a leg cycle ergometer (Monark, Lc4 Stockholm, Sweden). The participants started the session with a submaximal exercise test at 75 W for 18 min, followed by an incremental exercise test where power was increased by 25 W every minute until exhaustion. The maximal power output (Pmax) was recorded. After 15 min of recovery, three 30-s sprints at 200% of Pmax and separated by 20 s of passive recovery were performed by each participant. Heart rate (M400, Polar Electro, Kempele, Finland) and gas exchanges (Metalyzer ® 3B, Cortex Biophysik GmbH, Germany) were measured during the exercise test. Hydration was controlled during the entire study (4-ml water/kg body mass/intake after warm-up, maximal exercise and sprints).
Data on body composition and body mass were collected by bioelectrical impedance analysis using an InBody 720 analyser with InBody 3.0 software (BioSpace, Seoul, South Korea). Tympanic temperature was measured with a digital ear thermometer (Omron Gentle Temp 520) in all experimental sessions. Systolic and diastolic blood pressures (BP) were measured with a tensiometer (Omron M6, Healthcare Co., Ltd., Kyoto, Japan) during each experimental session. Blood pressure and tympanic temperature were measured before and after exercise protocol.
Environmental conditions
All participants completed four trials under two environmental conditions in a temperature-controlled room: control at 21 °C and warm at 31 °C, all at > 60% relative humidity. Environmental conditions were controlled with the wet bulb globe temperature (Delta Ohm, Padova, Italia) during all experimental sessions.
Biochemical analysis
Plasma chlorine (Cl−), sodium (Na+) and potassium (K+) concentrations were measured with an ADVIA 1200/1800 electrolyte analyzer, and the alkaline reserve by enzymatic method. Several markers of muscle damage were also followed namely creatine phosphokinase and lactate dehydrogenase.
Creatine phosphokinase (CPK, ng/mL) was determined according to the method of IFCC (1980), measured using the ADVIA 1800 clinical chemical analyzer. Serum lactate dehydrogenase (LDH, U/L) was determined using the pyruvate/NADH ratio measured by the ADVIA 1200/1800 (Siemens Healthcare Diagnostics, Eschborn, Germany).
Biomarkers of cardiac injury were investigated: troponin (ng/mL), myoglobin (ng/mL), n-terminal pro-brain natriuretic peptide (NT-proBNP, pg/ml) and creatine phosphokinase (CPK-MB) were determined by commercial chemiluminescence assays for ADVIA Centaur (Siemens Medical Solutions Diagnostics, Fernwald, Germany).
Blood lactate was drawn at rest and directly after the exercise protocol from the fingertip and analyzed on the Lactate Pro 2 (AKRAY Europe, Amstelveen, the Netherlands), a handheld point-of care analyzer that operates by enzymatic amperometric detection.
Haemoglobin electrophoresis test
To verify AS and AA genotypes, blood samples were collected in EDTA tubes at rest and screened by isoelectric focusing. The results were confirmed by citrate agar electrophoresis. Positive test results for SCT were determined by the presence of HbS (< 40%) and a normal percentage of other haemoglobin.
Hemorheological measurements
All hemorheological measurements were carried out within 1–2 h of the venipuncture, following the guidelines for international standardization in blood rheology techniques/measurements.
Blood viscosity was determined at native hematocrit, 25 °C and several shear rates: 11.25, 22.5, 45, 90 and 225 s−1 using a cone/plate viscometer (Brookfield DVII + with CPE40 spindle, Brookfield Engineering Labs., Natick, MA, USA). Red blood cell (RBC) deformability was determined at 37 °C at two shear stresses (0.30 and 30 Pa) by laser diffraction (ecktacytometry), using the Laser-assisted Optical Rotational Cell Analyzer (LORCA, RR Mechatronics, Hoorn, The Netherlands). RBC aggregation was determined at 37 °C via syllectometry, i.e., laser backscatter vs. time, using the LORCA after adjustment of hematocrit to 40%, and was reported as the aggregation index AI (%). The RBC disaggregation threshold (γthr, in s−1), i.e., the strength/robustness of RBC aggregates, was determined using a reiteration procedure.
