Abstract
Purpose
We investigated the role of noradrenergic sympathetic nerves in the cutaneous circulation at rest and in response to local heating.
Methods
Dorsal forearm and lateral leg sites were each instrumented with 2 microdialysis fibers, 2 local skin heaters, and 2 laser-Doppler probes. All sites were heated from 33° to 42 °C. Each limb had 1 skin site treated with bretylium tosylate (BT) to block noradrenergic sympathetic neurotransmitter release and 1 site infused with lactated Ringer’s (Control).
Results
During baseline (33 °C), cutaneous vascular conductance (CVC; laser-Doppler flux/blood pressure) at control (24 ± 2 %max) and BT-treated (29 ± 4 %max) sites in the leg was significantly higher than the forearm (control: 12 ± 1 %max; BT-treated: 17 ± 2 %max) (P = 0.032 and P = 0.042). At 42 °C local skin temperature, the initial peak CVC response with BT decreased compared to control at both forearm (62 ± 3 vs. 86 ± 6 %max, P < 0.01) and leg (67 ± 3 vs. 77 ± 2 %max, P = 0.035) sites. CVC at the forearm with BT was lower than that of the leg (P = 0.02). With control, plateau phase (~35 min at 42 °C) CVC was greater in the leg (98 ± 2 %max) than the forearm (89 ± 4 %max) (P = 0.027). BT reduced the peak CVC in the leg (90 ± 4 %max, P = 0.027) and in the forearm (69 ± 5 %max, P < 0.01). CVC at the BT-treated sites was reduced more in the forearm than in the legs (P < 0.01).
Conclusions
The contribution of noradrenergic sympathetic nerves during local heating differs between leg and forearm at rest and with skin heating.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skin blood flow is important in human thermoregulation for regulating heat exchange between the body and the surrounding environment (Johnson et al. 2014). Skin can be heavily perfused, with maximal forearm skin blood flow estimated near 275 ml 100 ml tissue−1 min−1 (Johnson and Proppe 1996). Consequently, even small differences in the skin blood flow response throughout different regions could markedly affect overall thermoregulation. The forearms and lower-leg regions comprise ~6.5 and ~14.5 % of the surface area of the human body, respectively (Cross et al. 2008). The majority of research examining the mechanisms of the vascular response to changes in local skin temperature (T loc) has been performed on the forearm, hands, and fingers, with minimal data collected from other parts of the body such as the leg. However, we have previously reported differences in the involvement of nitric oxide synthase (NOS) in the cutaneous thermal hyperemia in response to local skin heating between the forearms and legs (Del Pozzi et al. 2013). Therefore, an understanding of the mechanisms of control in different regions is of great importance.
The hyperaemic response to increasing T loc is accomplished principally through the actions of nitric oxide (NO), sensory nerves, and noradrenergic sympathetic nerves (Tew et al. 2011d; Carter and Hodges 2011; Hodges et al. 2009b, 2008; Minson et al. 2001; Kellogg et al. 2009, 1999; Stewart et al. 2011). This skin blood flow response follows a biphasic pattern which starts with a rapid, transient initial peak, succeeded by a brief nadir and a secondary prolonged vasodilatation to a sustained plateau (Minson et al. 2001). The initial peak is thought to be mediated by both sensory and sympathetic nerves (Houghton et al. 2006; Hodges et al. 2008; Minson et al. 2001; Carter and Hodges 2011), while the sustained vasodilatation to prolonged skin heating, i.e. plateau phase, is primarily dependent on eNOS (Kellogg et al. 2008a) and endothelial-derived hyperpolarizing factors (EDHF) (Brunt and Minson 2012).
Investigating the regional skin blood flow patterns and their underlying mechanisms, we previously found a difference in the basal skin blood flow in the forearms and legs due to greater NO contribution (Del Pozzi et al. 2013) and endothelial activity (Hodges and Del Pozzi 2014) in the skin of the legs than in the skin of the arms. Furthermore, in response to local skin heating, the initial peak at leg skin sites was significantly lower than that achieved in the forearms (Del Pozzi et al. 2013). Under pre- or post-synaptic adrenergic blockade, the initial peak of the forearm was, surprisingly, either abolished (Houghton et al. 2006; Hodges et al. 2008, 2009a, b) or diminished (Hodges et al. 2009a, b; Tew et al. 2011d; Hodges and Sparks 2013) in response to local skin heating. These data suggested that noradrenergic nerves contribute to achieve a complete initial vasodilator response. In addition, post-synaptic adrenergic antagonism revealed the important contribution of both noradrenaline (NA) and neuropeptide Y in the initial vasodilator response (Hodges et al. 2008; Hodges and Sparks 2013). Different pharmacological stimuli have shown greater α-adrenoceptor sensitivity in the vascular responsiveness of the legs compared to the forearms (Pawelczyk and Levine 2002; Yamazaki and Yuge 2011). However, whether or not sympathetic function in the cutaneous circulation differs between forearms and legs to thermal stimuli is not known. Additionally, some pathological conditions such as diabetes, peripheral arterial disease, and postural tachycardia syndrome typically present themselves first in the lower limbs. Consequently, it is important to determine if the mechanisms involved in the regulation of the cutaneous microvasculature are the same between different regions of the body.
