Abstract
Schizophrenia is a severe neuropsychiatric disease that is associated with neurobiological alterations in multiple brain regions and peripheral organs. Negative symptoms and cognitive deficits are present in about half of patients and are difficult to treat, leading to an unfavorable functional outcome. To investigate the impact of aerobic exercise on various neurobiological parameters, we conducted a narrative review. Add-on aerobic exercise was shown to be effective in improving negative and general symptoms, cognition, global functioning, and quality of life in schizophrenia patients. Based on findings in healthy individuals and animal models, this qualitative review gives an overview of different lines of evidence on how aerobic exercise impacts brain structure and function and molecular mechanisms in patients with schizophrenia and how its effects could be related to clinical and functional outcomes. Structural magnetic resonance imaging studies showed a volume increase in the hippocampus and cortical regions in schizophrenia patients and healthy controls after endurance training. However, results are inconsistent and individual risk factors may influence neuroplastic processes. Animal studies indicate that alterations in epigenetic mechanisms and synaptic plasticity are possible underlying mechanisms, but that differentiation of glial cells, angiogenesis, and possibly neurogenesis may also be involved. Clinical and animal studies also revealed effects of aerobic exercise on the hypothalamus–pituitary–adrenal axis, growth factors, and immune-related mechanisms. Some findings indicate effects on neurotransmitters and the endocannabinoid system. Further research is required to clarify how individual risk factors in schizophrenia patients mediate or moderate the neurobiological effects of exercise on brain and cognition. Altogether, aerobic exercise is a promising candidate in the search for pathophysiology-based add-on interventions in schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
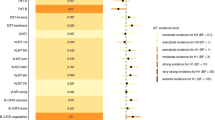
Schizophrenia is one of the most debilitating psychiatric disorders. Although antipsychotic medication is effective in reducing positive symptoms in schizophrenia patients, it is less successful in treating negative symptoms [1] and cognitive deficits [2]. These symptoms, however, cause the most long-term disability and disease-associated burden [3]. Thus, novel treatment strategies that promote functional recovery by decreasing negative symptoms and cognitive deficits are warranted. Studies have suggested that aerobic exercise as an add-on therapy may meet this need [4, 5]. Aerobic exercise was shown to be superior to various control conditions in improving positive, negative, and general symptom severity, global and social functioning, need of care, and quality of life in schizophrenia patients [3, 6,7,8] (Fig. 1). Furthermore, it was found to significantly ameliorate cognitive deficits in schizophrenia, with specific effects on working memory, attentional processes, and social cognition [9]. It was also shown to be effective in promoting physical health and reducing the risk of patients with schizophrenia to develop a somatic comorbid disorder [10,11,12]; this is of particular importance, because people with schizophrenia consistently have higher morbidity and mortality than the general population. The life expectancy of people with schizophrenia is shortened by 10–20 years [4, 13], because they have a higher risk than the general population for cardiovascular disease [14], metabolic syndrome [15], diabetes [16], and respiratory diseases [17]. Unhealthy lifestyle habits, such as heavy smoking [18], poor diet [19], and low levels of physical activity [20], are likely to play important roles in the development of these conditions. Finally, certain antipsychotics and the symptoms of the disease itself often lead to weight gain and metabolic syndrome [21].
Impairments in neuroplasticity, inhibitory functioning, and connectivity that result in failed neuroregeneration have been discussed as the underlying causes of negative symptoms and cognitive deficits in patients with schizophrenia [22]. Aerobic exercise has been suggested as a promising intervention to target these deficits by modulating neuroplasticity. However, there is still some ambiguity regarding the underlying neurobiological mechanisms of exercise in schizophrenia patients. Unfortunately, this current lack of understanding has hampered the design of efficient exercise programs intended to have the greatest possible benefits in schizophrenia.
Based on findings in healthy individuals and animal models, this narrative review aims to give an overview of different lines of evidence on how exercise impacts brain structure and function and molecular mechanisms in patients with schizophrenia (Fig. 2) and how these effects could be related to the clinical and functional outcomes of this severe disorder.

Legends: Firth et al. [33], Weinstein et al. [35], Svatkova et al. [51], Brockett et al. [68], Voisin et al. [85], van Praag [26], Pereira et al. [77], Szuhany et al. [110], Meeusen and De Meirleir [144], Tantimonaco et al. [177], Stranahan et al. [183], Gomes da Silva et al. [200]
Postulated neurobiological effects of aerobic exercise in schizophrenia patients.
Thereby, we covered several research areas, ranging from structural findings to the effects on cellular level and molecular mechanisms. The literature was not systematically searched, extracted, and synthesized. However, for every of the following topics, a focused literature search based on the PubMed database has been conducted. So far, research has focused on aerobic formats of exercise, which seem to be most promising. On the basis of previous recommendations for schizophrenia patients [23, 24], we will concentrate on the effects of long-term aerobic training.
Structural plasticity
Structural magnetic resonance imaging (sMRI) findings, with a focus on gray matter
The hippocampus plays a vital role in declarative learning and memory formation. Notably, several psychiatric and neurological disorders, including schizophrenia, have been associated with hippocampal dysfunction. This may be because some symptoms are common to these disorders, such as aspects of cognitive impairment [25]. At the same time, the hippocampus has been identified as a brain region that is sensitive to the effects of physical activity, an aspect that has been extensively studied in rodents [26, 27]. In particular, aerobic training seems to promote hippocampal volume and function, as specified below.
An increase in hippocampal volume in response to aerobic exercise has been consistently observed in animal models [28, 29], and a number of human studies have also found that aerobic exercise can lead to improvements in learning and memory performance and that these improvements are associated with increased hippocampal volume. For example, Erickson et al. [30] showed that a correlation between fitness and short-term memory in a large sample of healthy elderly adults was mediated by increases in hippocampal volume. Similar results were found in another study in healthy adults, which showed increases in bilateral hippocampal volume after 10 weeks of an aerobic exercise intervention program [31]. However, despite these and other promising findings [32, 33], overall evidence from studies on the effects of aerobic exercise on hippocampal volume in humans is less robust. Firth et al. recently undertook a meta-analysis of controlled trials on this topic. Across 14 eligible controlled trials in a total of 737 participants, they found no significant effect of aerobic exercise on total hippocampal volume (g = 0.120, 95% CI 0.02–0.26, p = 0.082). However, compared with control conditions, aerobic exercise had positive effects on left hippocampal volume in terms of a volume increase. As post hoc analyses revealed, these findings were driven through aerobic exercise preventing the physiological volumetric decrease in comparison to control conditions [33]. Studies in older adults in particular have shown that exercise interventions can counteract age-related brain atrophy [34]. This effect might mediate the association between aerobic fitness and executive function [35]. Moreover, higher physical fitness levels have been associated not only with larger hippocampi [36] but also with larger cortical areas, especially frontal regions [35, 37, 38]. Again, systematic research on this issue is lacking.
Four of the studies in the meta-analysis by Firth et al. [33] investigated the impact of exercise on hippocampal volume in patients with schizophrenia. When analyzing these studies in a total of 107 people with schizophrenia or first-episode psychosis, the authors detected no significant increase in the total, right, or left hippocampal volume compared with control conditions (g = 0.149, 95% CI − 0.31 to 0.60, p = 0.53) [33]. However, because of the relatively small sample sizes across the studies, which did not allow for further subgroup analysis, they were unable to rule out possible benefits of aerobic exercise on hippocampal volume in schizophrenia on the basis of the null findings [33]. In patients with schizophrenia, individual risk factors may contribute to conflicting results [39, 40]. Indeed, schizophrenia polygenetic risk scores have been shown to significantly influence the exercise-mediated volume increase of specific subregions of the hippocampus [41].
Effects on white matter
Although most of the current literature focuses on assessing gray matter changes, some papers also report on the impact of aerobic exercise on white matter integrity [25]. White matter tracts interconnect distant cortical regions and are required to allow complex information processing in large-scale networks [42, 43]. In cross-sectional studies, both aerobic fitness and endurance exercise have been shown to affect white matter tracts in healthy individuals [32, 44]. In a study by Burdette et al., older adults at risk for cognitive decline (because they were aged 70–85 years and had self-reported memory loss) participated in an exercise intervention (150 min/week of aerobic training), cognitive training, a combined treatment of exercise and cognitive training, or a healthy aging educational control group. After 4 months of the intervention, MRI measures of resting brain blood flow and connectivity were performed. The authors showed that physical exercise was associated with increased connectivity between prefrontal, cingulate, and hippocampal areas, which resulted in better performance on several cognitive tasks [45].
A recent meta-analysis assessed the effects of aerobic exercise on white matter volume, lesions, and microstructure in older healthy adults. The authors concluded that, across all 29 eligible studies, physical activity correlated with greater white matter volume, resulting in small but significant effect sizes [46].
Abnormalities in white matter integrity have been reported in patients with schizophrenia, particularly in frontal and temporal cortices, by studies using diffusion tensor imaging (DTI), a method that assesses the diffusion properties of water molecules to infer microstructural white matter changes [47, 48]. Other studies have shown an abnormal myelination of the tracts responsible for communication between these regions [49, 50]. Svatkova et al. [51] conducted a longitudinal intervention study in 33 patients with schizophrenia and 48 healthy controls. The participants were randomly assigned to either 6 months of training (1 h training session, consisting of 40 min of aerobic and 20 min of anaerobic exercise, twice weekly) or a life-as-usual condition. Using DTI, the researchers showed that the training led to an increased integrity in particular of white matter fiber tracts related to motor functioning, such as the corpus callosum, corticospinal tract, and superior longitudinal fascicle, whereas life-as-usual led to a decreased fiber integrity. Remarkably, this benefit was seen in both the patients with schizophrenia and the healthy controls [51].