Oxidative stress markers
Plasma pro-oxidative markers Plasma aliquots obtained from EDTA samples were stored at − 80 °C until analysis. Plasma adavanced oxidation protein products (AOPP) concentration was determined using a semi-automated method and the AOPP assay kit (OxiSelect™ AOPP Assay Kit, Cell Biolabs, Inc.) (Witko-Sarsat et al. 1996). Plasma malondialdehyde (MDA) level was determined using a method based on thiobarbituric acid (TBA) reactions and formation of MDA-TBA adducts quantified fluorometrically (Ex/Em = 532/553 nm) (ab118970 Assay Kit, Abcam®). Plasma myeloperoxidase (MPO) protein levels were quantified by ELISA technique (ab119605 Kit, Abcam®). Plasma nitrotyrosine, evaluated through the end product of protein nitration induced by peroxynitrite, was measured by Elisa (av210603 Kit, Abcam®). Plasma nitric oxide (NO) end products were determined after the enzymatic conversion of nitrate to nitrite by nitrate reductase and the colorimetric detection of nitrite using the Griess method (ADI-917-020 Kit, Enzo). Plasma heat shock protein 70 (HSP70) was measured with the high-sensitivity ENZ-KIT-101 Kit (Enzo) according to the manufacturer’s instructions.
RBC antioxidant defence RBC pellets from citrate blood samples were treated with four volumes of an aqueous solution containing 5% metaphosphoric acid, and the lysates obtained from 50 µl of RBCs were stored at -80 °C until assay. The colorimetric measurement of reduced (GSH) and oxidized (GSSG) RBC glutathione is based on the reaction of the sulfhydryl group of GSH with Ellman’s reagent, giving a yellow-colored product (ADI-900-160 Kit, Enzo).
RBC pellets from EDTA blood samples were lysed in four volumes of ice-cold water. The lysates’ aliquots were stored at − 80 °C until they were used for the assessment of the enzymatic antioxidant defence through RBC superoxide dismutase (SOD) and catalase (Cat) activities. RBC SOD activity was determined by a colorimetric assay based on its ability to scavenge superoxide radicals generated by xanthine oxidase and hypoxanthine, which form a colorimetric reaction in the presence of a tetrazolium salt (Kit 706002, Cayman Chemical). RBC catalase activity was also determined by a colorimetric assay based on the formation of a colored formaldehyde induced by the reaction of catalase with methanol in the presence of a chromogen (707002 Kit, Cayman Chemical).
Skin blood flow
Skin blood flow (SkBF) and microvascular reactivity response to local heating protocol were measured by laser Doppler flowmetry using the Periflux System 5000 (Perimed, Järfälla, Sweden) and its associated software Perisoft, which enables continuous SkBF recording. A temperature-controlled skin probe was attached to a distal finger pad with adhesive tape.
The skin temperature was obtained through the probe of the device and was raised locally to 42 °C at a rate of 0.1 °C/s. This protocol induces a biphasic increase in SkBF: (1) a rapid increase with a peak (peak phase) reached within the first 5 min of local heating, which is related to axon reflex, and (2) a prolonged plateau (plateau phase), which appears 20–25 min after the beginning of the hyperthermic stimulus and is mainly induced by NO production.
For resting sessions, SkBF was measured for 45 min: 5 min without local heating (baseline and post heating) and 35 min during local heating. For exercise sessions, SkBF was measured after the exercise protocol for 10 min: 5 min baseline and 5 min under local heating.
Laser Doppler blood flow (perfusion unit, recorded in mV) was divided by the individual mean arterial pressure (MAP) and expressed as cutaneous vascular conductance (CVC, mV/mm Hg).
The signal was processed as follows: the baseline corresponds to the SkBF without heating for 5 min out of the 10-min measurement). The two responses to local hyperthermia: (1) peak max value over the first 5 min and (2) plateau average over the last 10 min of local hyperthermia. SkBF was averaged point by point (6 Hz) over the entire recording for all AAs and all ASs.
Statistical analyses
Analyses of variance (ANOVA) with repeated measures were performed on SkBF. Resting and exercise sessions were analyzed separately with group (AA, AS) as the between-subject variable. Pre-post exercise (two levels: T0 and T50), environmental condition (21 °C, 31 °C) and phases (baseline, peak and plateau) were used as within-subject variables when required.
ANOVAs with repeated measures were performed on all laboratory measurements (biochemical, oxidative stress and hemorheological parameters), blood pressure, heart rate and tympanic temperature with group (AA, AS) as the between-subjects variable, and pre-post exercise (two levels: T0 and T50), and environmental conditions (21 °C, 31 °C) as the within-subjects variable. ANOVAs were applied to oxygen uptake and maximal power (Pmax) with group (AA, AS) as the between-subjects variable, and environmental condition (21 °C, 31 °C) as the within-subjects variables.
Data were tested for sphericity using Mauchly’s test and if the assumption of sphericity was violated, the Greenhouse–Geisser correction was undertaken to adjust the degrees of freedom. Tukey's post hoc tests were performed to identify mean differences among conditions when group x temperature x time interaction was significant.
All results were analyzed with the SPSS 23 software package (SPSS Inc, Chicago, IL, USA). Statistical significance was set at P < 0.05. Unless otherwise stated, data are presented as mean ± SD.
