Abstract
Some patients with primary central nervous system lymphoma (PCNSL) may initially present with similar clinical, magnetic resonance imaging, and routine cerebrospinal fluid (CSF) findings as those observed in multiple sclerosis (MS). The MRZ reaction (MRZR), composed of the three respective antibody indices (AIs) against measles, rubella, and varicella zoster virus, appears to be the most specific CSF marker for MS. This study aimed to determine whether a positive MRZR and other routine CSF markers help differentiate between MS and PCNSL. Data regarding brain biopsy, CSF routine tests, cytopathological examination and immunophenotyping of CSF cells were assessed in 68 PCNSL patients. MRZR was determined, as possible, in PCNSL patients (n = 37) and in those with MS (n = 74; age and sex matched to PSCNL patients) and psychiatric disorders (PD; n = 78). Two stringency levels for a positive antibody index (AI) evaluation (AI ≥ 1.5 and 2.0) were applied, and MRZR was considered positive in cases with ≥ 2 positive AIs (MRZR-2). Using the common AI threshold of ≥ 1.5, MS patients exhibited positive MRZR-2 (58.1%) more frequently than PCNSL (8.1%) and PD patients (2.6%; p < 0.0001 for each comparison with the MS group) corresponding to a positive predictive value (PPV) of 89.6% and a negative predictive value (NPV) of 78.0%. On applying the stricter AI threshold of ≥ 2.0, 37.8% of MS patients were MRZR-2 positive; however, all patients with PCNSL and PD were MRZR-2 negative (p < 0.0001 for each comparison with the MS cohort) resulting in a PPV of 100% and an NPV of 71.4%. Consequently, a positive MRZR-2 result may contribute toward the distinction between MS and PCNSL owing to its high specificity and PPV for MS in the context of the present study. Among the other CSF parameters only a quantitative intrathecal IgG synthesis (present in 49.3% of MS patients but in none of the PCNSL or PD patients; p < 0.0001 for each comparison with the MS group) reliably indicated MS rather than PCNSL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is a form of extranodal non-Hodgkin lymphoma without the evidence of systemic spread that mainly affects the brain and less frequently the cerebrospinal fluid (CSF), eyes or the spinal cord. PCNSL accounts for about 6% of all cases of malignant brain neoplasia [1, 2]. Histopathologically, PCNSL is a B-cell lymphoma in > 96% [3] that expresses monoclonal light chain immunoglobulins (Igs) in 90% [4]. Even though immunodeficiency is a strong predisposing factor, PCNSL also occurs in immunocompetent subjects at an average age of 55 years with an increase in the incidence rates over the past few decades [4]. Patients with PCNSL gradually develop neurologic symptoms within days or weeks. The most frequent symptoms are focal neurologic deficits (56–70%) [1], including hemiparesis and, less commonly, blurred vision or decreased visual acuity owing to an involvement of one or both eyes (10%) [4, 5]. Thus, PCNSL can mimic the clinical onset of multiple sclerosis (MS), especially of the primary progressive MS (PPMS) which usually starts at around 50 years of age [6]. In up to 50% of immunocompetent PCNSL patients, magnetic resonance imaging (MRI) initially shows multiple and often bilateral periventricular lesions that may appear very similar to those observed in MS [4]. In the CSF analyses of PCNSL patients, routine parameters often show only unspecific alterations (e.g. slightly increased total cell count in up to 50% and oligoclonal bands (OCB) in 30% [4]; both findings compatible with MS also). Cytopathological examinations of the CSF cells reveal leptomeningeal dissemination of PCNSL in only 10–15% [7, 8]. Thus, making a distinction between MS and PCNSL can be challenging in some cases and require a brain biopsy, the diagnostic gold standard [9].
The MRZ reaction (MRZR) is a polyspecific intrathecal humoral immune response found in patients with MS. It comprises antibody synthesis against the three most frequent antigens measles (M), rubella (R), and varicella zoster (Z), assessed using the three respective antibody indices (AIs) [10]. Several studies have shown a positive MRZR in the majority of relapsing–remitting MS (RRMS) patients [11] as well as in PPMS patients [6]. The pathophysiological role of MRZR remains unclear to date; the main clinical significance is its potential to contribute to the differential diagnosis of MS because a positive MRZR appears highly specific for MS [11]. This is especially helpful in distinguishing MS patients from healthy subjects [12] and those with autoimmune [13,14,15] or infectious MS-mimics [16, 17]. However, the prevalence of a positive MRZR in PCNSL is unknown. Therefore, this study aimed to assess the frequency of a positive MRZR in PCNSL patients compared to that in patients with MS and those with psychiatric disorders (PD).
