Abstract
Aim
The inter-relationships between mean body and local skin temperatures have previously been established for controlling hand and foot blood flows. Since glabrous skin contains many arteriovenous anastomoses, it was important to repeat those experiments on non-glabrous regions using the same sample and experimental conditions.
Methods
Mild hypothermia (mean body temperature 31.4 °C), normothermia (control: 36.0 °C) and moderate hyperthermia (38.3 °C) were induced and clamped (climate chamber and water-perfusion garment) in eight males. Within each condition, five localised thermal treatments (5, 15, 25, 33, 40 °C) were applied to the left forearm and right calf. Steady-state forearm and calf blood flows were measured (venous occlusion plethysmography) for each of the resulting 15 combinations of clamped mean body and local skin temperatures.
Results
Under the normothermic clamp, cutaneous blood flows averaged 4.2 mL 100 mL−1 min−1 (±0.28: forearm) and 5.4 mL 100 mL−1 min−1 (±0.27: calf). When mildly hypothermic, these segments were unresponsive to localised thermal stimuli, but tracked those changes when normothermic and moderately hyperthermic. For deep-body (oesophageal) temperature elevations, forearm blood flow increased by 5.1 mL 100 mL−1 min−1 °C−1 (±0.9) relative to normothermia, while the calf was much less responsive: 3.3 mL 100 mL−1 min−1 °C−1 (±1.5). Three-dimensional surfaces revealed a qualitative divergence in the control of calf blood flow, with vasoconstrictor tone apparently being released more gradually.
Conclusion
These descriptions reinforce the importance of deep-tissue temperatures in controlling cutaneous perfusion, with this modulation being non-linear at the forearm and appearing linear for the calf.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When the thermal status of the body moves away from thermoneutrality, the first autonomic defence is a modification of the convective delivery of heat to the skin surface via the manipulation of cutaneous blood flow (Werner et al. 2008). During such states, tissue temperatures within several thermoreceptive fields are simultaneously changing and, in these circumstances, feedback from the deep-body (core) sensors more powerfully modulates cutaneous blood flow (Wyss et al. 1974; Proppe et al. 1976; Werner et al. 2008; Jessen 2011). However, the impact of cutaneous temperature changes is also important (Werner et al. 2008; Jessen 2011; Romanovsky 2014). This is because rapid variations in peripheral thermal feedback can elicit immediate and pronounced autonomic responses (Brown and Brengelmann 1970; Nadel et al. 1971; Libert et al. 1978; Tipton 1989), particularly when the central thermal status is relatively stable. Indeed, this peripheral feedback can also be important during thermal adaptation (Regan et al. 1996; Tipton et al. 2013; Taylor 2014). Furthermore, both the cutaneous arterioles and venules respond to localised temperature variations (Taylor et al. 1984; Pérgola et al. 1993; Johnson et al. 2014), although the extent of those localised influences is determined by the status of the background sympathetic tone, which is itself largely dictated by the deep-body thermal status (Spealman 1945; Pérgola et al. 1993; Caldwell et al. 2014). Thus, variations in instantaneous cutaneous blood flow result from a complex interaction of whole body and local thermal influences, and those interactions were explored in this project with respect to the forearm and calf.
The hands and feet are particularly well suited to modifying local heat exchanges (Caldwell et al. 2014), and can fulfil prominent thermoregulatory roles, not just as dry heat exchangers, but as physiological evaporators (Taylor et al. 2006, 2014a; Machado-Moreira et al. 2008). Nevertheless, the glabrous (non-hairy) skin of those regions is uniquely endowed with arteriovenous anastomoses (Clark 1938; Nagasaka et al. 1987; Elstad et al. 2014) that can dramatically alter local blood flow (Molyneux and Bryden 1981; Hales 1985). Therefore, whilst the inter-relationship between mean body and local skin temperatures in the control of hand and foot blood flows has recently been described (Caldwell et al. 2014), it was important to repeat those experiments, emphasising skin in which these anastomoses were lacking (i.e. non-glabrous skin), and this was the focus of the current experiment. However, we must also understand that these limb segments differ not just in the nature of the overlying skin, but within their underlying anatomical structures (e.g. bone and muscle masses and vasculature) and morphological configurations.
In this study, segmental blood flows of the forearm and calf were mapped over a wide range of clamped mean body and local skin temperatures, following the methods of Caldwell et al. (2014). This was performed using purpose-built, water-filled, displacement plethysmographs (Caldwell and Taylor 2014) that permitted simultaneous thermal clamping and segmental blood flow measurements. It was anticipated that mean body temperature changes would again dominate the control of local blood flow, although it was now expected that less extreme blood flow changes would occur at these non-glabrous sites than were observed at the hands and feet of the same population sample, studied under identical experimental conditions (Caldwell et al. 2014).
Methods
Details of the methods for thermally stimulating and clamping discrete skin regions, along with the simultaneous measurement of segmental blood flow, have been reported elsewhere (Caldwell et al. 2014; Caldwell and Taylor 2014). Herein, data pertaining to the thermal modulation of cutaneous blood flow of the human forearm and calf under these same experimental conditions are reported. Accordingly, only the novel methods are described in detail, whilst the other methods are presented in summary form.
