Abstract
Purpose
Long-term effects of exercise training are well studied. Acute hemodynamic responses to various training modalities, in particularly strength training (ST), have only been described in a few studies. This study examines the acute responses to ST, high-intensity interval training (HIIT) and moderate-intensity continuous training (MCT).
Methods
Twelve young male subjects (age 23.4 ± 2.6 years; BMI 23.7 ± 1.5 kg/m2) performed an incremental exertion test and were randomized into HIIT (4 × 4-min intervals), MCT (continuous cycling) and ST (five body-weight exercises) which were matched for training duration. The cardiopulmonary (impedance cardiography, ergo-spirometry) and metabolic response were monitored.
Results
Similar peak blood lactate responses were observed after HIIT and ST (8.5 ± 2.6 and 8.1 ± 1.2 mmol/l, respectively; p = 0.83). The training impact time was 90.7 ± 8.5% for HIIT and 68.2 ± 8.5% for MCT (p < 0.0001). The mean cardiac output was significantly higher for HIIT compared to that of MCT and ST (23.2 ± 4.1 vs. 20.9 ± 2.9 vs. 12.9 ± 2.9 l/min, respectively; p < 0.0001). VO2max was twofold higher during HIIT compared to that observed during ST (2529 ± 310 vs. 1290 ± 156 ml; p = 0.0004). Among the components of ST, squats compared with push-ups resulted in different heart rate (111 ± 13.5 vs. 125 ± 15.7 bpm, respectively; p < 0.05) and stroke volume (125 ± 23.3 vs. 104 ± 19.8 ml, respectively; p < 0.05).
Conclusions
Despite an equal training duration and a similar acute metabolic response, large differences with regard to the training impact time and the cardiopulmonary response give evident. HIIT and MCT, but less ST, induced a sufficient cardiopulmonary response, which is important for the preventive effects of training; however, large differences in intensity were apparent for ST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The preventive and rehabilitative effects of physical exercise are well studied, especially for endurance activities (Strasser et al. 2013; Haykowsky et al. 2013; Weston et al. 2014; Streckmann et al. 2014; Parmenter et al. 2015; Cornelis et al. 2016). The majority of the published intervention studies compare moderate-intensity continuous training (MCT) with high-intensity interval training (HIIT) (Smart et al. 2013; Milanović et al. 2015; Liou et al. 2016; Bækkerud et al. 2016; Cornelis et al. 2016; Green et al. 2017). These studies were mostly conducted as superiority trials with independent study groups to investigate long-term effects (VO2max). Cardiac parameters such as stroke volume (SV) or cardiac output (CO) were measured less frequently (Lepretre et al. 2004; Daussin et al. 2007, 2008; Cattadori et al. 2011; Gayda et al. 2012; Fu et al. 2013); therefore, the available information on different training modalities has been heterogeneous (Helgerud et al. 2007; Smart et al. 2013; Iellamo et al. 2013; Conraads et al. 2015; Fisher et al. 2015; Ramírez-Vélez et al. 2017). In addition to the methodological differences in physiological and metabolic parameters, this heterogeneity is probably also caused by the different intensities, durations and frequencies of the interventions. The current literature frequently does not describe the duration of the training in the given target range of intensity (training impact time).
Acute physiological reactions of the organism to various training modalities have been considered in several studies (Lepretre et al. 2004; Lamotte et al. 2010; Gayda et al. 2012; Chilton et al. 2014; Tschakert et al. 2015; Rozenek et al. 2016; Cipryan et al. 2017; Green et al. 2017), whereby the recorded parameters were concentrated on basic parameters (Chilton et al. 2014; Tschakert et al. 2015; Cipryan et al. 2017; Green et al. 2017). Hemodynamic parameters have so far only been analyzed during HIIT and MCT (Lepretre et al. 2004; Gayda et al. 2012), but not in comparison to ST.
In summary, a study comparing HIIT, MCT and ST with regard to acute cardiac parameters is lacking. Therefore, the aim of this randomized crossover study was to investigate acute cardiopulmonary and metabolic effects of HIIT, MCT and ST matched for exercise duration. Due to the known long-term effects of training interventions, the strongest cardiopulmonary responses should be expected for HIIT and the weakest for ST.
Methods
Subjects
The study was conducted in accordance with the latest revision of the Declaration of Helsinki and was approved by the Ethical Committee of the Medical Faculty, University of Leipzig (reference number 088/18-ek). Written informed consent was obtained from all participants. The study group consisted of 12 active and healthy males (Table 1). The exclusion criteria included cardiac, pulmonary or inflammatory diseases, sports inactivity or any other medical contraindications at the time of the examinations. Furthermore, the subjects had to be able to perform the strength exercises technically and conditionally.
Study design
The participants were tested four times in a 2-week period (pre-examination and three exercise interventions). The pre-examination included a medical history, questionnaire (sports activity, smoking, and alcohol consumption), height and weight measurement, an electrocardiogram (Cardiax, Mesa Medizintechnik GmbH, Germany), pulmonary function test (Easy on-PC, ndd Medizintechnik AG, Switzerland) and bioelectrical impedance analysis (bio-impedance analyzer STA/BIA, Akern, Italy). Subsequently, if all parameters were unremarkable, the participants performed an incremental exertion test (IET) until exhaustion to assess the maximal power output (Pmax) and cardiac and pulmonary maximum values.
