Abstract
Purpose
Our aim is to develop a new generation of suprachoroidal–transretinal stimulation (STS) retinal prosthesis using a dual-stimulating electrode array to enlarge the visual field. In the present study, we aimed to examine how position and size of the visual field—created by a retinal prosthesis simulator—influenced mobility.
Methods
Twelve healthy subjects wore retinal prosthesis simulators. Images captured by a web camera attached to a head-mounted display (HMD) were processed by a computer and displayed on the HMD. Three types of artificial visual fields—designed to imitate phosphenes—obtained by a single (5 × 5 electrodes; visual angle, 15°) or dual (5 × 5 electrodes ×2; visual angle, 30°) electrode array were created. Visual field (VF)1 is an inferior visual field, which corresponds to a dual-electrode array implanted in the superior hemisphere. VF2 is a superior visual field, which corresponds to a single-electrode array implanted in the inferior hemisphere. VF3 is a superior visual field, which corresponds to a dual-electrode array implanted in the inferior hemisphere. In each type of artificial visual field, a natural circular visual field (visual angle, 5°) which imitated the vision of patients with advanced retinitis pigmentosa existed at the center. Subjects were instructed to walk along a black carpet (6 m long × 2.2 m wide) without stepping on attached white circular obstacles. Each obstacle was 20 cm in diameter, and obstacles were installed at 40-cm intervals. We measured the number of footsteps on the obstacles, the time taken to complete the obstacle course, and the extent of head movement to scan the area (head-scanning). We then compared the results recorded from these 3 types of artificial visual field.
Results
The number of footsteps on obstacles was lowest in VF3 (One-way ANOVA; P = 0.028, Fisher’s LSD; VF 1 versus 3 P = 0.039, 2 versus 3 P = 0.012). No significant difference was observed for the time to complete the obstacle course or the extent of head movement between the 3 visual fields.
Conclusion
The superior and wide visual field (VF3) obtained by the retinal prosthesis simulator resulted in better mobility performance than the other visual fields.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
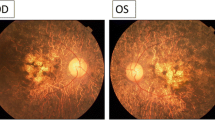
Hereditary retinal dystrophies, particularly retinitis pigmentosa, have no established therapy and are among the leading causes of blindness worldwide, especially in developed countries [1, 2]. In recent years, artificial vision technology has begun to attract attention as a mode of therapy. Artificial vision technology recovers vision by electrically stimulating neurons at specific locations along the visual pathway. Among these technologies, the most widely developed approaches involve retinal prostheses, which insert stimulating electrodes at the retina. There are three types of retinal prostheses, classified according to the position in which the electrodes are inserted: epiretinal prostheses [3, 4], subretinal prostheses [5,6,7], and suprachoroidal prostheses [8,9,10]. Our aim was to develop a suprachoroidal type of retinal prosthesis (STS, suprachoroidal–transretinal stimulation) [10].
The simplest method to further improve vision through retinal prostheses in the future is to increase the resolution by reducing the size and increasing the number of stimulating electrodes. Previously, Zrenner et al. stimulated the retina with 1500 stimulating electrodes, obtaining good results; however, the number of electrodes and visual acuity are not necessarily directly proportional [11]. Our group conducted a clinical trial of an STS retinal prosthesis, which contained 49 stimulating electrodes. In the present clinical trial, we observed that participants were unable to discriminate between two phosphenes induced simultaneously by adjacent stimulating electrodes because the phosphenes overlapped. This finding indicates that in STS retinal prostheses, to discriminate between two phosphenes, it is necessary to increase the distance between the stimulating electrodes with the current value at which phosphenes are obtained. Therefore, we aim to improve next-generation STS by enlarging the area of the electrode array to expand the visual field rather than by increasing the number of stimulating electrodes and increasing resolution.
One of the merits of expanding the visual field is that the visual information obtained at any one time increases. Furthermore, the position of the visual field induced by the retinal prosthesis can be selected depending on the insertion position of the electrode array. It is still to be determined which visual field position is most advantageous. Generally, it has been concluded that an inferior visual field has a more profound influence on quality of life (QOL) than a superior visual field [12,13,14]. However, it is not yet known whether these findings hold true for an artificial visual field induced by retinal prosthesis; therefore, further research is required.
