Abstract
Chronic reductions in cerebral blood flow (CBF) and cerebrovascular reactivity to CO2 are risk factors for cerebrovascular disease. Higher aerobic fitness is associated with higher CBF at any age; however, whether CBF or reactivity can be elevated following an exercise training intervention in healthy individuals is unknown. The aim of this study was to assess the effect of exercise training on CBF and cerebrovascular reactivity at rest and during exercise in young and older individuals. Ten young (23 ± 5 years; body mass index (BMI), 26 ± 3 kg m−2; \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \), 35 ± 5 ml kg−1 min−1) and 10 older (63 ± 5 years; BMI, 25 ± 3.0 kg m−2; \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \), 26 ± 4 ml kg-1 min−1) previously sedentary individuals breathed 5 % CO2 for 3 min at rest and during steady-state cycling exercise (30 and 70 % heart rate range (HRR)) prior to and following a 12-week aerobic exercise intervention. Effects of training on middle cerebral artery blood velocity (MCAv) at rest were unclear in both age groups. The absolute MCAv response to exercise was greater in the young (9 and 9 cm s−1 (30 and 70 % HRR, respectively) vs. 5 and 4 cm s−1 (older), P < 0.05) and was similar following training. Cerebrovascular reactivity was elevated following the 12-week training at rest (2.87 ± 0.76 vs. 2.54 ± 1.12 cm s−1 mm Hg−1, P = 0.01) and during exercise, irrespective of age. The finding of a training-induced elevation in cerebrovascular reactivity provides further support for exercise as a preventative tool in cerebrovascular and neurological disease with ageing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The maintenance of adequate cerebral blood flow (CBF) is critical to maintain a constant supply of oxygen and nutrients to the metabolically active brain. The control of CBF is multi-factorial, influenced largely by the partial pressure of arterial carbon dioxide (PaCO2) and to a lesser extent by cerebral metabolism, mean arterial pressure (MAP), cardiac output (\( \mathop{Q}\limits^{ \cdot } \)) distribution and neurogenic activity (Ainslie and Duffin 2009). Chronic reductions in CBF and impairments in its control are risk factors for cerebrovascular disease. A reduced absolute cerebral blood flow may result in stroke (Markus 2004) and is a major risk factor for Alzheimer's disease and dementia (de la Torre 2010). In addition, an impaired ability of the cerebral vasculature to respond to changes in PaCO2 (termed cerebrovascular reactivity) is a risk factor for—and a consequence of—cerebrovascular disease (Gur et al. 1996; Markus and Cullinane 2001; Silvestrini et al. 2000). Assessment of the cerebrovascular response to alterations in PaCO2 (by measuring changes in middle cerebral artery blood flow velocity (MCAv)) is a well-established means to estimate the physiological ‘reserve’ of cerebral perfusion (Ainslie and Duffin 2009).
Global CBF declines gradually with ageing, by 25–30 % between 20 and 80 years of age (Ainslie et al. 2008; Buijs et al. 1998; Demirkaya et al. 2008; Krejza et al. 1999; Liu et al. 2011) or ~5 % per decade (Grolimund and Seiler 1988). The effect of healthy ageing on cerebrovascular CO2 reactivity is less clear, however. Hypercapnic reactivity has been found to be both lower (Reich and Rusinek 1989; Yamamoto et al. 1980) and unchanged (Davis et al. 1983; Ito et al. 2002; Kastrup et al. 1998; Schwertfeger et al. 2006; Galvin et al. 2010) with advancing age, while hypocapnic reactivity has been found to be elevated (Galvin et al. 2010), unchanged (Ito et al. 2002) and reduced (Yamaguchi et al. 1979; Tsuda and Hartmann 1989). Differences in measurement technique, stimulus magnitude (i.e. PaCO2 change) and subject age make inter-study comparison difficult.
In addition, MCAv has been shown to be increased ~10–25 % with higher aerobic fitness across the adult lifespan (Ainslie et al. 2008), but the reasons remain unclear. One cross-sectional study indicated that higher fitness is related to larger frontal and temporal volumes of grey matter (Colcombe et al. 2006). Other potential mechanisms may involve more endothelium-dependent vasodilatation as a result of more NO bioavailability (Green et al. 2004) and/or cerebral angiogenesis (Rhyu et al. 2010; Swain et al. 2003; Ding et al. 2006; Black et al. 1990). In support of this, age-induced cerebral atrophy appears to be less marked in those with higher aerobic fitness (Colcombe et al. 2003). Furthermore, 6 months of aerobic exercise training can even increase brain volume in previously sedentary older individuals (Colcombe et al. 2006), so a corresponding increase in CBF would seem plausible. Yet Ivey et al. (2011) found no increase in CBF following 6 months of aerobic-based exercise training in chronic hemiparetic stroke patients. In summary, cross-sectional data indicate that fitness training may increase CBF, consistent with the demonstrated improvements in neuronal mass and metabolism, but it remains to be shown whether CBF is actually increased with training or whether this occurs in both young and older healthy individuals.
Another important consideration is whether ageing impacts on CBF responses to common daily activity (e.g. exercise) and if so, why? Only two studies have assessed the effect of age on the CBF response to sub-maximal exercise, and both observed no differential effect of age on the exercise-induced increase in CBF (Fisher et al. 2008; Heckmann et al. 2003). In addition to the CBF response, cerebrovascular CO2 reactivity is also increased during exercise (Ogoh et al. 2008; Rasmussen et al. 2006). Although the effects of exercise on CBF (Ogoh and Ainslie 2009; Querido and Sheel 2007) and cerebrovascular reactivity (Ogoh et al. 2008; Rasmussen et al. 2006) have been relatively well documented in young individuals, any influencing effect of older age on these parameters has not been established. Due to the conflicting evidence on the effect of age on cerebrovascular reactivity at rest, it is unclear what effect (if any) age has on cerebrovascular reactivity during exercise.