Subjects
Eight males participated in three trials following the provision of written, informed consent. All were asymptomatic, physically active non-smokers [25.4 years (standard deviation (SD) 6.4), mass 74.5 kg (SD 8.7), height 1.71 m (SD 0.04)]. Procedures were approved by the Human Research Ethics Committee (University of Wollongong) in accordance with the regulations of the National Health and Medical Research Council (Australia), and in compliance with the Declaration of Helsinki.
Procedural overview
This experiment was based on a repeated-measures design, with participants (dressed only in swimming costumes) acting as their own controls and completing three different trials. Subjects were kept in a supine posture throughout all phases of this experiment, and every trial commenced with a subject status check and preliminary set-up (~40 min), including the donning of a water-perfusion garment. This was followed by a pre-treatment water immersion in one of three temperatures (15, 34, 39 °C; ~45 min), transfer to a climate-regulated chamber and final instrumentation (~15 min). The purpose of these water immersions was to elicit three whole-body thermal states that would then be clamped throughout the experiment, whilst standardising the possible hydrostatic influences on the intravascular fluid volume (Stocks et al. 2004) that may be elicited by this pre-treatment. Accordingly, subjects were removed from the water at the following oesophageal temperatures: 35.4 °C (SD 0.38), 37.0 °C (SD 0.27) or 39.2 °C (SD 0.13). To prevent transient changes in thermal state, participants were immediately covered with cold or warm towels, which permitted partial skin drying, and the perfusion suit was briefly supplied with either cold (10 °C), thermoneutral (34 °C) or hot water (48 °C). These strategies were used to sustain the central thermal state during horizontal movement (gurney) into a pre-conditioned climate chamber. The experimental phase then commenced in which local skin temperature treatments were applied (~180 min), whilst the chamber set to one of three states: 15 °C (20 % relative humidity), 28 °C (40 % relative humidity) or 38 °C (40 % relative humidity). During these treatments (supine), the perfusion suit was now supplied with water at either 15°, 34° or 48 °C. These combinations of the pre-experimental water immersion temperature, chamber air temperature and perfused water temperature facilitated deep-body, mean skin and mean body temperature clamping throughout experimentation in each of three targeted states: mild hypothermia, normothermia (control) and moderate hyperthermia.
Left forearm and right calf blood flows were measured using bespoke water-displacement plethysmographs (Fig. 1; Caldwell and Taylor 2014). These two-compartment instruments permitted independent and rapid cooling or heating, followed by thermal clamping of the target limb segment. Five local treatment temperatures were used (15 min each) in one of two sequences: 5, 15, 25, 33 and 40 or 40, 33, 25, 15 and 5 °C. Treatments were alternated between the forearm and calf, with consecutive treatments of the same segment not occurring within 30 min. Therefore, across these trials, segmental blood flows were measured for 15 combinations of mean body (three states) and local skin temperature (five states), with the latter covering the broadest possible range of physiologically relevant, non-pathological skin temperatures.
A schematic of the forearm and calf plethysmographs (aluminium). The inner, cylindrical compartments enclosed each limb segment. These had internal diameters of 10.0 cm (forearm) and 17.5 cm, and respective depths of 15.0 and 20.5 cm. Each limb segment was covered with a snugly fitting latex membrane (sleeve) that was sealed within the plethysmograph using outer flanges secured to aluminium plates mounted on either end of the inner cylinder, creating water-tight seals. This chamber was then filled with water. The outer, water-filled compartments were designed to be of an approximately tenfold larger volume [width: 15.0 cm (forearm), 20.3 cm; height: 30.0 cm (forearm), 30.5 cm]. These compartments were isolated from the inner cylinder by aluminium walls, and these, in combination with the water volume differences, facilitated heat exchange between these compartments and the rapid cooling, heating and clamping of segmental skin temperatures. Water was circulated through the outer compartment from external, temperature-regulated water baths
Thermal clamping
The climate chamber and water-perfusion garment (140 tubes arranged in parallel, 1-m lengths to form jacket and trouser components: Paul Webb Associates, Yellow Springs, OH, USA) enabled the clamping of oesophageal, mean skin and mean body temperatures following each of the pre-experimental water immersions. The head, both hands, both feet and the left forearm or right calf were not contained within the perfusion garment, although those sites were either exposed to stable air temperatures or were housed within a displacement plethysmograph (Fig. 1). When not being treated, the left forearm and right calf were clamped at the same temperature as the water provided to the perfusion garment, as previously described (Caldwell et al. 2014). Thermal clamping for the rest of the body was sustained for the entire trial.
Standardisation
Trials were administered in a balanced order and at the same time of day within subjects, who were their own controls. Subjects presented in a euhydrated, well-rested and post-absorptive state, as described elsewhere (Caldwell et al. 2014).