Results
Physiological responses to exercise and plasma ion concentration did not differ between AA and AS and were affected in the same way by warm environment
As shown in Table 1, heart rate, blood pressure and skin temperature at rest and maximal exercise, and performance (Pmax) parameters did not differ between the two groups in response to exercise.
No complications were observed during the experimental sessions. During and after exercise, tympanic temperature was affected by environmental condition (P < 0.001) with higher values in a warm environment than control for all group. During the resting and exercise sessions, there was no significant single group effect or group-related interaction effect (P = 0.715) with the exception of skin temperature, which was higher at rest at 31 °C in AS as compared with AA in the condition.
The plasma concentration of Cl−, Na+, and K+ and the alkaline reserves (Table 2) did not present significant change between AA and AS (P > 0.593). The plasma concentration of Cl−, K+ and the alkaline reserves decreased after exercise tests (P < 0.002), but to the same extent in the AA and AS groups (no significant interaction). Cl− plasma concentrations were lower at 21 °C than at 31 °C for both groups.
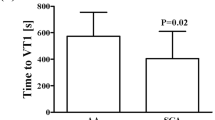
Blood lactate concentration Fig. 2.H was affected by exercise (P < 0.001) with higher values after exercise in the two conditions for the two groups. The environmental conditions did not affect blood lactate (P = 0.176). For blood lactate concentration, only the condition x time interaction was significant (P = 0.007). There was no significant single group effect or group-related interaction effect (all P > 0.167).
Microvascular reactivity was higher in AS after exercise
The results are summarized in Fig. 1 at rest (A and B) and after exercise (C and D). At rest, SkBF was no different between the two groups in response to the local heating protocol (P = 0.452). A simple effect of phase (baseline, peak and plateau) was observed, characterizing the reactivity to local heat (P < 0.001) for both groups. SkBF was higher at 31 °C than at 21 °C. The phase × environmental condition interaction was significant (P = 0.030), with marked variations between baseline peak and plateau at 21 °C. These variations were independent of the group (no other significant interaction involving the group were significantly different, all P > 0.780). A similar profile is reported after arterial pressure normalization (CVC results provided in table supplement data).
After the exercise tests, SkBF was different between the two groups (simple group effect: P = 0.019) with greater values found in the AS group. The simple effect of phase between baseline and peak was significant (P < 0.001). The phase × environmental condition interaction effect was significant (P < 0.001), with marked variations between baseline and peak at 21 °C but not at 31 °C. No other interactions were significant (P > 0.229).
Exercise increased and warm environment decreased blood viscosity but AA and AS were not different
Hematocrit, blood viscosity at all shear rates, RBC aggregation, and disaggregation threshold, and deformability (EI 0.30, 30) were not different between the groups (Table 3) (all P > 0.108).
For all groups, hematocrit, blood viscosity at all shear rates, and the aggregation index (AI) values were significantly higher after exercise than at rest (all P < 0.011).
Blood viscosity at 45, 90 and 225 s−1 was lower at 31 °C for both groups compared to 21 °C (all P > 0.043). For blood viscosity at 90 s −1, the condition x group interaction was significant (P = 0.039), with higher viscosity at 90 s−1 in AS at 21 °C compared to 31 °C, while viscosity was unchanged by the environmental temperature in AA. No other interactions were significant (all P > 0.099).
Markers of rhabdomyolysis and cardiac injury were affected by exercise but did not differ between AA and AS in either environment
None of the biomarkers used to identify cardiac injury and muscle damage (Fig. 2A–G) were significantly different between AA and AS groups (all P = 0.187). Exercise increased CPK, CPK-MB and NT-proBNP (P < 0.001, P < 0.001, P = 0.035, respectively). CPK, LDH and myoglobin (P = 0.042, P = 0.013, P = 0.012, respectively) were lower at 31 °C than at 21 °C. The time x group interaction effect was observed for CPK (P = 0.023), with higher CPK values in AA after exercise compared to before exercise, while CPK values remained unchanged in AS.
Markers of oxidative stress were affected by the group regardless of environmental conditions
The concentrations of the pro-oxidative markers, AOPP, MPO, MDA, nitrotyrosine, Hsp70, NO, (Fig. 3 and 4) were not different between the two groups (all P > 0.187).