Although cerebrovascular diseases such as stroke have been associated with an impaired cerebrovascular reactivity, and regular physical activity is known to reduce the risk of stroke, only one study has assessed the effect of fitness on cerebrovascular reactivity to CO2. Ivey et al. (2011) demonstrated an elevation in cerebrovascular reactivity to CO2 following 6 months of exercise training in stroke survivors. Whether similar improvements can be observed in healthy young and older individuals following a lesser amount of exercise training is unknown. This fitness-induced reduction in the risk of stroke is due to upregulation of endothelial NO synthase (Endres et al. 2003; Gertz et al. 2006; Lee and Paffenbarger 1998). Furthermore, it is known that hypercapnia-induced cerebrovascular vasodilatation is, at least in part, NO dependent (Peebles et al. 2007). Since systemic NO production/bioavailability is increased with exercise training (Kingwell et al. 1997), it seems possible that increases in aerobic fitness will be associated with increases in cerebrovascular reactivity.
The main purposes of this study were twofold: (1) to assess the effect of age on CBF and its reactivity at rest and during sub-maximal exercise and (2) assess improvements in the aforementioned parameters across 12 weeks of aerobic-based exercise training. We hypothesised that (1) cerebrovascular reactivity would be maintained in healthy older age and age would have no effect on the elevation in CBF or cerebrovascular reactivity during sub-maximal exercise and (2) 12 weeks of aerobic-based exercise training would increase CBF and its reactivity at rest and during exercise regardless of age.
Methods
Participants
Twenty-six participants (13 young and 13 older) volunteered for this study which was approved by the University of Otago's Human Ethics Committee and complied with the Declaration of Helsinki. All were inactive, participating in less than 30 min of exercise three times per week for ≥2 years. Six participants withdrew from the study during the training intervention for various reasons (too busy with work/university, loss of interest, poor health of family members). Consequently, 20 participants (10 young and 10 older, Table 1) completed the study. Participants were informed of the experimental procedures and potential risks involved in the study before their written consent was obtained. Participants were not taking any cardiovascular medications, all were non-smokers and none had any history of cardiovascular, cerebrovascular or respiratory disease. Participants all had a body mass index (BMI) ≤30 kg m−2, and none had any musculoskeletal problems which prevented them from exercising. All older females were post-menopausal.
Experimental design
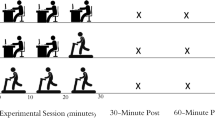
Participants reported to the laboratory on four occasions prior to training and twice after training. Before inclusion into the study, all participants were screened by means of a thorough medical history, physical activity history and 12-lead ECG. If any significant ECG abnormality or arrhythmia was detected, participants underwent a clinical transthoracic echocardiogram to exclude overt pathology. Following successful screening, participants underwent a maximal aerobic power (\( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \)) test. Participants then underwent the main testing protocol on two separate occasions, the first as a familiarisation and the second for data collection (pre-training). Prior to each session, participants were asked to abstain from alcohol and caffeine in the 12 h prior to testing and avoid a large meal in the 2 h prior to testing. Participants were also asked to arrive well-hydrated by consuming 1 L of water the evening prior to and 0.5 L the morning of testing. On arrival at the laboratory for the main session, participants voided their bladder prior to body composition assessment using bioelectrical impedance (Inbody 230, Biospace, Seoul, Korea). Following procurement of a venous blood sample and instrumentation, participants assumed a seated position for assessment of cerebrovascular reactivity. Following this assessment, participants were transferred to a cycle ergometer (Excalibur Sport, Lode B.V., The Netherlands) where they exercised at 30 % and then 70 % of heart rate range (HRR) whilst breathing room air for 5 min and 5 % CO2 (in air) for a further 3 min.
Participants then began the 12-week aerobic-based exercise intervention, as detailed below. Following the 12 weeks of training, participants underwent a second \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \) test and then a repeat of the main (pre-training) testing protocol. Relative exercise intensities for the post-training protocol were recalculated from the post-training \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \) test. To control for menstrual cycle phase in the young female participants, pre- and post-training testing was completed in the early follicular phase, when oestrogen and progesterone concentrations are at their lowest. In addition, each participant's post-training testing session was completed at the same time of the day (±2 h) as their pre-training session.
Exercise training protocol
The 12-week mostly supervised, aerobic-based exercise intervention took place in Dunedin, New Zealand in spring 2008 (1st September–23rd November). At the beginning of the intervention, participants were issued with a recordable heart rate monitor to use during each exercise session (Polar S610i monitors, Polar, Finland) and a physical activity diary. Participants were asked to record information about each exercise session in the diary (mode, duration and intensity). Fourteen supervised exercise sessions were scheduled each week (five circuit gym-based (treadmill, stationary bike, rowing machine, stepper, arm crank, skipping etc.), nine walking/jogging group-based), and participants could attend whichever sessions they wished. Participants were encouraged to attend the supervised scheduled sessions as much as possible; however, some preferred to exercise alone and/or at times that best suited their schedules. All participants followed the same progression in frequency (from three sessions per week (weeks 1–4) to four sessions per week (weeks 9–12)), intensity (from 50–65 % HRR (weeks 1–4) to 65–80 % HRR (weeks 9–12)) and duration (from 20–30 min per session (weeks 1–4) to 40–50 min (weeks 9–12)) of exercise sessions during the intervention. Exercise intensity (in percent of HRR) was determined for each participant from their maximal heart rate (HR) obtained during the initial \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \) test.