Physiological measurements
Arterial blood flow to the body segment of interest was measured using water-filled, displacement plethysmographs constructed for this experiment (Caldwell and Taylor 2014). Not reported in that communication were the dimensions of the forearm and calf plethysmographs (Fig. 1) used to clamp and manipulate local skin temperatures, and then to measure segmental blood flow. The internal volumes of the forearm and calf plethysmographs were 1450 and 5376 mL, respectively. These accommodated an average forearm volume of 512 mL (SD 138) and a calf volume of 624 mL (SD 145). Each limb segment was covered with a latex sleeve and sealed into the inner chamber of each plethysmograph. That compartment was then filled with water, with its corresponding displacement during venous occlusion (proximally positioned pneumatic cuffs) being proportional to arterial flow (Abramson et al. 1939). The occlusion cuffs were automatically and intermittently inflated and deflated (50 mmHg; Groothuis et al. 2003) over 2-min data collection periods, during which six inflation cycles were performed (8-s inflation and 12-s deflation). Water displacement was detected from pressure changes within a displacement port (MPS-201G, Memstech, Singapore), with that signal amplified (four-channel amplifier, Onspot, Australia), converted to a digital equivalent (NI USB-9162, National Instruments, Hungary) and sampled at 20 Hz (Labview: version 7, National Instruments, Hungary). In addition, arterial occlusion cuffs (inflated to 160 mmHg prior to data collection) were positioned downstream at the corresponding wrist and ankle to negate significant artefacts created by autonomically driven changes in hand and foot blood flows.
Heart rate was recorded continuously (15-s intervals; Polar Electro Sports Tester, Finland), while mean arterial blood pressure (right brachial artery) was determined prior to each skin-temperature treatment (Omron SEM-2, Omron Healthcare Inc., Kyoto, Japan). The latter was used to derive segmental vascular conductance. A deep-body approximation of the central blood temperature (oesophagus; Taylor et al. 2014b), and skin and plethysmograph water temperatures (inner and outer compartments) were also recorded continuously (15-s intervals) using thermistors and a portable data logger (Caldwell et al. 2014; 1206 Series Squirrel, Grant Instruments Ltd., UK). Area-weighted mean skin (ISO 9886 1992) and mean body temperatures were derived (Vallerand et al. 1992), with deep-body weighting coefficients for the latter varying across trials: 0.65 (mild hypothermia), 0.70 (normothermia) and 0.80 (moderate hyperthermia). For the derivation of mean skin temperature, eight local sites were measured (forehead, chest, scapula, upper arm, forearm, hand, thigh, calf). Forearm and calf skin temperatures were approximated from the water temperature of the inner chamber of each plethysmograph, as it had previously been established that those temperatures matched independently measured skin temperatures (dorsal forearm and anterior calf) below each of the limb-segment sleeves (Caldwell 2014).
Data analysis
Between-treatment and between-segment comparisons were evaluated using multivariate analysis of variance, with three clamped mean body temperatures, five local-temperature treatments and two blood-flow measurement sites. Tukey’s HSD post hoc procedure was used to identify sources of significant difference with a probability threshold of 5 %. Least squares, best-fit linear regression analyses were performed using individual data from each experimental condition; the resulting parameters were averaged within conditions. These analyses were applied to both blood flow and vascular conductance data to investigate inter-segmental relationships with local skin temperature, but within each clamped thermal state. Data are reported as means with standard errors of the means (±) for changes in the central dependent variables, or with SDs for highlighting data distributions.
Results
Experimental control and thermal clamping
This experiment was predicated on first altering the thermal status of each participant and then successfully clamping three distinctly different mean body temperatures. The methods adopted ensured the attainment of that objective, with oesophageal and mean skin temperatures remaining clamped throughout each trial (P > 0.05). As a consequence, and when averaged across all local treatments, three markedly different thermal steady states were achieved (P < 0.05): mild hypothermia [oesophageal temperature: 36.0 °C (SD 0.15); mean skin temperature: 22.8 °C (SD 0.21); mean body temperature: 31.4 °C (SD 0.13)], normothermia [37.0 °C (SD 0.03), 33.6 °C (SD 0.23), 36.0 °C (SD 0.07)] and moderate hyperthermia [38.5 °C (SD 0.06), 37.9 °C (SD 0.09), 38.3 °C (SD 0.03)]. In the normothermic and hypothermic trials, the average relative mass loss was 0.5 % (P > 0.05), but for the hyperthermic trial, this was 2.4 % (P < 0.05), as fluid replacement did not occur during experimentation. Nevertheless, mean arterial pressure remained relatively stable (P > 0.05), both among conditions and during the local skin treatments: mild hypothermia 103.3 mmHg (SD 2.5), normothermia 90.8 mmHg (SD 1.6) and moderate hyperthermia 87.7 mmHg (SD 1.3). There was, however, a predictable thermal offset for the hyperthermic heart rate relative to that observed during both normothermia and hypothermia: mild hypothermia 63 b min−1 (SD 2), normothermia 62 b min−1 (SD 1) and moderate hyperthermia 102 b min−1 (SD 1; P < 0.05).