Responses of blood concentration of A Advanced oxidation protein products AOPP, B malondialdehyde MDA (uM), C myeloperoxidase MPO (ng/mL), and D nitrotyrosine (ng/mL) and Heat shock protein 70 Hsp70 (ng/mL) (E), pre-exercise (T0) and post-exercise (T50) in AA group (solid line) and AS group (dashed line) at 21 °C (gray line) and 31 °C (black line). Values are mean ± SEM. *P < 0.05 vs. T0 **P < 0.001 vs. T0
Responses of antioxidants A catalase CAT (μmoles/min/gHb), B superoxide dismutase SOD (U/gHb), C oxide nitric NO (umol/L), D GSSG (nM), E GSH (nM) and F Glutathione Ratio (nM), pre-exercise (T0) and post-exercise (T50) in AA group (solid line) and AS group (dashed line) at 21 °C (gray line) and at 31 °C (black line). Values are mean ± SEM. P < 0.05 vs. AA
For both groups, nitrotyrosine and Hsp70 (Fig. 3) concentration were increased after exercise (P < 0.001, P = 0.014, respectively). Exercise did not affect the other parameters (all P > 0.101). The condition x group interaction was significant (P = 0.049) for MPO concentration. Concerning antioxidant status, SOD was higher (P = 0.044) while catalase was lower (P = 0.024) for the AS group compared to the AA group (Fig. 4). The environmental conditions (21 °C/31 °C) did not affect any of the measured biomarkers. All other interactions were not significant (all P > 0.068).
Discussion
The present study investigated the microvascular function at rest and after maximal exercise at 21 °C and 31 °C for both AS and AA groups. The major results are: (1) the skin blood flow response was normal in AS at rest and control environment (21 °C), but increased in warm environment (31 °C); (2) after maximal exercise, the microvascular dilatation was higher in the AS group compared to the AA group; (3) higher superoxide dismutase and lower catalase antioxidant activity suggested a disorder in oxidative homeostasis for the AS group; and (4) the AS group was comparable to the AA group concerning markers of muscle damage and blood rheology after exercise.
AS and AA were affected in the same way by exercising warm environment with regards to cardiovascular responses, electrolytes, cardiac and muscle injury biomarkers
Previous studies have emphasized specific aspects of physical ability and/or physiological responses to exercise in AS participants. This was not the main objective here, but the results of the present study did not evidence any difference between AA and AS for exercise power or heart rate measures during exercise. Although there are some controversies, similarities have been demonstrated between AA and AS in physical fitness and cardiovascular adaptations to exercise by previous studies from our group (Marlin et al. 2008; Sara et al. 2006), as well as others (Bilé et al. 1996). In addition, we report that lactate was increased after exercise in the same way for both groups and regardless of the environmental condition.
Exercise-induced rhabdomyolysis is a clinical and biochemical syndrome. It may lead to acute renal failure caused by myoglobinuria and, ultimately, death (Zimmerman and Shen 2013). Numerous case reports have described this type of complication in SCT carriers after exercise (Buchanan et al. 2020; Hedreville et al. 2009; Quattrone et al. 2015; Saxena et al. 2016). There were no overt clinical or biological signs of rhabdomyolysis and electrolyte imbalance among our cohort. CPK concentration was increased normally after maximal exercise without a significant group-related effect. The variations we reported with exercise are known to occur in trained and healthy individuals after intense exercise (Pedersen et al. 2019) and in AS athletes after submaximal (Messonnier et al. 2012) or maximal exercise (Gozal et al. 1992). Our results also showed that there was no cardiac injury. CPK-MB and NT-proBNP were higher after exercise but remained in the normal range. There was no difference between AA and AS for rhabdomyolysis or cardiac injury markers. This is the first study that provides information on these biomarkers after intense exercise in a warm environment in AS subjects.
Specific microvascular reactivity in AS and potential explanations
Recent studies in mice and human models of SCT support the presence of macrovascular and microvascular dysfunction (Diaw et al. 2015; Skinner et al. 2019, 2020). The microvascular function has not been deeply investigated in response to exercise in human with SCT. In this study, only measurements from glabrous skin were performed, which constitutes a limitation. It however provides valuable information on overall tissular perfusion and thermoregulatory mechanisms due to its singular structure (anastomoses and volume/surface ratio of capillaries) (Walløe 2015). Moreover, contrary to the forearm measurement, often used as a substitute for non-glabrous skin, the reproducibility is strong. This is an important point for this study containing several experimental sessions (Roustit et al. 2010).
We showed that SkBF and microvascular reactivity were not different between SCT and non-SCT carriers at rest regardless of environmental condition. However, we observed a greater ability of skin microvessels to dilate in response to local heating after exercise in the SCT participants. While cases of fatal events reported in SCT carriers would suggest an involvement of the microcirculation, our results do not support a systematically deleterious role of microvascular function in the physiological adaptations to exercise in SCT carriers.