Protocols and measurements
Assessment of maximal aerobic power (\( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \))
Participants performed the incremental maximal exercise test on a cycle ergometer (Velotron Elite, RacerMate Inc., Seattle, WA, USA), with starting workloads and increments dependent upon age and sex. Expired O2 and CO2 fractions were measured using an online gas analyser (Quark CPET, Cosmed, Rome, Italy), and \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \) was determined from the highest 20-s value.
CBF velocity arterial BP and heart rate
Blood flow velocity in the right middle cerebral artery (MCAv) was measured using a 2-MHz pulsed Doppler ultrasound system (DWL Doppler, Sterling VA, USA). Beat-to-beat BP was measured using finger photoplethysmography (Finometer, TPD Biomedical Instruments, The Netherlands). From the blood pressure waveform, HR, stroke volume (SV) and \( \mathop{Q}\limits^{ \cdot } \) were calculated using the Modelflow method which incorporates sex, age, height and mass data (BeatScope 1.0 software; TNO-TPD Biomedical Instruments). All data were sampled continuously at 200 Hz using an analogue digital converter (Powerlab/16SP ML795; ADInstruments, Colorado Springs, CO, USA) interfaced with a computer. Data were later analysed using a commercially available software (Chart version 5.4.2, ADInstruments). Total peripheral resistance (TPR) was estimated as MAP/\( \mathop{Q}\limits^{ \cdot } \). Cerebrovascular resistance was estimated as MAP/MCAv.
Respiratory variables
During each session, participants breathed through a leak-free respiratory mask (Hans-Rudolph 8980, Kansas City, MO), attached to a one-way valve (Hans-Rudolph 2700) and fitted with a spirometer (Hans-Rudolph bi-directional and linear pneumotachometer, Series 3830, Hans-Rudolph). Minute ventilation (\( {\mathop {V}\limits^{\text{.}} }_{{\text{E}}} \)) was calculated from the spirometer, and the partial pressures of end-tidal CO2 and O2 (PETCO2 and PETO2) were sampled from the leak-free mask and measured using a fast responding gas analyser (model CD-3A (CO2) and model S-3A/I (O2), AEI Technologies, Pittsburgh, PA). Changes in PETCO2 adequately reflect those of PaCO2, especially in the hypocapnic range (Thomas et al. 2009), and there is no evidence to indicate that healthy ageing affects this linear relationship between PaCO2 and PETCO2 (Marsden et al. 2011).
Biochemical variables
Prior to and following training, a 10-mL fasted venous blood sample was procured for analysis of lipid profile and glucose concentration. Lipid and glucose samples were analysed in duplicate using photometric analysis (Cobas c111, Roche Diagnostics Ltd., Basel, Switzerland).
Assessment of cerebrovascular CO2 reactivity
Cerebrovascular reactivity to hypercapnia and hypocapnia was assessed whilst seated at rest. Following baseline recordings (of MCAv and PETCO2), participants breathed a 5 % CO2 (in room air) gas mixture for 3 min (hypercapnia), and the change in PETCO2 from baseline was recorded. Following a recovery period to restore PETCO2, participants were then hyperventilated for 3 min to reach an equivalent reduction in PETCO2 (hypocapnia) to match the increase observed with prior hypercapnia. In addition, hypercapnic cerebrovascular reactivity was assessed during steady-state sub-maximal cycling exercise at 30 and 70 % of HRR. Cerebrovascular reactivity was calculated from the data obtained in the final minute of the 3-min intervention and assessed as ΔMCAv/ΔPETCO2. The use of only one level of hypercapnia (5 %) may over- or under-estimate MCAv reactivity to CO2 because there is an exponential relationship between the two variables. However, 5 % CO2 was chosen as the concentration for the CO2 stimulus because this is the maximum limit tolerated by most people during exercise whilst also wishing to limit the total period of exercise and hypercapnia required of (initially) untrained participants.
Statistical and data analysis
Steady-state resting data were obtained whilst seated following instrumentation and averaged over a 2-min period. A second 2-min baseline period (immediately prior to the assessment of cerebrovascular reactivity) was used for all resting reactivity analysis. Steady-state resting reactivity data were obtained from the average final 60 s of the 3-min hypercapnia or hypocapnia intervention. Reactivity was calculated as both absolute (change in MCAv per millimetre Hg change in PETCO2) and relative (change in MCAv (as a percentage of resting MCAv) divided by the change in PETCO2). Steady-state baseline data during cycling exercise were averaged over a 60-s period >4 min after the onset of exercise (or the increase in workload). Similar to rest, hypercapnia data were obtained in the final 60 s of the 3-min intervention.
To evaluate the effect of age on pre-exercise resting variables (i.e. purpose 1), one-way ANOVA were used. Effects of age and training on resting variables were assessed by two-factor repeated measures ANOVA. Furthermore, three-factor repeated measures ANOVA were conducted to assess the effect of training (purpose 2) on cerebrovascular responses and cerebrovascular reactivity during exercise (between-subjects factor: age; within-subjects factors: training and exercise). Any significant interactions were isolated using Bonferroni-controlled post hoc t tests. All data were analysed using SPSS statistical software (SPSS version 17.0, SPSS Inc., Chicago, IL). Statistical significance was established at an α level of 0.05, and data are expressed as means (±SD). In addition, reliability of the MCAv signal was compared from seated baseline measures during the familiarisation and main testing sessions prior to training.