We sought to determine whether the previously observed difference in the initial peak between the forearms and the leg was due to differences in noradrenergic sympathetic nerve function. We examined the effects of pre-synaptic noradrenergic sympathetic nerve blockade, using bretylium tosylate (BT), on the vasodilator response to local skin heating in the forearm and leg in young, healthy humans. Based on extant data (Pawelczyk and Levine 2002; Minson et al. 2001, 2002; Tew et al. 2011c, d; Yamazaki and Yuge 2011) and our previous findings (Hodges and Del Pozzi 2014; Del Pozzi et al. 2013), we hypothesized that blockade of the noradrenergic sympathetic nerves would reduce the initial peak response to local skin heating more in the skin of the legs than in the forearms. This supposition is based on the previously noted increased adrenergic sensitivity in legs compared to forearms, and may provide a mechanistic basis for the higher initial peaks observed in forearms than the legs (Del Pozzi et al. 2013).
Methods
Participants
This study was approved by the Institutional Review Board at The University of Alabama. All participants were fully informed of the experimental methods as well as the associated risks prior to their volunteering to be a participant. Verbal as well as written informed consent was obtained from each participant. All experimental protocols conformed to the guidelines set forth by the Declaration of Helsinki.
Nine participants were required, based on a priori power analysis with an α of 0.05, β of 0.90, and with standard deviations and expected required mean differences from our laboratory’s previous work within the field (Del Pozzi et al. 2013; Tew et al. 2011a, b; Carter and Hodges 2011) (nQuery Advisor, v. 3). Inclusion criteria were age between 19 and 35 years, with no diagnosis of any metabolic or cardiovascular disease. Exclusion criteria included current tobacco use or taking any medication other than prescription birth control. Nine healthy, active, but not trained individuals (27 ± 2 years, 6 men, and 3 women) participated. They were instructed to abstain from caffeine and alcohol for 24 h prior to testing and to not eat for 2 h prior to the testing session but were instructed to drink water ad libitum. Female subjects were all using oral contraceptives and currently in the low hormone phase of their routine as verified through self-report (Charkoudian 2001; Stephens et al. 2002).
Instrumentation and experimental procedures
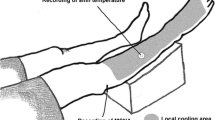
Due to the prolonged time commitment of the experiments (~3 h), participants visited the laboratory twice, one visit for each limb, with the order of testing randomized. All experiments started at 0700 h, and all protocols were performed in the same manner in a temperature controlled room ranging from 20 to 22 °C. Participants laid supine on an adjustable gurney, and two skin sites were chosen on either the forearm (dorsal aspect) or the leg (lateral aspect) depending on the session. As a temporary anesthetic, ice packs were placed over the skin sites where the fibers were to be placed. Following temporary anesthesia, custom-built microdialysis fibers were placed using the same techniques as previously described by our laboratory (Del Pozzi et al. 2013). Ninety min were allowed for the hyperaemia associated with the needle insertion trauma to subside (Cracowski et al. 2011; Anderson et al. 1994; Hodges et al. 2009a). An integrated skin heater and temperature monitor (model SH02, Moor Instruments Devon, UK) was used to monitor and adjust local skin temperature. Red blood cell flux was measured via laser-Doppler flowmetry (MoorVMS-LDF2, Moor Instruments, Devon, UK) and was used to provide an index of skin blood flow (Johnson 1990; Öberg 1990). Laser-Doppler flow (LDF) probes (VP12, Moor Instruments, Devon, UK) were placed within a small opening in the skin heaters to monitor red blood cell flux.
Lactated Ringer’s was infused at both sites at a rate of 4 µl min−1 for the first 30 min of the 90 min trauma resolution period. After 30 min of trauma resolution, one site, either forearm or leg, depending on the day, was chosen as a control, and lactated Ringer’s continued to be infused. At the experimental skin site, BT (US Pharmacopeia, Rockville, MD) was administered at a concentration of 10 mM (Tew et al. 2011d; Carter and Hodges 2011; Hodges et al. 2009b). After 30 min of drug infusion, the participant was further instrumented with local skin heaters that were set at 33 °C (thermoneutral) and placed on top of the microdialysis fibers enabling the control and monitoring of T loc at the site of measurement. Following the 90 min of trauma resolution (Anderson et al. 1994; Cracowski et al. 2011; Hodges et al. 2009a), it was confirmed that LDF data had stabilized before data collection began. Before baseline measurements were recorded, the efficacy of the BT was verified by performing a cold pressor test on the contra-lateral arm. This test elicits a transient sympathetic-dependent vasoconstriction that is abolished under conditions of sympathetic nerve blockade. 10 min after confirmation of sympathetic blockade, baseline measurements were recorded (Fig. 1). Following baseline measurements (10 min), the local skin heating protocol was performed by increasing T loc 0.5 °C 10 s−1 until T loc had reached 42 °C (Hodges and Sparks 2013; Del Pozzi et al. 2013). T loc was maintained at 42 °C for 35 min at which time a stable plateau had been reached, and verified, representing a physiological maximum (Taylor et al. 1984). Following the stabilization of the plateau phase, sodium nitroprusside (SNP) was infused at both control and treatment sites at a concentration of 58 mM for 35 min to pharmacologically induce maximal cutaneous vasodilatation (Kellogg et al. 2005, 2008a, b, 2009).
