Abstract
Purpose
Angiogenesis plays a key role in glioblastoma, but most anti-angiogenic therapy trials have failed to change the poor outcome of this disease. Despite this, and because bevacizumab is known to alleviate symptoms, it is used in daily practice. We aimed to assess the real-life benefit in terms of overall survival, time to treatment failure, objective response, and clinical benefit in patients with recurrent glioblastoma treated with bevacizumab.
Methods
This was a monocentric, retrospective study including patients treated between 2006 and 2016 in our institution.
Results
202 patients were included. The median duration of bevacizumab treatment was 6 months. Median time to treatment failure was 6.8 months (95%CI 5.3–8.2) and median overall survival was 23.7 months (95%CI 20.6–26.8). Fifty percent of patients had a radiological response at first MRI evaluation, and 56% experienced symptom amelioration. Grade 1/2 hypertension (n = 34, 17%) and grade one proteinuria (n = 20, 10%) were the most common side effects.
Conclusions
This study reports a clinical benefit and an acceptable toxicity profile in patients with recurrent glioblastoma treated with bevacizumab. As the panel of therapies is still very limited for these tumors, this work supports the use of bevacizumab as a therapeutic option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common and aggressive primary brain tumor in adults. The standard of care, unchanged since 2005, recommends maximal safe surgery followed by chemo radiotherapy and adjuvant temozolomide. Glioblastoma continues to be an incurable disease, with median survival of 15–18 months. Only 9% of patients will survive for ≥ 5 years from diagnosis [1, 2]. Besides the poor prognosis, this disease has a devastating impact on patient quality of life, causing neurological and psychological disorders [3].
It is a complex and heterogeneous disease with a highly invasive and infiltrative potential. These characteristics explain the challenge of achieving complete resection and also lead to tumor resistance to therapy [4, 5]. Almost all patients will relapse after first-line treatment and despite several clinical trials, there is no standard in second-line treatment for patients with recurrent disease [1, 6]. Although more is known about the molecular mechanisms of glioma, no major survival benefit has yet been reported. The most common alterations described are chromosome 1p/19q codeletion, isocitrate dehydrogenase (IDH) mutation, amplification of epidermal growth factor receptor (EGFR), methyl-guanine methyl transferase gene promoter (MGMT), platelet-derived growth factor receptor alpha (PDGFRα), telomerase reverse transcriptase (TERT), phosphatase and tensin homologue (PTEN), and cyclin dependent kinase inhibitor 2A(CDKN2A) [7,8,9,10,11].
Glioblastoma is the most vascularized glial tumor, and angiogenesis plays a key role in its development and proliferation [12]. Neo-vessels form from preexisting blood vessels due to vascular endothelial growth factor (VEGF) expression by tumor and stromal cells in the presence of hypoxia [13]. Alternative mechanisms like vasculogenesis (formation of new vessels de novo) may also occur, explaining the complexity of treating glioblastoma [3, 14].
In 2004, bevacizumab, an anti-VEGF humanized immunoglobulin G1 monoclonal antibody, became the first anti-angiogenic to be tested in these patients. Since then, some clinical trials have questioned the benefit of bevacizumab alone or in association with chemotherapy [15, 16]. Results have been disappointing; despite an increase in progression-free survival (PFS), no impact in overall survival (OS) has been seen [17]. Small-molecule tyrosine kinase inhibitors, such as sorafenib, cediranib, and regorafenib, have shown some efficacy in phase 2 and 3 trials, but results remain modest or not definitively demonstrated [18,19,20,21].
In view of the clinical trial data, bevacizumab use in recurrent glioblastoma was fully approved by the Food and Drug Administration(FDA) in the USA and denied by the European Medicine Agency, making its use difficult in this setting [22, 23]. Data suggest that its clinical benefit comes mainly from reducing edema and corticosteroid use but also by reducing hospital stays and decreasing the cost of care; it therefore has a symptomatic effect, leading to improved quality of life [24].
Among neuro-oncologists, bevacizumab is widely used due to observed clinical benefit and lack of standard treatment options [25]. Based on some signs of efficacy from phase 2 and 3 trials, bevacizumab is used either in monotherapy or in combination with lomustine, temozolomide, or carboplatin [16, 17, 26,27,28]. Combination with salvage re-irradiation is an option whenever feasible/available, and this combination has shown efficacy in many retrospective studies. The RTOG 1205/NCT01730950 phase 2 study, tested bevacizumab with re-irradiation prospectively in recurrent glioblastoma. While full results are pending, bevacizumab with re-irradiation improved PFS versus bevacizumab alone (6-month PFS 54% versus 29%; HR = 0.42 [95%CI 0.3–0.5; p = 0.001]) [29,30,31].
Real-life patients are not always as fit as those included in clinical trials are: they can harbor more comorbidities and sometimes more aggressive disease with rapid clinical deterioration. However, real-world data can provide valuable observations on treatment patterns, safety, and benefits in a wider range of patient characteristics. To date, there has only been few real-world cohort in patients with recurrent glioblastoma treated with bevacizumab, the results of which support its use in these patients [29].
This work sought to assess the real-life clinical benefit to patients treated with bevacizumab in this setting. We conducted a retrospective analysis in our institution based on all patients with recurrent glioblastoma who had received bevacizumab.