In the present study, we investigated the effect of an expanded visual field and the effect of visual field position, on participant mobility—an important visual behavior—using a retinal prosthesis simulator.
Subjects and Methods
Subjects
Twelve healthy volunteers (4 males, 8 females) with an average age of 26.8 ± 5.5 years (± SD) were included in the study. All participants had best-corrected visual acuity (BCVA) ≥ 20/20. The procedures used in this study adhered to the principles of the Declaration of Helsinki and were approved by the Ethics Committee of Osaka University Hospital. A full explanation of the purpose of the study and the procedures to be used was presented to the participants, who all signed an informed consent form. It was made clear to all participants that they were free to withdraw from the study at any time.
Methods
Each participant, wearing full correction lenses and a retinal prosthesis simulator, underwent a mobility test. For the mobility test, white circular cloths with a diameter of 20 cm were placed on a black carpet measuring 6 m × 2.2 m. Obstacles were placed on the carpet at an interval of 40 cm (Fig. 1). Participants were instructed to pass the length of the carpet without stepping on obstacles. In addition, participants were equipped with a head-mounted iPod touch® (Apple, Cupertino, USA) with gyroscope function; visual scanning through head movement (hereafter referred to as head-scanning) during the mobility test was measured simultaneously. During the mobility test, the retinal prosthesis simulator presented images received through three different processing methods (described in the following sections). The time taken to pass through the obstacle course, the number of steps taken on obstacles, and the extent of head-scanning for each processing method were compared. The time taken to pass through the obstacle course was measured by a stopwatch and the number of steps taken on an obstacle was measured visually.
Retinal prosthesis simulator
The retinal prosthesis simulator receives images from a web camera (BSW20KM11BK, Buffalo, Nagoya, Japan) placed on a head-mounted display (HMD) (HMZ-T1®, SONY, Tokyo, Japan). The input images are processed with a custom-built program (Nidek, Gamagohri, Japan) on a laptop computer (PC-GL19614GU, NEC, Tokyo, Japan) then displayed on the HMD. The retinal prosthesis simulator displayed a retinal prosthesis visual field of 15° (visual angle) per side, imitating an electrode array consisting of 5 × 5 stimulating electrodes in three ways: ① dual-electrode array inferior visual field (visual field (VF)1), ② single-electrode array superior visual field (VF2), and ③ dual-electrode array superior visual field (VF3), in addition to a central circular natural visual field with a diameter of 5° (visual angle) (Fig. 2a). The central natural visual field imitates the vision of patients with advanced retinitis pigmentosa (Fig. 2b). The visual acuity of the central natural visual field was measured as having a value of approximately 1.0 logMAR (logarithm of the minimum angle of resolution) units. In the retinal prosthesis simulator, if the average luminance range of one electrode exceeds a certain value, it is displayed as one light spot (Fig. 2b). The laptop for processing images was contained in a rucksack, which was carried by the participant (Fig. 3).
Pattern diagrams of three types of visual fields displayed by the retinal prosthesis simulator. a The retinal prosthesis simulator displayed a central circular natural visual field with a diameter of 5° (visual angle) and the retinal prosthesis visual field 15° (visual angle) on one side in three different ways: VF1, dual-electrode array inferior visual field; VF2, single-electrode array superior visual field; VF3, dual-electrode array superior visual field. b A schematic view of what the participants see (VF3). When the participant sees an obstacle with the retinal prosthesis simulator, the artificial visual fields are displayed as light spots for the corresponding part, and the central natural visual field shows the actual image in low resolution
Actual picture of the retinal prosthesis simulator. The participant is wearing a head-mounted display with a web camera. A laptop computer for processing the images taken by the web camera is kept in the rucksack on the participant’s back. An iPod touch® is attached to the back of the participant’s head
Head-scanning
Subjects wore a 6th generation iPod touch® on their head, and the extent of head-scanning during the mobility test was measured through a built-in gyro sensor. Using the custom-built program, the horizontal, vertical, and rotational angular velocities of the head were measured every 0.02 s, and the absolute values of these values were integrated to obtain the total extent of head-scanning during the test. Among the three directions of head movement, horizontal and vertical directions were analyzed.