Post-training MCAv at rest was corrected (to account for the lowered post-training PETCO2), by multiplying the difference in PETCO2 by each individual’s post-training hypocapnic cerebrovascular reactivity and adding this to the MCAv. Coefficient of variation was calculated as the total unbiased error, divided by the grand mean and multiplied by 100 %. Intra-class correlation was also used to determine reliability (Hopkins 2000). Age effects on pre-training variables were analysed using the 26 individuals (n = 13 in each group) who began the study. Effects of training were analysed using the 20 individuals who completed the training (i.e. n = 10 in each group). There were no apparent sex-related statistical differences in our main outcome variables; thus, data for males and females were pooled for analysis. Finally, due to many poor Finometer traces during exercise, the blood pressure data are not reported.
Results
Effect of age on resting variables (pre-training data)
Participant characteristics and cardiorespiratory and cerebrovascular variables
Despite greater height, body mass and muscle mass in the young (P < 0.05, Table 1), both age groups had a similar BMI and body fat percentage. As expected, \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \) was lower in the older individuals (P < 0.01). Apart from an elevated systolic BP (~15 %, P < 0.05; Table 2) in the older participants, all other cardiovascular variables (i.e. HR, MAP, diastolic BP, SV, \( \mathop{Q}\limits^{ \cdot } \) and TPR) were not different with age. Mean MCAv, systolic MCAv and diastolic MCAv were lower (~27, ~22 and ~32 %, respectively; P < 0.01), and CVR was higher (~53 %, P < 0.01) in the older participants. All respiratory variables were not different with age.
Cerebrovascular reactivity
Resting cerebrovascular reactivity (i.e. the change in MCAv (in centimetres per second) per millimetre Hg change in PETCO2) to both hypocapnia (1.4 (young) vs. 1.8 cm s−1 mm Hg−1 (older)) and hypercapnia (1.5 (young) vs. 1.2 cm s−1 mm Hg−1 (older), Table 3) was similar between young and older participants (both P > 0.05, Fig. 2). However, when cerebrovascular reactivity is considered in relative terms (i.e. percent change in MCAv per millimetre Hg change in PETCO2), the hypocapnic reactivity was elevated in the older participants (3.9 (older) vs. 2.3 % mm Hg−1 (young), P < 0.01), whilst hypercapnic reactivity was not (2.5 (older) vs. 2.4 % mm Hg−1 (young), P = 0.55). Ventilatory sensitivity to hypercapnia tended to be higher in the young participants at rest (P = 0.07); however, the variability in this group was twice that of the older individuals.
Effect of age on responses to acute exercise (pre-training data)
Cardiorespiratory and cerebrovascular variables
MCAv was elevated above resting values during sub-maximal cycling exercise at 30 and 70 % of HRR in both young and older participants (P < 0.01). The younger individuals exhibited a greater absolute increase in MCAv during exercise (7 and 9 cm s−1 (30 and 70 % (uncorrected for exercise-induced reductions in PETCO2) HRR, respectively) vs. 2 and 2 cm s−1, respectively (older); P = 0.02); however, when expressed as a relative change, there was no reliable difference between age groups (11 and 14 % (30 and 70 % HRR, respectively; young) vs. 5 and 4 %, respectively (older); P = 0.21). Mean PETCO2 was also elevated with exercise (~2–3 mm Hg, P < 0.01), in both young and older participants. As expected, greater absolute increases in HR were observed in the young (P < 0.01), and the absolute \( {\mathop {V}\limits^{\text{.}} }_{{\text {E}}} \) response to exercise tended to be higher in the young (P = 0.07). Cerebral TOI was unchanged during exercise (P > 0.05).
Cerebrovascular reactivity
Hypercapnic cerebrovascular reactivity was increased during exercise at both 30 and 70 % of HRR (P < 0.01), independent of age. Both groups exhibited approximately twofold increases in the MCAv response to elevations in PETCO2 at 70 % HRR (1.5 (rest)–2.6 cm s−1 mm Hg−1 (70 %, young) and 1.2–2.5 cm s−1 mm Hg−1 (70 %, older), Table 3). Ventilatory sensitivity to hypercapnia was also elevated above resting levels during exercise (P < 0.01).
Effect of training on resting variables
Training
Of the 26 participants who started the training programme, 20 (77 %; 10 young, 10 older) completed the entire 12-week training intervention. Although body mass and BMI were unchanged (P > 0.05, Table 1), body composition was altered favourably, with an increase in muscle mass (~2 %) and reduction in body fat (~5 %, both P < 0.05). In addition, \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \), a measure of cardiorespiratory fitness, was increased by ~6 % (P < 0.05). All training-induced anthropometric changes were comparable across age. Fasted plasma glucose was lowered across training (P < 0.05, Table 2), but lipid variables were unchanged (P > 0.05).
Cardiorespiratory and cerebrovascular variables
On initial assessment, resting MCAv was unchanged with training (P > 0.05, Table 2); however, independent of changes in alveolar ventilation, measured PETCO2 was lowered post-training (P < 0.05). When this effect of resting hypocapnia on MCAv was corrected for (see ‘Methods’), MCAv was elevated following training (P = 0.02, Fig. 1). This elevation was apparent in 17/20 participants and averaged 4 ± 6 cm s−1 (range, −8 to +18 cm s−1). Resting HR was reduced following training; however, this reduction was greater in the young (P < 0.05).
