Abstract
Purpose
To compare laser photocoagulation and intravitreal injection of bevacizumab (IVB) treatment for retinopathy of prematurity (ROP).
Methods
The study included 52 eyes of 26 patients after ROP treatment who were observed up to 5 years of age. Twenty-eight eyes received laser photocoagulation as the initial treatment (laser group), and twenty-four eyes underwent IVB (IVB group). We collected data on gestational age, birth weight, 1- and 5-min Apgar scores, zone and stage at the time of treatment, recurrence of ROP and best-corrected visual acuity (BCVA) (logMAR), equivalent spherical value (SE), ocular complications, and developmental delay at the age of 5.
Results
More zone I low-stage eyes were treated with IVB than laser. There was no difference in BCVA (p = 0.836). Although the mean SE was not different between the groups (p = 0.280), the prevalence of myopia was significantly higher in the laser group (p = 0.020). Developmental delay was observed in 3 of 14 and 3 of 12 cases in the laser and IVB groups, respectively (p = 0.596). Retinal holes were observed in 2 eyes in the IVB group, with 1 developing localized retinal detachment. There were no significant differences between the groups in the other factors.
Conclusions
Compared to laser for ROP, IVB was not inferior in neurodevelopment or visual outcome and was superior in refractive error. As cases in the IVB group showed retinal holes, long-term follow-up with fundus examination is recommended after IVB.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is one of the most common causes of visual disability and blindness in children. Laser photocoagulation of the avascular retina is the current standard treatment for ROP [1] and is highly successful [2]. However, adverse effects such as laser-induced myopia [3], visual field reduction [4], and suboptimal visual results [5] have been reported. In 2007, anti-vascular endothelial growth factor (VEGF) intravitreal therapy appeared as a new treatment modality for ROP [6]. The BEAT-ROP study showed that the recurrence rate was lower with intravitreal injection of bevacizumab (IVB) than laser treatment in the zone I stage 3 ROP [7]. The advantages of anti-VEGF treatment compared with laser treatment include the ease and speed of injection under topical anesthesia, faster regression of active ROP [8], lower rates of severe myopia after treatment [3], and lesser visual field reduction [4]. However, there are concerns about the long-term effects on ocular health and potential influence on neurodevelopment after anti-VEGF therapy because VEGF is critical for retinal vascular development [9] and neurogenesis during brain development [10]. Moreover, a previous study reported that patients with eyes treated with IVB had peripheral retinal abnormalities at 9 months old, including large avascular area, abnormal branching, and shunt [11]. Eyes with peripheral retinal abnormalities have a risk of retinal diseases such as a retinal hole or rhegmatogenous retinal detachment. However, no information is available on the long-term ocular safety of IVB for ROP. Regarding neurodevelopment, Morin et al. [12] reported that more neurodevelopmental impairment was observed after IVB than after laser treatment at 18 months of age. In addition, Kennedy et al. and Lien et al. [13, 14] reported that there was no significant difference in neurodevelopment between IVB and laser at 18 to 22 and 24 months of age, respectively. However, no previous studies have assessed the neurodevelopmental outcome of preschool children who were treated for ROP with IVB. The purpose of this study was to compare ocular and neurodevelopmental safety and treatment results at 5 years of age between laser and IVB therapies.
Methods
We studied a series of consecutive patients who underwent treatment for ROP at the University of Tsukuba Hospital between October 2007 and October 2014. This retrospective cohort study was approved by the Institutional Review Board of the Tsukuba University Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki. All parents provided written informed consent before ROP treatment.
Retinopathy of prematurity was defined according to the International Committee for Classification of ROP protocol [15]. The indications for treatment included patients whose retinopathy met the criteria (type 1 ROP) established by the Early Treatment for Retinopathy of Prematurity Study (ETROP) [16]. The staging and treatment determination were performed by a single pediatric retinal specialist (Y.O.). Treatment, if required, was performed within 72 h of type 1 ROP diagnosis. Before January 2012, all patients with type 1 ROP received laser photocoagulation as the first-line treatment. After the publication of the BEAT-ROP study, IVB was offered as a possible alternative to laser therapy for type 1 ROP. The parents were offered the choice of laser or IVB after the pros and cons of each treatment had been fully explained. We also explained the status of the off-label use of IVB for ROP treatment. The final decision to treat with laser or IVB was made by the parents. Between January 2012 and October 2014, all parents selected IVB.