Localised temperature treatments
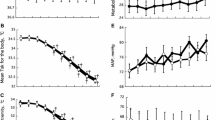
With this experimental control, it was assumed the only sites that might provide variations in either static or dynamic thermoafferent feedback would be the thermosensitive tissues sealed within the plethysmographs (left forearm and right calf). Moreover, the five localised thermal stimulations were reproducibly applied to those sites (Fig. 2a). Whilst these treatments differed significantly from one another (P < 0.05), thermal stimuli applied to the forearm did not differ from those applied to the calf within any of the five treatment levels (P > 0.05); these took approximately 10 min to stabilise. Accordingly, those treatments were layered across stable, deep-body temperatures, which differed significantly across these whole-body thermal states (Fig. 2b; P < 0.05), but not during the localised forearm or calf treatments (P > 0.05).
a Five localised skin-temperature treatments applied to the left forearm and right calf, and averaged across three clamped, whole-body thermal states: mild hypothermia, normothermia and moderate hyperthermia. These five treatments were applied by modifying and then clamping the water temperature of the outer compartment of each plethysmograph (Fig. 1), with each local thermal treatment being significantly different (P < 0.05). The target treatment temperatures are displayed on the abscissa, while the actual temperatures achieved are shown on the ordinate. Data are means with standard errors of the means (N = 8). b Mean deep-body (oesophageal) temperatures, averaged across the five skin-temperature treatments, but within the three targeted thermal states. Significant differences are illustrated by the symbols: †(relative to mild hypothermia; P < 0.05) and ‡(relative to the normothermic condition; P < 0.05)
Cutaneous vascular conductance and blood flow
The changes in vascular conductance accompanying these thermal treatments of the forearm and calf are shown in Fig. 3. These data show that, within each of the three thermally clamped states, the segmental vascular responses tracked changes in the localised thermal stimuli. When mildly hypothermic, however, neither limb segment was responsive, and even when normothermic, those segments were much less sensitive to these treatments. Thus, vasoconstriction and vasodilatation were much more powerfully induced when subjects were pre-heated. Indeed, significant between-treatment vascular differences were only observed between moderate hyperthermia and the other clamped conditions (P < 0.05). Whilst it is standard practice to report vascular responses in conductance units, the emphasis here was upon autonomically controlled convective heat transfer (mass flow). Therefore, since mean arterial pressures did not differ significantly across either trials or treatments (P > 0.05), expressing these data in this form provided no further information, so the results that follow are presented in flow units.
Vascular conductance of the left forearm (a) and right calf (b) measured using water-displacement, venous occlusion plethysmography. Data were collected within each of three clamped, whole-body thermal states (mild hypothermia, normothermia, moderate hyperthermia) with five local skin-temperature treatments applied to each segment (5, 15, 25, 33, 40 °C). Data are means with bi-directional standard errors of the means with mean linear regression lines obtained by averaging parameters derived for each participant. The sample size for each local treatment was eight unless otherwise noted, and when data were lost within a local treatment, the corresponding data for the same treatment were omitted from the other thermal states. The mean correlation coefficients for the forearm were: 0.84 (mild hypothermia), 0.85 (normothermia) and 0.99 (moderate hyperthermia). For the calf, these coefficients averaged: 0.73 (mild hypothermia), 0.97 (normothermia) and 0.91 (moderate hyperthermia). Symbols show sources of significant differences in segmental vascular conductance for these localised skin-temperature treatments (P < 0.05), and with respect to either mild hypothermia (†) or normothermia (‡)
Across all treatments, forearm and calf blood flows generally fell between the lower and upper limits observed for the foot and hand (respectively) for identical thermal states and localised thermal treatments (Caldwell et al. 2014). But unlike our companion experiment, in which segmental blood flows of the hand exceeded those of the foot across almost every combination of mean body and local skin temperatures, the current trials revealed similar normothermic flows for both the forearm and calf. When in this state, and when locally treated with temperatures close to the thermoneutral mean skin temperature (33 °C), forearm blood flows averaged 4.2 mL 100 mL−1 min−1 (±0.9), whilst those of the calf were 5.4 mL 100 mL−1 min−1 (±1.2; P > 0.05). Since the limb-segment tissue volume contained within each plethysmograph could be approximated for each individual (assuming cylindrical geometry), then absolute segmental blood flows could be approximated. In the normothermic state, those flows averaged 21.1 mL min−1 (±4.45; forearm) and 35.2 mL min−1 (±9.11; P > 0.05), with only two subjects having lower calf blood flows.
Within the mildly hypothermic and normothermic trials, the vascular responses to altered local skin temperatures were minimal. The mean slopes (sensitivities) of the forearm and calf relationships between segmental blood flow and the change in local skin temperature were 0.04 mL 100 mL−1 min−1 °C−1 (forearm: ±0.01) and 0.02 mL 100 mL−1 min−1 °C−1 (±0.11) when subjects were mildly hypothermic (P > 0.05), and during normothermia, both flows were equivalent and <0.1 mL 100 mL−1 min−1 °C−1 (±0.03). During moderate hyperthermia, the vascular thermosensitivity of both segments increased [0.22 mL 100 mL−1 min−1 °C−1 (forearm: ±0.07) and 0.18 mL 100 mL−1 min−1 °C−1 (±0.05); P > 0.05]. Nevertheless, within each segment, and across the three whole-body thermal states, vascular thermosensitivity was significantly elevated with each step change in the clamped mean body temperature (P < 0.05), when compared to the hypothermic trial. Thus, when moving from mild hypothermia to normothermia, forearm vascular sensitivity increased 219 %, whilst the corresponding change for the calf was 796 %. That difference was dictated by the lower sensitivity of the hypothermic calf. Relative to the normothermic trial, moderate hyperthermia was associated with approximately equal vascular sensitivity increases for each segment: 250 % (forearm) and 224 % (calf; P > 0.05).