In summary, these studies demonstrate that aerobic exercise is able to induce structural adaptations in motor function-related brain regions and associated fiber connections. Furthermore, the beneficial effects of exercise with respect to cerebrovascular health play an important role in white matter integrity. These benefits include the preservation of arterial elasticity and wall integrity and a reduction in arterial stiffness and blood pressure [46].
Functional imaging findings
In addition to brain imaging with MRI, electrophysiological techniques, including electroencephalography (EEG), functional magnetic resonance imaging (fMRI), functional near-infrared spectroscopy (fNIRS), and transcranial magnetic stimulation (TMS), may also be helpful in providing insight into the effects of aerobic exercise on brain activity and functioning [52]. For example, in healthy older adults, changes in task-related brain activation and functional connectivity through long-term exercise were demonstrated with fMRI [53, 54]. In addition, aerobic training was shown to increase functional connectivity between the frontal, posterior, and temporal cortices in both the default mode network (DMN) and the frontal executive control networks [55]. Compared with sedentary individuals, healthy, active individuals showed differences in motor cortical excitability, as assessed by motor cortex TMS, and motor cortical plasticity via paired-associative stimulation could only be induced in physically active people [56]. Older studies indicate changes in EEG amplitude and visual-evoked potentials (VEPs) after marathon running [57, 58]. One recently published study showed that 3 months of aerobic endurance training (30 min, 3 times/week) on bicycle ergometers increased motor cortical inhibition, assessed by TMS, in both healthy controls and schizophrenia patients, with no significant group differences [59].
Neurogenesis
Neurogenesis refers to the process of generating new neurons from precursor cells. Evidence from genetic studies, animal models, and imaging studies suggests that aberrant neurogenesis may contribute to the pathogenesis, pathophysiology, and symptoms of schizophrenia [60].
Improvements in spatial learning and memory after chronic aerobic exercise have been associated with physiological and structural neuronal changes, including neurogenesis [26, 61]. In rodents, studies demonstrated that aerobic exercise promotes neurogenesis in the dentate gyrus subregion of the hippocampus [26, 27]. Moreover, in humans, regular aerobic exercise has been shown to increase cell density and shape in a number of hippocampal regions [62, 63]. These changes in brain cell composition after exercise have been shown to relate to greater volumes of subregions of the hippocampus and to the total size of the hippocampus seen with structural MRI in rodents [64,65,66].
Until recently, the adult human hippocampus was considered to be able to continue generating new neurons up to adulthood, and aerobic exercise was thought to be a possible way to enhance neurogenesis [67]. However, evidence from human studies on hippocampal volume increase in response to aerobic exercise is less robust than that from animal studies [32, 33]. Findings regarding neurogenesis as the underlying mechanism are also equivocal in humans. Whereas some studies have suggested that new neurons are added to the adult dentate gyrus every day, others have found many fewer putative new neurons [67]. To get to the bottom of the contradictory data, Sorrells et al. examined surgical resection samples from patients with epilepsy and postmortem samples from controls and detected no young neurons in the dentate gyrus [67]. In the monkey hippocampus, they found proliferation of neurons in the subgranular zone in early postnatal life, but decreased neurogenesis during juvenile development. The group concluded that even though a recruitment of young neurons to the primate hippocampus occurs during the first years of life, neurogenesis in the dentate gyrus does not continue, or is extremely rare, in adult humans. Their findings raise important questions about how the function of the dentate gyrus differs between humans and species in which adult hippocampal neurogenesis is preserved, such as rodents. It follows that even though exercise-induced neurogenesis could be shown in animals, it probably does not occur in humans.
Gliogenesis
In rodents, studies examined whether exercise could alter the structure and function of astrocytes. Astrocytes form the majority of glial cells in the human central nervous system (CNS) and play an important role in the regulation of blood flow and trophic support, both functions that have numerous implications for neuronal functioning and synaptic growth [68]. Moreover, astrocytes modulate glutamate metabolism and transmission. Abnormality in these processes is highly correlated with schizophrenia phenotypes [69].
Using immunolabeling for astrocyte and synaptic markers in rodents, two studies observed an increase in astrocyte cell body size in the hippocampus, medial prefrontal cortex, and orbitofrontal cortex in response to running compared with the sedentary control condition [68, 70]. The authors concluded that aerobic exercise alters astrocyte morphology and leads to specific changes in astrocyte markers.
Animal models have also provided some evidence to suggest an association between exercise and the proliferation of oligodendrocyte progenitor cells. Throughout adulthood, oligodendrocyte progenitor cells continue to differentiate into mature oligodendrocytes, a process that is essential for continued myelination. For example, running was shown to increase the number of immature and mature oligodendrocytes in the spinal cord of the mouse [71] and to increase differentiation of oligodendrocyte precursors after hypoperfusion of the brain [72]. These results suggest the existence of complex interactions between environmental factors, oligodendrocyte lineage development, and brain function [73].
The effects of aerobic exercise on glia proliferation and differentiation in schizophrenia patients or healthy controls are widely unknown. Positive findings, for example from DTI studies, as mentioned above, could reinforce the relevance of physical exercise as a strategy for the regeneration of white matter tracts.
Angiogenesis
Angiogenesis is broadly defined as the formation of new blood vessels from the existing vasculature and is regulated by angiogenic growth factors, among others [74]. The maintenance of adequate cerebral blood flow is essential for a constant supply of oxygen and nutrients, which, in turn, is essential for the energy-requiring processes memory formation and consolidation [43]. Morphological, genetic, neuroimaging, and postmortem gene expression studies implicate cerebral microvasculature and changes in angiogenesis as a potential contributor to the pathophysiology of schizophrenia [74].
However, studies have shown that, in healthy older adults, greater aerobic capacity, achieved through regular physical activity, leads to higher cerebral blood flow and that dementia is associated with a reduced cerebral blood flow [75, 76]. A 3-month aerobic exercise intervention by Pereira et al. in healthy middle-aged participants resulted in an increased cerebral blood volume in the dentate gyrus region of the hippocampus, which correlated with improved learning and better memory performance [77], indicating that the vascular adaptations might contribute to subsequent neuroplasticity [78]. In schizophrenia patients, angiogenesis as a result of aerobic exercise still requires further investigation.
The literature on both animal and, to a limited extent, human studies suggests that gliogenesis, vascular adaptations, and possibly neurogenesis represent the primary mechanisms on the cellular level, and that all three are promoted by exercise. These adaptations are followed in turn by changes in molecular pathways, which will be further considered below.
Epigenetic alterations
Epigenomic profiling means linking genotype to differential gene expression [79]. A major epigenetic mechanism is methylation of cytosine bases within the genome. If this methylation occurs within the promoter region of genes, it results in repression of transcription, thus enabling transcriptional control [80]. Histone modification of chromatin is another epigenetic mechanism that influences gene expression [81]. Altered DNA methylation and histone post-translational modifications have been detected in the brain and blood cells of patients with schizophrenia [82,83,84]. In addition, micro-RNAs (miRNAs) that regulate the transcriptome, such as miR137, have been shown to be differentially expressed in brain regions of schizophrenia patients [82, 83]. Because environmental factors play a major role in epigenetic regulation [82], studies have investigated the respective effects of aerobic exercise. A review of 25 studies on the effect of physical activity on DNA methylation in humans concluded that long-term exercise can change methylation in a highly tissue- and gene-specific manner [85]. Studies that examined these mechanisms in rodents showed that exercise regulates DNA methylation and histone acetylation in the hippocampus [86]. Interestingly, animal studies even showed an influence of paternal exercise on the offspring’s hippocampal DNA methylation compared with the offspring of sedentary fathers [87, 88]. These findings indicate that exercise-induced epigenetic mechanisms have trans-generational effects.
Exercise enhances the activity of histone acetyltransferases and histone deacetylases, both of which play an important role in the regulation of histone acetylation and modulate gene transcription [89]. These mechanisms may contribute to the transcriptional regulation underlying the improvements in cognitive function seen in rodents after long-term aerobic exercise [89]. Moreover, in animals, BDNF expression was shown to be enhanced through epigenetic mechanisms [86].
In addition, aerobic exercise is able to modulate the expression of memory-related miRNAs [86]. There are multiple interactions between miRNAs and epigenetic factors. On one hand, in many cell types, the expression of some miRNAs is silenced by DNA methylation and modulated by histone modifications. On the other hand, miRNAs can directly target epigenetic factors, such as DNA methyltransferases and histone deacetylases, which lead to adaptations in chromatin structure [90]. Exercise-induced memory improvements were shown to be accompanied by changes in the hippocampal miRNA-mRNA regulatory network in animals [91,92,93]. A comparison of endurance athletes and healthy controls found linear correlations between miRNA and both resting heart rate and maximum oxygen uptake [94]. The authors concluded that muscle-enriched miRNAs are regulated by aerobic exercise training and can serve as biomarkers of cardiorespiratory fitness [94]. However, there is a need for more research exploring epigenetic effects in human populations and patients with schizophrenia.