Statistical analyses
One-way analysis of variance (ANOVA) and Fisher’s least significant difference (Fisher’s LSD) test were used for comparisons between the three groups. A p value of 0.05 or less was considered significant. SigmaPlot version 13.0® (SystatSoftware Inc., San Jose, USA) analytical software was used for analysis.
Results (Table 1)
Number of steps taken on obstacles
The average number of steps taken on obstacles were 6.5 ± 4.1 (VF1), 7.2 ± 5.0 (VF2), and 3.8 ± 2.6 (VF3), respectively. One-way ANOVA revealed these results to be statistically significantly different (P = 0.028). Furthermore, statistically significant differences were observed between VF1 and VF3 (P = 0.039, Fisher’s LSD) and between VF2 and VF3 (P = 0.012, Fisher’s LSD).
Time taken to pass through the obstacle course
The average times taken to pass through the obstacle course were 47.6 ± 22.4 s (VF1), 50.7 ± 25.2 s (VF2), and 44.0 ± 26.1 s (VF3), respectively. This was included as reference data because there was no significant difference in one-way ANOVA (P = 0.12); however, time taken to pass through the obstacle course tended to be shorter for VF3 than for VF2 (P = 0.040, paired t test).
The extent of head-scanning
The average extent of head-scanning in the vertical direction was 274.9 ± 167.6°(VF1), 287.3 ± 167.6°(VF2), and 244.7 ± 174.5°(VF3), respectively. There was no significant difference in one-way ANOVA (P = 0.55). The average extent of head-scanning in the horizontal direction was 533.2 ± 253.6°(VF1), 568.5 ± 371.0°(VF2), and 423.2 ± 289.4°(VF3), respectively. This was included as reference data as there was no significant difference in one-way ANOVA (P = 0.072); however, the extent of head-scanning in the horizontal direction tended to be smaller for VF3 than for VF2 (P = 0.029, paired t test).
Discussion
In the present study, we simulated the use of retinal prosthesis for patients with advanced retinitis pigmentosa using healthy participants and evaluated walking ability. The rationale for selecting walking ability as an outcome is that this parameter is greatly influenced by the visual field, which is important for locating a wide range of targets and obstacles. Furthermore, in patients with visual field disturbances, it has been reported that mobility performance can be improved by training visual scanning using saccades, unlike other activities, such as reading [15, 16]. As described later, we considered that saccades are equivalent to head-scanning in retinal prosthesis patients, and that evaluating head-scanning would be an indicator of the quality of mobility of retinal prosthesis patients.
As indicators of walking ability, we evaluated three parameters: the number of steps taken on obstacles on the obstacle course, the time taken to pass through the obstacle course, and the extent of head-scanning. In general, patients with a retinal prosthesis featuring external cameras rely on head movements to find targets because the camera does not follow eye movements [17]. Currently, retinal prostheses have started to be developed that incorporate gaze tracking systems [18, 19]. Despite these developments, we hypothesize that visual scanning based on head movements will continue to be a necessary skill for the time being due to current limitations with the gaze tracking system, such as calibration accuracy and delay. Patients with a retinal prosthesis are often elderly people; therefore, lots of head movement may prove a heavy burden for patients. For this reason, we selected head-scanning as one of the parameters for evaluation because reducing head-scanning by enlarging the visual field may be helpful for patients.
In the present study, we evaluated mobility with three visual field patterns and found that the number of steps on obstacles was significantly smaller in VF3 than in VF1 or VF2. Although only included as reference data, in VF3, the time taken to pass through the obstacle course tended to be shorter, and the extent of head-scanning tended to be smaller than in VF2. Generally, an inferior visual field is thought to have a larger influence on QOL than a superior visual field [12,13,14]. However, in this experiment, better performance was observed with a superior visual field than with an inferior visual field. The reason for this may be that in ultra-low vision conditions, participants cannot avoid seeing their feet when walking. Seeing their feet, participants can then obtain visual information in the direction of travel from the superior visual field, improving performance with the superior visual field. It has previously been reported that superior visual field disorders have a larger impact on the ability to observe obstacles when driving as compared to inferior visual field disorders [20]. The most important visual field position in everyday life may change depending on tasks; therefore, it is necessary to consider this on an activity-by-activity basis.