All treatments were performed by a single pediatric retinal specialist (Y.O.). When intubation was deemed necessary to treat ROP, the patients were intubated. We used fentanyl (1–3 μg/kg per dose) as an anesthetic during intubation and before and during the treatment. All laser treatments were performed using an argon laser indirect ophthalmoscope (OcuLight SLx, Iridex Corporation, Mountain View, CA, USA). The laser treatment was applied at the following settings: wavelength, 515 nm; duration, 0.3 s; and power, 250–350 mW. Before IVB, the ocular surface was anesthetized with 4% lidocaine (Xylocaine) eye drops. The eyelids and conjunctiva were rinsed with 5% povidone–iodine. A sterile eyelid speculum was inserted, and bevacizumab 0.625 mg (total volume, 0.025 mL) was injected into the vitreous cavity via the pars plana.
Recurrences requiring additional treatment after laser or IVB were defined as recurrence plus disease or progressive extraretinal proliferation. Patients requiring additional laser treatment within 2 weeks after initial treatment due to incomplete laser treatment were not considered to be recurrences. One pediatric retinal specialist (Y.O.) selected laser or IVB as the secondary treatment.
Data collection
The following parameters were collected from the patients’ records: gestational age; birth weight; 1- and 5-min Apgar scores; the presence of respiratory distress syndrome, sepsis, intraventricular hemorrhage, and necrotic enteritis; duration of oxygen therapy and ventilation, ROP zone, and stage at the time of treatment. Outcome parameters were recurrence rate of ROP, best-corrected visual acuity (BCVA), spherical equivalent (SE), presence of myopia, ocular side effects, developmental delay, and intelligence quotient (IQ) or developmental quotient (DQ) score at 5 years of age. We also collected the data regarding the total amount of fentanyl used and whether the patient was reintubated during the treatment.
Best-corrected visual acuity was measured with the Landolt chart and expressed as a logarithm of minimal angle resolution (logMAR). Cycloplegic refraction was measured with an auto ref-keratometer (RC-5000, Tomey Corporation, Nagoya, Japan), and the SE was noted. Myopia was defined as a condition in which the SE was ≤−0.5 diopter (D) [17]. Development was evaluated at 5 years of age. If possible, the Wechsler Intelligence Scale for Children IV (WISC IV) was used, and the intelligence quotient (IQ) was measured. If the patients were difficult to test with the WISC IV, we used the Kyoto Scale of Psychological Development (KSPD). The KSPD is a standard test in Japan in which developmental quotient (DQ) is derived. It is considered that DQ is similar to IQ [18, 19]. An IQ or DQ (IQ/DQ) score of <70 was defined as an indicator of developmental delay [20]. Some patients whose development level was estimated as normal by pediatricians were not tested with WISC IV and KSPD, and the IQ/DQ score was assumed to be 100.
Statistical analysis
Unpaired t-tests were used to compare gestational age, birth weight, 1- and 5-min Apgar scores, oxygen administration period, ventilator use period, total amount of fentanyl used, BCVA, SE, and IQ/DQ scores between the laser and IVB groups. Fisher’s exact probability tests were used to compare the presence of respiratory distress syndrome, sepsis, intraventricular hemorrhage and necrotic enteritis, reintubation, ROP zone, plus disease at the time of treatment, the recurrence rate of ROP, ocular side effects, myopia, and developmental disorder at 5 years of age. The Mann–Whitney U-test was used to compare the stage of ROP at the time of treatment. Logistic regression analyses were used to identify factors associated with developmental delay. All analyses were conducted using SPSS (version 26, IBC Corp., Chicago, IL, USA). A p value less than 0.05 was considered statistically significant.
Results
Subjects
We included 52 eyes of 26 patients with ROP. Twenty-eight eyes of 14 infants were treated with laser, and 24 eyes of 12 infants were treated with IVB as the first-line treatment. Baseline characteristics of the 2 groups are shown in Table 1. There were no statistically significant differences between the groups. The status of ROP at the time of treatment is shown in Table 2. In the IVB group, more zone I eyes and a lower stage of eyes were treated than in the laser group (p = 0.039 and p = 0.010, respectively). The total amount of fentanyl used for the treatment of ROP was significantly higher in the laser group (6.5 ± 2.6 μg/kg) than that in the IVB group (1.7 ± 2.5 μg/kg) (p < 0.001). Six patients in the IVB group did not receive fentanyl administration during the treatment. One patient in the IVB group could not be extubated before IVB, while the others in the IVB group and all the patients in the laser group were extubated before the treatment. Reintubation was performed in all the patients in the laser group and one patient in the IVB group. There was a significant difference in the rate of reintubation between both groups (p < 0.001).