Data from a representative participant, in cutaneous vascular conductance (CVC) as a percentage of max. Four skin sites, two on the arm (circles) and two on the leg (triangles); each limb had one untreated site (open symbol) and one site treated with bretylium tosylate (BT) (closed symbol). Note the reduction in CVC in both arms and legs under conditions of BT treatment. Sections A and B indicate 5-min periods of data analysis for baseline and plateau phases of local skin heating. ↑ indicates time period of increasing local skin temperature
Data collection and analysis
Since it has been shown through direct (Park and Guntheroth 1970) and indirect (Sareen et al. 2012) methods that supine mean arterial pressure (MAP) does not differ between the forearm and the leg, blood pressure was measured through oscillometry in the contra-lateral arm every 5 min throughout the duration of the study protocol. MAP was calculated as
Data were collected at 50 Hz and stored on a personal computer to be analyzed offline using signal-processing software (Acqknowledge v4.2, Biopac MP150, Camino Goleta, CA). LDF data were converted to cutaneous vascular conductance (CVC) by dividing LDF (mV) by the calculated MAP (mmHg). Data were normalized to maximal vasodilatation and expressed as a percentage of the maximum CVC (%CVCmax) of each site.
Comparison of absolute CVC among subjects is difficult with LDF measurements due to the large heterogeneity of the cutaneous circulation (Johnson et al. 1984); therefore, laser-Doppler data were normalized to maximal dilatation values. The fact that LDF does not produce data with a credible unit (e.g. ml/100 ml tissue/min) has always been a major limitation of the technique (Öberg 1990; Johnson 1990). Thus, expression of the LDF data as a %CVCmax is necessary if meaningful comparisons are to be made among participants and groups.
Due to the short duration of the initial peak, 30-s portions of CVC were used. Stable 5-min periods of CVC data were used for both the baseline and the plateau phases (Fig. 1). The percentage contribution of sympathetic (BT) nerves was calculated using the following equation (Wong 2013; Del Pozzi et al. 2013):
Time data for the onset of vasodilatation, initial peak, nadir, and plateau phase from the start of local skin heating were recorded and measured in ms and presented in s. This analysis was performed by the same investigator who was blinded to the limb and treatment of the blood flow waveforms.
Text and illustrative results are reported as the mean ± standard deviation. All analysis performed was by paired t-statistics or when appropriate, a repeated measure analysis of variance. Bonferroni post hoc analysis was performed when deemed appropriate. Statistical significance was set a priori at P < 0.05. Since there was no discernible difference between the data of the female and the male participants, data were combined and analyzed together. All data were analyzed using SPSS software version 19.0 (SPSS, inc., Chicago, Illinois, USA).
Results
Figure 1 illustrates the skin blood flow responses in CVC as a percentage of maximum dilatation from a representative subject to 35 min of local skin heating at two forearm and two legs sites. At baseline with a T loc of 33 °C, CVC at the leg was higher than the forearm. Following treatment with BT leg, CVC was still higher than the forearm even though treatment with BT increased flux at both the forearm and leg sites. With an increase in T loc at 10 min, the initial peak response for the untreated control site in the forearm was higher when compared to leg. However, following treatment with BT, the initial peak response of the leg was higher than that of the forearm. Additionally, the leg had a higher plateau phase response than that of the forearm even under conditions of sympathetic blockade. Following treatment with BT, the plateau phase CVC at both the forearm and the leg was reduced.
CVC Data presented as a percentage of maximal dilatation
Basal
Figure 2 presents the average responses for all 9 participants, in CVC as a percentage of max (%max), at a T loc of 33 °C (thermoneutral). CVC averaged 12 ± 1 %max at forearm control sites and 17 ± 2 %max at sites treated with BT (P < 0.01) (Fig. 2a). CVC at control leg sites averaged 24 ± 2 %max and at BT treated sites 29 ± 4 %max (P < 0.01). CVC was significantly higher in the legs compared to the arms at control and at BT-treated skin sites (both P < 0.001). The increase in the CVC following the BT treatment was similar for both forearm and leg (P = 0.4). The percent contribution of noradrenergic function to basal CVC was less in the skin of the forearm (−41 ± 3 %) than the leg (−22 ± 4 %) (Fig. 2b) (P < 0.001).
Baseline (33 °C) cutaneous vascular conductance represented as a percentage of maximum for each region at control and during bretylium tosylate (BT) intervention (Panel A). Note that, blockade of sympathetic nerves with BT causes an increase in basal CVC. Baseline (33 °C) percent contribution of noradrenergic sympathetic nerves for each region (Panel B). Under basal conditions, these data indicate that the arms have greater tonic sympathetic-mediated vasoconstriction than the legs. * indicates P < 0.05 compared to control. † indicates P < 0.05 compared to arm. ‡ indicates P < 0.05 compared to BT treated arm
Initial Peak
Upon local skin heating, CVC during the initial peak responses at the forearm skin sites treated with BT was significantly less than at the control skin sites (62 ± 3 %max BT treated and 86 ± 2 %max control P < 0.001) (Fig. 3a). CVC initial peak responses at the leg skin sites were also reduced with BT treatment (67 ± 3 %max BT treated and 77 ± 2 % max control and, P = 0.005). CVC responses at the untreated skin sites to the onset of local skin heating in the forearm were higher than those of the leg sites (P = 0.01). In contrast, the initial peak of the skin sites treated with BT was significantly higher in the leg than that of the forearm (P < 0.01). The contribution of sympathetic function to the initial peak response was higher in the forearm (27 ± 4 %) when compared to the leg (13 ± 3 %) (P < 0.001) (Fig. 3b).