Materials and methods
Patient selection
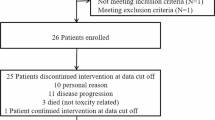
We retrospectively collected clinical data for 202 patients from our institution, the Gustave Roussy comprehensive cancer center, treated from 2006 to 2016. Data from all adult patients with histologically proven glioblastoma who received bevacizumab at any point during their disease were analyzed. Histology other than glioblastoma or brain metastases was not included.
Treatment and patient analysis
The following patient characteristics were evaluated: performance status (PS) ECOG (Eastern Cooperative Oncology Group Performance Status), sex, age, neurological deficit, increased intracranial pressure (ICP) symptoms, and occurrence of seizure. Data on type of surgery (resection or biopsy) and modality of radiation therapy and its combination or not with temozolomide or either radiation therapy or chemotherapy alone were reviewed and collected. Surgery was considered R0 if there were no signs of residual disease on the postoperative MRI done within 72 h of intervention. Data regarding the chemotherapy used in combination with bevacizumab in first-line and any subsequent line treatment were collected. The median time to first relapse (median TFR) was defined as the interval between the end of the complete Stupp regimen and bevacizumab initiation.
The response to treatment was evaluated by MRI every 2–3 months. The clinical response was also recorded and was defined as symptom amelioration (ICP, seizures, and neurological deficit) and improvement of PS.
Progression was discussed in a multidisciplinary tumor board (MDTB). Macdonald or RANO (Response assessment in neuro-oncology) criteria (once these validated as a new standard), were used to assess the response on MRI. Progressive disease (PD) was defined as a further increase of initial enhancement on the next two follow-up MRIs or a fatal outcome within 6 months of diagnosis. Pseudo-progression was defined when a decrease or no further enhancement was seen on the next two follow-up MRIs.
Other criteria, such as the delay to radiological response after bevacizumab initiation, clinical response, and type of maximal response, were collected. The maximal response was defined as the best radiological response during treatment with bevacizumab: complete response (CR), stable disease (SD), or partial response (PR). Other tumor characteristics, such as anatomical location date of surgery, extent of resection, and treatment toxicities, were also collected from electronic patient files.
Data collection
We searched the Gustave Roussy database using the keywords “glioblastoma” and “bevacizumab” to collect potentially eligible files.
Statistical analysis
As bevacizumab can be given as maintenance therapy, it can also be used on a stop and start basis. Therefore, we chose to measure time to treatment failure (TTF), defined as the time between bevacizumab initiation and confirmed treatment failure (radiological MRI confirmation), discontinuation, or death, rather than PFS. OS was described as the time from initial diagnosis to death or the last follow-up for surviving patients. Relapse OS was calculated from relapse to death or the last follow-up for surviving patients.
Descriptive statistics were calculated for all quantitative variables (age, tumor location, neutrophil count).
Survival analysis was calculated using the Kaplan–Meier method and the log-rank test to compare associations between variables and TTF or OS using SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA). A p value of p < 0.05 was considered statistically significant. A univariate and multivariate linear regression were performed using Wilcoxon–Mann–Whitney test, Belsley–Kuh–Welsch technique, Breusch–Pagan test and Shapiro–Wilk test. A p value < 0.05 was considered statistically significant. Patients with missing data were excluded from analysis. Statistical analysis was performed with the online application EasyMedStat (version 3.21.5 www.easymedstat.com).
Results
A total of 202 patients with glioblastoma were included in this study: 121 (60%) were male and 81 (40%) female. Median age at diagnosis was 58 years (range 18–80). Glioblastomas were similarly distributed between both hemispheres: 95 (47%) were located in the right side and 90 (45%) in the left side. The most common locations were frontal (n = 56, 30%) and temporal lobes (n = 62, 34%). Seventeen patients (8%) had bilateral glioblastoma.
Standard treatment
A total of 145 (72%) patients were treated by surgery, and the surgery was R0 in only 67 patients (n = 46%). The remaining 57 (28%) patients had tumor biopsies only (no patients were treated without histology). Most patients received concomitant standard Stupp chemoradiotherapy (n = 195, 97%) followed by adjuvant temozolomide (n = 180, 89%) with a median of six cycles. At the end of the Stupp regimen, 36 (18%) patients were considered to have PD by the MDTB and 6 (3%) had a clear pseudo progression, assessed by radiological review.
Table 1 summarizes baseline characteristics and details of patients’ standard treatment at diagnosis.
Relapse pattern
For the patients that progressed during adjuvant temozolomide treatment or less than 6 months after the end of the Stupp regimen, the median TFR was 0.9 months, while for those progressing after 6 months, the median TFR was 12.9 months. The median TFR from initial diagnosis was 9.4 months and 11 months, respectively. Twenty-two patients were able to have a second surgery (11%), and 17 (9%) received re-irradiation.
The median duration of bevacizumab treatment was 6 months. Half of the patients (n = 101, 50%) had a radiological response: best radiological responses were PR (47%) and CR (3%), mainly at the first MRI, within a median of 1.6 months. Most patients had a good ECOG PS at bevacizumab initiation (Table 2).