Subsequently, all subjects had to perform the three exercise interventions (MCT, HIIT and ST) in a randomized order (block randomization) at the same time of the day.
The intensities of the interventions were selected according to the standard protocols for prevention and rehabilitation sports in the literature. The workload was based on the results of the Pmax and HRmax during the IET and matched for the exercise duration (25 min; excluding warm up and cool down). IET, HIIT and MCT were performed on a semi-recumbent ergometer (ergometrics 900, ergoline GmbH, Bitz, Germany) at a constant speed of 60–70 revolutions per minute. ST consisted of five different exercises that were executed on a sports mat on the floor.
Incremental exertion test (IET)
The test started at a workload of 50 W with an increment of 15 W each minute until volitional exhaustion occurred. Each subject continued for an additional 5-min recovery period at a workload of 25% of Pmax. Maximum values for power output (IET-Pmax) and HR (IET-HRmax) were used for load control of the subsequent sessions.
Moderate-intensity continuous training (MCT)
MCT was performed for 25 min at a continuous target workload equating to 70% IET-HRmax. This session started with a 5-min warm up at 50% IET-Pmax and finished with a 5-min cool-down phase at 25% IET-Pmax. In total, the MCT session lasted 35 min.
High-intensity interval training (HIIT)
The HIIT session started with a 5-min warm up at 50% IET-Pmax. Subsequently, four intervals of 4 min each (4 × 4 min) at 85–95% IET-HRmax were performed and separated by 3-min active resting periods at 25% IET-Pmax. The training session terminated with a 5-min cool down at 25% IET-Pmax. The total HIIT exercise time was 35 min.
Strength training (ST)
ST combined five different exercises that were performed using each subject’s own body weight. Each exercise consisted of five sets of 40 s of loading and a 20-s resting phase. Intensity was standardized over time per repetition of 3 s (time under tension). To support the subject, a clock was set at a frequency of 60 beats per minute (bpm). ST included squats (knee bends), push-ups, isometric back extension, isometric leg raise and inverted rows in that specific order. An individual warm-up was performed during ST before the attachment of the measuring electrodes. After the last set, subjects were requested to sit up slowly and sit on a chair until circulatory parameters returned to baseline.
Measurements
Cardiac output (CO), stroke volume (SV) (measured by impedance cardiography; Physioflow, Manatec Biomedical, Macheren, France), heart rate (HR) (Cardiax, MESA Medizintechnik GmbH, Benediktbeuern, Germany), maximum oxygen consumption (VO2max) and minute ventilation (VE) (K4b2, COSMED, Rome, Italy) were monitored continuously at rest, during training and after the training sessions. These values were collected continuously and averaged at 10-s intervals. Mean and peak values of HIIT, MCT and ST during the exercise (25 min excluding warm up and cool down) were calculated. Furthermore, all 10-s intervals of HR, CO, VE, VO2 and VCO2 were accumulated to compare absolute values of the whole sessions, including resting and loading periods.
The arteriovenous oxygen difference was computed using Fick’s principle with avDO2 = VO2/CO. Cardiac work (CW) was measured in Joules (J) and calculated according to the formula CW = SV × SBP. For better comparability of the pulmonary parameters, the VO2 of each training session was set in relation to the VO2max of IET and depicted as a percentage (%VO2max).
Blood lactate concentration (LAC), blood pressure (BP) and rating of perceived exertion (RPE; from 1 to 10, if 10 was total exhaustion) were observed at rest, at the end of each interval (HIIT), every 5 min during MCT and after each exercise (ST) as well as at 1, 3, and 5 min of recovery. During ST, the blood pressure measured during the rest periods (not under tension). Blood samples of 20 µl were taken from the earlobe and analyzed immediately via the enzymatic–amperometric method (Super GL, Dr. Müller Gerätebau GmbH, Freital, Germany).
Statistical analysis
All values are expressed as the means and standard deviation unless otherwise stated, and the significance level was defined as p < 0.05. Data were analyzed using Microsoft Office Excel® 2007 for Windows (Microsoft Corporation, Redmond, Washington, USA) and GraphPad Prism 7 for Windows, Version 7.04 (GraphPad Software Inc., California, USA). For distribution analysis, the D’Agostino–Pearson normality test was used. If normality distribution was evident, statistical comparisons were made using one-way repeated measures ANOVA with Turkey’s post hoc test for multiple comparisons. Otherwise, the Friedman non-parametric test and Dunn’s post hoc test were used for the comparison of the different training methods.
Results
Incremental exertion test
Maximum values of IET are shown in Table 2. The average duration of IET was 16.0 ± 2.8 min, and the subjects achieved an average Pmax of 276 ± 41.7 W, which corresponds to a relative power of 3.5 ± 0.4 W/kg.
Comparison of training interventions
The presentation of the three interventions in this study focused on the peak and cumulated values. For IIT and ST, a mean value does not reflect the adaptation-relevant stimuli.
Training impact time
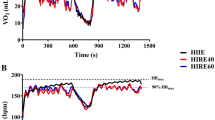
The HR during MCT and HIIT increased over time or in each interval, respectively (Fig. 1a). During MCT, the HR reached the target range (70% HRmax) after 139 ± 127 s and was maintained 90.7 ± 8.5% of the time (training impact time). During HIIT, the HR increased from interval to interval and was maintained for the following proportions of time: (first: 46.3 ± 22.6%; second: 68.9 ± 11.6%; third: 75.4 ± 8.5%; fourth: 82.2 ± 4.7%). During HIIT, within the 4 × 4-min intervals, the HR was maintained within the target range (85–95% HRmax) 68.2 ± 8.5% of the time. During ST, there was no defined HR target range.