Patients, materials, and methods
Patients
This was a retrospective study that enrolled patients treated at the Medical Centre of the University Freiburg in Germany between 2005 and 2017, using an electronic database search. Lumbar puncture (LP) had already been performed in all patients for clinical purposes after obtaining written consent. PCNSL patients were diagnosed by oncologists of the Department of Haematology, Oncology, and Stem-Cell Transplantation according to the respective criteria for the baseline evaluation for PCNSL [9]. Except the patients with a sole intraocular manifestation (often classified as PCNSL) without any central nervous system (CNS) affection, all available PCNSL patients with recorded results of the respective brain biopsy and CSF analyses at the time of first diagnosis were enrolled. MS patients were selected from a cohort (comprising 103 PPMS patients and 100 RRMS patients) from an earlier study [6] using a previously established in-house matching software [19] to select age- and sex-matched MS patients in a 2:1 (MS:PCNSL) ratio. A diagnosis of MS was established according to the 2010 revised McDonald criteria [18]. The disease duration of MS patients was determined according to medical records as the time interval between clinical onset and the LP. For comparing these two study groups comprising patients with neurological disorders, 78 patients with PD were included. These PD patients were studied in a recent project that assessed the prevalence of MRZR in 39 patients with schizophreniform syndromes and 39 patients with bipolar disorders [20]. Data concerning the ethnicity and immunization status of the study patients were unavailable. The ethics committee of the Medical Centre of the University Freiburg approved the study (EK-Fr 489/14).
Materials and methods
MRZR was analysed at the Department of Virology of the University of Freiburg. All routine CSF measurements were conducted in the CSF laboratory of the University Freiburg. Total immunoglobulin (Ig) concentrations in the serum and the CSF were determined nephelometrically (ProSpect System, Siemens, Germany), while measles-, rubella- and varicella-(IgGspec) levels in the CSF and the serum were measured using an enzyme-linked immunosorbent assay (Serion classic ELISA, Germany). MRZR was determined from the three respective virus-specific AIs that were calculated as follows: AI (antibody index) = QIgG[spec]/QIgG[total], if QIgG[total] < Qlim, and AI = QIgG[spec]/Qlim, if QIgG[total] > Qlim [21]. For a positive AI result indicative of intrathecal IgG production against the respective pathogen, two different thresholds were applied as described in earlier studies: ≥ 1.5 [22] and ≥ 2.0 [23]. Most previous studies have varied as to how many positive AIs are required for a positive MRZR [6]. In this study, MRZR-2 (defined as at least two positive AIs) was used because of its higher specificity for MS [6, 11]. In cases where an AI could not be calculated because no antibodies could be detected in the CSF, the AI was considered as 1.0 (negative) [6, 15]. The individual age-related normal range of albumin quotient (QAlb) was calculated according to Reiber’s formula: QAlb < (4 + age/15) × 10−3 [24].
This study focused on PCNSL; therefore, additional data regarding the following items were obtained from the patients’ medical records: (1) brain biopsy assessment that was routinely performed at the Department of Pathology; (2) CSF routine analyses (including total cell count, age-related albumin quotient, quantitative intrathecal antibody synthesis, and OCB); (3) cytopathological examination of the CSF cells that was routinely performed at the Department of Pathology and (4) immunophenotyping of the CSF cells using flow cytometric analyses routinely performed at the Department of Haematology, Oncology, and Stem-Cell Transplantation.
The specificity of MRZR was calculated as true negatives/(true negatives + false positives) and the sensitivity as true positives/(true positives + false negatives). The positive predictive value (PPV) of MRZR was calculated as true positives/(true positives + false positives) and the negative predictive value (NPV) as true negatives/(true negatives + false negatives).
Statistical analyses
Statistical testing of the differences between the study groups with respect to sex, prevalence of positive MRZ-AIs, prevalence of positive MRZR, and prevalence of abnormal CSF results was performed using the Fisher’s exact test (two-tailed). Comparisons of the metric parameters (mean MRZ-AI and mean age) were performed using the Kruskal–Wallis test with Dunn’s post-test. A p value < 0.05 was considered statistically significant.