Considering that the extent of head-scanning tended to be smaller, and the time taken to pass through the obstacle course tended to be shorter with a wide visual field, dual-electrode array, we conclude that participants can obtain a wide range of information about obstacles simultaneously when using this mode, resulting in a reduction of the extent of head movement and time taken to pass through the obstacle course. It has been reported previously that glaucoma patients with narrowed visual fields complete more saccades than healthy controls when performing tasks to which they are unaccustomed and that these patients require more time to perform the task [21]. If we consider saccades and head-scanning of retinal prosthesis patients to be similar, we would conclude that the width of the visual field affected the results in our study, in keeping with previous findings. As results regarding head-scanning and time required to complete obstacle course are only tendencies and did not reach statistical significance, it is necessary to increase the number of participants and test these again in the future.
Finally, the conditions of the mobility test in our study consisted of high-contrast obstacles allocated at equal intervals; in the future, it is necessary to evaluate walking ability under more natural circumstances.
In the present study, we examined the size and position of the visual field in the simulated retinal prosthesis and found that walking performance improved depending on the conditions, particularly when using the VF3 setup. We should also consider other activities to fully evaluate the effects of size and position of visual field on walking ability, particularly in realistic conditions.
References
Iwase A, Araie M, Tomidokoro A, Yamamoto T, Shimizu H, Kitazawa Y, Tajimi Study G (2006) Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 113:1354–1362. https://doi.org/10.1016/j.ophtha.2006.04.022
Kocur I, Resnikoff S (2002) Visual impairment and blindness in Europe and their prevention. Br J Ophthalmol 86:716–722
Humayun MS, Weiland JD, Fujii GY, Greenberg R, Williamson R, Little J, Mech B, Cimmarusti V, Van Boemel G, Dagnelie G, de Juan E (2003) Visual perception in a blind subject with a chronic microelectronic retinal prosthesis. Vis Res 43:2573–2581
Rizzo JF 3rd, Wyatt J, Loewenstein J, Kelly S, Shire D (2003) Perceptual efficacy of electrical stimulation of human retina with a microelectrode array during short-term surgical trials. Invest Ophthalmol Vis Sci 44:5362–5369
Zrenner E (2002) Will retinal implants restore vision? Science 295:1022–1025. https://doi.org/10.1126/science.1067996
Chow AY, Chow VY, Packo KH, Pollack JS, Peyman GA, Schuchard R (2004) The artificial silicon retina microchip for the treatment of vision loss from retinitis pigmentosa. Arch Ophthalmol 122:460–469. https://doi.org/10.1001/archopht.122.4.460
Lorach H, Goetz G, Mandel Y, Lei X, Galambos L, Kamins TI, Mathieson K, Huie P, Dalal R, Harris JS, Palanker D (2015) Performance of photovoltaic arrays in-vivo and characteristics of prosthetic vision in animals with retinal degeneration. Vis Res 111:142–148. https://doi.org/10.1016/j.visres.2014.09.007
Wong YT, Chen SC, Seo JM, Morley JW, Lovell NH, Suaning GJ (2009) Focal activation of the feline retina via a suprachoroidal electrode array. Vis Res 49:825–833. https://doi.org/10.1016/j.visres.2009.02.018
Shivdasani MN, Luu CD, Cicione R, Fallon JB, Allen PJ, Leuenberger J, Suaning GJ, Lovell NH, Shepherd RK, Williams CE (2010) Evaluation of stimulus parameters and electrode geometry for an effective suprachoroidal retinal prosthesis. J Neural Eng 7:036008. https://doi.org/10.1088/1741-2560/7/3/036008