Graphs show the mean cardiac responses (n = 12) to high-intensity interval training (HIIT), moderate-intensity continuous training (MCT) and strength training (ST) with warm-up and recovery periods. HR, heart rate (a); SV, stroke volume (b); CO, cardiac output (c); SBP and DBP, systolic and diastolic blood pressure (d). In ST the blood pressure measurements were taken during the 20-s resting phase. The values were surely higher during the time under tension
Cumulative values during the matched intervention periods
To compare the three training modalities, the parameters HR, CO, VE, VO2 and VCO2 were accumulated over the training duration (Table 3). Compared to ST, HIIT showed a significantly higher O2 consumption, cardiac output, breathing volume and heart rate. During the training sessions, MCT showed an intermediate response. Only for VCO2, no significant difference was observed between HIIT and MCT, although the VCO2 value for HIIT was highest.
Peak and mean values of the cardiopulmonary response
Baseline values were measured prior to each session (values are not shown), and there were no significant differences in hemodynamics. Figure 1 shows the time course of HR, CO, SV and CW across the three training types (HIIT, MCT and ST). The three training interventions showed large differences with regard to the peak cardiopulmonary response with the exception of DBP, HR and SV (Figs. 1, 2 and Table 2). There was no significant difference in peak SV between HIIT and MCT, and the ST value was significantly lower (Table 2). The mean SV during HIIT vs. MCT vs. ST was 155 ± 31 ml vs. 157 ± 22 ml vs. 109 ± 24 ml, respectively (p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.45). The mean CO during the interventions was significantly different for HIIT, MCT and ST (23.2 ± 4.1 l/min vs. 20.9 ± 2.9 l/min vs. 12.9 ± 2.9 l/min, respectively; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.65). The mean and peak HR were highest for HIIT. The peak HR was not different between MCT and ST (Table 2). On average, the HR in ST was 66.6% of HRmax (120 ± 13.7 bpm), in HIIT 83.3% (150 ± 9.8 bpm) and in MCT 73.8% (133 ± 8.3 bpm; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.59). The mean SBP was different (HIIT, MCT and ST: 185 ± 12.6 mmHg vs. 170 ± 16.5 mmHg vs. 150 ± 12.2 mmHg, respectively; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.53) and the mean DBP showed no differences (HIIT, MCT and ST: 73 ± 9.9 mmHg vs. 70 ± 9.3 mmHg vs. 74 ± 8.3 mmHg, respectively; p = 0.298; \(\eta_{\text{p}}^{2}\) = 0.03) during the exercise interventions.
The course of VE and VO2 is shown in Fig. 2, and the peak values are presented in Table 2. As with the hemodynamic parameters, the pulmonary values for HIIT were significantly highest for both the peak and mean values. With regard for only the mean value of VCO2 for HIIT compared to MCT, no significant difference could be found (mean VCO2: HIIT 2451 ± 361 ml vs. MCT 2002 ± 292 ml vs. ST 1330 ± 179 ml, respectively; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.74). MCT and ST differed in the mean values of the following parameters: mean VE: HIIT 76.2 ± 11.3 l/min vs. MCT 55.6 ± 8.1 l/min vs. ST 43.4 ± 5.9 l/min (p = 0.0001; \(\eta_{\text{p}}^{2}\) = 0.72); mean VO2: HIIT 2529 ± 310 ml vs. MCT 2189 ± 338 ml vs. ST 1290 ± 156 ml (p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.79) but not in the peak values (Table 2).
While the peak value of %VO2max for MCT (68.7 ± 9.4%) is only slightly above the mean (65.0 ± 5.4%), during HIIT the subjects averaged 98.0 ± 10.0% of the peak value and 75.4 ± 7.3% of the mean value for the entire session. For ST, both the mean (38.5 ± 3.9%) and peak values (56.5 ± 11.8%) were the lowest.
Blood lactate concentration, arteriovenous difference of oxygen, rating of perceived exertion
The LAC steady state was reached for MCT but not for HIIT and ST (Fig. 3a). The comparison of the three training sessions showed a significant difference across all mean values (mean LAC: HIIT 7.4 ± 2.3 mmol/l vs. MCT 2.5 ± 1.2 mmol/l vs. ST 5.7 ± 0.7 mmol/l, respectively; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.65). The peak values of HIIT and ST were almost equal and significantly higher than that for MCT (Table 2).
Mean performance curves (n = 12) for lactic acid, and rating of perceived exertion during high-intensity interval training (HIIT), moderate-intensity continuous training (MCT) and strength training (ST) with warm-up and recovery periods. LAC blood lactate concentration (a); RPE rating of perceived exertion (b)
No significant difference in avDO2 could be found, except at the peak values for ST and MCT (avDO2 for ST was significantly higher than that for MCT; Table 2). The mean for avDO2 was 11.1 ± 1.8 ml/dl for HIIT, 10.5 ± 1.2 ml/dl for MCT and 10.3 ± 2.2 ml/dl for ST (p = 0.3387: \(\eta_{\text{p}}^{2}\) = 0.03) for ST. While the peak values of RPE are significantly different from each other, the mean values only differ between HIIT and MCT/ST (mean RPE: HIIT 6.1 ± 0.9 vs. MCT 4.8 ± 1.2 vs. ST 5.1 ± 1.1, respectively; p = 0.0068; \(\eta_{\text{p}}^{2}\) = 0.23). Figure 3b shows the course of the RPE.