Synaptic plasticity
After being exposed to internal and external influences, the brain is able to respond on the synaptic level. A study in rodents showed that hippocampal dendritic length and dendritic spine complexity can be enhanced through exercise [63]. Kohman et al. [95] conducted a study with a microarray on whole hippocampal samples from adult and aged mice that were housed with or without a running wheel. The results showed that running increased the expression of genes related to cell growth, and attenuated the expression of genes involved in immune function and chromatin remodeling. A study with a similar design demonstrated an upregulation of genes involved with synaptic trafficking (synapsin I, synaptotagmin, and syntaxin), signal transduction pathways (Ca2+/calmodulin-dependent protein kinase II, CaM-KII, mitogen-activated/extracellular signal-regulated protein kinase, MAP-K/ERK I and II, protein kinase C, and PKC-delta) and transcription regulators (cAMP response element-binding protein, and CREB) [96].
Exercise can also promote synaptic plasticity by facilitating long-term potentiation (LTP), as shown in animals [97,98,99]. LTP refers to the strengthening of synaptic connections between neurons and is considered as a cellular model of learning and memory [100]. In young rodents, aerobic exercise was able to stimulate LTP and reverse the age-related decline of LTP compared with sedentary controls [32]. Alongside morphological changes to the neural cells and their vasculature, these mechanisms may contribute to ameliorating learning and memory impairments. Their significance in patients with schizophrenia needs to be further investigated in future studies.
Growth factors
The upregulation of various neurotrophic factors is assumed to be one of the underlying mechanisms mediating neuroplasticity through physical activity [76]. It is well documented that neurotrophic factors can facilitate the maturation, proliferation, and survival of neurons [38, 101].
BDNF
Brain-derived neurotrophic factor (BDNF) not only has an integral role in supporting neuronal survival and growth, but also improves functional connectivity by increasing synaptogenesis and dendritic spine density [100]. It is widely distributed throughout the CNS and can be found in particularly high concentrations in the hippocampus, neocortex, cerebellum, striatum, and amygdala [101]. BDNF unfolds its effects on neurogenesis and synaptic transmission by binding to one of its receptors, high-affinity tropomyosin-related kinase-B (Trk-B). Binding to Trk-B results in receptor dimerization and trans-autophosphorylation of tyrosine residues in the cytoplasmic domains of the receptor, which in turn initiates a number of intracellular signaling cascades [38]. In models of normal aging and neurodegenerative conditions, treating cultured hippocampal or cortical neurons with exogenous BDNF protects them against dysfunction and degeneration [102, 103]. Moreover, BDNF has been shown to be essential for the maintenance of synaptic plasticity [102]. After applying BDNF to organotypic hippocampal slices in culture, a higher density of dendritic spines and synapses can be observed and the expression of synaptic proteins such as synaptophysin, synaptobrevin, and synaptotagmin rises [104].
The strongest evidence for acute exercise-induced increases of BDNF in the brain is derived from rodent studies [38, 105]. Using BDNF-mutant mice, Korte and colleagues first demonstrated that BDNF has a functional role in memory formation [106]. In the same year, it was reported that rats showed increased BDNF gene expression in the hippocampus and certain layers of the caudal neocortex after 7 days of wheel running [107], providing the first evidence that growth factors may be responsible for the beneficial effects of exercise on the brain [43]. Blocking BDNF receptors, however, abolished the downstream effects of exercise on cognitive performance and memory [100]. This defect was rescued with BDNF replacement, either by injecting the BDNF-expressing adenovirus [108] or by supplying exogenous BDNF [109].
In humans, immediately preceding exercise has also been shown to increase peripheral BDNF levels significantly. A meta-analysis by Szuhany and colleagues revealed that, after regular aerobic training, healthy individuals showed a higher increase in peripheral BDNF after immediately preceding physical activity (g = 0.59) than previously sedentary individuals showed after only a single session of exercise (g = 0.46) [110]. Regarding resting BDNF levels after a program of regular exercise, Szuhany et al. found a low but significant effect size of g = 0.27. Moreover, exercise-induced expression of BDNF seems to be age-dependent and less pronounced in older individuals [111] and women [110].
In patients with schizophrenia, serum BDNF levels were shown to be significantly lower than in healthy controls [112, 113], and were associated with cognitive impairment [114]. Several studies have examined the link between aerobic exercise and BDNF in schizophrenia patients. Peripheral BDNF was shown to increase after aerobic exercise compared with an inactive control group consisting of either patients with schizophrenia receiving treatment as usual [115,116,117,118] or healthy controls [119]. Moreover, after aerobic exercise, positive correlations were demonstrated between BDNF and cognitive enhancements [120], providing an important clinical link to enhanced neuroplasticity.
Although there are several growth factors that may play a role in the chronic effects of exercise, besides BDNF insulin-like growth factor (IGF-1) and vascular endothelial growth factor (VEGF) have received the most interest. BDNF interacts with both IGF-1 and VEGF, both of which stimulate the growth of endothelial cells, which express nitric oxide synthase. Nitric oxide synthase in turn is required for exercise-induced upregulation of BDNF in the hippocampus [38, 121].
IGF-1
Studies comparing trained and sedentary individuals demonstrated that IGF-1 levels are significantly higher in trained individuals [32]. In addition, both animal and human studies revealed that exercise is associated with an increased peripheral level of IGF-1 [122]. Circulating IGF-1 crosses the blood–brain barrier [123], enhances synaptic plasticity and neuronal survival, and increases concentrations of BDNF [124]. IGF-1 replacement was shown to enhance learning and memory in rats [125].
Compared with healthy controls, schizophrenia patients exhibit reduced levels not only of BDNF but also of IGF-1 [126, 127]. To the best of our knowledge, so far, only one study has assessed changes in peripheral IGF-1 levels in schizophrenia patients after aerobic exercise: Andrade et al. found no differences in peripheral IGF-1 levels induced by 20 weeks of aerobic exercise [128].
VEGF
VEGF is produced by skeletal muscle cells and secreted into the circulation. Acute exercise increases VEGF mRNA in skeletal muscle, whereas VEGF protein itself is reduced immediately after acute exercise [129]. However, chronic exercise is able to restore and even increase skeletal muscle VEGF mRNA and protein levels [130]. Even though VEGF does not readily cross the blood–brain barrier, in animals, increased levels were shown in the hippocampus after exercise [131].
Regarding patients with schizophrenia, a meta-analysis by Misiak and colleagues in 15 eligible studies revealed no significant differences in VEGF levels between patients and controls [132]. However, heterogeneity across the studies was significant in the majority of the analyses [132]. Insufficient data were available on exercise-induced changes in VEGF levels in patients with schizophrenia.
Other growth factors that represent potential targets for future investigations, because they have been shown to change with exercise, include nerve growth factor (NGF) [96], neurotrophin-3 (NT-3), neurotrophin-4 (NT-4), fibroblast growth factor type 2 [133], VGF growth factor [134], and galanin [48, 135, 136].
Neurotransmitter systems
Because of technical challenges, only a few studies have examined the effects of exercise on the neurotransmitter systems in the brain of awake humans. Instead, most studies have been conducted in rodents, using techniques such as in vivo microdialysis or high-performance liquid chromatography (HPLC) analysis of postmortem brain tissue [137, 138]. These studies have shown that aerobic exercise influences several neurotransmitter systems in the brain, such as serotonin (5-hydroxytryptamine, 5-HT), dopamine, acetylcholine, and norepinephrine. We will discuss these effects below to indicate future research areas that may identify possible beneficial effects of aerobic exercise on neurotransmitters in schizophrenia patients.
Serotonin
The monoamine neurotransmitter serotonin (5-HT) is known to play an important role in the process of learning and memory in the hippocampus [139]. However, its transmission in the hippocampus is disrupted in schizophrenia [25, 140], which likely contributes to the deficits in memory often associated with the disorder [65, 141, 142].
Animal studies have shown that chronic exercise increases 5-HT concentrations in the brain, particularly in the striatum, hippocampus, hypothalamus, and frontal cortex [143, 144]. Physical activity is presumed to increase the relative proportion of free tryptophan peripherally as the underlying mechanism for the increases in 5-HT concentrations: During exercise, free fatty acids displace tryptophan from binding with albumin, and the unbound tryptophan is able to cross the blood–brain barrier and form 5-HT [145]. Moreover, an exercise-induced modulation of enzymes results in an altered metabolism of 5-HT [146]. The extent to which these mechanisms occur in patients with schizophrenia and how they contribute to neuroplasticity and reduced negative symptoms has not yet been examined.
Norepinephrine
The effect of exercise on brain concentrations of norepinephrine has also been evaluated in animal studies. Meeusen et al. reported that chronic exercise leads to an increase in the concentration of norepinephrine in the whole brain [144]. Moreover, a study in mice showed that exercise-induced reductions in depression-like behavior were correlated with an increase in hippocampal norepinephrine [147]. Although norepinephrine is involved in a variety of cognitive processes [148], changes in cognitive functioning related to exercise-induced effects on norepinephrine have not yet been well evaluated in healthy humans or patients with schizophrenia [52].