Treatment safety and efficacy of retinopathy of prematurity treatment
No recurrence was observed after laser photocoagulation. On the other hand, in the IVB group, 2 of 4 eyes with zone I and 2 of 20 eyes with zone II ROP needed additional treatment due to recurrence. The two eyes with zone I ROP underwent additional laser 10 weeks after IVB, after which, ROP regressed. Two eyes with zone II ROP underwent additional IVB 8 weeks after initial IVB, after which, ROP temporarily regressed. However, additional laser treatment was needed 3 weeks after the second IVB because additional recurrence was observed in both eyes. Finally, ROP in all eyes in both groups regressed without retinal detachment, corneal opacity, or lens opacity. In zone II ROP, there was no significant difference in recurrence rate between the groups (laser, 0%; IVB, 10%; p = 0.168).
Safety and efficacy results at the age of 5 for ROP are shown in Table 3. There was no significant difference in BCVA and SE at the age of 5 between the two groups (p = 0.836 and p = 0.186, respectively). The prevalence of myopia was significantly higher in the laser group than in the IVB group (p = 0.020).
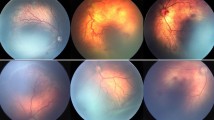
Retinal holes were observed in 2 eyes in the IVB group, of which 1 developed retinal detachment. The patient was reassessed monthly without surgery because the retinal detachment was localized without progression (Fig. 1). In contrast, retinal holes were not observed in the laser group, although there was no significant difference in the incidence of the retinal hole between the groups (p = 0.208). In the laser group, esotropia was observed in 3 patients. Accommodative esotropia was not observed, and the visual acuity of these patients was good. In the IVB group, esotropia was not observed, and there was no significant difference between the groups with regard to the incidence of esotropia (p = 0.140). In the IVB group, intermittent exotropia was observed in 2 patients, whereas it was not observed in the laser group. There was no significant difference between the groups with regard to the incidence of intermittent exotropia (p = 0.208).
Developmental delay at 5 years of age was identified in 3 out of 14 cases in the laser group and 3 out of 12 cases in the IVB group. There was no significant difference between the two groups (p = 0.596) (Table 3). The IQ/DQ scores were 77.9 ± 15.6 in the laser group and 84.0 ± 16.5 in the IVB group, with no significant differences between the two groups (p = 0.352) (Table 3). Logistic regression analyses revealed that the duration of ventilation had a significant predictive value for the presence of developmental delay at 5 years of age (beta 0.11; OR 1.11; 95% CI 1.02–1.22; p = 0.018; OR and CI for ventilator use period are given per day). Other factors (gestation weeks, birthweight, 1- and 5-min Apgar scores, presence of respiratory distress syndrome, sepsis, intraventricular hemorrhage and necrotic enteritis, duration of oxygen therapy, and the type of first-line treatment [laser or IVB]) had no significant predictive value.
Discussion
In the BEAT ROP study, in eyes with zone I stage 3 ROP, the recurrence rate was lower with IVB than laser treatment. However, few studies have since directly compared the treatments [8, 21]. Mueller et al. and Hwang et al. studied treatment outcomes after IVB versus laser treatment for ROP. Mueller et al. [8] reported no recurrences occurring in infants treated with laser and in 12% of infants treated with IVB. Hwang et al. [21] also reported a similar recurrence rate with both laser and IVB (zone I, 19 and 20%; zone II, 0 and 0%, respectively). In our study, there was no significant difference between the laser and IVB groups in the recurrence rate of zone II ROP (0 and 10%, respectively). Judging from previous reports and our results, we considered that, in terms of recurrence rate, there might not be a large difference between laser and IVB for zone II ROP.
In this study, no significant difference was observed between the groups in visual acuity at the age of 5. Previous studies have compared visual outcomes between patients treated with IVB and laser and reported that no significant difference was observed in visual acuity between the treatment groups at the ages of 1 [8] and 4 to 6 [22] years. Judging from previous studies and our study, we considered IVB to have the same therapeutic effect on visual acuity as laser.