Treatment modality
Patients received bevacizumab alone or in association with radiation therapy, lomustine, irinotecan, or temozolomide. The dose of bevacizumab ranged between 10 mg/kg every 2 weeks and 15 mg/kg every 3 weeks intravenously. For the chemotherapy, standard doses were used; lomustine, 90 mg/m2; irinotecan, 180 mg/m2, and temozolomide, 150–200 mg/m2. The duration of first bevacizumab administration was 1.5 h, then 1 h for the second, and 30 min starting for the third administration. This protocol has since been simplified to a 30 min infusion due to sufficient data supporting the scarcity of allergic reactions.
Clinical benefit
At first follow-up (6–8 weeks), 75 patients (37%) experienced an improvement in PS, while 3 patients (1%) experienced a worsening in PS, due to progression (Table 2). The majority (n = 158, 78%) had symptoms, such as ICP, seizure, and neurological deficit, before treatment initiation and more than half (n = 114, 56%) experienced symptom improvement. Clinical improvement was assessed by neuro-oncologists based on clinical examination, PS, and patient self-reported information.
Bevacizumab
Most patients (87%, n = 175) received bevacizumab alone or in association with standard chemotherapy at first relapse. Twenty-one (10%) patients received bevacizumab with re-irradiation, because of significant edema and to avoid radio-necrosis. Twelve patients who experienced PD after finishing bevacizumab were re-challenged at progression. Among them, 5 (42%) showed a PR, 2 (16%) had SD, and 5 (42%) experienced PD.
None of the 202 patients experienced an anaphylactic reaction. Grade 1/2 hypertension (n = 34, 17%) and grade 1 (n = 20, 10%) proteinuria were the most common toxicities experienced by patients. Thromboembolic events due to bevacizumab treatment also occurred, as follows: 8 patients developed deep vein thrombosis without treatment discontinuation, and 4 others discontinued treatment after experiencing stroke (3 patients) or pulmonary embolism (1 patient).Twelve patients (6%) had gastrointestinal (GI), cerebral, head and neck, or urinary system hemorrhagic events related to bevacizumab treatment. Six patients (3%) experienced lethal toxicity: 4 (2%) had GI perforation, 1 (0.5%) had cerebral hemorrhage, and 1 (0.5%) had arterial bleeding. Intratumoral hemorrhage was found in 15 patients (7%) and only in 4 (2%), the treatment was discontinued.
Subsequent lines
A proportion of patients received second (n = 110, 54%) and third-line (n = 44, 22%) treatment. In second-line treatment, the majority received lomustine (n = 68/110, 62%), while the carboplatin was the most common in third-line treatment (n = 12/44, 27%). Another proportion of patients (n = 70/202, 35%) continued with bevacizumab in the second line after modification/change of the chemotherapy backbone (e.g., temozolomide switched to lomustine).
Survival
The median TTF was 6.8 months (95%CI 5.3–8.2) and the median OS 23.7 months (95%CI 20.6–26.8) (Fig. 1A and B). Patients treated with radiotherapy and bevacizumab had a median TTF of 7 months and median OS of 25.5 months. The median relapse OS was 13.5 months (95%CI 11.6–15.3). Two patients (1%) were still alive without active treatment and with controlled disease at the end of the study. Ninety-three patients (46%) exceeded 24 months of OS, with median OS reaching 35.6 months (range 24–117). The median OS was higher in younger versus older patients but the distribution of the groups did not allow for statistical analysis.
Symptoms and survival
Symptom worsening was associated with shorter TTF compared with symptom amelioration or stability as follows: median TTF 4.1 months (95%CI 3.7–4.5) versus 7.1 months (95%CI 5.4–8.7) and 10.23 months (95%CI 7.0–13.4), p = 0.001 by log-rank test. The difference between the symptom amelioration group and stability group was not statistically significant.
Radiological response and survival
Rapid response to bevacizumab was associated with longer TTF and was statistically significant, p = 0.02 by log-rank test. An evaluation of the best MRI response and OS or TTF revealed that patients with PD had the shortest OS and TTF compared with other groups: 15.8 months (95%CI 12.8–18.7) and 1.7 months (95%CI 1.5–1.9), respectively, p = 0.001 by log-rank test; PR group 26.16 months (95%CI 22.5–29,7) and 8.23 months (95%CI 6.9–9.5), respectively; CR group 46.83 months (95%CI 24.7–68.9) and 11.47 months (95%CI 9.5–13.3), respectively; and SD group 21.43 months (95%CI 17.2–25.5) and 6.1 months (95%CI 4.1–8.0) (Fig. 2).
A Time to treatment failure (months) according to best radiological response. This figure shows Time to treatment failure (assessed in months) in patients treated with bevacizumab according to their best MRI response. The best MRI response is defined as the best radiological response achieved during treatment with bevacizumab. CR complete response, PD progressive disease, PR partial response, SD stable disease. B Overall survival (months) according to best radiological response. This figure shows the association between overall survival, assessed in months, in patients treated with bevacizumab according to their best MRI response. The best MRI response is defined as the best radiological response, achieved during treatment with bevacizumab. CR complete response, PD progressive disease, PR partial response, SD stable disease
Prognostic factors
Arterial hypertension
Thirty-four patients (17%) developed hypertension during bevacizumab treatment, of whom 23 responded to treatment (partial response).