Comparison of the strength training exercises
The cardiopulmonary and metabolic parameters are shown in Fig. 4. Overall, large differences become apparent. The highest SV was reached during squats; however, the lowest HR and LAC were measured during this exercise. The CO showed less differences (squats: 13.8 ± 2.5 l/min; push-ups: 12.9 ± 2.7 l/min; isometric back extension: 12.6 ± 4.1 l/min; isometric leg raise: 11.7 ± 3.2 l/min; inverted rows: 13.4 ± 2.9 l/min, respectively; p = 0.007; \(\eta_{\text{p}}^{2}\) = 0.05). The calculated avDO2 was highest during IR and lowest for isometric exercises (squats: 10.3 ± 2.4 ml/dl; push-ups: 11.3 ± 2.3 ml/dl; isometric back extension: 8.6 ± 2.1 ml/dl; isometric leg raise: 9.7 ± 2.5 ml/dl; inverted rows: 12.1 ± 2.5 ml/dl, respectively; p = 0.007; \(\eta_{\text{p}}^{2}\) = 0.22).
Graphs show the mean values of strength training exercises (n = 12; loading and resting phases). Squats (S), Push-ups (PU), Isometric back extension (IBE), Isometric leg raise (ILR) and Inverted rows (IR). HR, heart rate (a; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.26); SV stroke volume (b; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.11); VO2 oxygen uptake (c; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.82); LAC blood lactate concentration (d; p < 0.0001; \(\eta_{\text{p}}^{2}\) = 0.11). Post hoc tests: * (p < 0.05)
Discussion
The main finding of this randomized crossover study was that high-intensity interval training and moderate-intensity continuous training exert greater acute cardiopulmonary effects compared to that of ST. In addition, the specific hemodynamic responses to various body-weight ST exercises are described for the first time. Despite the same training time, the mean intensity factors, such as the mean power output (Table 2), show differences between the interventions. The different physiological response is, of course, also due to this.
Training impact time (proportion of time at the target intensity)
Comparing the results of training studies is difficult, because the intensity, intervals and duration of the training sessions often differ significantly (Haykowsky et al. 2013; Cornelis et al. 2016). Furthermore, there is usually no information about how long the subjects actually stayed in the targeted HR range (training impact time), which is key information, since training effects change with duration and intensity of an exercise (Wenger and Bell 1986). In this study, subjects needed approximately 140 s to adjust the cardiac load during HIIT and MCT. For MCT, subjects spent approximately 90% of the exercise duration in the training impact zone; whereas for HIIT, they spent 68% of the exercise duration in the training impact zone. It can be assumed that a high value of the training impact time also results in an improved realization of the desired training target. Also in ST there could be the possibility to determine the training impact time. Here, the training impact time corresponds to the accumulated time under tension in the defined intensity (percentage of the maximum repetition of 1 repetition). Further research is needed to assess the training impact time as a factor of training effectiveness. Nevertheless, the reporting of the training impact time could be facilitated the comparison of training effects from different studies in addition to common intensity parameters.
Hemodynamic response in HIIT and MCT
There was no difference in the acute response of SV between HIIT and MCT with significantly higher blood pressure in HIIT, which resulted in a higher cardiac work load. In addition, a higher intensity with correspondingly higher HR causes a higher CO in HIIT compared to that in MCT. Therefore, studies suggest that in particular, HIIT significantly improved left ventricular ejection fraction and left ventricular end-diastolic diameter (Wisløff et al. 2007; Daussin et al. 2007; Weston et al. 2014; Bækkerud et al. 2016; Cornelis et al. 2016) which, in turn, leads to an improved pumping function of the heart. These improvements seemed to occur less with MCT than HIIT. (Weston et al. 2014; Cornelis et al. 2016; Karlsen et al. 2017). Nevertheless, the training‐induced increase in VO2max is not exclusively due to improved contractility of the heart muscle, but seems to be significantly supported by an enlargement of the blood volume, which is associated with a higher venous return (Montero et al. 2015; Lundby et al. 2017). The increase in exercise-induced hypervolemia and CO due to exercise seems to depend on the baseline level of the aerobic capacity (Astorino et al. 2017).
Hemodynamic response in ST
During ST, lower values of SV and SBP were shown compared to that of the endurance methods. It should be noted that the blood pressure measurements were taken during the 20-s resting phase. The blood pressure would have been considerably higher during the exercise phase (Taylor et al. 2017). In summary, the intensity of the strength training exercises performed in this study does not seem to be sufficient to achieve chronic left ventricular adaptions (Wenger and Bell 1986; Fagard 1997; Spence et al. 2011). A recently published study investigating acute and long-term responses to HIIT, MCT and ST demonstrated that the endurance methods, but not ST, are important for cellular aging processes (Werner et al. 2018). Nevertheless, resistance training can lead to improved clinical outcomes in heart failure patients (Jewiss et al. 2016), and the combination of endurance training and ST seems to cause higher modifications (Vincent et al. 2002; Currie et al. 2015; Jewiss et al. 2016).