Notwithstanding these differences, both limb segments responded similarly across the three trials (Fig. 3), with vascular conductance almost superimposed during moderate hyperthermia. Consequently, within-trial differences in either segmental conductance or blood flow were not significant during any local treatment (P > 0.05). Therefore, neither the maximal nor minimal vascular changes differed between the forearm and calf.
To evaluate the relative impact of changes in deep-body and local skin temperature in the modulation of segmental blood flows, intra-segmental flow comparisons were made when both the forearm and calf skin temperatures were about 33 °C, but with sustained normothermic and hyperthermic clamps. In the latter circumstance, the deep-body (oesophageal) temperature was displaced upwards by 1.5 °C (±0.1) during the forearm treatments, and 1.6 °C (±0.1) when the calf was studied. The corresponding changes in segmental blood flow were 7.2 (±0.9; forearm) and 4.3 mL 100 mL−1 min−1 (±2.0; calf). Thus, for equivalent elevations in this deep-body temperature index, forearm blood flow increased by 5.1 mL 100 mL−1 min−1 °C−1 relative to flows observed when normothermic, while the calf was less responsive, rising by 3.3 mL 100 mL−1 min−1 °C−1. During the normothermic clamp, the increases in both forearm and calf blood flows, over a 35 °C elevation in local skin temperature (5–40 °C), were only 0.09 mL 100 mL−1 min−1 °C−1. Consequently, the vascular sensitivities of both the forearm and calf were dramatically more dependent upon elevations in deep-body temperature than an equivalent change in local skin temperature.
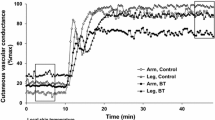
Three-dimensional surfaces
From these data, three-dimensional surfaces (Figs. 4, 5) were constructed to describe the cutaneous vascular responses of mildly hypothermic, normothermic and moderately hyperthermic individuals during the localised application of cutaneous thermal stimuli covering a 35 °C range. Each surface is coded using the colour spectrum to identify flow variations between minimal (blue) and maximal perfusion (orange), and these may be compared with the corresponding surfaces created for the hands and feet in the same subjects under identical conditions (Caldwell et al. 2014).
A three-dimensional surface for forearm blood flow across a 6.9 °C range of mean body temperatures and a 35 °C range of local skin temperatures. Participants were resting, semi-nude and supine (N = 8) following each of three pre-experimental treatments [separate trials: mild hypothermia: 36.0 °C (oesophageal temperature); normothermia: 37.0 °C; moderate hyperthermia: 38.5 °C]. Mean body temperatures were clamped throughout each trial, whilst five local skin-temperature treatments were applied (~5, 15, 25, 33, 40 °C). Segmental blood flows were measured using water-displacement, venous occlusion plethysmography. Data are averages for each of the 15, three-dimensional coordinates with other points derived through extrapolation. Surface colours identify blood flow variations; blue is minimal and orange maximal flow. The white, transparent plane represents the mean, normothermic calf blood flow (5.4 mL 100 mL−1 min−1)
A three-dimensional surface to describe the interaction of calf blood flow with variations in mean body and local skin temperatures in supine, resting subjects (N = 8). Participants were pre-heated or pre-cooled to induce three different thermal states [separate trials: mild hypothermia: 36.0 °C (oesophageal temperature); normothermia: 37.0 °C; moderate hyperthermia: 38.5 °C]. Mean body temperatures were then clamped and five local-temperature treatments were applied (~5, 15, 25, 33, 40 °C). Data are average three-dimensional coordinates, with colour coding to identify minimal (blue) and maximal (orange) flow variations. The white plane indicates the mean, normothermic forearm blood flow (4.2 mL 100 mL−1 min−1)
For the hands and feet (Caldwell et al. 2014), maximal flows differed by almost a factor of two, whilst during these trials, forearm and calf blood flows overlapped extensively throughout the range of observed flows, yielding similar mean segmental perfusion rates during the normothermic trial when the local stimulation temperature was 33 °C [4.2 (forearm) and 5.4 mL 100 mL−1 min−1]. These data are represented as white planes in Figs. 4 and 5, but, for comparative purposes, each plane shows the normothermic blood flow of the other limb segment. The corresponding foot and hand blood flows under those normothermic conditions were 2.8 (foot) and 6.7 mL 100 mL−1 min−1 (Caldwell et al. 2014).