In this study, myopia was observed more frequently in the laser group than in the IVB group. Previous studies have assessed the influences of IVB and laser on refractive error. Geloneck et al. [3] investigated refractive error in the BEAT-ROP cohort at 2.5 years of age. They reported that the prevalence of very high myopia (≦−8.00 D) was higher in eyes that received laser than in eyes that received IVB. Lee et al. [22] studied the influence of IVB and laser on the refractive error in 4 to 6 years old children after ROP treatment and reported that eyes treated with laser had a significantly higher degree of myopia. Judging from previous reports and our study, we determined that the risk of myopia is lower in eyes treated with IVB than in eyes treated with laser.
In the IVB group, retinal holes were observed in 2 eyes, with retinal detachment observed in 1 of the 2 eyes. To the best of our knowledge, no studies have reported cases of a retinal hole or rhegmatogenous retinal detachment in eyes with regressed ROP after anti-VEGF therapy. VEGF plays an important role in normal retinal vascular development [9], and thus, anti-VEGF treatment in neonatal eyes may affect normal vascular growth. Lepore et al. studied the structural outcome at 4 years of age in eyes treated with IVB using fluorescein angiography. They reported that all eyes treated with IVB showed abnormalities at the periphery, such as avascular area, vessel leakage, shunts, abnormal vessel branching, and tangles; whereas a small number of eyes treated with laser showed abnormalities at the periphery [23]. Hamad et al. [24] studied late-onset retinal findings and complications in untreated ROP and reported that, of patients with avascular retina, 84.1% showed associated peripheral retinal findings such as lattice-like changes, retinal holes, and retinal tears. We speculate that some eyes have a large avascular area in the peripheral retina after IVB treatment. Therefore, they might have an increased lifetime risk of a retinal hole or retinal detachment compared with eyes treated with laser. Yoon et al. reported anti-VEGF with deferred laser therapy. They performed laser therapy on the avascular retina extending to the ora serrata after retinal vascularization following IVB treatment. They reported that anti-VEGF with deferred laser therapy yielded better anatomical outcomes (without retinal fold, disc dragging, retrolental tissue obscuring the view of the posterior pole, or retinal detachment) and lesser myopic refractive error than conventional laser therapy [25]. We suspected that it might be more effective to conduct laser treatment on the avascular retina after IVB to reduce the risk of retinal detachment throughout the lifetime of ROP patients. Snyder et al. [26] reported a case of ROP reactivation at 2.5 years of age after bevacizumab monotherapy. Laser on the avascular retina after IVB may also prevent late recurrence, as reported by Snyder et al. Further investigation is needed to compare the incidence of retinal detachment or late recurrence between IVB monotherapy and IVB with deferred laser therapy.
Esotropia was observed in 3 of 14 patients (21.4%) in the laser group and was not observed in the IVB group. However, there was no significant difference between the laser and the IVB groups in the incidence of esotropia. Gnanaraj et al. [27] studied long-term results following cryotherapy or laser photocoagulation for ROP and reported that esotropia was observed in 27.3% of patients. Our result is consistent with theirs. Intermittent exotropia was observed in 2 of 12 patients (16.7%) in the IVB group in this study. Wu et al. [28] reported that exotropia was observed in 1% of eyes treated with bevacizumab, a lower incidence rate than that in our study. The reason for this discrepancy is unclear. The age at examination was 1.5 years in the aforementioned study, so exotropia might have been overlooked due to the difficultly of testing strabismus.
VEGF is considered to be crucial for the development of organs in infants [29]. Disturbance of vascular development at the cerebral level could be detrimental to brain development. Thus, the influence of anti-VEGF therapy for ROP on neurodevelopment is of concern, and this concern has triggered research assessing the influence of IVB on neurodevelopment. Morin et al. [12] reported that IVB may be associated with higher rates of neurodevelopmental impairment at 1.5 years of age in comparison with laser. Kennedy et al. and Lien et al. [13, 14] reported that, in terms of developmental outcomes, there was no significant difference between IVB and laser at 18 to 22 and at the corrected age of 24 months, respectively. However, there are no studies on the long-term safety of anti-VEGF therapy for ROP with regard to neurodevelopment. In this study, the incidence of developmental delay and IQ/DQ scores were not significantly different between the laser and the IVB groups at 5 years of age. Logistic regression analysis revealed that only the duration of ventilation was an independent risk factor for developmental delay, while the type of treatment (laser or IVB) did not show any significant association with developmental delay. Walsh et al. [30] investigated the risk factors for an 18-month neurodevelopmental disability among extremely low birth weight (501 to 1000 g) infants and reported that the risk of neurodevelopmental disability increased if the infant required protracted mechanical ventilation. Their result is consistent with ours. Based on the results of previous studies and our study, IVB is likely to be as safe for neurodevelopment as laser in the long term for ROP treatment. We considered that the general conditions of the infants, and not the treatment procedure for ROP, might have an influence on their neurodevelopment.
