Abstract
Muscle β-enolase deficiency is a very rare inherited metabolic myopathy caused by an enzymatic defect of distal glycolysis. So far, the condition has been described in only one patient with mutations in ENO3 in a compound heterozygous state who presented with exercise intolerance, post-exercise myalgia and mild hyperCKemia but no pigmenturia. We describe two men, one Italian and one Turkish, with consanguineous parents, who complained of several episodes of intense myalgia, cramps, generalized muscle tenderness and dark urine. No other family members reported similar symptoms. In both cases, there was a very mild rise in lactate during a forearm exercise test. Muscle biopsy showed minimal changes with no lipid or glycogen accumulation. Biochemical studies on muscle tissue demonstrated a marked reduction of muscle β-enolase activity (20 and 10 % of residual activity, respectively). Molecular genetic analysis of ENO3 gene revealed two novel homozygous missense mutations, (p.Asn151Ser and p.Glu187Lys). Both mutations segregated as expected in the two families. Although quite rare, muscle β-enolase deficiency should be considered in the differential diagnosis of patients presenting with recurrent rhabdomyolysis. It may present also with a more severe phenotype than previously thought.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enolase is an important enzyme of terminal glycolysis which catalyzes the interconversion of 2-phosphoglyceric acid (PGA) and phosphoenolpyruvate. For several species, enolases are dimeric, with subunit molecular masses of 40000–50,000 Da [1].
In mammals, enolase is composed by three subunits (α, β, γ), encoded by three different genes; the subunits associate to form both homo- and heterodimers. The α subunit is expressed in many tissues, γ primarily in neurones whereas β is prevalent in muscle [2].
Chronologically, muscle β-enolase deficiency was the last discovered enzyme deficiency among the distal glycolytic defects. In fact, in 2001, Comi et al. [3] reported the first patient presenting with a benign phenotype characterized by exercise intolerance, myalgia after physical exertion, mild hyperCKemia but no pigmenturia. Muscle β-enolase residual activity was about 5 %; the patient harbored two heterozygous mutations in ENO3 gene [3].
Two new patients are reported herein with genetically confirmed β-enolase deficiency, both presenting with a severe phenotype including recurrent episodes of acute rhabdomyolysis.
Cases report
Case 1 A 44-year-old Italian man, born from consanguineous parents, complained of symptoms since his 20s, which included several episodes characterized by myalgia, cramps, generalized muscle tenderness and presence of intense dark urine. At 42 years of age, he developed muscle aches and generalized muscle weakness after vigorous physical exercise followed by acute renal insufficiency with anuria. Because of the presence of a massive rhabdomyolysis (serum CK was 214,000 IU/L) and myoglobinuria, he urgently required multiple dialysis cycles to obtain immediate restoration of renal function. After few weeks, he was referred to the University Neuromuscular Centre of Messina for investigations for exercise intolerance, persistent cramps and myalgia.
At that time, neurological examination was unremarkable; he was overweight with a BMI of 27 kg/m2. Laboratory investigations, at rest, showed normal serum CK levels (208 IU/L n.v. 0–200). He achieved a walking distance of 282 m during a 6-min walk test (6MWT).
Neurophysiological examination, including electromyography and nerve conduction velocities, revealed a myopathic pattern with reduced amplitude and duration of MUP (10.3 mV) with mean duration on quadriceps −28 %.
Cardiac assessment with electrocardiogram and echocardiography was normal.
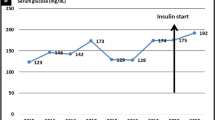
Forearm ischemic exercise test evidenced no venous lactate rise (Fig. 1). Muscle MRI revealed mild fatty infiltration of the distal part of the thighs.
Case 2 A 28-year-old Turkish male was referred to the Neuromuscular Centre at the National Hospital for Neurology and Neurosurgery of London with a history of exercise-induced muscle pain and cramps. His parents were also consanguineous. Symptoms had been present since early childhood; he was able to jog slowly, but never able to run quickly for more than a few minutes without stopping due to myalgia and cramps. He also developed similar symptoms when walking quickly or up an incline. From 17 years of age, he had a number of episodes of myalgia and weakness affecting lower limbs and paraspinal muscles associated with “coca-cola” colored urine consistent with myoglobinuria. On one such occasion, after playing football, he required admission to hospital for intravenous fluids because CK level was found to be significantly elevated at 75,000 IU/L (normal <250 IU/L). Neurological examination revealed mild left-sided scapular winging but no other abnormalities. BMI was 25.8 kg/m2 and he was able to walk 1,000 m during a 12-min walk test (12MWT) without evidence of a “second-wind” phenomenon.