Whilst quantitative differences in segmental blood flows were minimal, these three-dimensional presentations reveal a qualitative divergence. That is, forearm blood flow fell more sharply to its lower normothermic level when the mean body temperature was reduced to the normothermic state (Figs. 3, 4). It then changed very little when mild hypothermia was induced. Conversely, these same step changes in the whole-body thermal state resulted in more uniform vascular responses within the calf. As a result, the three-dimensional surface for the calf illustrates that, whilst the thermal dominance of the deep-body tissues over thermoeffector control was still evident, vasoconstrictor tone was released more gradually across the mean body temperatures investigated (31.4–38.3 °C).
Discussion
This experiment has permitted the development of detailed descriptions for the inter-relationships among forearm and calf skin blood flows across 15 diverse combinations of mean body and local skin temperatures. Within this project, two working hypotheses were tested. Firstly, it was postulated that changes in mean body temperature, but not localised cutaneous stimuli, would dominate the control of blood flowing to these non-glabrous skin sites (forearm and calf). This was verified, as had previously been shown for the hands and feet (Caldwell et al. 2014), and for cutaneous blood flow in general (Wyss et al. 1974; Proppe et al. 1976). Secondly, it was anticipated that those thermal stimuli would elicit less extreme blood flow changes than were observed at the hands and feet following identical treatments. This too was supported, and whilst this project was largely descriptive in nature, two related and possibly novel observations arose. The cutaneous blood flow responses of both limb segments to these local thermal stimuli were much more pronounced when the mean body temperature was elevated, relative to the responses observed within the hypothermic and normothermic states. This pattern was more apparent at the forearm. Therefore, the most powerful constriction and dilatation of these blood vessels will be seen in pre-heated individuals. In addition, whilst those responses were linear in nature (Fig. 3), when viewed in a three-dimensional configuration (Figs. 4, 5), an obvious non-linear pattern of blood flow emerged for the forearm, but not the calf.
An implicit assumption underpinning this research is that whilst the method used (venous occlusion plethysmography) will detect flow changes within all vascular beds contained within the field of measurement, those measurements will also permit one to draw conclusions relating primarily to cutaneous blood flow. This assumption has been validated for thermally induced variations in the limb blood flow of both resting (Edholm et al. 1956; Detry et al. 1972; Johnson et al. 1976) and exercising individuals (Johnson and Rowell 1975), providing the limb in question remains inactive, although our understanding of muscle blood flow within these states is somewhat imprecise (Johnson et al. 2014; Crandall and Wilson 2015). Accordingly, it is widely accepted that, under the conditions used in this experiment, plethysmographically determined limb-segment volume changes will mostly reflect those of the cutaneous vascular compartment. Nevertheless, it is possible that the intra-individual muscle blood flows varied over these trials since muscle temperatures would have changed, albeit to a smaller extent, across the three thermal states. In the absence of either muscle temperature or blood flow data, the impact of these variations remains unknown.
On the basis of this assumption, the veracity of the premiss that vascular conductance can be maximised through the local application of heat to the skin of normothermic individuals (42 °C: Taylor et al. 1984) was evaluated, as it was with regard to hand and foot perfusion (Caldwell et al. 2014). Data presented in Fig. 3 reinforce the truism that maximal cutaneous vascular conductance can only be obtained when local heating is applied during whole-body hyperthermic states, and this applies to both non-glabrous and glabrous vascular beds (Caldwell et al. 2014). In fact, one could predict the forearm vascular conductance of a moderately hyperthermic person, at local skin temperature <10 °C, would be significantly higher than if that individual was normothermic and locally heated to 42 °C.
From Fig. 3, it is clear that the cutaneous vascular conductance rises linearly with increments in local skin temperature, albeit imperceptibly so when participants were hypothermic, and minimally when normothermic. This characteristic was especially evident at the forearm, which resembled the responses of the hands and feet (Caldwell et al. 2014), and is reflected within the precipitous blood flow reductions as the mean body temperature was reduced (Fig. 4). This characteristic results from the powerful, thermo-protective influence exerted by the underlying vasoconstrictor tone evident during mild hypothermia and, to a lesser extent, during normothermia. Indeed, this is perhaps the most striking difference between Figs. 4 and 5. It is recognised, of course, that the resolution of these arrays is limited due to investigating only 15 thermal combinations, although it was the vascular responses induced when moving into the normothermic state that were largely responsible for abrupt reduction in blood flow.
At the calf, cutaneous blood flows declined in a more linear fashion with reductions in mean body temperature, and the deep-body temperature influence on this change was less powerful. This presumably reflected a more gradual release of the background constrictor tone. Indeed, while the vascular beds of the forearms (Figs. 3, 4), hands and feet seem to be dominated by this autonomic constrictor drive during normothermia (Roddie et al. 1957), that tonic activity appears to be a less powerful modulator of cutaneous blood flow at the calf. This observation requires verification, and notwithstanding the resolution qualification noted above, it may have implications for regional differences in the neural control of the cutaneous vascular beds and heat exchange, and to the extent that reductive observations derived from very small skin sites can be applied to vascular control within an integrated organism. It also leads one to ask why the vascular responses of the forearm and hand might be more alike, whilst those of the calf and foot appear somewhat dissimilar. However, since these observations were derived only from healthy and asymptomatic males, then it is perhaps necessary to verify these outcomes within a similar sample of women.