Dopamine
Optimal dopamine levels are important, because dopamine plays a key role in motivation [149] and mood, and is involved in the pathogenesis of schizophrenia [150]. Repeated exercise leads to adaptations in the dopaminergic system through several mechanisms, as has been shown in animals. These mechanisms include modulation of dopaminergic turnover [151] and optimization of enzyme functions, such as tyrosine hydroxylase activity [152], and calcium levels [153, 154]. Peripheral catecholamines do not cross the blood–brain barrier. However, aerobic exercise leads to increased levels of serum calcium, which is transported to the brain via the calcium–calmodulin system. This, in turn, enhances the brain dopamine synthesis through a calmodulin-dependent system [155]. An increase in dopamine concentrations after aerobic exercise is region-specific. Whereas dopamine levels were higher in the hypothalamus and midbrain after aerobic exercise training, they were lower in the prefrontal cortex, hippocampus, and striatum [137, 144]. However, research regarding adaptations in the dopaminergic system through aerobic exercise in schizophrenia patients is still lacking.
Glutamate
Glutamate plays a central role in synaptic plasticity [156], and alterations in the glutamate system, such as a hypofunction of the N-methyl-D-aspartate receptor, have been linked to the pathogenesis of schizophrenia [157, 158]. Aerobic exercise is able to enhance glutamate turnover [159] by improving calcium regulation [160] and, as has been demonstrated in animals [161], leads to increased glutamate levels in the anterior cingulate cortex. Exercise upregulates glutamatergic-related genes [96, 162] and increases both the expression of NR2A and NR2B glutamatergic receptors [163] and mRNA and protein expressions of NMDA receptors [164] in the hippocampus; these effects are associated with neurogenesis and synaptic plasticity [154, 163]. In healthy humans, a proton magnetic resonance spectroscopy (H-MRS) study visualized changes in glutamate in the primary visual cortex and the anterior cingulate cortex after exercise: aerobic exercise increased glutamate in both cortical areas, leading to higher resting states after 1 week [161]. Nevertheless, future studies are needed to investigate the relationship between exercise-induced changes in the glutamate system and cognition in schizophrenia patients.
Acetylcholine
The nicotinergic acetylcholine (nAch) receptors α7 and α4β2 have been reported in postmortem studies to be lower in the prefrontal cortex and hippocampus in patients with schizophrenia than in healthy controls and to be related to cognitive deficits [165, 166]. Decreased receptor function is related to cognitive deficits, especially learning and memory. Agonists of the nAch receptor α improve cognition and may be effective in the treatment of schizophrenia [167]. In an animal model of schizophrenia, the DISC1 transgenic mouse, voluntary exercise improved hippocampus-dependent spatial memory and social recognition [168]. In exercising rats, 24 h after spatial memory testing, an upregulation of muscarinic receptor density and an increase in high-affinity choline uptake were found, concomitant with a reduction in hippocampal high-affinity choline uptake [169]. Moreover, the animals demonstrated an enhanced depolarization-induced activation of high-affinity choline uptake. Animal models showed that brain acetylcholine levels increase during aerobic exercise, specifically in the hippocampus and cortex. This increase in acetylcholine supports the generation of hippocampal theta activity, which enhances synaptic plasticity and memory formation [170, 171]. Therefore, changes in the acetylcholine system may be involved in exercise-induced improvements in cognitive function; however, this relationship has not yet been investigated in patients which schizophrenia.
Endocannabinoid system
The endocannabinoid system, including altered expression of the cannabinoid 1 (CB1) receptor, has been implicated in the pathophysiology of schizophrenia [172, 173]. It represents a neuromodulatory system that is known to regulate emotional and cognitive processes, resulting in analgesia, sedation, anxiolysis, and a sense of wellbeing [155, 174]. This system comprises cannabinoid 1 and 2 (CB1 and CB2) receptors, which are expressed at high density in the brain and periphery [175].
Sparling et al. [176] reported the first evidence that exercise is able to activate the endocannabinoid system by showing elevated plasma anandamide levels in healthy runners and cyclists when compared with sedentary controls. Exercise can help to modulate the endocannabinoid system, which may mediate some of the beneficial impacts of exercise on cognition and mood [177, 178]. Although this hypothesis has not yet been further investigated, the effects of exercise on the endocannabinoid system might contribute to its positive effects on cognition and mood in schizophrenia patients.
Hypothalamus–pituitary–adrenal (HPA) axis hormones
HPA axis dysregulation and altered blood cortisol levels are implicated in mental stress, and are suggested to be a pathophysiological factor in schizophrenia, especially during acute episodes [179,180,181]. In addition, BDNF expression is suppressed under conditions of chronic adverse stress, because hippocampal BDNF mRNA is negatively correlated with plasma glucocorticoid levels. This has been shown in animals to lead to an impaired ability of neurons to protect themselves against injury and disease, as outlined previously [182].
Although physical exercise is an acute stressor, chronic exercise can have neuroprotective effects. Some of the hypotheses presented in the literature that address the correlation between the HPA axis and exercise suggest that biological changes in the activity of the HPA axis could be an effective feedback mechanism via enhanced density and efficiency of mineralocorticoid receptors, lower cortisol levels, and inhibition of cortisol synthesis [183]. However, results concerning brain HPA axis hormones are somewhat equivocal. There is only weak evidence that exercise alters cortisol concentrations in humans [184]. Regarding the expression of corticotrophin-releasing hormone (CRH) mRNA, some authors stated that it is decreased in the hypothalamus after long-term exposure to exercise [185], whereas others found either no significant effect [186] or an initial increase followed by a return to original levels [187].
The findings concerning the effect of chronic exercise on brain corticosteroid receptor mRNA gene expression are contradictory [119, 186].
Summing up, there is no clear evidence for biological changes in the activity of the HPA axis after exercise in either healthy individuals or schizophrenia patients.
Immune-related mechanisms
In patients with schizophrenia, increased brain inflammatory markers [188] and a chronic low-grade systemic inflammation with microglia activation [189, 190] have been reported, and inflammation has been proposed to affect cognitive functioning [191]. However, in schizophrenia, a reduced expression of immune-related genes has also been detected and related to disturbed synaptic processes [192]. In this context, treatment with antipsychotics may influence the expression of pro-inflammatory genes [193].
Animals with increased brain inflammatory factors (such as TNF-alpha, IL-6, CRP, and 1IL-1beta) show depression-like and sickness behavior [194, 195]. The levels of the neuroinflammatory mediators and also the sickness behavior can be attenuated by voluntary aerobic exercise [196]. Aerobic exercise has been shown to be a promising intervention to reduce inflammation in the periphery and the brain of animals [197, 198].
Acute exercise leads to a rapid elevation in peripheral levels of IL-6, but the rise of inflammatory markers is quickly followed by the induction of anti-inflammatory substances, such as IL-1ra, IL-10, and soluble tumor necrosis factor receptor. Regular exercise, on the other hand, downregulates systemic inflammation via homeostatic adaption [103, 199]. Several studies have shown an inverse association between regular exercise and various inflammatory biomarkers, such as TNF-α [200], IFN-γ [197], and IL-1β [198, 201, 202]. In addition, aerobic exercise leads to a reduction of IL-18, CRP, TNF-alpha, and IL-1beta [203, 204] and a marked increase in anti-inflammatory mediators, such as IL-10 [205, 206]. Moreover, exercise results in a decrease in pro-inflammatory visceral white fat mass [198, 204], in the proliferation of microglia [197], and in the hippocampal expression of immune-related genes [207, 208].
In schizophrenia patients, changes in C-reactive protein (CRP) were studied after 8 weeks of high-intensity interval training (HIIT). Although CRP decreased by 66%, the difference from the non-exercising control group was not statistically significant [209]. Another study examined serum CRP, IL-6, and TNF-alpha levels in obese patients with schizophrenia after a 10-week lifestyle intervention (including lifestyle modification, psychosocial treatment, behavior therapy, and aerobic exercise). The authors were not able to find any significant changes in comparison to the control group, which consisted of matched controls without psychiatric disorders [117]. However, levels of circulating pro-inflammatory cytokines in the blood are confounded by many factors, including smoking, obesity, sleep disorders, and poor oral health, all of which are common in schizophrenia and further contribute to the inflammatory burden in schizophrenia patients [103, 120, 210]. Thus, to date, the extent to which aerobic exercise can improve cognitive functioning in schizophrenia via alterations in the expression of immune-related genes remains unclear.
Exercise-induced generation of reactive oxygen species
Increased free radical production and an impaired antioxidant defense system have been shown to be involved in the pathophysiology of schizophrenia [211]. In addition, oxidative changes have been shown to interfere with the stability of genomic DNA in the brain of schizophrenia patients [212]. Oxidative stress is defined as an imbalance between antioxidants and reactive oxygen species (ROS) (e.g., superoxide, hydrogen peroxide, and hydroxyl radical) [213]. It has been suggested that the beneficial effects of regular aerobic exercise are partly based on its ability to generate ROS [214]. Exercise-induced ROS production contributes to the induction of antioxidants, DNA repair, and protein-degrading enzymes [155]. Long-term exercise may be helpful in optimizing the enzymatic antioxidant system and mitigating oxidative damage in schizophrenia patients, but this issue has not been studied yet [154].
Discussion
The aim of this narrative review was to give an overview of different lines of evidence on how exercise impacts brain function at different levels in patients with schizophrenia. We wanted to clarify how those effects of exercise could be related to the clinical and functional outcomes.
The past years have seen a growing number of publications on the neurobiological mechanisms of exercise, but few have reported on these effects in patients with schizophrenia. Although the clinical effects of exercise in schizophrenia are becoming increasingly evident, more research on the underlying neuroadaptive processes is warranted.