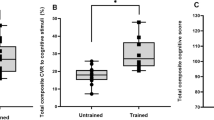
Effect of training on cerebrovascular reactivity at rest
Resting hypercapnic cerebrovascular reactivity was elevated following training in both young and older individuals (combined, 1.9 ± 0.7 vs. 1.4 ± 0.6 cm s−1 mm Hg−1 (pre-training); P = 0.01; Fig. 2), whereas hypocapnic cerebrovascular reactivity was unchanged (P > 0.05). Furthermore, ventilatory sensitivity to hypercapnia was unchanged (P > 0.05).
Absolute (± SD) changes in middle cerebral artery blood flow velocity (MCAv, top) during normocapnia, hypercapnia (5 % CO2) and hyperventilation-induced hypocapnia (PETCO2) at rest, prior to (grey) and following (black) 12 weeks of aerobic-based exercise training in up to 10 young and 10 older individuals and the corresponding calculated cerebrovascular CO2 reactivity (MCAv-CO2 reactivity, bottom). ‡P < 0.05, different from pre-training
Effect of training on responses to acute exercise
Absolute workrates were increased by 28 % and 31 % for younger and older participants respectively, following training (i.e., to attain the same proportion of HRR).
Cardiorespiratory and cerebrovascular variables
Similar to pre-training, the young individuals exhibited a greater absolute increase in MCAv in response to exercise (9 and 9 cm s−1 (30 and 70 % HRR, respectively) vs. 5 and 4 cm s−1, respectively (older); age × exercise interaction, P < 0.05; Fig. 3). Training itself had no effect on the MCAv response to exercise in either age group (P > 0.05). The \( {\mathop {V}\limits^{\text{.}} }_{{\text {E}}} \) and PETCO2 responses to exercise were different following training (training × exercise interactions, P < 0.05), with an increased \( {\mathop {V}\limits^{\text{.}} }_{{\text {E}}} \) at 70 % HRR (+14 L min−1 vs. pre-training, P < 0.05) and reduced PETCO2 at 30 and 70 % HRR (−4 mm Hg vs. pre-training (at 70 % HRR), P < 0.05). When MCAv was corrected for the exercise-induced hypocapnia at 70 % HRR, the measured MCAv was significantly lower than the corrected value (P < 0.05); however, this did not differ with age. Like pre-training, the HR response to exercise was lower in the older individuals (P < 0.05). In addition, training resulted in an elevated HR response at 70 % HRR (+5 beats min−1 vs. pre-training, P < 0.05).
Middle cerebral artery blood flow velocity (MCAv) (a), partial pressure of end-tidal CO2 (PETCO2) (b), minute ventilation (\( {\mathop {V}\limits^{\text{.}} }_{{\text {E}}} \)) (c) and heart rate (HR) (d) response (I). Absolute or relative change from rest (II) to sub-maximal cycling exercise at 30 and 70 % of HRR in young and older individuals prior to and following a 12-week exercise training intervention. In (I), pre-training values are depicted in grey and post-training in black. Furthermore, change score differences (i.e. absolute value or percentage point change) in response to exercise between pre- and post-training are displayed in the right column (III). *P < 0.05 different from young; ‡P < 0.05, different from pre-training
Cerebrovascular reactivity
Similar to pre-training values, cerebrovascular reactivity to hypercapnia was increased during sub-maximal exercise (P < 0.05), with a similar response across age. Similar to resting hypercapnic reactivity, the 12 weeks of training increased reactivity responses during the sub-maximal exercise in both groups (by 0.3–0.6 cm s-1 mm Hg−1, P = 0.03 vs. pre-training values; Fig. 4). Although ventilatory sensitivity was elevated during exercise, the response did not differ to pre-training (P > 0.05).
Absolute changes in middle cerebral artery blood flow velocity (MCAv) (a) during normocapnia, hypercapnia (5 % CO2) and hyperventilation-induced hypocapnia (PETCO2) at rest and during cycling exercise at 30 and 70 % HRR, prior to (grey) and following (black) 12 weeks of aerobic based exercise training in up to 10 young and 10 older individuals. Corresponding calculated cerebrovascular CO2 reactivity (MCAv-CO2 reactivities in young (b) and older (c) individuals) and individual change scores between pre- and post-training (d). †P < 0.05, different from rest; ‡P < 0.05, different from pre-training
Discussion
This is the first known study to assess the effect of age and training on MCAv and cerebrovascular CO2 reactivity both at rest and during exercise. The major finding from this study was that following a 12-week aerobic-based exercise training intervention, we observed an elevation in the cerebrovascular reactivity to hypercapnia, both at rest and during acute exercise. Of note, this fitness-induced elevation in cerebrovascular reactivity occurred independently of age and was possibly associated with increased MCAv at rest. These findings support the use of exercise as a therapeutic tool in the prevention of cerebrovascular disease.
Influence of age on cerebral blood flow and cerebrovascular reactivity at rest and during exercise
Older individuals have been reported to have a maintained (Davis et al. 1983; Ito et al. 2002; Kastrup et al. 1998; Schwertfeger et al. 2006; Galvin et al. 2010) and reduced (Reich and Rusinek 1989; Yamamoto et al. 1980) hypercapnic cerebrovascular reactivity compared to younger individuals. The reasons for the discrepancy are likely to be multi-factorial and may include differences in CBF measurement technique (i.e. transcranial Doppler (TCD), Xe inhalation and positron emission tomography), the extent of the CO2 stimulus and whether incorporated into a room air or hyperoxic solution, the age ranges used to describe ‘older’, and posture (Galvin et al. 2010). Data from this study are in support of a maintained cerebrovascular reactivity to hypercapnia in older age. Indeed, Kastrup et al. (1998), who used TCD to assess changes in MCAv to 5 % CO2 (a similar protocol to this study), observed no effect of age on hypercapnic reactivity in men. Interestingly, they did observe an elevated reactivity to CO2 in pre-menopausal women, but not in post-menopausal women. That finding indicates a potential effect of oestrogens on cerebrovascular reactivity to CO2 (Kastrup et al. 1998). In contrast, we observed no effect of sex on cerebrovascular reactivity; however, all older females were post-menopausal and all young females were tested in the low oestrogen (early follicular) phase of the menstrual cycle or during the ‘sugar-pill’ week if using oral contraceptives (when oestrogen was low).