Since the upper limbs are principally involved in fine-motor activities, then a moderate vasoconstrictor tone under basal conditions will serve a thermo-protective role for the more susceptible musculature of the hands and forearms. If these resting observations translate into exercising states, then one may be tempted to seek an evolutionary explanation that relates to the possible parallel development of bipedalism and persistence hunting (Liebenberg 2006), both of which occurred within warm-dry climates (Gowlett 2001; Cerling et al. 2011), and the combination of which would impose unique selective pressures on early hominins (Lieberman 2015). Since long-duration bipedal exercise dictates that heat production is dominated by muscular activity of the legs, which are much less effected by cooling (Taylor et al. 2014a), it could be advantageous if these regions could more readily and more directly dissipate this heat from their overlying surfaces.
Conclusion
In combination with our previous communication on the cutaneous vascular responses of the hands and feet (Caldwell et al. 2014), the current investigation has resulted in the provision of a comprehensive survey of cutaneous blood flow variations across a broad range of thermal states. These three-dimensional descriptions of the mean body and local thermal relationships with glabrous (hand and foot) and non-glabrous (forearm and calf) skin blood flows have reinforced the importance of deep-tissue temperatures in the modulation of cutaneous perfusion. Indeed, locally mediated vasoconstrictor and vasodilator responses were significantly more powerful in people who had first experienced whole-body warming. These data also highlight clear regional differences in vascular control, as recently defined for sudomotor function (Taylor and Machado-Moreira 2013), with the more distal sites typically experiencing greater blood flow extremes. Finally, the non-linear pattern of blood flow changes evident in the forearm, hands and feet with changes in mean body temperature appeared to be absent for the calf.
References
Abramson DI, Zazeela H, Marrus J (1939) Plethysmographic studies of peripheral blood flow in man: I. Criteria for obtaining accurate plethysmographic data. Am Heart J 17:194–205
Brown AC, Brengelmann GL (1970) The interaction of peripheral and central inputs in the temperature regulation system. In: Hardy JD, Gagge AP, Stolwijk JAJ (eds) Physiological and behavioral temperature regulation. C.C Thomas, Springfield, pp 684–702
Caldwell JN (2014) Exploring thermal interactions with vasomotion, sudomotion and thermogenesis. Doctor of Philosophy, University of Wollongong, Australia
Caldwell JN, Taylor NAS (2014) Water-displacement plethysmography: a technique for the simultaneous thermal manipulation and measurement of whole-hand and whole-foot blood flows. Physiol Meas 35:1781–1795
Caldwell JN, Matsuda-Nakamura M, Taylor NAS (2014) Three-dimensional interactions of mean body and local skin temperatures in the control of hand and foot blood flows. Eur J Appl Physiol 114:1679–1689
Cerling TE, Wynn JG, Andanje SA, Bird MI, Korir DK, Levin NE, Mace W, Macharia AN, Quade J, Remien CH (2011) Woody cover and hominin environments in the past 6 million years. Nature 476:51–56
Clark ER (1938) Arterio-venous anastomoses. Physiol Rev 18:229–247
Crandall CG, Wilson TE (2015) Human cardiovascular responses to passive heat stress. Compr Physiol 5:17–43
Detry JM, Brengelmann GL, Rowell LB, Wyss C (1972) Skin and muscle components of forearm blood flow in directly heated resting man. J Appl Physiol 32:506–511
Edholm OG, Fox RH, Macpherson RK (1956) The effect of body heating on the circulation in skin and muscle. J Physiol 134:612–619
Elstad M, Vanggaard L, Lossius AH, Walløe L, Bergersen TK (2014) Responses in acral and non-acral skin vasomotion and temperature during lowering of ambient temperature. J Therm Biol 45:168–174
Gowlett JAJ (2001) Out in the cold. Nature 413:33–34
Groothuis JT, van Vliet L, Kooijman M, Hopman MT (2003) Venous cuff pressures from 30 mmHg to diastolic pressure are recommended to measure arterial inflow by plethysmography. J Appl Physiol 95:342–347
Hales JRS (1985) Skin arteriovenous anastomoses, their control and role in thermoregulation. In: Johansen K, Burggren WW (ed) Cardiovascular shunts: phylogenetic, ontogenetic and clinical aspects. Proceedings of the Alfred Benzon symposium, Copenhagen, vol 21, pp 433–448
ISO 9886 (1992) Evaluation of thermal strain by physiological measurements. International Standard Organisation, Geneva
Jessen C (2011) Interaction of body temperatures in control of thermoregulatory effector mechanisms. Compr Physiol, Supplement 14: Handbook of physiology, environmental physiology: 127–138. First published in print 1996