Animal studies have provided consistent evidence that exercise results in brain morphological changes and functional adaptations, including an increase in the concentrations of neurotrophic factors and neurotransmitters.
Animal models provide a valuable source of information, because they enable experimental approaches and give insights into the molecular and cellular mechanisms that cannot be investigated in humans. Although animal models have revealed much about the potential neurobiological mechanisms of exercise effects on brain and cognition, the findings often cannot be easily generalized to humans because of the physiological and behavioral differences between humans and other species. Evidence from human studies on the neuroadaptive processes of exercise is limited to date. Because of the often small effect sizes and numerous negative findings, conclusions must be drawn cautiously. Given the rather limited amount of research, especially in patients with schizophrenia, it is currently not possible to either confirm or refute any of the above-mentioned neurobiological explanations. However, research to date indicates that, in schizophrenia patients, aerobic exercise has an impact on brain structure (e.g., as shown by MRI studies) and function (e.g., as shown by TMS studies), epigenetic mechanisms, gene expression, and neurotransmitters, restores BDNF levels, and may influence immune-related genes (Fig. 2).
In general, exercise research comes with some limitations, because the interventions depend on the participants’ compliance. Patients with schizophrenia may often have a diminished motivation to be physically active, which is why research might represent a positive selection [76]. In addition, treatment with antipsychotics may increase sedation and muscular exhaustion. Therefore, patients performing aerobic exercise need concomitant supervision and encouragement by sports scientists [23]. Furthermore, the duration, frequency, and modality of aerobic exercise training differ between studies [215].
Additional research is needed to clarify the role of the cellular and molecular pathways in patients with schizophrenia. The field will profit from additional randomized-controlled trials, which have the potential to systematically establish a causal relationship between aerobic exercise, its neurobiological effects, and outcome parameters, such as negative symptoms and cognitive deficits.
We have little knowledge on the optimal intensity, duration, and frequency of exercise that may be required for exercise-induced changes to interact with schizophrenia or on the type of exercise that may be most beneficial [23, 216]. Further research is required to clarify in more detail how individual differences in patients with schizophrenia mediate or moderate the effects of exercise on the brain and cognition. In this context, it may be important to examine the effects of genetic and environmental risk factors on the individual response to aerobic exercise.
Limitations of this narrative review include the lack of systematic literature research, which increases the risk of selection and evaluation bias. However, the main aim of this review was to give an overview of the current knowledge about the impact of aerobic exercise on neurobiological functions from the macro- to the micro-level with a focus on schizophrenia patients to foster a general debate and discuss rationales for future research.
Even though its underlying neurobiological mechanisms have not yet been fully clarified, exercise remains a promising candidate in the search for interventions that address the negative and cognitive symptoms of patients with schizophrenia and, thus, improve their outcome.
References
Fusar-Poli P et al (2015) Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull 41(4):892–899
Nielsen RE et al (2015) Second-generation antipsychotic effect on cognition in patients with schizophrenia—a meta-analysis of randomized clinical trials. Acta Psychiatr Scand 131(3):185–196
Vancampfort D et al (2012) The functional exercise capacity is correlated with global functioning in patients with schizophrenia. Acta Psychiatr Scand 125(5):382–387
Vancampfort D, Rosenbaum S, Probst M, Stubbs B (2018) Aerobic exercise in people with schizophrenia. In: Budde H, Wegner M (eds) The exercise effect on mental health, neurobiological mechanisms. Routledge, New York
Falkai P, Malchow B, Schmitt A (2017) Aerobic exercise and its effects on cognition in schizophrenia. Curr Opin Psychiatry 30(3):171–175
Dauwan M et al (2016) Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophr Bull 42(3):588–599
Malchow B et al (2015) Effects of endurance training combined with cognitive remediation on everyday functioning, symptoms, and cognition in multiepisode schizophrenia patients. Schizophr Bull 41(4):847–858
Schmitz N, Kruse J, Kugler J (2004) The association between physical exercises and health-related quality of life in subjects with mental disorders: results from a cross-sectional survey. Prev Med 39(6):1200–1207
Firth J et al (2016) Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull 43(3):546–556
Rosenbaum S et al (2014) Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry 75(9):964–974
Firth J et al (2015) A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med 45(7):1343–1361
Scheewe TW et al (2013) Exercise therapy improves mental and physical health in schizophrenia: a randomised controlled trial. Acta Psychiatr Scand 127(6):464–473
Laursen TM, Munk-Olsen T, Vestergaard M (2012) Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry 25(2):83–88
Li M et al (2014) Schizophrenia and risk of stroke: a meta-analysis of cohort studies. Int J Cardiol 173(3):588–590
Vancampfort D et al (2015) Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry 14(3):339–347
Vancampfort D et al (2016) Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry 15(2):166–174
De Hert M et al (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10(1):52–77
Stubbs B et al (2015) How can we promote smoking cessation in people with schizophrenia in practice? A clinical overview. Acta Psychiatr Scand 132(2):122–130
Heald A et al (2015) Diet, exercise and the metabolic syndrome in schizophrenia: a cross-sectional study. Schizophr Res 169(1–3):494–495
Stubbs B et al (2016) How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res 176(2–3):431–440
Correll CU et al (2015) Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry 14(2):119–136
Falkai P et al (2015) Kraepelin revisited: schizophrenia from degeneration to failed regeneration. Mol Psychiatry 20(6):671–676
Keller-Varady K et al (2016) Endurance training in patients with schizophrenia and healthy controls: differences and similarities. Eur Arch Psychiatry Clin Neurosci 266(5):461–473
Ogunyankin F et al (2018) Effects of exercise-based interventions in severe mental illness: a feasibility study. Eur Arch Psychiatry Clin Neurosci. https://doi.org/10.1007/s00406-018-0864-8
Kandola A et al (2016) Aerobic exercise as a tool to improve hippocampal plasticity and function in humans: practical implications for mental health treatment. Front Hum Neurosci 10:373
van Praag H (2008) Neurogenesis and exercise: past and future directions. Neuromol Med 10(2):128–140
Sack M et al (2017) Early effects of a high-caloric diet and physical exercise on brain volumetry and behavior: a combined MRI and histology study in mice. Brain Imaging Behav 11(5):1385–1396
van Praag H et al (2005) Exercise enhances learning and hippocampal neurogenesis in aged mice. J Neurosci 25(38):8680–8685
Vivar C, Potter MC, van Praag H (2013) All about running: synaptic plasticity, growth factors and adult hippocampal neurogenesis. Curr Top Behav Neurosci 15:189–210
Erickson KI et al (2009) Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus 19(10):1030–1039
Parker BA et al (2011) Effect of exercise training on hippocampal volume in humans: a pilot study. Res Q Exerc Sport 82(3):585–591
Voss MW et al (2013) The influence of aerobic fitness on cerebral white matter integrity and cognitive function in older adults: results of a one-year exercise intervention. Hum Brain Mapp 34(11):2972–2985
Firth J et al (2018) Effect of aerobic exercise on hippocampal volume in humans: a systematic review and meta-analysis. Neuroimage 166:230–238
Colcombe S, Kramer AF (2003) Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci 14(2):125–130
Weinstein AM et al (2012) The association between aerobic fitness and executive function is mediated by prefrontal cortex volume. Brain Behav Immun 26(5):811–819
Makizako H et al (2015) Moderate-intensity physical activity, hippocampal volume, and memory in older adults with mild cognitive impairment. J Gerontol A Biol Sci Med Sci 70(4):480–486
Cahill LS et al (2015) MRI-detectable changes in mouse brain structure induced by voluntary exercise. Neuroimage 113:175–183
McMorris T, Corbett J (2018) Neurobiological changes and exercise. In: Budde H, Wegner M (eds) The exercise effect on mental health: neurobiological mechanisms. CRC Press
Pajonk FG et al (2010) Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry 67(2):133–143
Malchow B et al (2016) Effects of endurance training on brain structures in chronic schizophrenia patients and healthy controls. Schizophr Res 173(3):182–191