Results
Study population
In total, 261 patients with a documented diagnosis of PCNSL were retrospectively screened for the correct diagnosis according to the brain biopsy results and sufficient clinical and CSF data as well as enough available CSF/serum samples for the determination of MRZR. In 193 (73.9%) of these patients, no CSF analysis had been performed at the Medical Centre of the University Freiburg; the most frequent reasons for this included previous CSF analysis elsewhere or unwillingness of the patient to undergo LP. Detailed histopathological, CSF, and brain MRI results were available for the remaining 68 patients with a documented diagnosis of PCNSL. In 31 of these 68 PCNSL patients, there were no CSF/serum samples available; therefore, those patients could not be included in the MRZR analyses. Finally, in 37 well-characterized PCNSL patients, MRZR could be determined. Table 1 shows the key demographic features of the three MRZ study groups. MS patients (comprising 53 patients with PPMS and 21 with RRMS) were younger than the PSCNL patients and older compared to the PD patients. The mean disease duration of MS patients was 5.6 years (range 0–39; SD 7.3). There were no significant differences in the sex distribution in the three groups.
Virus-specific antibody indices
Results of the single MRZ-AIs in the three study cohorts are presented in Table 2. More MS patients had two or three positive AIs than patients of both the other study groups. No statistically significant differences were found in the mean values of any of the three AIs of the PCNSL and PD patients. However, compared to these two non-MS groups, MS patients had significantly more frequent positive AIs and higher mean AI values for all the three viruses.
MRZR
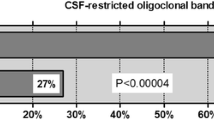
A positive MRZR-2 was found in few patients with PCNSL (8.1%) and PD (2.6%; p > 0.05) using the common AI threshold of ≥ 1.5. In contrast to both these study groups, the MS cohort showed a statistically significantly higher prevalence of positive MRZR-2 (58.1%; p < 0.0001 for each comparison with the MS group; Fig. 1). In the context of the present study groups, the MRZR-2 specificity for MS was 95.7%, the PPV was 89.6% and the NPV was 78.0%.
Frequency of positive MRZR-2 (≥ 2 positive antibody indices for measles, rubella, or varicella zoster) in patients with primary central nervous system lymphoma (PCNSL), multiple sclerosis (MS), and psychiatric disorders (PD) using two different thresholds for a positive antibody index (AI) result: ≥ 1.5 (left) and ≥ 2.0 (right)
Applying the more stringent threshold of ≥ 2.0 for positive AI gave no positive MRZR-2 in both, the PCNSL and PD patients; whereas the MRZR-2 sensitivity for MS was 37.8% (p < 0.0001 for each comparison with the MS group; Fig. 1). Consequently, with a threshold of > 2.0 for positive AI, the specificity and PPV of MRZR-2 for MS rose to 100%; whereas the NPV decreased to 71.4% in the present study cohorts.
Clinical and paraclinical baseline characteristics of the three MRZR-2-positive PCNSL patients are shown in Table 3; none of them fulfilled the revised McDonald criteria for MS [18]. The two MRZR-2 positive PD patients (both diagnosed with an endogenous schizodepressive disorder) have been described in detail in a recent study [20]; most importantly, they did not show any clinical or paraclinical signs of MS, and consequently did not fulfil the 2010 revised McDonald criteria [18].
Histopathological findings in PCNSL patients
Brain biopsy of the 68 PCNSL patients showed malignant B-cell non-Hodgkin lymphoma in 67 cases (98.5%) and an anaplastic T-cell lymphoma in one patient (1.5%). Cytopathological analyses of the CSF cells were performed for 44 PCNSL patients; lymphoma cells were detected in one patient (2.3%).