Johnson JM, Rowell LB (1975) Forearm skin and muscle vascular responses to prolonged leg exercise in man. J Appl Physiol 39:920–924
Johnson JM, Brengelmann GL, Rowell LB (1976) Interactions between local and reflex influences on human forearm skin blood flow. J Appl Physiol 41:826–831
Johnson JM, Minson CT, Kellogg DL (2014) Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr Physiol 4:33–89
Libert JP, Candas V, Vogt JJ (1978) Sweating response in man during transient rises of air temperature. J Appl Physiol 44:284–290
Liebenberg L (2006) Persistence hunting by modern hunter–gatherers. Curr Anthropol 47:1017–1025
Lieberman DE (2015) Human locomotion and heat loss: an evolutionary perspective. Compr Physiol 5:99–117
Machado-Moreira CA, Caldwell JN, Mekjavic IB, Taylor NAS (2008) Sweat secretion from palmar and dorsal surfaces of the hands during passive and active heating. Aviat Space Environ Med 79:1034–1040
Molyneux GS, Bryden MM (1981) Comparative aspects of arteriovenous anastomoses. In: Harrison RJ, Holmes RL (eds) Progress in anatomy. Cambridge University Press, Cambridge, pp 207–227
Nadel ER, Bullard RW, Stolwijk JAJ (1971) Importance of skin temperature in the regulation of sweating. J Appl Physiol 31:80–87
Nagasaka T, Cabanac M, Hirata K, Nunomura T (1987) Control of local heat gain by vasomotor response of the hand. J Appl Physiol 63:1335–1338
Pérgola PE, Kellogg DL, Johnson JM, Kosiba WA, Solomon DE (1993) Role of sympathetic nerves in the vascular effects of local temperature in human forearm skin. Am J Physiol 265:H785–H792
Proppe DW, Brengelmann GL, Rowell LB (1976) Control of baboon limb blood flow and heart rate—role of skin vs. core temperature. Am J Physiol 231:1457–1465
Regan JM, Macfarlane DJ, Taylor NAS (1996) An evaluation of the role of skin temperature during heat adaptation. Acta Physiol Scand 158:365–375
Roddie IC, Shepherd JT, Whelan RF (1957) The contribution of constrictor and dilator nerves to the skin vasodilation during body heating. J Physiol 136:489–497
Romanovsky AA (2014) Skin temperature: its role in thermoregulation. Acta Physiol 210:498–507
Spealman CR (1945) Effect of ambient air temperature and of hand temperature on blood flow in hands. Am J Physiol 145:218–222
Stocks JM, Patterson MJ, Hyde DE, Jenkins AB, Mittleman KD, Taylor NAS (2004) Effects of immersion water temperature on whole-body fluid distribution in humans. Acta Physiol Scand 182:3–10
Taylor NAS (2014) Human heat adaptation. Compr Physiol 4:325–365
Taylor NAS, Machado-Moreira CA (2013) Regional variations in transepidermal water loss, eccrine sweat gland density, sweat secretion rates and electrolyte composition in resting and exercising humans. Extreme Physiol Med 2:4
Taylor WF, Johnson JM, O’Leary D, Park MK (1984) Effect of high local temperature on reflex cutaneous vasodilation. J Appl Physiol 57:191–196
Taylor NAS, Caldwell JN, Mekjavic IB (2006) The sweating foot: local differences in sweat secretion during exercise-induced hyperthermia. Aviat Space Environ Med 77:1020–1027
Taylor NAS, Machado-Moreira CA, van den Heuvel AMJ, Caldwell JN (2014a) Hands and feet: physiological insulators, radiators and evaporators. Eur J Appl Physiol 114:2037–2060
Taylor NAS, Tipton MJ, Kenny GP (2014b) Considerations for the measurement of deep-body, skin and mean body temperatures. J Therm Biol 46:72–101
Tipton MJ (1989) The initial responses to cold-water immersion in man. Clin Sci 77:581–588
Tipton MJ, Wakabayashi H, Barwood MJ, Eglin CM, Mekjavic IB, Taylor NAS (2013) Habituation of the metabolic and ventilatory responses to cold-water immersion in humans. J Therm Biol 38:24–31
Vallerand AL, Savourey G, Hanniquet A, Bittel JHM (1992) How should body heat storage be determined in humans: by thermometry or calorimetry? Eur J Appl Physiol 65:286–294
Werner J, Mekjavic IB, Taylor NAS (2008) Concepts in physiological regulation: a thermoregulatory perspective. In: Taylor NAS, Groeller H (eds) Physiological bases of human performance during work and exercise. Churchill Livingstone Elsevier, Edinburgh, pp 325–340
Wyss CR, Brengelmann GL, Johnson JM, Rowell LB, Niederberger M (1974) Control of skin blood flow, sweating, and heart rate: role of skin vs. core temperature. J Appl Physiol 36:726–733
Acknowledgments
Joanne N. Caldwell held an Australian Post-Graduate Award from the University of Wollongong (Australia).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Additional information
Communicated by Narihiko Kondo.
Rights and permissions
About this article
Cite this article
Caldwell, J.N., Matsuda-Nakamura, M. & Taylor, N.A.S. Interactions of mean body and local skin temperatures in the modulation of human forearm and calf blood flows: a three-dimensional description. Eur J Appl Physiol 116, 343–352 (2016). https://doi.org/10.1007/s00421-015-3288-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-015-3288-4