Papiol S et al (2017) Polygenic risk has an impact on the structural plasticity of hippocampal subfields during aerobic exercise combined with cognitive remediation in multi-episode schizophrenia. Transl Psychiatry 7(6):e1159
Fields RD (2008) White matter in learning, cognition and psychiatric disorders. Trends Neurosci 31(7):361–370
Lehmann N, Taubert M (2018) Improvement in motor learning. In: Budde HW (ed) The exercise effect on mental health, neurobiological effects. Routledge, New York
Herting MM et al (2014) White matter connectivity and aerobic fitness in male adolescents. Dev Cognit Neurosci 7:65–75
Burdette JH et al (2010) Using network science to evaluate exercise-associated brain changes in older adults. Front Aging Neurosci 2:23
Sexton CE et al (2016) A systematic review of MRI studies examining the relationship between physical fitness and activity and the white matter of the ageing brain. Neuroimage 131:81–90
Fitzsimmons J, Kubicki M, Shenton ME (2013) Review of functional and anatomical brain connectivity findings in schizophrenia. Curr Opin Psychiatry 26(2):172–187
Vakhrusheva J et al (2016) Aerobic exercise in people with schizophrenia: neural and neurocognitive benefits. Curr Behav Neurosci Rep 3(2):165–175
Reid MA et al (2016) A combined diffusion tensor imaging and magnetic resonance spectroscopy study of patients with schizophrenia. Schizophr Res 170(2–3):341–350
Cassoli JS et al (2015) Disturbed macro-connectivity in schizophrenia linked to oligodendrocyte dysfunction: from structural findings to molecules. NPJ Schizophr 1:15034
Svatkova A et al (2015) Physical exercise keeps the brain connected: biking increases white matter integrity in patients with schizophrenia and healthy controls. Schizophr Bull 41(4):869–878
Basso JC, Suzuki WA (2017) The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: a review. Brain Plast 2(2):127–152
Colcombe SJ et al (2004) Neurocognitive aging and cardiovascular fitness: recent findings and future directions. J Mol Neurosci 24(1):9–14
Voss MW et al (2010) Plasticity of brain networks in a randomized intervention trial of exercise training in older adults. Front Aging Neurosci 2:32
Voss MW et al (2016) Fitness, but not physical activity, is related to functional integrity of brain networks associated with aging. Neuroimage 131:113–125
Cirillo J et al (2009) Motor cortex plasticity induced by paired associative stimulation is enhanced in physically active individuals. J Physiol 587(Pt 24):5831–5842
Honzak R et al (1985) Changes in the EEG spectrum at a two-week intensive endurance training. Act Nerv Super (Praha) 27(1):10–14
Gliner JA et al (1979) Visual evoked potentials and signal detection following a marathon race. Med Sci Sports 11(2):155–159
Roeh A et al (2018) Effects of three months of aerobic endurance training on motor cortical excitability in schizophrenia patients and healthy subjects. Neuropsychobiology. https://doi.org/10.1159/000489714
Weissleder C, North HF, Weickert CS (2019) Important unanswered questions about adult neurogenesis in schizophrenia. Curr Opin Psychiatry 32(3):170–178
Van der Borght K et al (2007) Exercise improves memory acquisition and retrieval in the Y-maze task: relationship with hippocampal neurogenesis. Behav Neurosci 121(2):324–334
Uysal N et al (2005) The effects of regular aerobic exercise in adolescent period on hippocampal neuron density, apoptosis and spatial memory. Neurosci Lett 383(3):241–245
Redila VA, Christie BR (2006) Exercise-induced changes in dendritic structure and complexity in the adult hippocampal dentate gyrus. Neuroscience 137(4):1299–1307
Clark PJ et al (2008) Intact neurogenesis is required for benefits of exercise on spatial memory but not motor performance or contextual fear conditioning in C57BL/6J mice. Neuroscience 155(4):1048–1058
Biedermann S et al (2012) In vivo voxel based morphometry: detection of increased hippocampal volume and decreased glutamate levels in exercising mice. Neuroimage 61(4):1206–1212
Herting MM (2018) Exercise in cognition and motor learning. In: Budde H, Wegner M (eds) The exercise effect on mental health: neurobiological mechanisms. CRC Press
Sorrells SF et al (2018) Human hippocampal neurogenesis drops sharply in children to undetectable levels in adults. Nature 555:377
Brockett AT, LaMarca EA, Gould E (2015) Physical exercise enhances cognitive flexibility as well as astrocytic and synaptic markers in the medial prefrontal cortex. PLoS ONE 10(5):e0124859
Mei YY, Wu DC, Zhou N (2018) Astrocytic regulation of glutamate transmission in schizophrenia. Front Psychiatry 9:544
Bernardi C et al (2013) Treadmill exercise induces hippocampal astroglial alterations in rats. Neural Plasticity 2013:709732
Krityakiarana W et al (2010) Voluntary exercise increases oligodendrogenesis in spinal cord. Int J Neurosci 120(4):280–290
Jiang T et al (2017) Physical exercise improves cognitive function together with microglia phenotype modulation and remyelination in chronic cerebral hypoperfusion. Front Cell Neurosci 11:404
Tomlinson L, Leiton CV, Colognato H (2016) Behavioral experiences as drivers of oligodendrocyte lineage dynamics and myelin plasticity. Neuropharmacology 110(Pt B):548–562
Katsel P et al (2017) Microvascular anomaly conditions in psychiatric disease Schizophrenia–angiogenesis connection. Neurosci Biobehav Rev 77:327–339
Murrell CJ et al (2013) Cerebral blood flow and cerebrovascular reactivity at rest and during sub-maximal exercise: effect of age and 12-week exercise training. Age 35(3):905–920
Bragina IN, Voelcker-Rehage C (2018) Exercise effect in older adults. In: Budde H, Wegner M (eds) The exercise effect on mental health: neurobiological mechanisms. CRC Press
Pereira AC et al (2007) An in vivo correlate of exercise-induced neurogenesis in the adult dentate gyrus. Proc Natl Acad Sci USA 104(13):5638–5643
Christie BR et al (2008) Exercising our brains: how physical activity impacts synaptic plasticity in the dentate gyrus. Neuromol Med 10(2):47–58
Glatt SJ et al (2011) Similarities and differences in peripheral blood gene-expression signatures of individuals with schizophrenia and their first-degree biological relatives. Am J Med Genet B Neuropsychiatr Genet 156b(8):869–887
Szyf M (2014) Examining peripheral DNA methylation in behavioral epigenetic and epigenetic psychiatry: opportunities and challenges. Epigenomics 6(6):581–584
Peter CJ, Akbarian S (2011) Balancing histone methylation activities in psychiatric disorders. Trends Mol Med 17(7):372–379
Schmitt A et al (2014) The impact of environmental factors in severe psychiatric disorders. Front Neurosci 8:19
Schmitt A et al (2017) Consensus paper of the WFSBP task force on biological markers: criteria for biomarkers and endophenotypes of schizophrenia, part III: Molecular mechanisms. World J Biol Psychiatry 18(5):330–356
Bahari-Javan S et al (2017) HDAC1 links early life stress to schizophrenia-like phenotypes. Proc Natl Acad Sci USA 114(23):E4686–E4694
Voisin S et al (2015) Exercise training and DNA methylation in humans. Acta Physiol (Oxf) 213(1):39–59
Fernandes J, Arida RM, Gomez-Pinilla F (2017) Physical exercise as an epigenetic modulator of brain plasticity and cognition. Neurosci Biobehav Rev 80:443–456
Mega F et al (2018) Paternal physical exercise demethylates the hippocampal DNA of male pups without modifying the cognitive and physical development. Behav Brain Res 348:1–8
Yeshurun S, Hannan AJ (2019) Transgenerational epigenetic influences of paternal environmental exposures on brain function and predisposition to psychiatric disorders. Mol Psychiatry 24(4):536–548
Maejima H et al (2018) Exercise enhances cognitive function and neurotrophin expression in the hippocampus accompanied by changes in epigenetic programming in senescence-accelerated mice. Neurosci Lett 665:67–73
Bianchi M et al (2017) Coordinated actions of MicroRNAs with other epigenetic factors regulate skeletal muscle development and adaptation. Int J Mol Sci 18(4):840
Dong J et al (2018) MicroRNA-132 is associated with the cognition improvement following voluntary exercise in SAMP8 mice. Brain Res Bull 140:80–87
Kashimoto RK et al (2016) Physical exercise affects the epigenetic programming of rat brain and modulates the adaptive response evoked by repeated restraint stress. Behav Brain Res 296:286–289
Fernandes J et al (2018) Hippocampal microRNA-mRNA regulatory network is affected by physical exercise. Biochim Biophys Acta 1862(8):1711–1720
Denham J, Prestes PR (2016) Muscle-enriched MicroRNAs isolated from whole blood are regulated by exercise and are potential biomarkers of cardiorespiratory fitness. Front Genet 7:196
Kohman RA et al (2011) Voluntary wheel running reverses age-induced changes in hippocampal gene expression. PLoS ONE 6(8):e22654
Molteni R, Ying Z, Gómez-Pinilla F (2002) Differential effects of acute and chronic exercise on plasticity-related genes in the rat hippocampus revealed by microarray. Eur J Neurosci 16(6):1107–1116
Radahmadi M, Hosseini N, Alaei H (2016) Effect of exercise, exercise withdrawal, and continued regular exercise on excitability and long-term potentiation in the dentate gyrus of hippocampus. Brain Res 1653:8–13
Zheng F et al (2016) Voluntary running depreciates the requirement of Ca2 + -stimulated cAMP signaling in synaptic potentiation and memory formation. Learn Mem 23(8):442–449