The total amount of fentanyl used and rate of reintubation was lower in the IVB group than those in the laser group. Novitskaya et al. [31] investigated anesthetic procedures for ROP interventions in the UK, and they reported that fewer patients who received intravitreal injections received general anesthesia, intravenous sedation, and intubation than those who received laser injections. Based on this result as well as our own findings, we concluded that IVB can be performed with lighter anesthesia than laser therapy.
The limitations of this study include that it is a retrospective historical control study and the relatively small number of patients. Moreover, more zone I low-stage eyes were treated with IVB than laser. Laser therapy can contribute to visual field constriction, especially in the zone I ROP; thus, we considered that IVB tended to be chosen as the preferred treatment of zone I ROP. In the IVB group, a lower stage of eyes was generally treated than in the laser group. It is known that IVB may induce fibrous contractions followed by tractional retinal detachment in ROP with proliferative tissue [32]; thus, we considered that laser therapy tended to be chosen as the preferred treatment of a higher stage of ROP. In terms of development tests, 5 patients who were assessed as developing normally by pediatricians were not tested with WISC IV. Further prospective studies which are well matched for the zone and stage of ROP with larger sample sizes are needed.
In conclusion, there was no significant difference in BCVA between the 2 groups, and the prevalence of myopia was significantly lower in the IVB group than in the laser group. There was no significant difference in the incidence of developmental delay and IQ/DQ scores at the age of 5 between the groups. Retinal hole and localized retinal detachment were observed in a few cases in the IVB group. Thus, long-term follow-up with fundus examinations might be required after IVB due to the potential lifetime risk of retinal detachment.
References
Hartnett ME, Penn JS (2012) Mechanisms and management of retinopathy of prematurity. N Engl J Med 367:2515–2526
Hurley BR, McNamara JA, Fineman MS et al (2006) Laser treatment for retinopathy of prematurity: evolution in treatment technique over 15 years. Retina 26:S16–S17
Geloneck MM, Chuang AZ, Clark WL et al (2014) Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol 132:1327–1333
McLoone E, O’Keefe M, McLoone S, Lanigan B (2007) Effect of diode laser retinal ablative therapy for threshold retinopathy of prematurity on the visual field: results of Goldmann perimetry at a mean age of 11 years. J Pediatr Ophthalmol Strabismus 44:170–173
Mutlu FM, Sarici SU (2013) Treatment of retinopathy of prematurity: a review of conventional and promising new therapeutic options. Int J Ophthalmol 6:228–236
Chung EJ, Kim JH, Ahn HS, Koh HJ (2007) Combination of laser photocoagulation and intravitreal bevacizumab (Avastin) for aggressive zone I retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 245:1727–1730
Mintz-Hittner HA, Kennedy KA, Chuang AZ, BEAT-ROP Cooperative Group (2011) Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 364:603–615
Mueller B, Salchow DJ, Waffenschmidt E et al (2017) Treatment of type I ROP with intravitreal bevacizumab or laser photocoagulation according to retinal zone. Br J Ophthalmol 101:365–370
Sarlos S, Rizkalla B, Moravski CJ, Cao Z, Cooper ME, Wilkinson-Berka JL (2003) Retinal angiogenesis is mediated by an interaction between the angiotensin type 2 receptor, VEGF, and angiopoietin. Am J Pathol 163:879–887
Rosenstein JM, Krum JM, Ruhrberg C (2010) VEGF in the nervous system. Organogenesis 6:107–114
Lepore D, Quinn GE, Molle F et al (2014) Intravitreal bevacizumab versus laser treatment in type 1 retinopathy of prematurity: report on fluorescein angiographic findings. Ophthalmology 121:2212–2219
Morin J, Luu TM, Superstein R et al (2016) Neurodevelopmental outcomes following bevacizumab injections for retinopathy of prematurity. Pediatrics 137:e20153218
Kennedy KA, Mintz-Hittner HA (2018) Medical and developmental outcomes of bevacizumab versus laser for retinopathy of prematurity. J AAPOS 22:61–65.e1