Initial peak (onset of warming protocol) cutaneous vascular conductance represented as a percentage of maximum for each region at control and during bretylium tosylate (BT) intervention (Panel A). Initial peak (onset of warming protocol) percent contribution of sympathetic noradrenergic nerves for each region (Panel B). * indicates P < 0.05 compared to control. † indicates P < 0.05 compared to arm. ‡ indicates P < 0.05 compared to BT treated arm
Plateau Phase
During the plateau phase, with T loc maintained at 42 °C for 35 min, CVC at the control sites averaged 89 ± 4 and 98 ± 2 %max in the forearms and legs, respectively (P = 0.019) (Fig. 4a). CVC responses at forearm and leg sites treated with BT were 69 ± 5 and 90 ± 4 %max, respectively (P < 0.001). At a T loc of 42 °C, CVC was significantly lower at the BT-treated sites when compared to the untreated control sites for forearms (P < 0.001) and legs (P = 0.027). The percent contribution of noradrenergic sympathetic function during the plateau to sustained local heating is presented in Fig. 4b. The contribution to the vasodilator response of the forearm, 22 ± 3 %, is significantly greater than the leg, 8 ± 4 % (P < 0.01).
Plateau phase (42 °C) cutaneous vascular conductance represented as a percentage of maximum for each region at control and during bretylium tosylate (BT) intervention (Panel A). Plateau phase (42 °C) percent contribution of sympathetic noradrenergic nerves for each region (Panel B). * indicates P < 0.05 compared to control. † indicates P < 0.05 compared to arm. ‡ indicates P < 0.05 compared to BT treated arm
CVC data not normalized to maximal dilatation
When the data are expressed as absolute CVC (mV mmHg−1), and not normalized to maximum, the BT-treated forearm and leg sites were significantly different from their respective control sites through all phases of the protocol (Table 1). Limb comparison data show that the leg exhibited significantly higher CVC values at baseline (33 °C). However, during the initial peak, there was no statistical difference between the forearm and the leg. During the prolonged plateau phase, the leg CVC was greater than that of the forearm. Following the administration of SNP to induce a pharmacological maximum CVC, the two limb sites were statistically the same.
Time to onset of vasodilatation, initial peak, nadir, and plateau
As can be seen in Fig. 5a, the time to onset of vasodilatation differed when comparing the forearm (19.9 ± 1.9 s) and the leg (38.9 ± 2.1 s) at control sites (P = 0.001). Additionally, after BT treatment, the onset of vasodilatation in the forearms and legs (72.6 ± 4.8 s forearms and 104.2 ± 3.0 s legs) was further delayed in comparison to control sites and remained statistically different (P = 0.001).
Temporal variations in vasodilatation to local skin warming at a rate of 0.5 °C 10 s−1 between the arm and leg with and without pre-synaptically blocked noradrenergic sympathetic nerve function via bretylium tosylate (BT) treatment. Time to onset of vasodilatation (Panel A), initial peak (Panel B), nadir (Panel C), and plateau (Panel D) is presented. * indicates P < 0.05 compared to control. † indicates P < 0.05 compared to arm. ‡ indicates P < 0.05 compared to BT treated arm
The delay in vasodilatation observed in the leg when compared to the forearm continued through the formation of the initial peak, with the leg (139.8 ± 4.9 s) taking longer than the forearm (118.2 ± 2.1 s) at control sites (Fig. 5b). With BT treatment, this delay of vasodilatation was further exaggerated between the forearm (130.9 ± 4.6 s) and the leg (202.2 ± 9.6 s) and was significantly different from the respective control site (P < 0.001) and corresponding limb (P < 0.001).
The time to the nadir phase of the skin blood flow response during local skin heating was longer in the legs (155.0 ± 4.2 s) compared to the forearms (131.4 ± 1.8 s; P = 0.001) (Fig. 5c). This delay in the time course of the skin blood flow response was also observed with the administration of BT (158.6 ± 6.6 vs. 299.7 ± 7.8 s, forearms and legs, respectively; P < 0.001).
The time to the plateau phase was longer in the legs compared to the forearms at control sites (P < 0.001) (Fig. 5d). When comparing the BT-treated sites to the control sites, both the forearm and leg BT-treated sites were slower to achieve plateaus (P < 0.001 for both). However, there was no difference in duration between BT-treated sites of the forearms and the legs (P > 0.05).