The median TTF was longer in patients with hypertension, compared to those without as follow: 14.67 months (95%CI 9.51–19.58) versus 7.43 months (95%CI 6.39–8.48) and was statistically significant, p < 0.001.
Neutrophil count
Based on previous data on neutrophil count as a predictive factor for bevacizumab efficacy, we chose to set the neutrophil count cut-off at 6000/mm3. The patient group with a neutrophil count < 6000/mm3, had a longer median TTF than those with neutrophil count > 6000/mm3 (median TTF 7.6 months [95%CI 6.4–8.8]), versus 4.3 months [95%CI 3.0–5.5]). The association between neutrophil count and TFF was statistically non-significant for both groups, with log-rank p values of 0.132 and 0.139, respectively.
Location
Bilateral location was associated with the worst TTF compared with right and left tumors, and this was statistically significant (3 months versus 6.8/7.1 months, p = 0.041 by log-rank test). The association with OS was not statistically significant (13.3 months versus 25.7/21.4 months, respectively, p = 0.243 by log-rank test).
Sex and age
Univariate analysis revealed that female patients had longer median TTF (8.8 versus 5.1 months, HR = 0.66, 95%CI 0.4–0.8, p = 0.005) and better median OS (28.1 versus 19.1 months, HR = 0.61 95%CI 0.4–0.8, p = 0.001) than male patients. Younger age (< 58 years) was also associated with a better TTF: median TTF 7.5 versus 5.8 months in older patients, HR = 0.68 95%CI 0.51–0.91, p = 0.01.The OS was numerically better in younger and older patients, without statistical significance as follow: median OS 25.2 versus 21.3 months, HR = 0.74, 95%CI 0.55–0.99, p = 0.46.
Multivariate analysis
A multivariate analysis was performed to assess the relationship between OS and the explanatory variables as neutrophil count, age, tumor location, and sex (Fig. 3A). Bilateral glioblastoma was associated with lower survival (p-0.01), while female gender with highest survival (p = 0.0469). Age and neutrophil count were independently associated with OS.
The multivariate linear regression between TTF and the same explanatory variables revealed no impact on time to treatment failure (Fig. 3B).
Discussion
Despite the lack of survival benefit of bevacizumab for patients with recurrent glioblastoma, bevacizumab given as monotherapy or in association with chemotherapy are accepted options in clinical practice [26, 29]. We chose to study patients treated with bevacizumab throughout the recurrent disease journey, with most patients receiving bevacizumab at first relapse (88%). The most frequently prescribed biweekly regimens were bevacizumab/lomustine, bevacizumab/irinotecan, and bevacizumab monotherapy. Around a third of patients (35%) continued with anti-angiogenic treatment with a switch in chemotherapy backbone until definitive failure, mainly due to the clinician’s choice and a lack of options.
As median survival of patients with glioblastoma is often under 2 years [29], the quality of life is an important aspect for these patients. Because overall survival and time to treatment failure values do not always translate to clinical practice, we also focused on real-life aspects, such as amelioration of symptoms and neurological deficit, tolerance, rapidity and duration of response. In our study, more than 50% (n = 114, 56%) of patients experienced an improvement in their symptoms by the first evaluation after bevacizumab initiation (first MRI, 6–8 weeks after bevacizumab initiation) and this was associated with a longer time to treatment failure. Among the neuro-oncologist community, bevacizumab is widely prescribed, particularly for its capacity to improve symptoms [31]. However, bevacizumab is also considered “an expensive super steroid”, and there is a lot of criticism regarding its use in patients with glioblastoma. Most studies suggest that the benefit of bevacizumab is due to its capacity to reduce cerebral edema and corticosteroids use, and this should not be considered a pejorative fact, as the gain in quality of life is very important for these patients [32]. Several studies have included neurocognitive evaluation (using mini-mental state examination) in quality of life assessment and have revealed that it can predict radiological and clinical progression, highlighting the need for careful monitoring even starting at diagnosis [33, 34]. The most robust and controversial data on quality of life are those from the two prospective trials, AVAglio [35] and RTOG-0825 [36], in which patients with newly diagnosed glioblastoma were treated with bevacizumab. In the AVAglio trial, the deterioration free survival (quality of life questionnaires), was significantly longer in the bevacizumab arm than in the placebo arm, while in the RTOG-0825 trial, the deterioration of cognitive, motor and communication skills over time was greater in the bevacizumab group than in the placebo group. Quality of life was also assessed in the recurrent setting, and reported contrasting data, making it difficult to conclude whether bevacizumab was having a positive or negative impact; more research is needed in this field [30, 37]. In our study, none of the patients experienced symptom aggravation due to bevacizumab treatment. As it was a retrospective study, no quality of life or mini-mental questionnaires were performed, so it remains difficult to draw conclusions. Although the AVAglio [35] and RTOG-0825 [36] trials administered bevacizumab on a biweekly schedule, based on data from treatment of colon cancer [38], we chose a triweekly administration to offer patients a better quality of life and fewer hospital visits.