CSF findings in patients with PCNSL and MS
The majority of the 68 PCNSL patients (89.7%) and the 74 MS patients (93.2%; p > 0.05) showed at least one abnormal routine CSF parameter. In PCNSL patients, the most frequent pathological findings included a dysfunction of the blood–CSF barrier (elevated QAlb in 69.1%) followed by an elevated total CSF cell count (50.0%; mean cell count of pleocytosis: 11.0/µL; range 5–29/µL; standard deviation (SD) 6.4) which was observed less frequently in MS patients (insufficient data regarding QAlb; elevated cell count in 25.0%, p < 0.01; mean cell count of pleocytosis: 14.1/µL, range 5–38/µL; SD 9.3). Within the MS cohort, RRMS patients had higher CSF cell counts in case of pleocytosis (19.6/µL) compared to PPMS patients (9.6/µL; p < 0.05). In PCNSL patients, intrathecal synthesis of Igs was found in 15.6% (IgM) (isolated IgM synthesis in 11.2%) and in 4.4% (IgA); while a quantitative intrathecal synthesis of IgG was not found in any PCNSL patient. There was intrathecal synthesis of IgG in 49.3% (p < 0.0001), and that of IgA or IgM in 10.0% (p > 0.05 for both compared to PCNSL patients) of the MS patients. OCB, exclusively in the CSF, were observed in 15.6% of the PCNSL patients; identical OCB in the CSF and serum and an elevated CSF lactate level were less frequent (both 13.3%). MS patients more frequently exhibited OCB in the CSF (91.9%; p < 0.0001); data regarding CSF lactate levels were not available for all MS patients. Within the MS group, there were no significant differences regarding MRZR-2 positivity, the quantitative intrathecal synthesis of IgG/A/M and OCB positivity between RRMS and PPMS patients. Immunophenotyping of the CSF cells was performed in 53 PCNSL patients with results indicative for PCNSL (increased CD 20- and CD19-positive B cells with monoclonal surface Igs) in 7.5%.
Discussion
To our knowledge, this is the first investigation of MRZR in PCNSL patients. The main findings were that PCNSL patients may show similar clinical features and routine CSF results as MS patients; however, a positive MRZR-2 with the AI threshold of ≥ 2.0 and a quantitative intrathecal IgG synthesis were only found in MS patients.
MRZR
In the present PCNSL cohort, MRZR-2 (using the standard AI threshold of ≥ 1.5) was found negative in the vast majority of patients, similar to patients with rheumatologic disorders with CNS involvement (own data under review), acute disseminated encephalomyelitis [15], neuromyelitis optica [13], paraneoplastic neurological disorders [14] and neurosarcoidosis [15], corresponding to a specificity of > 90% in the context of these important differential diagnoses of MS. This is in line with a recent MRZR review that reported an overall MRZR-2 specificity of 97% for MS in a meta-analysis that did not include data of PCNSL patients [11]. By using the more stringent AI threshold of ≥ 2.0 the MRZR-2 specificity and PPV for MS could be further increased to even 100% (with a reduced sensitivity of almost 40%) in the present study. Consequently, MRZR-2 does not appear to be a general marker of chronic autoimmune inflammatory CNS processes as was once suggested more than 20 years ago [25].
The reasons for the MRZR-2 positivity in the three PCNSL patients in the current study remain unclear. Each of the three MRZR-2 positive PCNSL patients had one AI = 1.0, indicating that the other two slightly increased AIs were not false-positive results owing to general protein alterations. It is conceivable that the PCNSL might have induced the IgG production against the MRZ viruses because PCNSL patients are known to occasionally exhibit intrathecal synthesis of IgM [26] or oligoclonal IgG [4], even in the absence of detectable leptomeningeal dissemination. The distinct brain biopsy result, the absence of a history of symptoms suggestive of MS relapses, and the unfulfilled McDonald criteria [18] in all the MRZR-2-positive PCNSL patients are arguments against the simultaneous presence of MS. As expected, the prevalence of positive MRZR-2 in PD patients was very low. Similar to the MRZR-2 positive PCNSL patients, the two MRZR-2 positive PD patients showed only slight elevations in the AIs (≤ 1.9), potentially owing to an unspecific phenomenon, considering that these two patients did not exhibit any clinical or paraclinical signs of MS or any other inflammatory neurological disorder. A similar MRZR-2 positivity (with the standard AI threshold of ≥ 1.5), as exhibited by the present MS group, has also been reported in several previous studies [10, 22, 27, 28], and in the recent comprehensive MRZR review [11]. It has to be mentioned, that the mean disease duration and age of MS patients were unusual high for the first diagnosis of RRMS. This was most probably due to the matching with PCNSL patients leading to a PPMS-dominated MS cohort with older patients in a more advanced state of their individual disease course.