In the present study, the strenuous exercise was followed by an increase in viscosity for both groups. This adaptation is well described in the literature, both in healthy subjects (Nader et al. 2019) and SCT carriers, and is mainly due to the changes in hematocrit and RBC aggregation. No significant differences were observed between AA and AS participants at rest or after exercise regardless of the environmental condition. This finding could seem surprising as several studies reported higher blood viscosity in AS than in AA both at rest (Tripette et al. 2009) and in response to exercise (Connes et al. 2006). One explanation might be that the participants in this study followed a strict hydration protocol, which might have corrected the hemorheological alterations described in SCT carriers, as previously reported (Diaw et al. 2014; Tripette et al. 2010a,b). In addition, RBC deformability, a strong contributor to blood viscosity, was not impacted by SCT. Enhanced oxidative stress has been shown to cause a decrease in RBC deformability in sickle cell disease (Hierso et al. 2014). The oxidative stress/antioxidant profile was rather similar between AA and AS at rest and after exercise, and the plasma NO concentration remained unchanged after exercise. This could explain the lack of difference in RBC deformability between the two groups, confirming previous findings (Tripette et al. 2010a,b). The lack of difference in blood viscosity and other RBC rheological parameters between AA and AS at rest and after exercise in both environments, associated with the greater vasodilation in AS in warm environment, would have resulted in normal organ perfusion and oxygen delivery. This would explain why the AS group did not show any biological or clinical signs of cardiac or muscle injury. Subsequently, plasma NO and RBC rheological parameters were probably not importantly involved in the improved microvascular function in the AS participants after exercise.
Concerning antioxidant defences, the SOD level was higher in AS compared to AA. In agreement relatively with earlier this results (Das et al. 1993). Generally, intensive exercise increases SOD activity in healthy young subjects and regular exercise attenuates ROS production. In our study, SOD activity remained unchanged after exercise for the AA group. All subjects in this study were in acceptable physical condition. On the other hand, the observation that SOD activity was higher in the AS subjects may be explained by the presence of haemoglobin S (< 39%), which accelerates heme autoxidation (Alayash 2018; Hebbel et al. 1988). This could lead to an increase in the antioxidant defences, particularly SOD activity prior to exercise. Indeed, SOD is a first-line antioxidant enzyme that can counteract the overproduction of intracellular ROS that can then be found in the extracellular environment (Ighodaro and Akinloye 2018; Wang et al. 2018).
These results suggest a higher oxidative stress in the AS RBCs has observed previous studies Das et al. 1993. Das et al. et al. (1993) they also observed a higher SOD activity in AS RBCs with a reduced activity of other anti-oxidant enzymes such as GPx. They suggested that the increase in SOD was probably induced by the release of RBCs sequestered in the spleen, since the increase in free radicals has the effect of deactivating SOD and that synthesis is unlikely in mature erythrocytes. However, we cannot state this here because we did not obtain a difference in haematocrit between AAs and ASs. We have reason to believe that such a thing occurs in view of the increased capacity for auto-oxidation of haem in the presence of haemoglobin S.
Perspectives
We observed differentiated SkBF responses to exercise. In AA, this response can be interpreted as a "ceiling effect" expressed by a healthy endothelium, as previously suggested (Francisco et al. 2017). Conversely, the SkBF observed in AS suggests a larger vasodilatatory reserve. Romero et al. investigated micro- and macrovascular function in elderly and younger subjects and found that a large reserve in vascular reactivity might not be the normal response (Romero et al. 2017), although this may be counterintuitive. We thus suggest that the SkBF profile we identified is not normal. This profile may instead be optimized to adapt to the physiological constraints specific to SCT carriers. In line with this view, previous studies have demonstrated vascular remodeling in active AS characterized by a decrease in the tortuosity of the vessels, which gives way to a greater density of large capillaries to the detriment of small capillaries (Vincent et al. 2010).
Conclusion
No evidence of severe vascular impairment, cardiac injury, rhabdomyolysis or occlusive events was observed in the sickle cell trait carriers of this study, despite conditions conducive to these types of complications. A specific profile was identified in this population, with enhanced microvascular reactivity after maximal exercise in stressful environment and slight pro-/antioxidant imbalance. Studies concerning the mechanisms underlying possible microvascular adaptations in trained AS are necessary. It would also be relevant to observe whether this increase dilatation persists in late recovery.