Furthermore, large differences in the SV and HR values were observed for the different strength exercises (Fig. 3). In particular, the SV for squats (knee bends) reached comparable values to that for HIIT. Dynamic exercise with large muscle groups generated significantly higher SV by an increased venous return (Laughlin 1999) in comparison to that generated during exercises with high isometric components. Due to ST based on the HIIT principle of Tabata et al. (1996), an intensity of 86% of maximum HR could be achieved (Emberts et al. 2013). Isometric exercise seems to be associated with a reduction in SV (Taylor et al. 2017) due to an increased acute left ventricular afterload and intrathoracic pressure (Weiner et al. 2012), which is also reflected in these results. Therefore, dynamic strength exercises of high intensity (additional load, large muscle groups) could probably cause cardiopulmonary adaptations.
Pulmonary response
HIIT achieved the highest values in the pulmonary parameters. The peak values were even 98.0% of the VO2max achieved during IET, and thus significantly higher than that in MCT and ST. Thereby, compared to MCT, HIIT showed a higher improvement in inspiratory muscular strength (Dunham and Harms 2012), which is similar to that observed from inspiratory muscle training (Karsten et al. 2018). In contrast, the expiratory lung function parameters (forced vital capacity, forced expiratory volume in 1 s) seem to be hardly influenced by endurance training (Dunham and Harms 2012; Chlif et al. 2017). Thus, the heterogeneous assessment of the increase in aerobic capacity observed in MCT and HIIT (Wisløff et al. 2007; Smart and Steele 2012; Freyssin et al. 2012; Fu et al. 2013; Iellamo et al. 2013; Bækkerud et al. 2016) seems to be only slightly affected by pulmonary adaptations. ST showed only minor or no improvements in lung function (Strasser et al. 2013; Liao et al. 2015). In the present study, the significantly lower acute response of ST compared to endurance training also suggests this outcome. Cardiopulmonary adaptations due to exercise are mainly determined by training intensity (Ismail et al. 2013; Scribbans et al. 2016; Ostman et al. 2017). Therefore, different exercise intensities of the applied interventions might very likely be the cause of the varying outcomes.
Peripheral and metabolic responses
The avDO2 was calculated from the CO and VO2max using the Fick principle. The peak avDO2 tended to be highest in ST. Enhanced metabolism, represented by a high avDO2, is a physiological factor that is involved in exercise-induced angiogenesis via VEGF in addition to the increased blood flow, shear stress and mechanical stretch (Gustafsson et al. 1999; Egginton 2009; Hoier and Hellsten 2014). Recent studies have also shown an increase in the capillary–fiber ratio as a result of angiogenesis and hypertrophy due to resistance training (Verdijk et al. 2016; Holloway et al. 2018). The high peak values of avDO2 and LAC concentration during ST in this study are in agreement with these results. During endurance exercise, the mitochondrial biogenesis is also stimulated intracellularly via PGX-1a (Olesen et al. 2010). LAC stimulates angiogenesis due to an increase in endothelial growth factor (Constant et al. 2000; Ferguson et al. 2018) and endothelial cell migration (Beckert et al. 2006). Furthermore, an increase in vasculogenesis from the stimulation of vasculogenic stem cells and elevations in HIF 1 levels (Milovanova et al. 2008) has been proven. There are indications that anaerobic training provokes better adaptations (vascular and mitochondrial) due to a significantly higher stem cell concentration (CD34+) and higher PGX-1a values than aerobic training (Shalaby et al. 2012; MacInnis et al. 2017; MacInnis and Gibala 2017). The higher LAC concentration in HIIT and ST could, therefore, be the trigger for stronger peripheral adaptations compared to that in MCT.
Limitations of the study
The sample size is small, and only male participants were enrolled; therefore, the interpretability and generalizability of the results are limited. However, this trial is the largest randomized crossover study performed to date regarding the acute hemodynamic responses in HIIT, MCT and ST. The difficulty of the investigation was the measurement of the hemodynamic parameters during strength training. Body movements and changes in position caused cable artifacts. We could reduce the artifacts using a compression shirt over the fixed electrodes and choosing only body-weight exercises. Minor differences in the training intensity were possible, but they were inherent to the respective exercises. Cardiac parameters obtained by impedance cardiography may be overestimated using absolute values (Siebenmann et al. 2015). However, since the intra-individual differences were compared, changes in these parameters were crucial compared to that achieved using the absolute values. In previous studies, thoracic impedance cardiography was also used to detect intra-individual changes in SV and CO (Lepretre et al. 2004; Daussin et al. 2007; Astorino et al. 2017). The different lactate values during the strength exercises may also be due to the order of the exercises and the associated accumulation effects.
Conclusions
This randomized crossover study examined for the first time the acute hemodynamic response of ST and two standard endurance training methods using equal training durations. HIIT and ST showed the same level of acute metabolic (blood lactate concentration) response. However, large differences with regard to the cardiopulmonary response between the training methods and the strength training exercises were observed. Additionally, the proportion of time in the intensity range during the endurance training showed large differences. In future studies, the information of the training impact time could enable a better comparability of training studies.
The evidenced chronic central and peripheral adaptations of endurance training and ST seem predominantly associated with these acute physiological reactions. In particular, the hematological changes caused by endurance training, which are likely to trigger the increase in cardiac output and the role of an enhanced metabolic response to preventive effects through ST, warrant further investigation.