Investigations revealed a normal serum CK at rest (113 IU/l, normal range 38–204 IU/l), serum carnitine and acylcarnitines, white cell α-glucosidase activity and co-enzyme Q10, serum amino acid profile and urinary organic acids levels. A forearm exercise test showed a very mild rise in lactate despite a normal rise in ammonia (Fig. 1). In vitro analysis using cultured skin fibroblasts showed normal fatty acid oxidation flux studies and normal CPT2 enzyme activity.
Cardiac evaluation, including electrocardiogram and echocardiography, was normal as well as neurophysiological assessment which included EMG and nerve conduction studies. Muscle MRI revealed fatty infiltration of the posterior calf muscles bilaterally, especially the soleus.
Muscle biopsy
Both patients underwent a muscle biopsy of vastus lateralis, after giving informed consent. Morphological studies showed no evidence of vacuoles on haematoxylin and eosin and Gomori-trichrome stained sections or cores with oxidative stains. Glycogen, lipid and mitochondrial staining, with periodic acid-Schiff (PAS) (Fig. 2), Sudan Black and sequential cytochrome oxidase and succinate dehydrogenase stains, respectively, were unremarkable.
Acid phosphatase staining and glycolytic histochemical stains for phosphorylase and phosphofructokinase were normal. Routine immunohistochemistry for the dystrophin panel of staining was normal. Electron microscopy analysis revealed a mild increase in muscle glycogen.
Biochemical studies on muscle homogenate revealed normal CPT 2, AMPD and respiratory chain enzymes activities. Muscle glycolytic enzymes activities as phosphorylase b kinase, phosphorylase, phosphofructokinase and phosphoglycerate mutase, phosphoglycerate kinase, phosphoglucomutase were also normal but β-enolase activity was markedly reduced, respectively, in case 1, to 0.15 nmol/min/mg protein (20 % residual activity) and, in case 2, to 0.06 (10 % r.a.) (n.v. 0.66 ± 0.1 nmol/min/mg prot).
Molecular genetic analysis
Direct sequence analysis of ENO3 gene revealed: in case 1, a missense homozygous mutation, c. 452 A>G transition in exon 7, changing an asparagine residue to serine at position 151 (p.Asn151Ser); in case 2, a homozygous variant c.559G>A, also located in exon 7 and affecting a highly conserved amino acid, changing a glutamic acid residue to lysine (p.Glu187Lys) (Fig. 3).
Genetic analysis of ENO3 gene: electropherograms of case 1 (a) and 2 (b) showing, respectively, the c.452 A>G mutation in exon 7 of ENO 3 gene that determines an amino acid substitution Asn to Ser at codon 151 (p. N151S) and the homozygous variant c.559G>A, located also in exon 7, changing a glutamic residue to a lysine at codon 187 (p.E187K). c Phylogenetic conservation of N151S and E187K amino acid residues in the β-enolase, showing that both residues were very well conserved through different species
Genetic analysis of the Italian family revealed that the mother (I:2) of the proband (II:4), one (II:3) of three asymptomatic brothers and his daughter (III:1) harbored the same mutation in heterozygous state (Fig. 4a). In case 2, the asymptomatic paternal uncle, the father (I:1) and the sister (II:2) carried the mutation in the heterozygous state whereas the proband’s mother was deceased and could not be tested (Fig. 4b).
Further genetic investigations were undertaken, but no mutations were found in RYR1, LPIN1, PYGM or PGAM2.
Discussion
Recurrent rhabdomyolysis is a condition that can occur in several acquired or inherited muscle disorders that can occasionally be life threatening because of severe renal complications [4].
Among the inherited metabolic myopathies, the most common cause of rhabdomyolysis is considered CPT2 deficiency [5], but it is also a frequent manifestation of some muscle glycogenoses as GSDV (McArdle disease) [6], GSD X [7] and GSD VII (Tarui disease) [8, 9].
We describe, herein, two new cases presenting with recurrent episodes of rhabdomyolysis as main clinical manifestation where biochemical workup on skeletal muscle revealed a primary deficiency of β-enolase (20 and 10 % of residual activity, respectively), thus confirming the diagnosis of a very rare defect of distal glycolysis.
This metabolic myopathy was firstly described in 2001 by Comi et al. [3], who reported a 47-year-old man with adult onset exercise intolerance, myalgia and mild hyperCKemia; the patient never complained of pigmenturia and he was able to work as a bus driver without any problem.
These two new cases are very similar to one another and both are more severely affected than the first reported case who presented with a milder phenotype.
All three β-enolase deficient patients showed a skeletal muscle involvement with no fixed muscle weakness and without evidence of any other organ involvement. In all three patients, there was a very mild rise of lactate during the forearm ischemic test.
Morphological studies were quite similar in all three cases: muscle biopsy showed only minimal changes, but the ultrastructural studies evidenced a mild glycogen accumulation. Muscle MRI did not show any specific diagnostic pattern in either case.