The effect of age on hypocapnic cerebrovascular reactivity is also controversial, with reports of an unchanged (Ito et al. 2002), reduced (Yamaguchi et al. 1979; Tsuda and Hartmann 1989) and even increased (Galvin et al. 2010) reactivity in older age. In the current study, absolute cerebrovascular reactivity to hypocapnia was comparable whereas relative cerebrovascular hypocapnic reactivity was actually higher with older age. However, because of the lower absolute MCAv in the older participants, any change in MCAv to hypocapnia will manifest in a disproportionately larger percent change in the older compared to the young. Thus, it seems that that there is a little effect of age on global cerebrovascular reactivity.
MCAv was elevated ~5–15 % in response to sub-maximal exercise in both young and older individuals. This magnitude of increase is similar to that observed by other authors using transcranial Doppler to assess blood flow velocity in the MCA during exercise (Hellstrom et al. 1996; Jorgensen et al. 1992; Linkis et al. 1995; Moraine et al. 1993; Ogoh et al. 2005). However, MCAv at 70 % HRR was similar or slightly reduced compared with that observed at 30 % HRR. This is in accordance with previous reports that the increase in MCAv is intensity dependent up until ~60 % of \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \), after which it declines back towards resting levels due to hyperventilation-induced hypocapnia (Hellstrom et al. 1996; Moraine et al. 1993). Below ventilatory threshold, the increase in CBF with exercise is likely driven by increases in cerebral metabolism and PaCO2, as a result of increased functional activation with motor activity (Hellstrom et al. 1996; Moraine et al. 1993); however, above this, the large disproportional increase in ventilation reduces PaCO2 and thus CBF despite progressive elevations in cerebral metabolism (Hellstrom et al. 1996; Moraine et al. 1993).
When expressed in absolute terms, the younger participants exhibited a greater increase (9 vs. 2 cm s−1 (older)) in MCAv during sub-maximal exercise. When expressed as a percent change from rest (14 % (young) vs. 4 % (older), at 70 % HRR), the age effect was not statistically significant (P = 0.21); however, this likely represents a lack of statistical power. Fisher et al. (2008) and Heckmann et al. (2003) have both assessed the effect of age on the MCAv response to sub-maximal exercise, and both found no differential effect of age. Surprisingly however, in both of these studies, there was no difference in resting MCAv with age, making comparison with this study difficult. Fisher et al. (2008) compared the MCAv response to 30 and 50 % HRR. Interestingly, although not significant, the absolute change in MCAv during exercise at 50 % was lower in their older individuals (~7 % increase from rest in the young vs. ~2 % in the older individuals), similar to our observations at 70 % HRR. In opposition to these findings by Fisher et al. and Heckmann et al., a recent study (Marsden et al. 2011) demonstrated similar findings to ours of a lesser increase in MCAv in older individuals in comparison to the young (15 vs. 28 %) during sub-maximal intensities. It seems that younger individuals with an already higher CBF have a greater absolute capacity to increase CBF. Whether the greater exercise-induced increase in MCAv in the young individuals is merely a function of a higher starting point or is due to the higher absolute workload required in the young to elicit the same percentage heart rates (thereby resulting in an increased neural activation and consequently metabolism) is unknown. It is not attributable to a larger exercise-induced rise in the perfusion pressure (MAP). Overall, the effect of age on the cerebrovascular response to exercise (both sub-maximal and maximal) requires further investigation.
An increase in hypercapnic cerebrovascular reactivity during exercise, as observed in this study, is similar to previous reports (Ogoh et al. 2008; Rasmussen et al. 2006; Ogoh et al. 2009). The exact mechanisms responsible for the increased reactivity are unknown; however, increases in cerebral activation, core temperature (Rasmussen et al. 2006) and CO2-induced increases in MAP (Ainslie et al. 2005) have been suggested. Similar to the findings from this study, Rasmussen et al. (2006) observed an approximately twofold increase in hypercapnic reactivity during exercise at 67 % \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \). The exercise-induced elevations in reactivity observed by Ogoh et al. (2008) were substantially less, at only 15–20 %, despite similar CBF measurement technique and CO2 stimulus to that in the present study. However, in that study, participants were only exercising at ~32 % \( {\mathop{V}\limits^{ \cdot }{_{\text{O2}}}}\max \), potentially indicating a relationship with exercise intensity. Although data from our study support that of Rasmussen et al. (2006) with regards to the extent of the MCAv response to changes in CO2, we did not observe further elevations in hypercapnic reactivity with increasing exercise intensity. Overall, in this study we observed that the increase in hypercapnic reactivity occurred independent of age, indicating a maintained control of CBF during exercise with healthy ageing.