Lien R, Yu MH, Hsu KH et al (2016) Neurodevelopmental outcomes in infants with retinopathy of prematurity and bevacizumab treatment. PLoS One 11:e0148019
International Committee for the Classification of Retinopathy of Prematurity (2005) The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 123:991–999
Good WV, Early Treatment for Retinopathy of Prematurity Cooperative Group (2004) Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 102:233–250
Flitcroft DI, He M, Jonas JB et al (2019) IMI - Defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Invest Ophthalmol Vis Sci 60:M20–M30
Kawabe K, Kondo S, Matsumoto M et al (2016) Developmental quotient to estimate intelligence in autism spectrum disorder. Pediatr Int 58:963–966
Koyama T, Osada H, Tsujii H, Kurita H (2009) Utility of the Kyoto Scale of Psychological Development in cognitive assessment of children with pervasive developmental disorders. Psychiatry Clin Neurosci 63:241–243
Shibasaki J, Mukai T, Tsuda K et al (2020) Outcomes related to 10-min Apgar scores of zero in Japan. Arch Dis Child Fetal Neonatal Ed 105:64–68
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR (2015) Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology 122:1008–1015
Lee YS, See LC, Chang SH et al (2018) Macular structures, optical components, and visual acuity in preschool children after intravitreal bevacizumab or laser treatment. Am J Ophthalmol 192:20–30
Lepore D, Quinn GE, Molle F et al (2018) Follow-up to age 4 years of treatment of type 1 retinopathy of prematurity intravitreal bevacizumab injection versus laser: fluorescein angiographic findings. Ophthalmology 125:218–226
Hamad AE, Moinuddin O, Blair MP et al (2020) Late-onset retinal findings and complications in untreated retinopathy of prematurity. Ophthalmol Retina 4:602–612
Yoon JM, Shin DH, Kim SJ et al (2017) Outcomes after laser versus combined laser and bevacizumab treatment for type 1 retinopathy of prematurity in zone I. Retina 37:88–96
Snyder LL, Garcia-Gonzalez JM, Shapiro MJ, Blair MP (2016) Very late reactivation of retinopathy of prematurity after monotherapy with intravitreal bevacizumab. Ophthalmic Surg Lasers Imaging Retina 47:280–283
Gnanaraj L, Brennan R, Cottrell DG (2003) Retinopathy of prematurity in practice II: long-term results following treatment for threshold disease. Eye (Lond) 17:189–193
Wu WC, Kuo HK, Yeh PT, Yang CM, Lai CC, Chen SN (2013) An updated study of the use of bevacizumab in the treatment of patients with prethreshold retinopathy of prematurity in Taiwan. Am J Ophthalmol 155:150–158.e1
Gerber HP, Hillan KJ, Ryan AM et al (1999) VEGF is required for growth and survival in neonatal mice. Development 126:1149–1159
Walsh MC, Morris BH, Wrage LA et al (2005) Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr 146:798–804
Novitskaya ES, Dahlmann-Noor AH, Adams GGW, Allen LE (2020) Retinopathy of prematurity treatment in the UK: trends in neonatal anaesthetic support and location of treatment from a national surveillance study. Eur J Pediatr. 179:1603–1607
Honda S, Hirabayashi H, Tsukahara Y, Negi A (2008) Acute contraction of the proliferative membrane after an intravitreal injection of bevacizumab for advanced retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 246:1061–1063
Author information
Authors and Affiliations
Contributions
Design of the study (T.M., A.K., M.N., Y.M., and T.O.); conduct of the study (T.M., Y.S., Y.O., and A.K.); data collection (T.M., F.O., S.H., and M.N.); management, analysis, and interpretation of the data (T.M., F.O., S.H., and M.N.); preparation of the manuscript (T.M. and Y.S.); review of the manuscript (F.O. and T.O.); approval of the manuscript (Y.O., A.K., S.H., M.N., and Y.M.,).
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murakami, T., Sugiura, Y., Okamoto, F. et al. Comparison of 5-year safety and efficacy of laser photocoagulation and intravitreal bevacizumab injection in retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 259, 2849–2855 (2021). https://doi.org/10.1007/s00417-021-05137-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05137-9