Fujikado T, Kamei M, Sakaguchi H, Kanda H, Endo T, Hirota M, Morimoto T, Nishida K, Kishima H, Terasawa Y, Oosawa K, Ozawa M, Nishida K (2016) One-year outcome of 49-channel suprachoroidal-transretinal stimulation prosthesis in patients with advanced retinitis pigmentosa. Invest Ophthalmol Vis Sci 57:6147–6157. https://doi.org/10.1167/iovs.16-20367
Stingl K, Schippert R, Bartz-Schmidt KU, Besch D, Cottriall CL, Edwards TL, Gekeler F, Greppmaier U, Kiel K, Koitschev A, Kühlewein L, MacLaren RE, Ramsden JD, Roider J, Rothermel A, Sachs H, Schröder GS, Tode J, Troelenberg N, Zrenner E (2017) Interim results of a multicenter trial with the new electronic subretinal implant alpha AMS in 15 patients blind from inherited retinal degenerations. Front Neurosci 11:445–445. https://doi.org/10.3389/fnins.2017.00445
Marigold DS, Patla AE (2008) Visual information from the lower visual field is important for walking across multi-surface terrain. Exp Brain Res 188:23–31. https://doi.org/10.1007/s00221-008-1335-7
Black AA, Wood JM, Lovie-Kitchin JE (2011) Inferior visual field reductions are associated with poorer functional status among older adults with glaucoma. Ophthalmic Physiol Opt 31:283–291. https://doi.org/10.1111/j.1475-1313.2010.00811.x
Abe RY, Diniz-Filho A, Costa VP, Gracitelli CP, Baig S, Medeiros FA (2016) The impact of location of progressive visual field loss on longitudinal changes in quality of life of patients with glaucoma. Ophthalmology 123:552–557. https://doi.org/10.1016/j.ophtha.2015.10.046
de Haan GA, Melis-Dankers BJ, Brouwer WH, Tucha O, Heutink J (2015) The effects of compensatory scanning training on mobility in patients with homonymous visual field defects: a randomized controlled trial. PLoS One 10:e0134459. https://doi.org/10.1371/journal.pone.0134459
de Haan GA, Melis-Dankers BJ, Brouwer WH, Tucha O, Heutink J (2016) The effects of compensatory scanning training on mobility in patients with homonymous visual field defects: further support, predictive variables and follow-up. PLoS One 11:e0166310. https://doi.org/10.1371/journal.pone.0166310
Sabbah N, Authie CN, Sanda N, Mohand-Said S, Sahel JA, Safran AB (2014) Importance of eye position on spatial localization in blind subjects wearing an Argus II retinal prosthesis. Invest Ophthalmol Vis Sci 55:8259–8266. https://doi.org/10.1167/iovs.14-15392
Caspi A, Roy A, Wuyyuru V, Rosendall PE, Harper JW, Katyal KD, Barry MP, Dagnelie G, Greenberg RJ (2018) Eye movement control in the Argus II retinal-prosthesis enables reduced head movement and better localization precision. Invest Ophthalmol Vis Sci 59:792–802. https://doi.org/10.1167/iovs.17-22377
Titchener SA, Shivdasani MN, Fallon JB, Petoe MA (2018) Gaze compensation as a technique for improving hand-eye coordination in prosthetic vision. Transl Vis Sci Technol 7:2. https://doi.org/10.1167/tvst.7.1.2
Glen FC, Smith ND, Crabb DP (2015) Impact of superior and inferior visual field loss on hazard detection in a computer-based driving test. Br J Ophthalmol 99:613–617. https://doi.org/10.1136/bjophthalmol-2014-305932
Dive S, Rouland JF, Lenoble Q, Szaffarczyk S, McKendrick AM, Boucart M (2016) Impact of peripheral field loss on the execution of natural actions: a study with glaucomatous patients and normally sighted people. J Glaucoma 25:e889–e896. https://doi.org/10.1097/IJG.0000000000000402
Funding
This study was supported by KAKENHI (Grants-in-Aid for Scientific Research B 16H05487).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of Osaka University Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Endo, T., Hozumi, K., Hirota, M. et al. The influence of visual field position induced by a retinal prosthesis simulator on mobility. Graefes Arch Clin Exp Ophthalmol 257, 1765–1770 (2019). https://doi.org/10.1007/s00417-019-04375-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04375-2