Further diagnostic findings in PCNSL patients
The routine CSF results of the PCNSL cohort (dysfunction of the blood–CSF barrier in 69%, elevated cell count in 50%, and OCB in 29%) matched those described for PCNSL patients in a previous study (elevated total protein in 70–90%, increased total cell count in about 50%, and OCB in 30%) [4], confirming these alterations as the distinctive routine CSF pattern of PCNSL patients. Among the CSF Ig parameters, an isolated intrathecal IgM synthesis was the most frequent finding in the present PCNSL cohort; a finding which has been previously reported [29]. The complete absence of a quantitative intrathecal synthesis of IgG in our PCNSL patients is supported by the findings of an earlier study [26]. In contrast, the quantitative intrathecal synthesis of IgG (observed in around 50% of the patients in the present MS cohort and as reported by Reiber et al. [22]) is the most frequent type of a quantitative intrathecal Ig synthesis in MS patients, indicating its good discriminative potential for distinguishing between MS and PCNSL. The combination of no quantitative IgG synthesis, but positive OCB in the CSF (found in around 50% of the MS patients studied previously by our research group [6]) has a much lower discriminative value because this combination was also found in 30% of the patients in the present PCNSL cohort. Further, a slight-to-moderate dysfunction of the blood–CSF barrier was found in 20% of MS patients, indicating a relatively weak discriminative potential of this most frequent abnormal CSF parameter in PCNSL patients [30]. In line with the study by Korfel el al. [8], immunophenotyping and cytopathological analyses did not detect features indicative of lymphoma in the vast majority of the present PCNSL patients, and thus did not contribute substantially to the differential diagnosis. Future biomarkers for detecting PCNSL prior to brain biopsy might be the microRNAs miR-21, miR-19, and miR-92a in the CSF because they were found to have a combined sensitivity and specificity of > 95% each, in the context of the respective study that included 17 MS patients as inflammatory controls [31]. In summary, the present CSF data suggest that of all the available established CSF parameters, only a positive MRZR-2 (with AI threshold ≥ 2.0) and a quantitative intrathecal synthesis of IgG seem indicators of MS in the context of PCNSL as differential diagnosis; although a quantitative intrathecal synthesis of IgG is not specific for MS, as it is the case with MRZR.
Regarding brain biopsy, the undisputed diagnostic gold standard, one should consider that there are reports of PCNSL patients with a misleading first biopsy result showing either only inflammatory demyelination indistinguishable from MS lesions [32, 33] or normal brain tissue after steroid treatment [34]. This did not happen in the present PCNSL cohort; however, it is a very relevant diagnostic problem that highlights the importance of establishing and using additional diagnostic markers for identifying patients who require a second brain biopsy in case of persistent diagnostic uncertainty following the first biopsy.
Limitations
The most important limitations of the present study include the monocentric, retrospective design and the limited number of patients with PCNSL. Nevertheless, to our knowledge, this is the first investigation of MRZR in this diagnosis group, the mean age of which, matches that of a larger British PCNSL cohort indicating that the present PCNSL group was a representative sample [35]. Despite the matching of the MS and the PCNSL groups, there were significant age differences between all three study groups that should be considered because patient age may have an effect on the prevalence of positive MRZR outcomes, as illustrated by the lower numbers in paediatric MS patients compared to those in the adult patients [36]. Further study limitations include the lack of data concerning ethnicity and vaccination status. This is important as local infection rates and vaccination status with respect to the three MRZ viruses may have influenced the MRZR results, as has been exemplarily shown for the rubella virus in Cuba [37]. Therefore, future validation attempts of the present MRZR results should conduct prospective trials on larger, multiethnic PCNSL cohorts with known vaccination status.
Conclusions
PCNSL may initially be difficult to distinguish from MS owing to their clinical and radiological similarities [32]. However, apart from the comparably invasive brain biopsy, the only quite MS-specific diagnostic marker that reliable indicates MS rather than PCNSL in the present study cohorts was a positive MRZR-2 with an AI threshold of ≥ 2.0. Thereby, the present study further strengthens the significance of CSF analyses as a valuable tool for ensuring prompt detection as well as differential diagnosis of MS [38].