In our study, our observed median TTF with bevacizumab of 6.8 months was in the range of almost all previous results with bevacizumab. The median PFS with bevacizumab monotherapy or a bevacizumab/chemotherapy combination in the BRAIN [27], EORTC 10161 [26], and GLARIUS [39] trials ranged between 4 and 9.7 months. Regarding survival, in our study, the median OS from initial diagnosis was 23.7 months, which is higher than the median OS reported in prospective trials (12–15 months). This could be explained by the fact our institution is a reference center in which patients may benefit from larger multimodal treatment options including clinical trials, a younger age at diagnosis, surgical expertise with more R0 margins, and/or re-irradiation. No phase 3 trials have shown that bevacizumab therapy results in a clinical benefit for patients with newly or recurrent glioblastoma, and thus bevacizumab was approved only by FDA authorities [22].
MRI is an essential tool in assessing tumor response in patients with glioblastoma. We assessed the association between radiological response and survival in our study and showed that the median duration to best radiological response was 1.6 months, corresponding to the first MRI evaluation in most cases. Patients with progressive disease at the first MRI evaluation had worse survival than other groups (complete response, partial response, stable disease, p < 0.001), suggesting that anti-angiogenic treatment should be stopped in the absence of efficacy during the first 2 months. Evidence of progression on early MRI (4 and 8 weeks) with bevacizumab-based therapy was shown to be a prognostic marker of poor survival in a prospective trial [40]. The evaluation of radiological response to anti-angiogenic therapy in glioblastoma is quite challenging. Pseudo-response, translated as a decrease in contrast enhancement according to Macdonald criteria, without a true antitumor effect but with clinical improvement, is believed to explain the difference between favorable evolution of MRI and poor survival in clinical studies [41]. Although the hypothesis behind the pseudo-response to anti-angiogenic therapies is not well understood, it is believed that after “normalization” of the abnormal tumor blood vessels, tumor cells self-adjust to the therapy by developing alternative pathways that enhance angiogenesis, activate tumor proliferation and invasion, and lead to more resistant tumors [42]. The RANO criteria, which include T2 and /T2 weighted-Fluid Attenuated Inversion Recovery (FLAIR) sequences, have been developed to take into account this pseudo-response and better assess progression in patients receiving anti-angiogenic therapy. These criteria are superior to the Macdonald criteria for evaluating pseudo-response but remain insufficient [43]. For better evaluation of the efficacy of anti-angiogenic treatments, new biomarkers are required and should be included as endpoints in clinical trials for patients with glioblastoma. Some data show a good correlation between fluoro-thymidine uptake on positron emission tomography/computerized tomography scanning and bevacizumab efficacy, but there is still a need for more prospective data [21].
Hypertension was the most common side effect associated with bevacizumab treatment. Some retrospective studies in metastatic colorectal cancer have suggested that patients who developed hypertension during bevacizumab treatment had better survival [44]. In glioblastoma, the relationship between bevacizumab-induced hypertension and PFS or OS is not very clear, but there is some evidence from retrospective studies suggesting that hypertension could be a biomarker of efficacy and better outcomes [45,46,47]. In our group patients that have developed hypertension had longer TTF, however, the number of patients was small (34 patients). In the two prospective trials AVAglio [35] and BELOB [36], all-grade hypertension was a common side effect (experienced by 39.9% and 56% of patients, respectively), but the study did not investigate whether there was a correlation between tumor response and survival data. The lack of prospective data does not allow a conclusion to be drawn.
Clinical data suggest that in glioblastoma, a high neutrophil count, considered to be a marker of inflammation, is associated with more aggressive disease and a poor outcome [48]. A baseline neutrophil-to-lymphocyte ratio of > 4 has been shown to be an independent prognostic factor for poor survival in newly diagnosed and treated patients with glioblastoma [49]. In preclinical studies, peritumoral neutrophil infiltration promotes tumor proliferation and correlates with tumor grade [50]. Some data support the potential proangiogenic role of neutrophils in both physiological and pathological conditions [51]. In un-resectable and recurrent glioblastoma treated with bevacizumab, Bertaut et al. [52] found an interaction between baseline neutrophil count and survival. The cut-off was set at 6000 neutrophils/mm3, and bevacizumab significantly improved survival in patients with a neutrophil count > 6000/mm3: 17.3 months (95%CI 14.6–20.4) versus 8.4 months (95%CI 6.4–10.3), p < 0.0001. The authors pointed out that the detrimental effect of neutrophil count was counterbalanced by the effect of bevacizumab treatment and suggested the use of neutrophil count as a predictive marker for efficacy in the recurrent setting. The results in our study were different: the group of patients with a higher neutrophil count (> 6000/mm3) had lower survival and TTF compared with the lower neutrophil count group (< 6000/mm3), but the difference was not statistically significant, making it difficult to draw conclusions in this setting. Female sex and younger age were factors associated with better survival while bilateral glioblastoma harbored the worst prognosis, which is consistent with observations from large retrospective studies [53,54,55].