References
Astorino TA, Edmunds RM, Clark A, King L, Gallant RA, Namm S, Fischer A, Wood KM (2017). High-intensity interval training increases cardiac output and \(\dot{V}{\text{O}}_{2\hbox{max} }\). Med Sci Sports Exerc 49:265–273
Bækkerud FH, Solberg F, Leinan IM, Wisløff U, Karlsen T, Rognmo Ø (2016) Comparison of three popular exercise modalities on \(\dot{V}{\text{O}}_{2\hbox{max} }\) in overweight and obese. Med Sci Sports Exerc 48:491–498
Beckert S, Farrahi F, Aslam RS, Scheuenstuhl H, Königsrainer A, Hussain MZ, Hunt TK (2006) Lactate stimulates endothelial cell migration. Wound Repair 14:321–324
Cattadori G, Schmid J-P, Brugger N, Gondoni E, Palermo P, Agostoni P (2011) Hemodynamic effects of exercise training in heart failure. J Card Fail 17:916–922
Chilton WL, Marques FZ, West J, Kannourakis G, Berzins SP, O’Brien BJ, Charchar FJ (2014) Acute exercise leads to regulation of telomere-associated genes and microRNA expression in immune cells. PLoS One 9:e92088
Chlif M, Chaouachi A, Ahmaidi S (2017) Effect of aerobic exercise training on ventilatory efficiency and respiratory drive in obese subjects. Respir Care 62:936–946
Cipryan L, Tschakert G, Hofmann P (2017) Acute and post-exercise physiological responses to high-intensity interval training in endurance and sprint athletes. J Sports Sci Med 16:219–229
Conraads VM, Pattyn N, De Maeyer C, Beckers PJ, Coeckelberghs E, Cornelissen VA, Denollet J, Frederix G, Goetschalckx K, Hoymans VY, Possemiers N, Schepers D, Shivalkar B, Voigt J-U, Van Craenenbroeck EM, Vanhees L (2015) Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int J Cardiol 179:203–210
Constant JS, Feng JJ, Zabel DD, Yuan H, Suh DY, Scheuenstuhl H, Hunt TK, Hussain MZ (2000) Lactate elicits vascular endothelial growth factor from macrophages: a possible alternative to hypoxia. Wound Repair 8:353–360
Cornelis J, Beckers P, Taeymans J, Vrints C, Vissers D (2016) Comparing exercise training modalities in heart failure: a systematic review and meta-analysis. Int J Cardiol 221:867–876
Currie KD, Bailey KJ, Jung ME, McKelvie RS, MacDonald MJ (2015) Effects of resistance training combined with moderate-intensity endurance or low-volume high-intensity interval exercise on cardiovascular risk factors in patients with coronary artery disease. J Sci Med Sport 18:637–642
Daussin FN, Ponsot E, Dufour SP, Lonsdorfer-Wolf E, Doutreleau S, Geny B, Piquard F, Richard R (2007) Improvement of VO2max, by cardiac output and oxygen extraction adaptation during intermittent versus continuous endurance training. Eur J Appl Physiol 101:377–383
Daussin FN, Zoll J, Dufour SP, Ponsot E, Lonsdorfer-Wolf E, Doutreleau S, Mettauer B, Piquard F, Geny B, Richard R (2008) Effect of interval versus continuous training on cardiorespiratory and mitochondrial functions: relationship to aerobic performance improvements in sedentary subjects. Am J Physiol Regul Integr Comp Physiol 295:R264–R272
Dunham C, Harms CA (2012) Effects of high-intensity interval training on pulmonary function. Eur J Appl Physiol 112:3061–3068
Egginton S (2009) Invited review: activity-induced angiogenesis. Pflugers Arch 457:963–977
Emberts T, Porcari J, Dobers-tein S, Steffen J, Foster C (2013) Exercise intensity and energy expenditure of a Tabata workout. J Sports Sci Med 12:612–613
Fagard RH (1997) Impact of different sports and training on cardiac structure and function. Cardiol Clin 15:397–412
Ferguson BS, Rogatzki MJ, Goodwin ML, Kane DA, Rightmire Z, Gladden LB (2018) Lactate metabolism: historical context, prior misinterpretations, and current understanding. Eur J Appl Physiol 118:691–728
Fisher G, Brown AW, Brown MMB, Alcorn A, Noles C, Winwood L, Resuehr H, George B, Jeansonne MM, Allison DB (2015) High intensity interval- vs moderate intensity- training for improving cardiometabolic health in overweight or obese males: a randomized controlled trial. PLoS One 10:e0138853
Freyssin C, Verkindt C, Prieur F, Benaich P, Maunier S, Blanc P (2012) Cardiac rehabilitation in chronic heart failure: effect of an 8-week, high-intensity interval training versus continuous training. Arch Phys Med Rehabil 93:1359–1364
Fu T, Wang C-H, Lin P-S, Hsu C-C, Cherng W-J, Huang S-C, Liu M-H, Chiang C-L, Wang J-S (2013) Aerobic interval training improves oxygen uptake efficiency by enhancing cerebral and muscular hemodynamics in patients with heart failure. Int J Cardiol 167:41–50
Gayda M, Normandin E, Meyer P, Juneau M, Haykowsky M, Nigam A (2012) Central hemodynamic responses during acute high-intensity interval exercise and moderate continuous exercise in patients with heart failure. Appl Physiol Nutr Metab 37:1171–1178
Green N, Wertz T, Laporta Z, Mora A, Serbas J, Astorino TA (2017) Comparison of acute physiological and psychological responses between moderate intensity continuous exercise and three regimes of high intensity training. J Strength Cond Res. https://doi.org/10.1519/jsc.0000000000002154