Abbreviations
- AI%:
-
Aggregation index
- AOPP:
-
Advanced oxidation protein products
- CAT:
-
Catalase
- CL– :
-
Chlorine
- CPK:
-
Creatine phosphokinase
- CPK-MB:
-
Creatine phosphokinase –myoglobin
- GSH:
-
Reduced glutathione
- GSSG:
-
Oxidized glutathione
- HSP70:
-
Heat shock protein 70
- LDH:
-
Lactate dehydrogenase
- K+ :
-
Potassium
- MDA:
-
Malondialdehyde
- MPO:
-
Myeloperoxidase
- NO:
-
Oxide nitric
- NT PROBNP:
-
N-terminal pro-brain natriuretic peptide
- RBC:
-
Red blood cell
- SCT:
-
Sickle cell trait
- SKBF:
-
Skin blood flow
- SOD:
-
Superoxide dismutase
References
Alayash AI (2018) Oxidative Pathways in the Sickle Cell and Beyond. Blood Cells Mol Dis 70:78–86. https://doi.org/10.1016/j.bcmd.2017.05.009
Bilé A, Le Gallais D, Mercier B, Martinez P, Ahmaidi S, Préfaut C (1996) Anaerobic exercise components during the force-velocity test in sickle cell trait. Int J Sports Med 17(4):254–258. https://doi.org/10.1055/s-2007-972842
Buchanan BK, Siebert DM, Suchsland MLZ, Drezner JA, Asif IM, O’Connor FG, Harmon KG (2020) Sudden Death Associated with Sickle Cell Trait before and after Mandatory Screening. Sports Health. https://doi.org/10.1177/1941738120915690
Charkoudian N, Stachenfeld NS (2014) Reproductive Hormone Influences on Thermoregulation in Women. In: Comprehensive Physiology (p. 793‑804). American Cancer Society. https://doi.org/10.1002/cphy.c130029
Chirico EN, Faës C, Connes P, Canet-Soulas E, Martin C, Pialoux V (2016) Role of exercise-induced oxidative stress in sickle cell trait and disease. Sports Med 46(5):629–639. https://doi.org/10.1007/s40279-015-0447-z
Connes P, Sara F, Hardy-Dessources M-D, Marlin L, Etienne F, Larifla L, Saint-Martin C, Hue O (2006) Effects of short supramaximal exercise on hemorheology in sickle cell trait carriers. Eur J Appl Physiol 97(2):143–150. https://doi.org/10.1007/s00421-006-0155-3
Das SK, Hinds JE, Hardy RE, Collins JC, Mukherjee S (1993) Effects of physical stress on peroxide scavengers in normal and sickle cell trait erythrocytes. Free Radical Biol Med 14(2):139–147. https://doi.org/10.1016/0891-5849(93)90004-e
Diaw M, Samb A, Diop S, Sall ND, Ba A, Cissé F, Connes P (2014) Effects of hydration and water deprivation on blood viscosity during a soccer game in sickle cell trait carriers. Br J Sports Med 48(4):326–331. https://doi.org/10.1136/bjsports-2012-091038
Diaw M, Pialoux V, Martin C, Samb A, Diop S, Faes C, Mury P, Sall Diop N, Diop S-N, Ranque B, Mbaye MN, Key NS, Connes P (2015) Sickle cell trait worsens oxidative stress, abnormal blood rheology, and vascular dysfunction in Type 2 Diabetes. Diabetes Care 38(11):2120–2127. https://doi.org/10.2337/dc15-0699
Francisco MA, Brunt VE, Jensen KN, Lorenzo S, Minson CT (2017) Ten days of repeated local forearm heating does not affect cutaneous vascular function. J Appl Physiol 123(2):310–316. https://doi.org/10.1152/japplphysiol.00966.2016 ((Bethesda, Md.: 1985))
Gozal D, Thiriet P, Mbala E, Wouassi D, Gelas H, Geyssant A, Lacour JR (1992) Effect of different modalities of exercise and recovery on exercise performance in subjects with sickle cell trait. Med Sci Sports Exerc 24(12):1325–1331
Harmon KG, Drezner JA, Klossner D, Asif IM (2012) Sickle cell trait associated with a RR of death of 37 times in national collegiate athletic association football athletes: a database with 2 million athlete-years as the denominator. Br J Sports Med 46(5):325–330. https://doi.org/10.1136/bjsports-2011-090896
Hebbel RP, Morgan WT, Eaton JW, Hedlund BE (1988) Accelerated autoxidation and heme loss due to instability of sickle hemoglobin. Proc Natl Acad Sci USA 85(1): 237‑241. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC279519/
Hedreville M, Connes P, Romana M, Magnaval G, David T, Hardy-Dessources M-D, Belloy M-S, Etienne-Julan M, Hue O (2009) Central retinal vein occlusion in a sickle cell trait carrier after a cycling race. Med Sci Sports Exerc 41(1):14–18. https://doi.org/10.12s49/MSS.0b013e31818313d0