Ohline SM, Abraham WC (2018) Environmental enrichment effects on synaptic and cellular physiology of hippocampal neurons. Neuropharmacology 145:3–12
Gomez-Pinilla F, Vaynman S, Ying Z (2008) Brain-derived neurotrophic factor functions as a metabotrophin to mediate the effects of exercise on cognition. Eur J Neurosci 28(11):2278–2287
Binder DK, Scharfman HE (2004) Mini review. Growth Factors 22(3):123–131
Rothman SM, Mattson MP (2013) Activity-dependent, stress-responsive BDNF signaling and the quest for optimal brain health and resilience throughout the lifespan. Neuroscience 239:228–240
Berk M et al (2013) So depression is an inflammatory disease, but where does the inflammation come from? BMC Med 11:200
Tartaglia N et al (2001) Protein synthesis-dependent and-independent regulation of hippocampal synapses by brain-derived neurotrophic factor. J Biol Chem 276(40):37585–37593
Berchtold NC, Castello N, Cotman CW (2010) Exercise and time-dependent benefits to learning and memory. Neuroscience 167(3):588–597
Korte M et al (1995) Hippocampal long-term potentiation is impaired in mice lacking brain-derived neurotrophic factor. Proc Natl Acad Sci USA 92(19):8856–8860
Neeper SA et al (1995) Exercise and brain neurotrophins. Nature 373(6510):109
Korte M et al (1996) Virus-mediated gene transfer into hippocampal CA1 region restores long-term potentiation in brain-derived neurotrophic factor mutant mice. Proc Natl Acad Sci 93(22):12547–12552
Patterson SL et al (1996) Recombinant BDNF rescues deficits in basal synaptic transmission and hippocampal LTP in BDNF knockout mice. Neuron 16(6):1137–1145
Szuhany KL, Bugatti M, Otto MW (2015) A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor. J Psychiatr Res 60:56–64
Mora F, Segovia G, del Arco A (2007) Aging, plasticity and environmental enrichment: structural changes and neurotransmitter dynamics in several areas of the brain. Brain Res Rev 55(1):78–88
Guillin O, Demily C, Thibaut F (2007) Brain-derived neurotrophic factor in schizophrenia and its relation with dopamine. Int Rev Neurobiol 78:377–395
Green MJ et al (2011) Brain-derived neurotrophic factor levels in schizophrenia: a systematic review with meta-analysis. Mol Psychiatry 16(9):960–972
Zhang XY et al (2012) Low BDNF is associated with cognitive impairment in chronic patients with schizophrenia. Psychopharmacology 222(2):277–284
Park H, Poo MM (2013) Neurotrophin regulation of neural circuit development and function. Nat Rev Neurosci 14(1):7–23
Kim HJ et al (2014) Increase of circulating BDNF levels and its relation to improvement of physical fitness following 12 weeks of combined exercise in chronic patients with schizophrenia: a pilot study. Psychiatry Res 220(3):792–796
Kuo FC et al (2013) Lifestyle modification and behavior therapy effectively reduce body weight and increase serum level of brain-derived neurotrophic factor in obese non-diabetic patients with schizophrenia. Psychiatry Res 209(2):150–154
Kimhy D et al (2015) The impact of aerobic exercise on brain-derived neurotrophic factor and neurocognition in individuals with schizophrenia: a single-blind, randomized clinical trial. Schizophr Bull 41(4):859–868
Chang Y-T et al (2008) Glucocorticoid signaling and exercise-induced downregulation of the mineralocorticoid receptor in the induction of adult mouse dentate neurogenesis by treadmill running. Psychoneuroendocrinology 33(9):1173–1182
Firth J et al (2017) The pro-cognitive mechanisms of physical exercise in people with schizophrenia. Br J Pharmacol 174(19):3161–3172
Chen MJ, Ivy AS, Russo-Neustadt A (2006) Nitric oxide synthesis is required for exercise-induced increases in hippocampal BDNF and phosphatidylinositol 3′ kinase expression. Brain Res Bull 68(4):257–268
Gill JM (2007) Physical activity, cardiorespiratory fitness and insulin resistance: a short update. Curr Opin Lipidol 18(1):47–52
Pan W, Kastin AJ (2000) Interactions of IGF-1 with the blood-brain barrier in vivo and in situ. Neuroendocrinology 72(3):171–178
Cotman CW, Berchtold NC (2002) Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci 25(6):295–301
Sonntag WE et al (2000) The effects of growth hormone and IGF-1 deficiency on cerebrovascular and brain ageing. J Anat 197(Pt 4):575–585
Martinotti G et al (2012) Nerve growth factor and brain-derived neurotrophic factor concentrations in schizophrenia: a review. J Biol Regul Homeost Agents 26(3):347
Venkatasubramanian G et al (2007) Insulin and insulin-like growth factor-1 abnormalities in antipsychotic-naive schizophrenia. Am J Psychiatry 164(10):1557–1560
Andrade e Silva B et al (2015) A 20-week program of resistance or concurrent exercise improves symptoms of schizophrenia: results of a blind, randomized controlled trial. Rev Bras de Psiquiatr 37(4):271–279
Gavin TP et al (2004) Angiogenic growth factor response to acute systemic exercise in human skeletal muscle. J Appl Physiol 96(1):19–24
Gustafsson T et al (2002) Increased expression of vascular endothelial growth factor in human skeletal muscle in response to short-term one-legged exercise training. Pflügers Archiv 444(6):752–759
Tang K et al (2010) Exercise-induced VEGF transcriptional activation in brain, lung and skeletal muscle. Respir Physiol Neurobiol 170(1):16–22
Misiak B et al (2018) Vascular endothelial growth factor in patients with schizophrenia: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 86:24–29
Gómez-Pinilla F, Dao L, So V (1997) Physical exercise induces FGF-2 and its mRNA in the hippocampus. Brain Res 764(1–2):1–8
Hunsberger JG et al (2007) Antidepressant actions of the exercise-regulated gene VGF. Nat Med 13(12):1476
Van Hoomissen JD et al (2004) Effects of β-adrenoreceptor blockade during chronic exercise on contextual fear conditioning and mRNA for galanin and brain-derived neurotrophic factor. Behav Neurosci 118(6):1378
Voss MW et al (2011) Exercise, brain, and cognition across the life span. J Appl Physiol 111(5):1505–1513
Meeusen R, Piacentini MF, De Meirleir K (2001) Brain microdialysis in exercise research. Sports Med 31(14):965–983
Lee GJ, Park JH, Park HK (2008) Microdialysis applications in neuroscience. Neurol Res 30(7):661–668
Buhot MC, Martin S, Segu L (2000) Role of serotonin in memory impairment. Ann Med 32(3):210–221
Naughton M, Mulrooney JB, Leonard BE (2000) A review of the role of serotonin receptors in psychiatric disorders. Hum Psychopharmacol 15(6):397–415
Meeter M et al (2006) Effects of 5-HT on memory and the hippocampus: model and data. Neuropsychopharmacology 31(4):712–720
Gray JA, Roth BL (2007) Molecular targets for treating cognitive dysfunction in schizophrenia. Schizophr Bull 33(5):1100–1119
Chen H-I et al (2008) Treadmill exercise enhances passive avoidance learning in rats: the role of down-regulated serotonin system in the limbic system. Neurobiol Learn Mem 89(4):489–496
Meeusen R, De Meirleir K (1995) Exercise and brain neurotransmission. Sports Med 20(3):160–188
Blomstrand E (2006) A role for branched-chain amino acids in reducing central fatigue. J Nutr 136(2):544S–547S
Kiank C et al (2010) Psychological stress-induced, IDO1-dependent tryptophan catabolism: implications on immunosuppression in mice and humans. PLoS ONE 5(7):e11825
Lee H et al (2013) Regular moderate or intense exercise prevents depression-like behavior without change of hippocampal tryptophan content in chronically tryptophan-deficient and stressed mice. PLoS ONE 8(7):e66996
McMorris T (2016) Developing the catecholamines hypothesis for the acute exercise-cognition interaction in humans: lessons from animal studies. Physiol Behav 165:291–299
Lammel S, Lim BK, Malenka RC (2014) Reward and aversion in a heterogeneous midbrain dopamine system. Neuropharmacology 76:351–359
Howes OD, Kapur S (2009) The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull 35(3):549–562
Mathes WF et al (2010) Dopaminergic dysregulation in mice selectively bred for excessive exercise or obesity. Behav Brain Res 210(2):155–163
Greenwood BN et al (2011) Long-term voluntary wheel running is rewarding and produces plasticity in the mesolimbic reward pathway. Behav Brain Res 217(2):354–362
Goffer Y et al (2013) Calcium-permeable AMPA receptors in the nucleus accumbens regulate depression-like behaviors in the chronic neuropathic pain state. J Neurosci 33(48):19034–19044
Phillips C (2017) Physical activity modulates common neuroplasticity substrates in major depressive and bipolar disorder. Neural Plast 2017:7014146
Deslandes A et al (2009) Exercise and mental health: many reasons to move. Neuropsychobiology 59(4):191–198
Holtmaat A, Svoboda K (2009) Experience-dependent structural synaptic plasticity in the mammalian brain. Nat Rev Neurosci 10(9):647
Howes O, McCutcheon R, Stone J (2015) Glutamate and dopamine in schizophrenia: an update for the 21st century. J Psychopharmacol 29(2):97–115
Hasan A et al (2014) The glutamate hypothesis of schizophrenia. Fortschr Neurol Psychiatr 82(8):447–456
Jia J et al (2009) Pre-ischemic treadmill training affects glutamate and gamma aminobutyric acid levels in the striatal dialysate of a rat model of cerebral ischemia. Life Sci 84(15–16):505–511
Sutoo DE, Akiyama K (1996) The mechanism by which exercise modifies brain function. Physiol Behav 60(1):177–181
Maddock RJ et al (2016) Acute modulation of cortical glutamate and GABA content by physical activity. J Neurosci 36(8):2449–2457