Gustafsson T, Puntschart A, Kaijser L, Jansson E, Sundberg CJ (1999) Exercise-induced expression of angiogenesis-related transcription and growth factors in human skeletal muscle. Am J Physiol 276:H679–H685
Haykowsky MJ, Timmons MP, Kruger C, McNeely M, Taylor DA, Clark AM (2013) Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol 111:1466–1469
Helgerud J, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, Hoff J (2007). Aerobic high-intensity intervals improve \(\dot{V}{\text{O}}_{2\hbox{max} }\) more than moderate training: Med Sci Sports Exerc 39:665–671
Hoier B, Hellsten Y (2014) Exercise-induced capillary growth in human skeletal muscle and the dynamics of VEGF. Microcirc N Y N 1994(21):301–314
Holloway TM, Snijders T, van Kranenburg J, Van Loon LJC, Verdijk LB (2018) Temporal response of angiogenesis and hypertrophy to resistance training in young men. Med Sci Sports Exerc 50:36–45
Iellamo F, Manzi V, Caminiti G, Vitale C, Castagna C, Massaro M, Franchini A, Rosano G, Volterrani M (2013) Matched dose interval and continuous exercise training induce similar cardiorespiratory and metabolic adaptations in patients with heart failure. Int J Cardiol 167:2561–2565
Ismail H, McFarlane JR, Nojoumian AH, Dieberg G, Smart NA (2013) Clinical outcomes and cardiovascular responses to different exercise training intensities in patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail 1:514–522
Jewiss D, Ostman C, Smart NA (2016) The effect of resistance training on clinical outcomes in heart failure: a systematic review and meta-analysis. Int J Cardiol 221:674–681
Karlsen T, Aamot I-L, Haykowsky M, Rognmo Ø (2017) High intensity interval training for maximizing health outcomes. Prog Cardiovasc Dis 60:67–77
Karsten M, Ribeiro GS, Esquivel MS, Matte DL (2018) The effects of inspiratory muscle training with linear workload devices on the sports performance and cardiopulmonary function of athletes: a systematic review and meta-analysis. Phys Ther 34:92–104
Lamotte M, Fleury F, Pirard M, Jamon A, van de Borne P (2010) Acute cardiovascular response to resistance training during cardiac rehabilitation: effect of repetition speed and rest periods. Eur J Cardiovasc Prev 17:329–336
Laughlin MH (1999) Cardiovascular response to exercise. Adv Physiol Educ 277:S244
Lepretre P, Koralsztein J, Billat VL (2004) Effect of exercise intensity on relationship between \(\dot{V}{\text{O}}_{2\hbox{max} }\) and cardiac output. Med Sci Sports Exerc 36:1357–1363
Liao W-H, Chen J-W, Chen X, Lin L, Yan H-Y, Zhou Y-Q, Chen R (2015) Impact of resistance training in subjects with COPD: a systematic review and meta-analysis. Respir Care 60:1130–1145
Liou K, Ho S, Fildes J, Ooi S-Y (2016) High intensity interval versus moderate intensity continuous training in patients with coronary artery disease: a meta-analysis of physiological and clinical parameters. Heart Lung Circ 25:166–174
Lundby C, Montero D, Joyner M (2017) Biology of VO2max: looking under the physiology lamp. Acta Physiol Oxf Engl 220:218–228
MacInnis MJ, Gibala MJ (2017) Physiological adaptations to interval training and the role of exercise intensity. J Physiol 595:2915–2930
MacInnis MJ, Zacharewicz E, Martin BJ, Haikalis ME, Skelly LE, Tarnopolsky MA, Murphy RM, Gibala MJ (2017) Superior mitochondrial adaptations in human skeletal muscle after interval compared to continuous single-leg cycling matched for total work. J Physiol 595:2955–2968
Milanović Z, Sporiš G, Weston M (2015) Effectiveness of high-intensity interval training (HIT) and continuous endurance training for VO2max improvements: a systematic review and meta-analysis of controlled trials. Sports Med Auckl NZ 45:1469–1481
Milovanova TN, Bhopale VM, Sorokina EM, Moore JS, Hunt TK, Hauer-Jensen M, Velazquez OC, Thom SR (2008) Lactate stimulates vasculogenic stem cells via the thioredoxin system and engages an autocrine activation loop involving hypoxia-inducible factor 1. Mol Cell Biol 28:6248–6261
Montero D, Cathomen A, Jacobs RA, Flück D, de Leur J, Keiser S, Bonne T, Kirk N, Lundby A-K, Lundby C (2015) Haematological rather than skeletal muscle adaptations contribute to the increase in peak oxygen uptake induced by moderate endurance training. J Physiol 593:4677–4688
Olesen J, Kiilerich K, Pilegaard H (2010) PGC-1alpha-mediated adaptations in skeletal muscle. Pflugers Arch 460:153–162
Ostman C, Jewiss D, Smart NA (2017) The effect of exercise training intensity on quality of life in heart failure patients: a systematic review and meta-analysis. Cardiology 136:79–89
Parmenter BJ, Dieberg G, Smart NA (2015) Exercise training for management of peripheral arterial disease: a systematic review and meta-analysis. Sports Med 45:231–244