Besides bevacizumab, other small tyrosine kinase inhibitors have been tested in recurrent glioblastoma. Cediranib, an oral pan-VEGF receptor, showed promising results in a phase 2 trial, but the phase 3 trial did not meet its primary endpoint. Sunitinib, sorafenib, and vandetanib have demonstrated some activity in early phase trials, but results were modest in subsequent phases [19, 21]. Recently, the REGOMA [45] randomized phase 2 trial comparing regorafenib with lomustine reported a significant improvement in survival with regorafenib. The median survival with regorafenib was 7.4 months (HR 0.50, 95%CI 0.33–0.75, log-rank p = 0.0009) versus 5.6 months in the lomustine group, with a 12-month survival of 38.9% versus 15%, respectively. These results are promising, but there is still uncertainty regarding its development in phase 3 trial.
Limitations
As a monocentric retrospective work, our study has intrinsic limitations. Patients and their data were assessed from electronic files, and although the data were checked several times, omissions may have occurred. Incomplete data were also present. We did not assess patients’ MGMT or IDH mutation status or steroid use. We analyzed all patients receiving bevacizumab treatment and there was no control group. The choice of TTF as a criterion of efficacy and continuing bevacizumab treatment despite progression was done because of clinical benefit and a lack of standard options.
Conclusion
The therapeutic panel for glioblastoma has remained unchanged over the last decade. Many trials have failed their primary endpoint without clinical practice changing, and there are still limited treatment options for these patients. Despite the lack of strong evidence for a survival benefit from phase 3 trials, anti-angiogenic therapy plays a key role in the tumorigenesis of glioblastoma. Our study, based on real-life patients, has revealed an improvement in time to treatment failure and survival with an acceptable toxicity profile, and supports the use of bevacizumab in symptomatic patients with recurrent glioblastoma. Besides survival, bevacizumab is associated with symptom amelioration and a clinical benefit, which play a key role in the life of these patients. The triweekly administration might be more practical for patients with glioblastoma, as many patients experience cognitive impairment and are dependent on relatives/careers. There is an urgent need for new biomarkers and trials of new treatment combinations in the glioblastoma field.
Contribution to the field statement—personal opinion
In the face of so many negative trials, a lack of standard options, and an aggressive disease, what needs to change in the field, and what can we do better?
Glioblastoma is a very heterogeneous disease, and we probably have to start to approach it not as a single entity but as distinct subtypes; for example, more aggressive first-line treatment of IDH-wildtype glioblastoma than IDH mutated glioblastoma.
The development of genomic profiling and tumor sequencing should help us gain a better understanding of the disease and treatment individualization for some subgroups of patients, for example those with neurotrophic tyrosine receptor kinase (NTRK) fusions. Permeability for systemic drugs is not always optimal in the brain; intratumoral or intrathecal treatment administration is more attractive but at the same time more invasive. The recent development of nanomedicine could diminish the invasiveness and allow administration of multiple treatments with lower risks [56, 57].
Multiple factors, such as an immunosuppressive environment, drug penetrance, and many others, make the use of immunotherapy in glioblastoma challenging. In the face of the development of so many therapies (vaccines, chimeric antigen receptor (CAR) T cell therapy, oncolytic viruses, radiotherapy, etc.), we must find the best treatment sequence and predictive biomarkers [58, 59].
The need for steroid use in patients with glioblastoma could also be problematic because of their immunosuppressive effect that thus might lead to interference with immunotherapy treatment tested within clinical trials. Because of its anti-edematous effect, bevacizumab could replace steroids at least for patients enrolled in clinical trials testing immunotherapy. Angiogenesis is a key element in glioblastoma, and the use of anti-angiogenic treatment has a strong rationale. In my opinion, bevacizumab should be tested in association with other new drugs, even though it is not easy to justify the use of a treatment that has not proved its efficacy in phase 3 trials. Moreover, the use of bevacizumab in a multimodal treatment approach with radiotherapy should be reviewed to find better treatment sequences and combinations.
We probably also need to change the way we design trials, the criteria for evaluating treatment efficacy, and the way that drugs are approved by health authorities. Bevacizumab should remain an accessible option for patients with glioblastoma until the arrival of new therapeutic options.
Data availability
Data available on request. The data presented in this study are available on request from the corresponding author.