Abbreviations
- AI:
-
Antibody index
- AIs:
-
Antibody indices
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- ECOG PS:
-
Eastern Cooperative Oncology Group Performance Status
- Ig:
-
Immunoglobulin
- IgG/M/A:
-
Immunoglobulin G/M/A
- LDH:
-
Lactate dehydrogenase
- LP:
-
Lumbar puncture
- MRI:
-
Magnetic resonance imaging
- MRZR:
-
Measles virus, rubella virus, and varicella zoster virus reaction
- MS:
-
Multiple sclerosis
- NPV:
-
Negative predictive value
- OCB:
-
Oligoclonal bands
- PCNSL:
-
Primary central nervous system lymphoma
- PD:
-
Psychiatric disorders
- PPMS:
-
Primary progressive MS
- PPV:
-
Positive predictive value
- QAlb:
-
Albumin quotient
- RRMS:
-
Relapsing–remitting MS
- SD:
-
Standard deviation
References
Grommes C, DeAngelis LM (2017) Primary CNS lymphoma. J Clin Oncol JCO2017727602. https://doi.org/10.1200/jco.2017.72.7602
Ostrom QT, Gittleman H, Xu J et al (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neurooncology 18(suppl_5):v1–v75. https://doi.org/10.1093/neuonc/now207
Bataille B, Delwail V, Menet E et al (2000) Primary intracerebral malignant lymphoma: report of 248 cases. J Neurosurg 92(2):261–266. https://doi.org/10.3171/jns.2000.92.2.0261
Schabet M, Herrlinger U, Weller M et al (1997) Neue Entwicklungen in Diagnostik und Therapie primärer non-Hodgkin-Lymphome des zentralen Nervensystems (New developments in diagnosis and therapy of primary non-Hodgkin’s lymphoma of the central nervous system). Nervenarzt 68(4):298–308
Grimm SA, Pulido JS, Jahnke K et al (2007) Primary intraocular lymphoma: an international primary central nervous system lymphoma collaborative group report. Ann Oncol 18(11):1851–1855. https://doi.org/10.1093/annonc/mdm340
Hottenrott T, Dersch R, Berger B et al (2017) The MRZ reaction in primary progressive multiple sclerosis. Fluids Barriers CNS 14(1):2. https://doi.org/10.1186/s12987-016-0049-7
Fischer L, Martus P, Weller M et al (2008) Meningeal dissemination in primary CNS lymphoma: prospective evaluation of 282 patients. Neurology 71(14):1102–1108. https://doi.org/10.1212/01.wnl.0000326958.52546.f5
Korfel A, Weller M, Martus P et al (2012) Prognostic impact of meningeal dissemination in primary CNS lymphoma (PCNSL): experience from the G-PCNSL-SG1 trial. Ann Oncol 23(9):2374–2380. https://doi.org/10.1093/annonc/mdr627
Abrey LE, Batchelor TT, Ferreri AJM et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23(22):5034–5043. https://doi.org/10.1200/jco.2005.13.524
Felgenhauer K, Reiber H (1992) The diagnostic significance of antibody specificity indices in multiple sclerosis and herpes virus induced diseases of the nervous system. Clin Investig 70(1):28–37
Jarius S, Eichhorn P, Franciotta D et al (2017) The MRZ reaction as a highly specific marker of multiple sclerosis: re-evaluation and structured review of the literature. J Neurol 264(3):453–466. https://doi.org/10.1007/s00415-016-8360-4
Wurster U, Stachan R, Windhagen A et al (2006) Reference values for standard cerebrospinal fluid examinations in multiple sclerosis. Results from 99 healthy volunteers. Mult Scler 12:P248
Jarius S, Franciotta D, Bergamaschi R et al (2008) Polyspecific, antiviral immune response distinguishes multiple sclerosis and neuromyelitis optica. J Neurol Neurosurg Psychiatry 79(10):1134–1136. https://doi.org/10.1136/jnnp.2007.133330
Jarius S, Eichhorn P, Jacobi C et al (2009) The intrathecal, polyspecific antiviral immune response: specific for MS or a general marker of CNS autoimmunity? J Neurol Sci 280(1–2):98–100. https://doi.org/10.1016/j.jns.2008.08.002
Hottenrott T, Dersch R, Berger B et al (2015) The intrathecal, polyspecific antiviral immune response in neurosarcoidosis, acute disseminated encephalomyelitis and autoimmune encephalitis compared to multiple sclerosis in a tertiary hospital cohort. Fluids Barriers CNS 12:27. https://doi.org/10.1186/s12987-015-0024-8