Hierso R, Waltz X, Mora P, Romana M, Lemonne N, Connes P, Hardy-Dessources M-D (2014) Effects of oxidative stress on red blood cell rheology in sickle cell patients. Br J Haematol 166(4):601–606. https://doi.org/10.1111/bjh.12912
Ighodaro OM, Akinloye OA (2018) First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): their fundamental role in the entire antioxidant defence grid. Alex J Med 54(4):287–293. https://doi.org/10.1016/j.ajme.2017.09.001
Kark JA, Posey DM, Schumacher HR, Ruehle CJ (1987) Sickle-cell trait as a risk factor for sudden death in physical training. N Engl J Med 317(13):781–787. https://doi.org/10.1056/NEJM198709243171301
Key NS, Connes P, Derebail VK (2015) Negative health implications of sickle cell trait in high income countries: from the football field to the laboratory. Br J Haematol 170(1):5–14. https://doi.org/10.1111/bjh.13363
Marlin L, Connes P, Antoine-Jonville S, Tripette J, Montout-Hedreville M, Sanouiller A, Etienne-Julan M, Hue O (2008) Cardiorespiratory responses during three repeated incremental exercise tests in sickle cell trait carriers. Eur J Appl Physiol 102(2):181–187. https://doi.org/10.1007/s00421-007-0570-0
Messonnier L, Samb A, Tripette J, Gogh BD, Loko G, Sall ND, Féasson L, Hue O, Lamothe S, Bogui P, Connes P (2012) Moderate endurance exercise is not a risk for rhabdomyolysis or renal failure in sickle cell trait carriers. Clin Hemorheol Microcirc 51(3):193–202. https://doi.org/10.3233/CH-2011-1524
Nader E, Skinner S, Romana M, Fort R, Lemonne N, Guillot N, Gauthier A, Antoine-Jonville S, Renoux C, Hardy-Dessources M-D, Stauffer E, Joly P, Bertrand Y, Connes P (2019) Blood rheology: key parameters, impact on blood flow, role in sickle cell disease and effects of exercise. Front Physiol. https://doi.org/10.3389/fphys.2019.01329
Nelson DA, Deuster PA, O’Connor FG, Kurina LM (2018) Sickle cell trait and heat injury among US Army soldiers. Am J Epidemiol 187(3):523–528. https://doi.org/10.1093/aje/kwx285
O’Connor FG, Bergeron MF, Cantrell J, Connes P, Harmon KG, Ivy E, Kark J, Klossner D, Lisman P, Meyers BK, O’Brien K, Ohene-Frempong K, Thompson AA, Whitehead J, Deuster PA (2012) ACSM and CHAMP summit on sickle cell trait: mitigating risks for warfighters and athletes. Med Sci Sports Exerc 44(11):2045–2056. https://doi.org/10.1249/MSS.0b013e31826851c2
Pedersen ES, Tengesdal S, Radtke M, Langlo KAR (2019) Major increase in creatine kinase after intensive exercise. Tidsskrift for Den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke. https://doi.org/10.4045/tidsskr.18.0120
Quattrone RD, Eichner ER, Beutler A, Adams WB, O’Connor FG (2015) Exercise collapse associated with sickle cell trait (ECAST): case report and literature review. Curr Sports Med Rep 14(2):110–116. https://doi.org/10.1249/JSR.0000000000000137
Reminy K, Hue O, Antoine-Jonville S (2020) Effect of warm environment on the skin blood flow response to food intake. Int J Hyperth 37(1):836–842. https://doi.org/10.1080/02656736.2020.1788174
Romero SA, Gagnon D, Adams AN, Cramer MN, Kouda K, Crandall CG (2017) Acute limb heating improves macro- and microvascular dilator function in the leg of aged humans. Am J Physiol Heart Circ Physiol 312(1):H89–H97. https://doi.org/10.1152/ajpheart.00519.2016
Roustit M, Blaise S, Millet C, Cracowski JL (2010) Reproducibility and methodological issues of skin post-occlusive and thermal hyperemia assessed by single-point laser Doppler flowmetry. Microvasc Res 79(2):102–108. https://doi.org/10.1016/j.mvr.2010.01.001
Sara F, Hardy-Dessources M-D, Marlin L, Connes P, Hue O (2006) Lactate distribution in the blood compartments of sickle cell trait carriers during incremental exercise and recovery. Int J Sports Med 27(6):436–443. https://doi.org/10.1055/s-2005-865844
Saxena P, Chavarria C, Thurlow J (2016) Rhabdomyolysis in a Sickle Cell Trait Positive Active Duty Male Soldier. U.S. Army Med Dep J 20–23.