References
Stupp R, Masson WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Koshy M, Villano JL, Dolecek TA et al (2012) Improved survival time trends for glioblastoma using the SEER 17 population-based registries. J Neurooncol 107:207–212
Di Carlo DT, Cagnazzo F, Benedetto N, Morganti R, Perrini P (2017) Multiple high-grade gliomas: epidemiology, management, and outcome. A systematic review and meta-analysis. Neurosurg Rev. https://doi.org/10.1007/s10143-017-0928-7
Bahadur S, Sahu AK, Baghel P et al (2019) Current promising treatment strategy for glioblastoma multiform: a review. Oncol Rev 13(2):417
Chen S, Le T, Harley BAC, Imoukhuede PI (2018) Characterizing glioblastoma heterogeneity via single-cell receptor quantification. Front Bioeng Biotechnol 6:92
Hanif F, Muzzafar K, Perveen K, Malhi SM, Simjee ShU (2017) Glioblastoma multiforme: a review of its epidemiology and pathogenesis through clinical presentation and treatment. Asian Pac J Cancer Prev 18(1):3–9
Shergalis A, Bankhead A 3rd, Luesakul U, Muangsin N, Neamati N (2018) Current challenges and opportunities in treating glioblastoma. Pharmacol Rev 70(3):412–445
Perrin SL, Samuel SM, Koszyca B et al (2019) Glioblastoma heterogeneity and the tumour microenvironment: implications for preclinical research and development of new treatments. Biochem Soc Trans 47(2):625–638
Han S, Liu Y, Cai SJ et al (2020) IDH mutation in glioma: molecular mechanisms and potential therapeutic targets. Br J Cancer 122(11):1580–1589
Saadeh FS, Mahfouz R, Assi HI (2018) EGFR as a clinical marker in glioblastomas and other gliomas. Int J Biol Markers 33(1):22–32
Lu VM, O’Connor KP, Shah AH et al (2020) The prognostic significance of CDKN2A homozygous deletion in IDH-mutant lower-grade glioma and glioblastoma: a systematic review of the contemporary literature. J Neurooncol 148(2):221–229
Brito C, Azevedo A, Esteves S et al (2019) Clinical insights gained by refining the 2016 WHO classification of diffuse gliomas with: EGFR amplification, TERT mutations, PTEN deletion and MGMT methylation. BMC Cancer 19(1):968
Cakar B, Muslu U, Bozkurt E et al (2018) Angiogenesis inhibition on glioblastoma multiforme cell lines (U-87 MG and T98G) by AT-101. J Oncol Sci 4(2):65–69
Das S, Marsden PA (2013) Angiogenesis in glioblastoma. N Engl J Med 369(16):1561–1563
Folberg R, Maniotis AJ (2004) Vasculogenic mimicry. APMIS 112(7–8):508–525
Kreisl TN, Kim L, Moore K et al (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27(5):740–745
Field KM, Simes J, Nowak AK et al (2015) Randomized phase 2 study of carboplatin and bevacizumab in recurrent glioblastoma. Neuro Oncol 17(11):1504–1513
Carra E, Barbieri F, Marubbi D et al (2013) Sorafenib selectively depletes human glioblastoma tumor-initiating cells from primary cultures. Cell Cycle 12(3):491–500
Batchelor TT, Mulholland P, Neyns B et al (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31(26):3212–3218
Lombardi G, Zustovich F, Farina P et al (2013) Hypertension as a biomarker in patients with recurrent glioblastoma treated with antiangiogenic drugs: a single-center experience and a critical review of the literature. Anticancer Drugs 24(1):90–97
Wick W, Platten M, Wick A et al (2015) Current status and future directions of anti-angiogenic therapy for gliomas. Neuro Oncol 18(3):315–328
Cohen MH, Shen YL, Keegan P et al (2009) FDA drug approval summary: bevacizumab (Avastin®) as treatment of recurrent glioblastoma multiforme. Oncologist 14(11):1131–1138
Balañá C, Etxaniz O, Bugés C et al (2011) Approval denied by the European Medicines Agency (EMA) for bevacizumab in the treatment of high-grade glioma recurrence: a good idea or a grave error? Clin Transl Oncol 13(3):209–210
Dirven L, van den Bent MJ, Bottomley A et al (2015) The impact of bevacizumab on health-related quality of life in patients treated for recurrent glioblastoma: results of the randomised controlled phase 2 BELOB trial. Eur J Cancer 51(10):1321–1330
Gramatzki D, Roth P, Rushing EJ et al (2018) Bevacizumab may improve quality of life, but not overall survival in glioblastoma: an epidemiological study. Ann Oncol 29(6):1431–1436
Wick W, Gorlia T, Bendszus M et al (2017) Lomustine and bevacizumab in progressive glioblastoma. N Engl J Med 377(20):1954–1963
Friedman HS, Prados MD, Wen PY et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740
Desjardins A, Reardon DA, Coan A et al (2012) Bevacizumab and daily temozolomide for recurrent glioblastoma. Cancer 118(5):1302–1312
Desjardins A, Herndon JE 2nd, McSherry F et al (2019) Single-institution retrospective review of patients with recurrent glioblastoma treated with bevacizumab in clinical practice. Health Sci Rep 2(4):e114
Li Y, Ali S, Clarke J et al (2017) Bevacizumab in recurrent glioma: patterns of treatment failure and implications. Brain Tumor Res Treat 5(1):1–9
Ranjan S, Skorupan N, Ye X et al (2020) Patterns of bevacizumab use in patients with glioblastoma: an online survey among experts in neuro-oncology. Neurooncol Pract 7(1):52–58
Nagpal S, Harsh G, Recht L (2011) Bevacizumab improves quality of life in patients with recurrent glioblastoma. Chemother Res Practice 2011:1–6
Torres IJ, Mundt AJ, Sweeney PJ et al (2003) A longitudinal neuropsychological study of partial brain radiation in adults with brain tumors. Neurology 60(7):1113–1118