Discussion
This study aimed to determine if the previously observed regional differences in the initial skin blood flow response to local skin heating between the forearm and leg (Del Pozzi et al. 2013) was due to the involvement of cutaneous noradrenergic sympathetic nerves. The initial skin blood flow response to local skin heating was reduced in both limbs when noradrenergic sympathetic nerves were blocked, and the reduction was greater in the forearms than in the legs. Cutaneous noradrenergic sympathetic nerves do not appear to completely explain the observed differences in the initial vasodilator responses to skin heating. Additionally, we found that under conditions of noradrenergic sympathetic nerve blockade, basal skin blood flow increased similarly in both forearms and legs. Finally, the sustained vasodilatation to maintained local skin heating was also reduced in both limbs following the sympathetic nerve block. The reduction was greater in the forearms compared to the legs. These data indicate that the contributions of noradrenergic sympathetic nerves to the control of skin blood flow at rest and during vasodilatation in response to local skin heating differ between the forearm and the leg.
We previously reported leg CVC was higher at baseline than the forearm under the control conditions (Del Pozzi et al. 2013; Hodges and Del Pozzi 2014), this persisted under BT treatment, with basal CVC increasing in both forearms and legs (Fig. 1). These data suggest a similar role for sympathetic nerves in the tonic vasoconstriction of the cutaneous vasculature at thermoneutral temperatures. Our previous data indicated that the differences in basal CVC between the forearm and leg could be almost entirely explained by greater NOS activity (Del Pozzi et al. 2013). In contrast to our findings, Yamazaki and Yuge (2011) found that when CVC is normalized to either baseline or maximal values, CVC of the legs and forearms was of similar levels. The methods and protocols used in the studies could explain the differences seen by the two laboratories. While Yamazaki and Yuge (2011) infused phenylephrine at seven increasing concentrations from 10−8 to 10−2 M simultaneously at the forearm and leg sites over 70 min, we heated the skin while pre-synaptically blocking the sympathetic neurotransmitters via BT administration. As well, taking the measurements on both extremities on the same or different days may have an influence on the results. During preliminary testing for our previous study examining regional differences (Del Pozzi et al. 2013), we found that the requirement to immobilize both the forearm and the leg of the participant led to marked complaints of discomfort, which seemed to affect the observed outcomes (data neither presented nor statistically analyzed). Consequently, we decided that investigating each limb separately would be the best avenue for our exploration of regional differences.
While there have been reports of BT abolishing the initial peak response in the skin of the forearm to local heating (Houghton et al. 2006; Hodges et al. 2009b), this seems to occur only during very slow local skin heating (0.1 °C min−1). In the present study, using a more rapid rate of skin heating (3 °C min−1), we found that BT only reduced the initial peak response, similar to previous studies employing faster heating rates and pre- and post-synaptic noradrenergic blockades (Hodges and Sparks 2014; Tew et al. 2011d; Carter and Hodges 2011; Hodges et al. 2009b). We also observed a similar effect on the initial peak and plateau responses in the leg skin sites treated with BT; however, an unexpected finding was that the contribution of sympathetic function was less in the legs than in the forearms (Figs. 2b, 3b). Previously, we postulated that the legs experience greater tonic vasoconstriction (and consequently increased noradrenergic activity), based on the findings that the physiological maximum reached in the legs at a local skin temperature of 42 °C accounts for a greater proportion of total blood flow achievable at a pharmacological max (CVC in response to SNP: Del Pozzi et al. 2013, observations confirmed in the present study). Furthermore, previous reports by other investigators found greater α-sensitivity to exogenous α-adrenoceptor agonists in the legs compared to the forearms (Yamazaki and Yuge 2011; Pawelczyk and Levine 2002), resulting in the hypothesis that the vasculature of the leg experiences a higher α-sensitivity to the noradrenergic nerve function. However, our current data from directly blocking sympathetic nerve function do not support this supposition. Furthermore, Yamazaki (2012) reported no difference between the vasoconstrictor responses of the forearm and leg in response to local skin cooling. Thus, it appears that cutaneous vascular responses to physiological stimuli and exogenous adrenergic agonists differ.
Increased peak CVC (plateau phase) in the legs when compared to the forearms is consistent with our previous findings (Del Pozzi et al. 2013). BT treatment had a marked effect on the plateau phase (sustained vasodilatation) in both limbs, indicating a role for sympathetic noradrenergic nerves and the involvement of the neurotransmitters NA and neuropeptide Y. This finding is similar to previous work examining the role of noradrenergic sympathetic nerves in cutaneous vasodilatation in response to local skin heating (Mosley 1969; Houghton et al. 2006; Hodges et al. 2008; Tew et al. 2011d). The observed smaller role for noradrenergic nerves in this study might be a function of the rate of heating. While the rate of heating employed in the current study is a relatively standard protocol, it is certainly faster than what would normally occur during exposure to a warming environment. Hodges et al. (2009b) showed that with a fast rate of local skin heating, noradrenergic sympathetic nerves appeared to be less involved in the sustained vasodilatation in response to local skin heating. Furthermore, Carter and Hodges (2011) demonstrated that rapid, noxious heating abolished the sympathetic nerve response to local skin heating in both the initial peak and plateau phases in the skin of the forearm. Thus, there does appear to be a rate dependency regarding the involvement of sympathetic nerves in the local heating-induced cutaneous vasodilator response, and this may be affecting the results of the present study.