Effect of training on MCAv
Measured resting MCAv was unchanged following the 12 weeks of training. However, training was associated with a lowered (measured) resting PETCO2. The reason for the lower PETCO2 following training is unknown; however, one group has found that the act of imagining dynamic exercise increased ventilation in athletes compared to non-athletes (Wuyam et al. 1995), potentially accounting for the 2-mm Hg reduction in PETCO2 following the training intervention, as participants were aware that they were about to perform exercise. When MCAv was corrected for the post-training alterations in PETCO2 (using the post-training hypocapnic reactivity), resting MCAv was significantly elevated following 12 weeks of aerobic-based exercise training. Fitness-induced elevations in MCAv have been observed in a cross-sectional cohort (Ainslie et al. 2008); however, this has not yet been demonstrated in a longitudinal study, and the present data provide some support for such an effect, but not clear support. It may be that the small sample size in this study was insufficient to accurately assess the effect of exercise training on MCAv.
Effect of training on resting variables
The 12 weeks of exercise training was associated with the expected reductions in body fat percentage and increases in muscle mass and maximal oxygen consumption. Although training had no effect on MAP, resting HR was reduced in both groups. A lowered resting HR is a common feature of exercise training (Thompson et al. 2001; Boutcher and Stein 1995) and may indicate an increased vagal outflow.
Cerebrovascular reactivity at rest
Cerebrovascular reactivity to hypercapnia was elevated, by 10–15 %, following the 12-week training intervention and without the confounding effects that were evident for the MCAv response. This elevation also occurred independently of age, indicating that healthy ageing does not affect the ability of the cerebrovascular bed to adapt to exercise training. This is only the second known study to report on the effect of fitness on cerebrovascular reactivity in humans. Ivey et al. (2011) demonstrated a ~30 % elevation in cerebrovascular reactivity to 6 % CO2 in stroke survivors following 6 months of exercise training. Interestingly, the elevation in fitness across the training intervention was positively correlated with the change in cerebrovascular reactivity, indicating that the increased aerobic capacity is at least, in part, responsible for the improved cerebrovascular reactivity. Swain et al. (2003) used MRI in rats to assess the cerebral responses to 10 % CO2 prior to and following at least 30 days of voluntary exercise or sedentary living. They found a 22 % increase in signal intensity during CO2 inhalation (when compared to pre-training) in the exercise group, indicating a more pronounced CBF response to hypercapnia, which supports the findings from this study and is independent of inferring an increased perfusion based on velocity measurements. Whether similar differences in cerebrovascular reactivity are observed in a cross-sectional cohort requires further investigation. An impaired cerebrovascular reactivity has been identified as a risk factor for stroke [4-6]. In addition, an elevated cardiorespiratory fitness has been associated with a reduced risk of stroke (Endres et al. 2003; Gertz et al. 2006; Lee and Paffenbarger 1998; Hooker et al. 2008). This fitness-induced elevation in cerebrovascular reactivity may provide an important physiological link in the relationship between fitness and cerebrovascular disease.
The mechanisms responsible for this increase in hypercapnic cerebrovascular reactivity following chronic exercise training are not well understood but likely involve NO. Cerebrovascular vasodilatation in response to hypercapnia is, in part, dependent upon NO bioavailability (Peebles et al. 2007). Nitric oxide has been reported to increase with exercise training (Green et al. 2004; Kingwell et al. 1997). Exercise training has also been shown to increase systemic endothelium-dependent vasodilatation (a NO-mediated response) (Green et al. 2004; Clarkson et al. 1999; Tinken et al. 2008). Furthermore, a link between the systemic endothelial function and cerebrovascular reactivity has been established (Ainslie et al. 2007; Lavi et al. 2006), indicating that any improvements in systemic vascular function might also be reflected in the cerebral circulation (as now demonstrated in this study). In addition, the reduced stroke risk and improved long-term outcome as a result of physical activity have been postulated to be due to upregulation of endothelial NO synthase (Endres et al. 2003; Gertz et al. 2006). Additional mechanisms potentially contributing to this increased cerebrovascular reactivity include brain-derived neurotrophic factor (Seifert et al. 2010) and insulin-like growth factor-1 (Llorens-Martin et al. 2010). Furthermore, hypocapnic cerebrovascular reactivity—a response which is not NO mediated (Peebles et al. 2007)—was unchanged following training, further supporting the suggestion that the training-induced elevation in hypercapnic reactivity is mediated by NO. Although the role of NO is a possibility based on this information, we acknowledge that this suggestion is purely speculative because we did not measure systemic or cerebrovascular NO.
Cerebral blood flow and its reactivity during exercise
Despite some indication of an elevated resting MCAv following exercise training, the MCAv response to exercise was unchanged, showing a 10–15 % increase. PETCO2 was elevated during exercise but was lower at both 30 and 70 % HRR (post-training) when compared with pre-training; however, this was also accompanied by a reduced resting PETCO2. Nevertheless, the overall observation is a relatively unchanged cerebrovascular response to sub-maximal exercise following training; thus, it seems that the control of CBF during exercise is maintained or even elevated with both increasing age and fitness.
Similar to pre-training, cerebrovascular reactivity was increased during sub-maximal exercise in both young and older individuals, indicating that the improved cerebrovascular control at rest is also apparent during exercise. This finding seems likely since the mechanisms responsible for the increased cerebrovascular reactivity at rest (i.e. potentially NO) following training should still be apparent during exercise. Although the mechanisms are unknown, it may reflect training/exercise-induced alterations in cerebral metabolism, which apart from PaCO2 is the most potent regulator of CBF. Whilst our findings are encouraging, we acknowledge that the extent of adaptation in reactivity across this 12-week intervention is small and may have a limited physiological or clinical relevance. Nevertheless, the findings were evident despite the improvements in aerobic fitness also being modest (6 % mean increase in V̇ O2 max) in this training study. Whether longer term or more intensive exercise might help improve CBF by the extent seen cross-sectionally for aerobically fit young (~12 %, ~10 cm s−1) and older (~20 %, ~10 cm s−1) adults remains unknown. Future studies might also quantify the ‘time course’ of such changes in MCAv and reactivity, as well as concomitant changes in autoregulation during a prolonged training intervention.