Despite our two patients presenting with a more severe phenotype, biochemical results showed a higher β-enolase residual activity (20 and 10 %, respectively) compared to 5 % of the first case. This could potentially relate to the lifestyles of the patients with the two herein described being more physically active than the first patient.
ENO3 genetic analysis correlated with the clinical and biochemical data in these two patients and identified novel homozygous missense mutations located in exon 7 as well as one of the two mutations reported in the previous case [10]. The mutations change highly conserved amino acid residues and are located in the catalytic site of the protein (Fig. 1c), close to residues 152, 159, 155 and 168 that contribute to the stabilization of the transition state of the protein [11, 12]. Both mutations segregate as expected in the two families; asymptomatic members tested were not homozygous for the mutation.
Although β-enolase deficiency is a rare autosomal recessive condition, its true incidence is likely to have been so far underestimated. Its symptoms could be either mild, as in the first reported case, or more severe with clinical features similar to other metabolic myopathies (i.e., rhabdomyolysis in these two cases). Our cases highlight that, in presence of recurrent episodes of dark urine, associated with hyperCKemia and myoglobinuria and often related to physical exercise, physicians should be aware of the possibility of β-enolase deficiency.
Nowadays, the access to new techniques for genetic testing (exome sequencing, specific gene panels) of patients with undiagnosed rhabdomyolysis could provide stronger tools to make easier the diagnostic approach to these rare disorders.
Following this consideration, it could be suggested that a panel containing all the genes specifically involved in the diagnosis of suspected metabolic myopathies related to the glycogen/glycogenolytic or lipid metabolism should be currently performed.
In conclusion, although, so far, only three cases of β-enolase deficiency have been reported, it is noticeable that these two new cases manifested with a very severe phenotype and with homozygous ENO3 mutations. Further cases may help to better define the full clinical spectrum of this disorder.
References
Kang HJ, Jung SK, Kim SJ, Chung SJ (2008) Structure of human alpha-enolase (hENO1), a multifunctional glycolytic enzyme. Acta Crystallogr D Biol Crystallogr 64(Pt 6):651–657
Chen S-H, Giblett ER (1976) Enolase: human tissue distribution and evidence for three different loci. Ann Hum Genet 39:277–280
Comi GP, Fortunato F, Lucchiari S et al (2001) Beta-enolase deficiency, a new metabolic myopathy of distal glycolysis. Ann Neurol 50:202–207
Oldfors A, DiMauro S (2013) New insights in the field of muscle glycogenoses. Curr Opin Neurol. 26:544–553
Gazzerro E, Andreu AL, Bruno C (2013) Neuromuscular disorders of glycogen metabolism. Curr Neurol Neurosci Rep 13(3):333
Quinlivan R, Buckley J, James M et al (2010) McArdle disease: a clinical review. J Neurol Neurosurg Psychiatry 81(11):1182–1188
Naini A, Toscano A, Musumeci O, Vissing J, Akman HO, DiMauro S (2009) Muscle phosphoglycerate mutase deficiency revisited. Arch Neurol 66(3):394–398
Musumeci O, Aguennouz M, Comi GP et al (2007) Identification of the infant-type R631C mutation in patients with the benign muscular form of CPT2 deficiency. Neuromuscul Disord 17(11–12):960–963
Musumeci O, Bruno C, Mongini T et al (2012) Clinical features and new molecular findings in muscle phosphofructokinase deficiency (GSD type VII). Neuromuscul Disord 22(4):325–330
Feo S, Oliva D, Barbieri G, Xu W, Fried M, Giallongo A (1990) The gene for the muscle-specific enolase is on the short arm of human chromosome 17. Genomics 6:192–194
Peshavaria M, Day INM (1991) Molecular structure of the human muscle-specific enolase gene (ENO3). Biochem J 275:427–433
Zhao S, Choy BS, Kornblatt MJ (2008) Effects of the G376E and G157D mutations on the stability of yeast enolase—a model for human muscle enolase deficiency. FEBS 275:97–106
Acknowledgments
This study was supported by EUROMAC Project No. 20121214 funded by European Commission and NHS England for Highly Specialised Services. We would also like to acknowledge the Association for Glycogen Storage Disorders [AGSD (UK)].
Conflicts of interest
All authors declare that they have no conflict of interest.
Ethical standard
The subjects reported in the study gave their informed consent to the clinical procedures performed during the diagnostic workup.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Musumeci, O., Brady, S., Rodolico, C. et al. Recurrent rhabdomyolysis due to muscle β-enolase deficiency: very rare or underestimated?. J Neurol 261, 2424–2428 (2014). https://doi.org/10.1007/s00415-014-7512-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7512-7