Not only are the absolute levels of vasodilatation and the degree of involvement of sympathetic nerve different between the vasculatures of the cutaneous circulation at forearm and leg sites, but we have also observed marked temporal differences in the vasodilator responses to local skin heating between the skin of the forearms and the legs (Fig. 4). The onset of vasodilatation is delayed in the skin of the legs compared to the skin of the forearms. Also, each phase of the vasodilator response to local skin heating (initial peak, nadir, and plateau) is delayed in the skin of the leg compared to that of the forearm. Pre-synaptic noradrenergic sympathetic nerve blockade with BT further increased the time to onset, initial peak, nadir, and plateau in both limbs. Interestingly, while BT treatment did further increase the delayed vasodilator response of the leg compared to the forearm for the onset, initial peak, and nadir phases; the time to establishing the plateau phase was not different between the forearm and the leg under conditions of BT treatment.
These data might be helpful in determining the severity of neuropathies found in the microcirculation of disease states such as diabetes (Strom et al. 2010; Sokolnicki et al. 2009, 2007) and peripheral artery disease (Hodges et al. 2014), where complications routinely appear first in the dependent periphery. If noninvasive methods for the detection of peripheral microvascular disease are to be realized, the subtle differences between the mechanisms of action in the microvascular of forearms and the legs must first be elucidated.
Experimental considerations
Because BT works pre-synaptically, we are not able to delineate between the roles of the sympathetic neurotransmitters, NA and neuropeptide Y, which could be involved in the sympathetic response to local heating, as has been performed in the forearm previously (Tew et al. 2011c; Hodges et al. 2008). Additionally, Hodges and Sparks (2013) demonstrated that the effects of antagonism of α-adrenoceptors after establishing the sustained vasodilatation (plateau phase) to local skin heating had no effect on this phase. Consequently, interpretation of the current effects of sympathetic blockade on both forearm and leg skin must also consider that the drugs were administered prior to the application of local skin heating. Finally, we reported that noradrenergic sympathetic blockade increased basal skin blood flow similarly in both forearms and legs. It is clear from the current study that the higher basal level of CVC in the legs is not due to sympathetic transmission. It is possible as previously suggested (Del Pozzi et al. 2013), that the higher basal levels are due to NOS. However, further systematic investigations are needed. Importantly, whether this difference is due to eNOS or nNOS isoforms is still unclear, as previously it has been suggested that the cutaneous vasodilator response in the forearm is due to eNOS (Kellogg et al. 2008a) and not nNOS (Kellogg et al. 2008b, 2009), while in legs, local heating-induced vasodilatation appears to be mediated primarily by nNOS (Stewart et al. 2007).
Conclusions
The present study clearly demonstrates that the contribution of noradrenergic sympathetic nerves in the cutaneous vasodilator response to local skin heating differs between the legs and forearms depending on the phase of the skin blood flow response. Under thermoneutral conditions, noradrenergic sympathetic nerve blockade increases both forearm and leg skin blood flow. In response to increased local skin temperature, the initial peak and plateau phases are both attenuated at forearm and leg sites under noradrenergic sympathetic nerve blockade, the effects of which are greater in the vasculature of the forearm compared to the leg. Additionally, the time to onset for each phase of the vasodilator response is greater in the leg compared to the forearm. These data support previous work that mechanisms of control of the cutaneous circulation are different between the forearm and the leg. Consequently, examination of different regions of skin requires the appropriate controls. As a result, comparisons among regions must consider these mechanistic differences.
Abbreviations
- BT:
-
Bretylium tosylate
- CVC:
-
Cutaneous vascular conductance
- EDHF:
-
Endothelial-derived hyperpolarizing factor
- eNOS:
-
Endothelial nitric oxide synthase
- LDF:
-
Laser-Doppler flow
- T loc :
-
Local skin temperature
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- NA:
-
Noradrenaline
- nNOS:
-
Neuronal nitric oxide synthase
- SNP:
-
Sodium nitroprusside
References
Anderson C, Andersson T, Wardell K (1994) Changes in skin circulation after insertion of a microdialysis probe visualized by laser Doppler perfusion imaging. J Invest Dermatol 102(5):807–811