Bednárová J, Stourac P, Adam P (2005) Relevance of immunological variables in neuroborreliosis and multiple sclerosis. Acta Neurol Scand 112(2):97–102. https://doi.org/10.1111/j.1600-0404.2005.00418.x
Puccioni-Sohler M, Kitze B, Felgenhauer K et al (1995) The value of CSF analysis for the differential diagnosis of HTLV-I associated myelopathy and multiple sclerosis. Arq Neuropsiquiatr 53(4):760–765
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69(2):292–302. https://doi.org/10.1002/ana.22366
Kaller CP, Loosli SV, Rahm B et al (2014) Working memory in schizophrenia: behavioral and neural evidence for reduced susceptibility to item-specific proactive interference. Biol Psychiatry 76(6):486–494. https://doi.org/10.1016/j.biopsych.2014.03.012
Endres D, Huzly D, Dersch R, Stich O, Berger B, Schuchardt F, Perlov E, Venhoff N, Hellwig S, Fiebich BL, Erny D, Hottenrott T, Tebartz van Elst L (2017) Do patients with schizophreniform and bipolar disorders show an intrathecal, polyspecific, antiviral immune response? A pilot study. Fluids Barriers CNS 14(1):34. https://doi.org/10.1186/s12987-017-0082-1
Reiber H (1998) Cerebrospinal fluid-physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult Scler 4(3):99–107. https://doi.org/10.1177/135245859800400302
Reiber H, Ungefehr S, Jacobi C (1998) The intrathecal, polyspecific and oligoclonal immune response in multiple sclerosis. Mult Scler 4(3):111–117. https://doi.org/10.1177/135245859800400304
Derfuss T, Hohlfeld R, Meinl E (2001) Multiple sclerosis. Chlamydia hypothesis in debate (Multiple Sklerose. Chlamydien-Hypothese in der Diskussion). Nervenarzt 72(10):820–823
Reiber H (1994) Flow rate of cerebrospinal fluid (CSF)—a concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J Neurol Sci 122(2):189–203
Graef IT, Henze T, Reiber H (1994) Polyspezifische Immunreaktion im ZNS bei Autoimmunerkrankungen mit ZNS-Beteiligung (Polyspecific immune reaction in the central nervous system in autoimmune diseases with CNS involvement). Z Arztl Fortbild (Jena) 88(7–8):587–591
Reiber H (2016) Cerebrospinal fluid data compilation and knowledge-based interpretation of bacterial, viral, parasitic, oncological, chronic inflammatory and demyelinating diseases. Diagnostic patterns not to be missed in neurology and psychiatry. Arq Neuropsiquiatr 74(4):337–350. https://doi.org/10.1590/0004-282x20160044
Rosche B, Laurent S, Conradi S et al (2012) Measles IgG antibody index correlates with T2 lesion load on MRI in patients with early multiple sclerosis. PLoS One 7(1):e28094. https://doi.org/10.1371/journal.pone.0028094
Kułakowska A, Mroczko B, Mantur M et al (2012) Multiplexing analysis of the polyspecific intrathecal immune response in multiple sclerosis. Methods 56(4):528–531. https://doi.org/10.1016/j.ymeth.2012.03.002
Reiber H, Peter JB (2001) Cerebrospinal fluid analysis: disease-related data patterns and evaluation programs. J Neurol Sci 184(2):101–122
Liebsch R, Kornhuber ME, Dietl D et al (1996) Blood-CSF barrier integrity in multiple sclerosis. Acta Neurol Scand 94(6):404–410
Baraniskin A, Kuhnhenn J, Schlegel U et al (2011) Identification of microRNAs in the cerebrospinal fluid as marker for primary diffuse large B-cell lymphoma of the central nervous system. Blood 117(11):3140–3146. https://doi.org/10.1182/blood-2010-09-308684
Ohe Y, Hayashi T, Mishima K et al (2013) Central nervous system lymphoma initially diagnosed as tumefactive multiple sclerosis after brain biopsy. Intern Med 52(4):483–488
Kuroda Y, Kawasaki T, Haraoka S et al (1992) Autopsy report of primary CNS B-cell lymphoma indistinguishable from multiple sclerosis: diagnosis with the immunoglobulin gene rearrangements analysis. J Neurol Sci 111(2):173–179
Chayasirisobhon S, Kumar V, Ali I et al (1987) Primary lymphoma of the central nervous system: a diagnostic problem. J Natl Med Assoc 79(2):198–200