Ramírez-Vélez R, Tordecilla-Sanders A, Téllez-T LA, Camelo-Prieto D, Hernández-Quiñonez PA, Correa-Bautista JE, Garcia-Hermoso A, Ramirez-Campillo R, Izquierdo M (2017) Similar cardiometabolic effects of high- and moderate-intensity training among apparently healthy inactive adults: a randomized clinical trial. J Transl Med 15:118
Rozenek R, Salassi JW, Pinto NM, Fleming JD (2016) Acute cardiopulmonary and metabolic responses to high-intensity interval training protocols using 60 s of work and 60 s recovery. J Strength Cond Res 30:3014–3023
Scribbans TD, Vecsey S, Hankinson PB, Foster WS, Gurd BJ (2016) The effect of training intensity on VO2max in young healthy adults: a meta-regression and meta-analysis. Int J Exerc Sci 9:230–247
Shalaby MN, Saad M, Akar S, Reda MAA, Shalgham A (2012) The role of aerobic and anaerobic training programs on CD(34 +) stem cells and chosen physiological variables. J Hum Kinet 35:69–79
Siebenmann C, Rasmussen P, Sørensen H, Zaar M, Hvidtfeldt M, Pichon A, Secher NH, Lundby C (2015) Cardiac output during exercise: a comparison of four methods. Scand J Med Sci Sports 25:e20–e27
Smart NA, Steele M (2012) A comparison of 16 weeks of continuous vs intermittent exercise training in chronic heart failure patients. Congest Heart Fail 18:205–211
Smart NA, Dieberg G, Giallauria F (2013) Intermittent versus continuous exercise training in chronic heart failure: a meta-analysis. Int J Cardiol 166:352–358
Spence AL, Naylor LH, Carter HH, Buck CL, Dembo L, Murray CP, Watson P, Oxborough D, George KP, Green DJ (2011) A prospective randomised longitudinal MRI study of left ventricular adaptation to endurance and resistance exercise training in humans. J Physiol 589:5443–5452
Strasser B, Siebert U, Schobersberger W (2013) Effects of resistance training on respiratory function in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Sleep Breath 17:217–226
Streckmann F, Zopf EM, Lehmann HC, May K, Rizza J, Zimmer P, Gollhofer A, Bloch W, Baumann FT (2014) Exercise intervention studies in patients with peripheral neuropathy: a systematic review. Sports Med 44:1289–1304
Tabata I, Nishimura K, Kouzaki M, Hirai Y, Ogita F, Miyachi M, Yamamoto K (1996) Effects of moderate-intensity endurance and high-intensity intermittent training on anaerobic capacity and VO2max. Med Sci Sports Exerc 28:1327–1330
Taylor KA, Wiles JD, Coleman DD, Sharma R, Oʼdriscoll JM (2017) Continuous cardiac autonomic and hemodynamic responses to isometric exercise. Med Sci Sports Exerc 49:1511–1519
Tschakert G, Kroepfl J, Mueller A, Moser O, Groeschl W, Hofmann P (2015) How to regulate the acute physiological response to “aerobic” high-intensity interval exercise. J Sports Sci Med 14:29–36
Verdijk LB, Snijders T, Holloway TM, van Kranenburg J, van Loon LJC (2016) Resistance training increases skeletal muscle capillarization in healthy older men. Med Sci Sports Exerc 48:2157–2164
Vincent KR, Braith RW, Feldman RA, Kallas HE, Lowenthal DT (2002) Improved cardiorespiratory endurance following 6 months of resistance exercise in elderly men and women. Arch Intern Med 162:673–678
Weiner RB, Weyman AE, Kim JH, Wang TJ, Picard MH, Baggish AL (2012) The impact of isometric handgrip testing on left ventricular twist mechanics. J Physiol 590:5141–5150
Wenger HA, Bell GJ (1986) The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Med 3:346–356
Werner CM, Hecksteden A, Morsch A, Zundler J, Wegmann M, Kratzsch J, Thiery J, Hohl M, Bittenbring JT, Neumann F, Böhm M, Meyer T, Laufs U (2018) Differential effects of endurance, interval, and resistance training on telomerase activity and telomere length in a randomized, controlled study. Eur Heart J. 10:10. https://doi.org/10.1093/eurheartj/ehy585
Weston KS, Wisløff U, Coombes JS (2014) High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med 48:1227–1234
Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, Tjønna AE, Helgerud J, Slørdahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen Ø, Skjærpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115:3086–3094
Funding
None declared.
Author information
Authors and Affiliations
Contributions
RF and SF conceived and designed research. RF and RH conducted experiments and analyzed the data. RF wrote the manuscript. SF designed and drafted and critically revised the manuscript. SF, RH, UL, KF and MB read, approved and critical revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Additional information
Communicated by Keith Phillip George.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Falz, R., Fikenzer, S., Holzer, R. et al. Acute cardiopulmonary responses to strength training, high-intensity interval training and moderate-intensity continuous training. Eur J Appl Physiol 119, 1513–1523 (2019). https://doi.org/10.1007/s00421-019-04138-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04138-1