Brunt VE, Minson CT (2012) KCa channels and epoxyeicosatrienoic acids: major contributors to thermal hyperaemia in human skin. J Physiol 590(Pt 15):3523–3534. doi:10.1113/jphysiol.2012.236398jphysiol.2012.236398
Carter SJ, Hodges GJ (2011) Sensory and sympathetic nerve contributions to the cutaneous vasodilator response from a noxious heat stimulus. Exp Physiol 96(11):1208–1217. doi:10.1113/expphysiol.2011.059907expphysiol.2011.059907
Charkoudian N (2001) Influences of female reproductive hormones on sympathetic control of the circulation in humans. Clin Auton Res 11(5):295–301
Cracowski JL, Gaillard-Bigot F, Cracowski C, Roustit M, Millet C (2011) Skin microdialysis coupled with laser speckle contrast imaging to assess microvascular reactivity. Microvasc Res 82(3):333–338. doi:10.1016/j.mvr.2011.09.009S0026-2862(11)00167-1
Cross A, Collard M, Nelson A (2008) Body segment differences in surface area, skin temperature and 3D displacement and the estimation of heat balance during locomotion in hominins. PLoS One 3(6):e2464. doi:10.1371/journal.pone.0002464
Del Pozzi AT, Carter SJ, Collins AB, Hodges GJ (2013) The regional differences in the contribution of nitric oxide synthase to skin blood flow at forearm and lower leg sites in response to local skin warming. Microvasc Res 90:106–111
Hodges GJ, Del Pozzi AT (2014) Noninvasive examination of endothelial, sympathetic, and myogenic contributions to regional differences in the human cutaneous microcirculation. Microvasc Res 93:87–91. doi:10.1016/j.mvr.2014.04.002S0026-2862(14)00062-4
Hodges GJ, Sparks PA (2013) Contributions of endothelial nitric oxide synthase, noradrenaline, and neuropeptide Y to local warming-induced cutaneous vasodilatation in men. Microvasc Res. doi:10.1016/j.mvr.2013.08.011
Hodges GJ, Sparks PA (2014) Noradrenaline and neuropeptide Y contribute to initial, but not sustained, vasodilatation to local skin warming in humans. Exp Physiol 99(2):381–392. doi:10.1113/expphysiol.2013.075549
Hodges GJ, Kosiba WA, Zhao K, Johnson JM (2008) The involvement of norepinephrine, neuropeptide Y, and nitric oxide in the cutaneous vasodilator response to local heating in humans. J Appl Physiol 105(1):233–240. doi:10.1152/japplphysiol.90412.2008
Hodges GJ, Chiu C, Kosiba WA, Zhao K, Johnson JM (2009a) The effect of microdialysis needle trauma on cutaneous vascular responses in humans. J Appl Physiol 106(4):1112–1118. doi:10.1152/japplphysiol.91508.2008
Hodges GJ, Kosiba WA, Zhao K, Johnson JM (2009b) The involvement of heating rate and vasoconstrictor nerves in the cutaneous vasodilator response to skin warming. Am J Physiol Heart Circ Physiol 296(1):H51–56. doi:10.1152/ajpheart.00919.2008
Hodges GJ, Nawaz S, Tew GA (2014) Evidence that reduced nitric oxide signal contributes to cutaneous microvascular dysfunction in peripheral arterial disease. Clin Hemorheol Microcirc. doi:10.3233/CH-141838
Houghton BL, Meendering JR, Wong BJ, Minson CT (2006) Nitric oxide and noradrenaline contribute to the temperature threshold of the axon reflex response to gradual local heating in human skin. J Physiol 572(Pt 3):811–820. doi:10.1113/jphysiol.2005.104067
Johnson JM (1990) The cutaneous circulation. In: Shepherd AP, Öberg PÅ (eds) Laser-Doppler blood flowmetry. Developments in cardiovascular medicine, vol 107. Springer, pp 121–139
Johnson JM, Proppe DW (1996) Cardiovascular adjustments to heat stress. Handbook of Physiology, Environmental Physiology, vol I. Am Physiol Soc, Bethesda, pp 215–243
Johnson JM, Taylor WF, Shepherd AP, Park MK (1984) Laser-Doppler measurement of skin blood flow: comparison with plethysmography. J Appl Physiol 56(3):798–803
Johnson JM, Minson CT, Kellogg DL Jr (2014) Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr Physiol 4(1):33–89. doi:10.1002/cphy.c130015
Kellogg DL Jr, Liu Y, Kosiba IF, O’Donnell D (1999) Role of nitric oxide in the vascular effects of local warming of the skin in humans. J Appl Physiol 86(4):1185–1190
Kellogg DL Jr, Zhao JL, Coey U, Green JV (2005) Acetylcholine-induced vasodilation is mediated by nitric oxide and prostaglandins in human skin. J Appl Physiol 98(2):629–632. doi:10.1152/japplphysiol.00728.2004
Kellogg DL Jr, Zhao JL, Wu Y (2008a) Endothelial nitric oxide synthase control mechanisms in the cutaneous vasculature of humans in vivo. Am J Physiol Heart Circ Physiol 295(1):H123–129. doi:10.1152/ajpheart.00082.2008
Kellogg DL Jr, Zhao JL, Wu Y (2008b) Neuronal nitric oxide synthase control mechanisms in the cutaneous vasculature of humans in vivo. J Physiol 586(3):847–857. doi:10.1113/jphysiol.2007.144642
Kellogg DL Jr, Zhao JL, Wu Y (2009) Roles of nitric oxide synthase isoforms in cutaneous vasodilation induced by local warming of the skin and whole body heat stress in humans. J Appl Physiol 107(5):1438–1444. doi:10.1152/japplphysiol.00690.2009
Minson CT, Berry LT, Joyner MJ (2001) Nitric oxide and neurally mediated regulation of skin blood flow during local heating. J Appl Physiol 91(4):1619–1626