Bessell EM, Dickinson P, Dickinson S et al (2011) Increasing age at diagnosis and worsening renal function in patients with primary central nervous system lymphoma. J Neurooncol 104(1):191–193. https://doi.org/10.1007/s11060-010-0457-5
Reiber H, Teut M, Pohl D et al (2009) Paediatric and adult multiple sclerosis: age-related differences and time course of the neuroimmunological response in cerebrospinal fluid. Mult Scler 15(12):1466–1480. https://doi.org/10.1177/1352458509348418
Robinson-Agramonte M, Reiber H, Cabrera-Gomez JA et al (2007) Intrathecal polyspecific immune response to neurotropic viruses in multiple sclerosis: a comparative report from Cuban patients. Acta Neurol Scand 115(5):312–318. https://doi.org/10.1111/j.1600-0404.2006.00755.x
Tumani H, Deisenhammer F, Giovannoni G et al (2011) Revised McDonald criteria: The persisting importance of cerebrospinal fluid analysis. Ann Neurol 70(3):520. https://doi.org/10.1002/ana.22508 (author reply 521)
Acknowledgements
Special thanks are due to the staff of the Institute of Virology who performed the immunoassays for the MRZ-AI and to the staff of the CSF laboratory at the Department of Neurology who analysed the CSF/serum samples for the routine parameters.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The cost of the article-processing charge was covered by the Albert Ludwig University of Freiburg.
Author information
Authors and Affiliations
Contributions
TH and ES initiated this study. TH performed parts of the statistical analyses and wrote the manuscript. ES and KF identified the PCNSL patients; DE and LTvE provided the psychiatric patients group. RD performed parts of the statistical analyses. DH supervised performance of the immunoassays in the Institute of Virology. OS supervised the performance of the CSF analyses. OS and DE supervised the study. All authors helped to draft the manuscript, read and approved the final manuscript version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the University Freiburg approved the study (EK-Fr 489/14).
Consent for publication
Not applicable.
Availability of data and supporting materials section
The data that support the findings of this study are included in this study or available from the corresponding author upon reasonable request.
Conflicts of interest
TH received travel grants from Bayer Vital GmbH and Novartis. ES, KF, RD and DE report no conflicts of interest with this study. BB received travel grants and/or training expenses from Bayer Vital GmbH, Ipsen Pharma GmbH, Norvartis, and Genzyme, as well as lecture fees from Ipsen Pharma GmbH. DH received lecture fees from Serion. LTvE received consulting and lecture fees, grant and research support from Eli Lilly, Janssen-Cilag, Novartis, Shire, UCB, GSK, Servier, Janssen, and Cyberonics. OS and SR report receiving consulting and lecture fees, grant and research support from Baxter, Bayer Vital GmbH, Biogen Idec, Genzyme, Merck Serono, Novartis, RG, Sanofi-Aventis and Teva. Furthermore, SR indicates that he is a founding executive board member of ravo Diagnostika GmbH (Oltmannsstraße 5, D-79100 Freiburg, Germany), which is selling in vitro diagnostic medical devices for the detection of infectious diseases and paraneoplastic autoantibodies.
Author information
All authors except OS are doctors working at the Medical Centre-University Freiburg, Germany; OS is working as a consultant physician at the medical care unit in Konstanz, Germany. TH, RD and DE are resident physicians; ES and KF are consultant physicians; BB and DH are senior physicians. SR and LTvE are chief physicians.
Rights and permissions
About this article
Cite this article
Hottenrott, T., Schorb, E., Fritsch, K. et al. The MRZ reaction and a quantitative intrathecal IgG synthesis may be helpful to differentiate between primary central nervous system lymphoma and multiple sclerosis. J Neurol 265, 1106–1114 (2018). https://doi.org/10.1007/s00415-018-8779-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8779-x