Singer DE, Byrne C, Chen L, Shao S, Goldsmith J, Niebuhr DW (2018) Risk of Exertional Heat Illnesses Associated with Sickle Cell Trait in U.S. Military. Military Medicine, 183(7‑8), e310–e317. https://doi.org/10.1093/milmed/usx085
Skinner S, Connes P, Sigaudo-Roussel D, Lo M, Liu KL, Nader E, Josset-Lamaugarny A, Charrin E, Martin C, Romanet-Faes C, Diaw M, Pialoux V, Fromy B (2019) Altered blood rheology and impaired pressure-induced cutaneous vasodilation in a mouse model of combined type 2 diabetes and sickle cell trait. Microvasc Res 122:111–116. https://doi.org/10.1016/j.mvr.2018.11.014
Skinner S, Liu KL, Lo M, Josset-Lamaugarny A, Charrin E, Martin C, Pialoux V, Fromy B, Connes P, Sigaudo-Roussel D (2020) Alterations in vascular reactivity in a transgenic mouse model of sickle cell trait. Br J Haematol 189(4):e154–e157. https://doi.org/10.1111/bjh.16577
Tripette J, Alexy T, Hardy-Dessources M-D, Mougenel D, Beltan E, Chalabi T, Chout R, Etienne-Julan M, Hue O, Meiselman HJ, Connes P (2009) Red blood cell aggregation, aggregate strength and oxygen transport potential of blood are abnormal in both homozygous sickle cell anemia and sickle-hemoglobin C disease. Haematologica 94(8):1060–1065. https://doi.org/10.3324/haematol.2008.005371
Tripette J, Connes P, Beltan E, Chalabi T, Marlin L, Chout R, Baskurt OK, Hue O, Hardy-Dessources M-D (2010a) Red blood cell deformability and aggregation, cell adhesion molecules, oxidative stress and nitric oxide markers after a short term, submaximal, exercise in sickle cell trait carriers. Clin Hemorheol Microcirc 45(1):39–52. https://doi.org/10.3233/CH-2010-1325
Tripette J, Loko G, Samb A, Gogh BD, Sewade E, Seck D, Hue O, Romana M, Diop S, Diaw M, Brudey K, Bogui P, Cissé F, Hardy-Dessources M-D, Connes P (2010b) Effects of hydration and dehydration on blood rheology in sickle cell trait carriers during exercise. Am J Physiol-Heart Circ Physiol 299(3):H908–H914. https://doi.org/10.1152/ajpheart.00298.2010
Vincent L, Féasson L, Oyono-Enguéllé S, Banimbek V, Denis C, Guarneri C, Aufradet E, Monchanin G, Martin C, Gozal D, Dohbobga M, Wouassi D, Garet M, Thiriet P, Messonnier L (2010) Remodeling of skeletal muscle microvasculature in sickle cell trait and alpha-thalassemia. Am J Physiol Heart Circ Physiol 298(2):375–384. https://doi.org/10.1152/ajpheart.00812.2009
Walløe L (2015) Arterio-venous anastomoses in the human skin and their role in temperature control. Temp Multidiscip Biomed J 3(1):92–103. https://doi.org/10.1080/23328940.2015.1088502
Wang Y, Branicky R, Noë A, Hekimi S (2018) Superoxide dismutases: Dual roles in controlling ROS damage and regulating ROS signaling. J Cell Biol 217(6):1915–1928. https://doi.org/10.1083/jcb.201708007
Witko-Sarsat V, Friedlander M, Capeillère-Blandin C et al (1996) Advanced oxidation protein products as a novel marker of oxidative stress in uremia. Kidney Int 49:1304–13. https://doi.org/10.1038/ki.1996.186
Zimmerman JL, Shen MC (2013) Rhabdomyolysis. Chest 144(3):1058–1065. https://doi.org/10.1378/chest.12-2016
Acknowledgements
We thank the participants, nurses (coordinated by Franceline Falla), and physicians (Patrick Chérubin, Nicolas Benoit) for their great involvement.
Funding
Funding for this work was provided by European Regional Development Fund & Région Guadeloupe 2015-FED-213.
Author information
Authors and Affiliations
Contributions
KR: formal analysis, investigation, methodology, writing– original draft, writing review & editing. ETNS: data curation, formal analysis, investigation, review & editing. MR: investigation, resources, writing-review & editing. PC: conceptualization, formal analysis, resources, writing – review & editing. SR: investigation, methodology. SH: investigation, methodology. OH: original draft, review & editing. MHD: investigation, methodology, writing – review & editing. SAJ: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, supervision, writing – original draft, writing – review & editing.
Corresponding author
Ethics declarations
Conflict interest
The author declares no financial or other conflict of interest that might bias this article.
Ethical approval
The participants were informed of the procedures and purposes of the study, which were in accordance with the institutional guidelines and the Helsinki Declaration of 2013 and was approved by the National Ethics Committee (CPP 17.10.10). This protocol described in this article is part of a larger project registered in EudraCT (TDEX: 2017-A02226-47) and Clinical Trials (NCT04028791).
Additional information
Communicated by Narihiko kondo.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reminy, K., Ngo Sock, E.T., Romana, M. et al. Strenuous exercise in warm environment is associated with improved microvascular function in sickle cell trait. Eur J Appl Physiol 122, 185–197 (2022). https://doi.org/10.1007/s00421-021-04821-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-021-04821-2