Gregoire CA et al (2018) RNA-sequencing reveals unique transcriptional signatures of running and running-independent environmental enrichment in the adult mouse dentate gyrus. Front Mol Neurosci 11:126
Vasuta C et al (2007) Effects of exercise on NMDA receptor subunit contributions to bidirectional synaptic plasticity in the mouse dentate gyrus. Hippocampus 17(12):1201–1208
Ren H et al (2017) Effects of different training loads on emotional state and mRNA and protein expressions of N-methyl-D-aspartate receptor subunits, postsynaptic density 95, and kinesin family member 17 in hippocampus of rats. Med Sci Monit 23:4954–4960
Martin-Ruiz CM et al (2003) Dementia rating and nicotinic receptor expression in the prefrontal cortex in schizophrenia. Biol Psychiatry 54(11):1222–1233
Wong DF et al (2018) Brain PET imaging of alpha7-nAChR with [18F]ASEM: reproducibility, occupancy, receptor density, and changes in schizophrenia. Int J Neuropsychopharmacol 21(7):656–667
Jones C (2018) alpha7 nicotinic acetylcholine receptor: a potential target in treating cognitive decline in schizophrenia. J Clin Psychopharmacol 38(3):247–249
Segal-Gavish H et al (2017) Voluntary exercise improves cognitive deficits in female dominant-negative DISC1 transgenic mouse model of neuropsychiatric disorders. World J Biol Psychiatry 20(3):243–252
Fordyce D, Farrar R (1991) Enhancement of spatial learning in F344 rats by physical activity and related learning-associated alterations in hippocampal and cortical cholinergic functioning. Behav Brain Res 46(2):123–133
Giocomo LM, Hasselmo ME (2007) Neuromodulation by glutamate and acetylcholine can change circuit dynamics by regulating the relative influence of afferent input and excitatory feedback. Mol Neurobiol 36(2):184–200
Buzsaki G (2005) Theta rhythm of navigation: link between path integration and landmark navigation, episodic and semantic memory. Hippocampus 15(7):827–840
Leweke FM et al (2018) Role of the endocannabinoid system in the pathophysiology of schizophrenia: implications for pharmacological intervention. CNS Drugs 32(7):605–619
Ibarra-Lecue, I., et al., The endocannabinoid system in mental disorders: Evidence from human brain studies. Biochem Pharmacol, 2018
Dietrich A, McDaniel WF (2004) Endocannabinoids and exercise. Br J Sports Med 38(5):536–541
Piomelli D (2003) The molecular logic of endocannabinoid signalling. Nat Rev Neurosci 4(11):873–884
Sparling P et al (2003) Exercise activates the endocannabinoid system. NeuroReport 14(17):2209–2211
Tantimonaco M et al (2014) Physical activity and the endocannabinoid system: an overview. Cell Mol Life Sci 71(14):2681–2698
Grassmann VM, Faulkner G, Can PA (2018) Prevent mental illness? In: Budde H, Wegner M (eds) The exercise effect on mental health: neurobiological mechanisms. CRC Press
Walker E, Mittal V, Tessner K (2008) Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol 4:189–216
Steen NE et al (2014) Altered systemic cortisol metabolism in bipolar disorder and schizophrenia spectrum disorders. J Psychiatr Res 52:57–62
Holsen LM et al (2013) HPA-axis hormone modulation of stress response circuitry activity in women with remitted major depression. Neuroscience 250:733–742
Murakami S et al (2005) Chronic stress, as well as acute stress, reduces BDNF mRNA expression in the rat hippocampus but less robustly. Neurosci Res 53(2):129–139
Stranahan AM, Lee K, Mattson MP (2008) Central mechanisms of HPA axis regulation by voluntary exercise. NeuroMol Med 10(2):118–127
Hayes LD et al (2015) Exercise-induced responses in salivary testosterone, cortisol, and their ratios in men: a meta-analysis. Sports Med 45(5):713–726
Bi S et al (2005) Running wheel activity prevents hyperphagia and obesity in Otsuka long-evans Tokushima Fatty rats: role of hypothalamic signaling. Endocrinology 146(4):1676–1685
Droste SK et al (2007) Voluntary exercise impacts on the rat hypothalamic-pituitary-adrenocortical axis mainly at the adrenal level. Neuroendocrinology 86(1):26–37
Park E et al (2005) Changes in basal hypothalamo-pituitary-adrenal activity during exercise training are centrally mediated. Am J Physiol Regul Integr Comp Physiol 289(5):R1360–R1371
Trepanier MO et al (2016) Postmortem evidence of cerebral inflammation in schizophrenia: a systematic review. Mol Psychiatry 21(8):1009–1026
Potvin S et al (2008) Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry 63(8):801–808
van Kesteren CF et al (2017) Immune involvement in the pathogenesis of schizophrenia: a meta-analysis on postmortem brain studies. Transl Psychiatry 7(3):e1075
Dickerson F et al (2007) C-reactive protein is associated with the severity of cognitive impairment but not of psychiatric symptoms in individuals with schizophrenia. Schizophr Res 93(1):261–265
Schmitt A et al (2011) Regulation of immune-modulatory genes in left superior temporal cortex of schizophrenia patients: a genome-wide microarray study. World J Biol Psychiatry 12(3):201–215
Kato T et al (2007) Risperidone significantly inhibits interferon-gamma-induced microglial activation in vitro. Schizophr Res 92(1–3):108–115
Garcia-Bueno B, Caso JR, Leza JC (2008) Stress as a neuroinflammatory condition in brain: damaging and protective mechanisms. Neurosci Biobehav Rev 32(6):1136–1151
Anisman H (2009) Cascading effects of stressors and inflammatory immune system activation: implications for major depressive disorder. J Psychiatry Neurosci 34(1):4–20
Littlefield AM et al (2015) Voluntary exercise attenuates LPS-induced reductions in neurogenesis and increases microglia expression of a proneurogenic phenotype in aged mice. J Neuroinflamm 12:138
Svensson M, Lexell J, Deierborg T (2015) Effects of physical exercise on neuroinflammation, neuroplasticity, neurodegeneration, and behavior: what we can learn from animal models in clinical settings. Neurorehabil Neural Repair 29(6):577–589
Petersen AM, Pedersen BK (2005) The anti-inflammatory effect of exercise. J Appl Physiol 98(4):1154–1162
Teixeira de Lemos E et al (2011) Differential effects of acute (extenuating) and chronic (training) exercise on inflammation and oxidative stress status in an animal model of type 2 diabetes mellitus. Mediat Inflamm. https://doi.org/10.1155/2011/253061
Gomes da Silva S et al (2013) Exercise-induced hippocampal anti-inflammatory response in aged rats. J Neuroinflamm 10:61
Erion JR et al (2014) Obesity elicits interleukin 1-mediated deficits in hippocampal synaptic plasticity. J Neurosci 34(7):2618–2631
Hamer M, Endrighi R, Poole L (2012) Physical activity, stress reduction, and mood: insight into immunological mechanisms. Methods Mol Biol 934:89–102
Eyre H, Baune BT (2012) Neuroimmunological effects of physical exercise in depression. Brain Behav Immun 26(2):251–266
Donges CE, Duffield R, Drinkwater EJ (2010) Effects of resistance or aerobic exercise training on interleukin-6, C-reactive protein, and body composition. Med Sci Sports Exerc 42(2):304–313
Aderbal SL Jr, Latini A (2018) Treating depression with exercise, an immune perspecitve. In: Budde HW (ed) The exercise effect on mental health, neurobiological mechanisms. Routledge, New York
Kadoglou NP et al (2007) The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus. Eur J Cardiovasc Prev Rehabil 14(6):837–843
Parachikova A, Nichol KE, Cotman CW (2008) Short-term exercise in aged Tg2576 mice alters neuroinflammation and improves cognition. Neurobiol Dis 30(1):121–129
Martin SA et al (2013) Effects of voluntary wheel running on LPS-induced sickness behavior in aged mice. Brain Behav Immun 29:113–123
Heggelund J et al (2011) Effects of high aerobic intensity training in patients with schizophrenia—a controlled trial. Nord J Psychiatry 65(4):269–275
McCreadie RG (2003) Diet, smoking and cardiovascular risk in people with schizophrenia. Br J Psychiatry 183(6):534–539
Wu JQ, Kosten TR, Zhang XY (2013) Free radicals, antioxidant defense systems, and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 46:200–206
Raza MU et al (2016) DNA damage in major psychiatric diseases. Neurotox Res 30(2):251–267
Sies H (2015) Oxidative stress: a concept in redox biology and medicine. Redox Biol 4:180–183
Radak Z et al (2008) Exercise, oxidative stress and hormesis. Ageing Res Rev 7(1):34–42
Malchow B et al (2013) The effects of physical exercise in schizophrenia and affective disorders. Eur Arch Psychiatry Clin Neurosci 263(6):451–467
Keller-Varady K et al (2018) A systematic review of trials investigating strength training in schizophrenia spectrum disorders. Schizophr Res 192:64–68
Acknowledgements
This research was funded by the following grants from the German Research Foundation (DFG): Klinische Forschergruppe (KFO) 241, and PsyCourse to PF (FA241/16-1). Further funding was received from the German Federal Ministry of Education and Research (BMBF) through the research network on psychiatric diseases ESPRIT (grant number 01EE1407E) to PF, AH, and AS. The authors would like to thank Jacquie Klesing, BMedSci (Hons), Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript. Ms. Klesing received compensation for her work from the LMU Munich, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maurus, I., Hasan, A., Röh, A. et al. Neurobiological effects of aerobic exercise, with a focus on patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci 269, 499–515 (2019). https://doi.org/10.1007/s00406-019-01025-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01025-w