Minson CT, Holowatz LA, Wong BJ, Kenney WL, Wilkins BW (2002) Decreased nitric oxide- and axon reflex-mediated cutaneous vasodilation with age during local heating. J Appl Physiol 93(5):1644–1649. doi:10.1152/japplphysiol.00229.2002
Mosley JG (1969) A reduction in some vasodilator responses in free-standing man. Cardiovasc Res 3(1):14–21
Öberg PA (1990) Laser-Doppler flowmetry. Crit Rev Biomed Eng 18:125–163
Park MK, Guntheroth WG (1970) Direct blood pressure measurements in brachial and femoral arteries in children. Circulation 41(2):231–237
Pawelczyk JA, Levine BD (2002) Heterogeneous responses of human limbs to infused adrenergic agonists: a gravitational effect? J Appl Physiol 92(5):2105–2113. doi:10.1152/japplphysiol.00979.2001
Sareen P, Saxena K, Sareen B, Taneja B (2012) Comparison of arm and calf blood pressure. Indian J Anaesth 56(1):83–85. doi:10.4103/0019-5049.93354IJA-56-83
Sokolnicki LA, Roberts SK, Wilkins BW, Basu A, Charkoudian N (2007) Contribution of nitric oxide to cutaneous microvascular dilation in individuals with type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 292(1):E314–318
Sokolnicki LA, Strom NA, Roberts SK, Kingsley-Berg SA, Basu A, Charkoudian N (2009) Skin blood flow and nitric oxide during body heating in type 2 diabetes mellitus. J Appl Physiol 106(2):566–570. doi:10.1152/japplphysiol.91289.2008
Stephens DP, Bennett LA, Aoki K, Kosiba WA, Charkoudian N, Johnson JM (2002) Sympathetic nonnoradrenergic cutaneous vasoconstriction in women is associated with reproductive hormone status. Am J Physiol Heart Circ Physiol 282(1):H264–272
Stewart JM, Medow MS, Minson CT, Taneja I (2007) Cutaneous neuronal nitric oxide is specifically decreased in postural tachycardia syndrome. Am J Physiol Heart Circ Physiol 293(4):H2161–2167. doi:10.1152/ajpheart.00600.2007
Stewart JM, Nafday A, Ocon AJ, Terilli C, Medow MS (2011) Cutaneous constitutive nitric oxide synthase activation in postural tachycardia syndrome with splanchnic hyperemia. Am J Physiol Heart Circ Physiol 301(3):H704–711. doi:10.1152/ajpheart.00171.2011
Strom NA, Sawyer JR, Roberts SK, Kingsley-Berg SM, Charkoudian N (2010) Local sensory nerve control of skin blood flow during local warming in type 2 diabetes mellitus. J Appl Physiol 108(2):293–297. doi:10.1152/japplphysiol.01077.200901077.2009
Taylor WF, Johnson JM, O’Leary D, Park MK (1984) Effect of high local temperature on reflex cutaneous vasodilation. J Appl Physiol 57(1):191–196
Tew GA, Klonizakis M, Crank H, Briers JD, Hodges GJ (2011a) Comparison of laser speckle contrast imaging with laser Doppler for assessing microvascular function. Microvasc Res. doi:10.1016/j.mvr.2011.07.007
Tew GA, Klonizakis M, Moss J, Ruddock AD, Saxton JM, Hodges GJ (2011b) Reproducibility of cutaneous thermal hyperaemia assessed by laser Doppler flowmetry in young and older adults. Microvasc Res 81(2):177–182. doi:10.1016/j.mvr.2010.12.001
Tew GA, Klonizakis M, Moss J, Ruddock AD, Saxton JM, Hodges GJ (2011c) Role of sensory nerves in the rapid cutaneous vasodilator response to local heating in young and older endurance-trained and untrained men. Exp Physiol 96(2):163–170. doi:10.1113/expphysiol.2010.055434
Tew GA, Saxton JM, Klonizakis M, Moss J, Ruddock AD, Hodges GJ (2011d) Aging and aerobic fitness affect the contribution of noradrenergic sympathetic nerves to the rapid cutaneous vasodilator response to local heating. J Appl Physiol. doi:10.1152/japplphysiol.01423.2010
Wong BJ (2013) Sensory nerves and nitric oxide contribute to reflex cutaneous vasodilation in humans. Am J Physiol Regul Integr Comp Physiol 304(8):R651–656. doi:10.1152/ajpregu.00464.2012
Yamazaki F (2012) Oral vitamin C enhances the adrenergic vasoconstrictor response to local cooling in human skin. J Appl Physiol 112(10):1689–1697
Yamazaki F, Yuge N (2011) Limb-specific differences in the skin vascular responsiveness to adrenergic agonists. J Appl Physiol 111(1):170–176. doi:10.1152/japplphysiol.00068.2011
Acknowledgments
We thank the participants for their time and commitment to this study. We also thank Dr. Stephen J. Carter and Ms. Ann B. Collins for their help in participant recruitment and screening and with data collection. This study was conducted by Andrew T. Del Pozzi in partial fulfillment of the requirements for the Doctor of Philosophy degree in the Department of Kinesiology at The University of Alabama. Finally, we thank Dr. Stephen S. Cheung for his critical review of the manuscript.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Narihiko Kondo.
Rights and permissions
About this article
Cite this article
Del Pozzi, A.T., Hodges, G.J. Comparison of the noradrenergic sympathetic nerve contribution during local skin heating at forearm and leg sites in humans. Eur J Appl Physiol 115, 1155–1164 (2015). https://doi.org/10.1007/s00421-014-3097-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-014-3097-1