Brown PD, Jensen AW, Felten SJ et al (2006) Detrimental effects of tumor progression on cognitive function of patients with high-grade glioma. J Clin Oncol 24(34):5427–5433
Chinot OL, Wick W, Mason W et al (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370(8):709–722
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370(8):699–708
Sharma A, Low J, Mrugala MM (2019) Neuro-oncologists have spoken—the role of bevacizumab in the inpatient setting. A clinical and economic conundrum. Neurooncol Pract 6(1):30–36
Allegra CJ, Yothers G, O’Connell MJ et al (2013) Bevacizumab in stage II-III colon cancer: 5-year update of the National Surgical Adjuvant Breast and Bowel Project C-08 trial. J Clin Oncol 31(3):359
Herrlinger U, Schäfer N, Steinbach JP et al (2016) Bevacizumab plus irinotecan versus temozolomide in newly diagnosed O6-methylguanine–DNA methyltransferase nonmethylated glioblastoma: the randomized GLARIUS trial. J Clin Oncol 34(14):1611–1619
Boxerman JL, Zhang Z, Safriel Y et al (2013) Early post-bevacizumab progression on contrast-enhanced MRI as a prognostic marker for overall survival in recurrent glioblastoma: results from the ACRIN 6677/RTOG 0625 Central Reader Study. Neuro Oncol 15(7):945–954
Arevalo OD, Soto C, Rabiei P et al (2019) Assessment of glioblastoma response in the era of bevacizumab: longstanding and emergent challenges in the imaging evaluation of pseudoresponse. Front Neurol 10:460
Kim WY, Lee HY (2009) Brain angiogenesis in developmental and pathological processes: mechanism and therapeutic intervention in brain tumors. FEBS J 276(17):4653–4664
Gatto L, Franceschi E, Tosoni A et al (2021) Distinct MRI pattern of “pseudoresponse” in recurrent glioblastoma multiforme treated with regorafenib: Case report and literature review. Clin Case Reports 9(8):e04604
Österlund P, Soveri L, Isoniemi H et al (2011) Hypertension and overall survival in metastatic colorectal cancer patients treated with bevacizumab-containing chemotherapy. Br J Cancer 104(4):599–604
Lombardi G, De Salvo GL, Brandes AA et al (2019) Regorafenib compared with lomustine in patients with relapsed glioblastoma (REGOMA): a multicentre, open-label, randomised, controlled, phase 2 trial. Lancet Oncol 20(1):110–119
Zhong J, Ali AN, Voloschin AD et al (2015) Bevacizumab-induced hypertension is a predictive marker for improved outcomes in patients with recurrent glioblastoma treated with bevacizumab. Cancer 121(9):1456–1462
Carvalho B, Lopes RG, Linhares P et al (2020) Hypertension and proteinuria as clinical biomarkers of response to bevacizumab in glioblastoma patients. J Neurooncol 147(1):109–116
Rahbar A, Cederarv M, Wolmer-Solberg N et al (2016) Enhanced neutrophil activity is associated with shorter time to tumor progression in glioblastoma patients. Oncoimmunology 5(2):e1075693
Bambury R, Teo M, Power D et al (2013) The association of pre-treatment neutrophil to lymphocyte ratio with overall survival in patients with glioblastoma multiforme. J Neurooncol 114(1):149–154
Massara M, Persico P, Bonavita O et al (2017) Neutrophils in gliomas. Front Immunol 8:1349
Tecchio C, Cassatella MA (2014) Neutrophil-derived cytokines involved in physiological and pathological angiogenesis. Angiogenesis, Lymphangiogenesis Clin Implic 99:123–137
Bertaut A, Truntzer C, Madkouri R et al (2016) Blood baseline neutrophil count predicts bevacizumab efficacy in glioblastoma. Oncotarget 7(43):70948
Trifiletti DM, Alonso C, Grover S et al (2017) Prognostic implications of extent of resection in glioblastoma: analysis from a large database. World Neurosurg 103:330–340
Gittleman H, Lim D, Kattan MW et al (2017) An independently validated nomogram for individualized estimation of survival among patients with newly diagnosed glioblastoma: NRG Oncology RTOG 0525 and 0825. Neuro Oncol 19(5):669–677
Chaichana KL, Jusue-Torres I, Lemos AM et al (2014) The butterfly effect on glioblastoma: is volumetric extent of resection more effective than biopsy for these tumors? J Neurooncol 120(3):625–634
Puhalla S, Elmquist W, Freyer D et al (2015) Unsanctifying the sanctuary: challenges and opportunities with brain metastases. Neuro Oncol 17(5):639–651
Louveau A, Smirnov I, Keyes TJ et al (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523(7560):337–341
Weenink B, French PJ, Sillevis Smitt PA et al (2020) Immunotherapy in glioblastoma: current shortcomings and future perspectives. Cancers 12(3):751
Yu MW, Quail DF (2021) Immunotherapy for glioblastoma: current progress and challenges. Front Immunol 12:676301
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
CS wrote the article under the supervision of SD. ER carried out the statistical analysis. FD reviewed the article. All the other authors had an equal contribution. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the Gustave Roussy Cancer Center.
Informed consent
Patient consent was waived due to the death of the patients. We sent a letter to the families of the patients to inform them of this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Smolenschi, C., Rassy, E., Pallud, J. et al. Bevacizumab in real-life patients with recurrent glioblastoma: benefit or futility?. J Neurol 270, 2702–2714 (2023). https://doi.org/10.1007/s00415-023-11600-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11600-w