Technical considerations
Although resting MCAv was unchanged following training, when it was corrected for the post-training hypocapnia, a training-induced elevation in MCAv was observed. This was only slightly greater (7 %) than our calculated day-to-day reproducibility of the MCAv technique (5.4 % older, 6.1 % young); therefore, the observed 7 % higher MCAv post-training may be due, in part, to day-to-day variation. We attempted to reduce this error as much as possible by ensuring that the MCAv signal was obtained by the same experimenter throughout the study. Although the operator was aware of the depth and gain of the Doppler settings from the baseline (pre-training) testing session, they were not aware of the pre-training MCAv value during the post-training testing session. The reasons for this reduction in PETCO2 following training are unclear. Alveolar ventilation (and its components, including chemoreflex control) was not measurably altered following training. Methodological issues might explain this reduction, yet this seems unlikely as the same gas analysers were used throughout the training study and were always calibrated with a 5 % (±0.2 %) CO2 gas mixture. It therefore seems most likely that this reduction in PETCO2 represented a normal day-to-day variation. Overall, further assessment of the effect of longitudinal exercise training on MCAv is warranted in a larger study population.
Another potential limitation of this study is the absence of a control group. The inclusion of a control group could have been helpful in determining the reason for the post-training reduction in PETCO2, whether due to a training effect or some other reason applicable to both groups (e.g. measurement error or seasonal effects). Nevertheless, it was felt that by ensuring participants were fully familiarised to the testing protocol before the main data collection period, we would be able to confidently assume that any differences following 12 weeks of training would be primarily a result of the training. In addition, all measures were deemed to be relatively insensitive to any placebo/expectation effects of having knowingly participated in a training study. All measures were reflective of actual physiological, rather than perceptual stress. Finally, calibration errors were considered improbable because the researchers were experienced in these procedures and the reactivity testing and calibrations used multiple gas cylinders both before and after the training intervention.
In summary, in addition to showing that age had no effect on cerebrovascular reactivity at rest or during exercise, we have revealed that cerebrovascular reactivity to hypercapnia (and possibly also resting MCAv) was increased following 12 weeks of aerobic-based exercise training in both young and older individuals. This finding is important as it (1) indicates that healthy older age does not compromise cerebrovascular function at rest or during sub-maximal exercise and (2) provides insight into the relationship between fitness and cerebrovascular disease. This is the first study to demonstrate this significant finding and provides important supporting evidence for the role of aerobic exercise in the improved control of CBF and in the prevention of cerebrovascular disease.
References
Ainslie PN, Duffin J (2009) Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: mechanisms of regulation, measurement, and interpretation. Am J Physiol Regul Integr Comp Physiol 296(5):R1473–95
Ainslie PN et al (2005) Differential responses to CO2 and sympathetic stimulation in the cerebral and femoral circulations in humans. J Physiol 566(2):613–24
Ainslie PN et al (2007) Early morning impairment in cerebral autoregulation and cerebrovascular CO2 reactivity in healthy humans: relation to endothelial function. Exp Physiol 92(4):769–77
Ainslie PN et al (2008) Elevation in cerebral blood flow velocity with aerobic fitness throughout healthy human ageing. J Physiol 586(16):4005–10
Black JE et al (1990) Learning causes synaptogenesis, whereas motor activity causes angiogenesis, in cerebellar cortex of adult rats. Proc Natl Acad Sci U S A 87(14):5568–72
Boutcher SH, Stein P (1995) Association between heart rate variability and training response in sedentary middle-aged men. Eur J Appl Physiol Occup Physiol 70(1):75–80
Buijs PC et al (1998) Effect of age on cerebral blood flow: measurement with ungated two-dimensional phase-contrast MR angiography in 250 adults. Radiology 209(3):667–74
Clarkson P et al (1999) Exercise training enhances endothelial function in young men. J Am Coll Cardiol 33(5):1379–85
Colcombe SJ et al (2003) Aerobic fitness reduces brain tissue loss in aging humans. J Gerontol A Biol Sci Med Sci 58(2):M176–180
Colcombe SJ et al (2006) Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Sci Med Sci 61(11):1166–70
Davis SM et al (1983) Cerebral blood flow and cerebrovascular CO2 reactivity in stroke-age normal controls. Neurology 33(4):391–9
de la Torre JC (2010) Vascular risk factor detection and control may prevent Alzheimer's disease. Ageing Res Rev 9(3):218–25
Demirkaya S et al (2008) Normal blood flow velocities of basal cerebral arteries decrease with advancing age: a transcranial Doppler sonography study. Tohoku J Exp Med 214(2):145–9
Ding YH et al (2006) Cerebral angiogenesis and expression of angiogenic factors in aging rats after exercise. Curr Neurovas Res 3(1):15–23
Endres M et al (2003) Mechanisms of stroke protection by physical activity. Ann Neurol 54(5):582–90
Fisher JP et al (2008) Regulation of middle cerebral artery blood velocity during dynamic exercise in humans: influence of aging. J Appl Physiol 105(1):266–73
Galvin SD et al (2010) Effects of age and coronary artery disease on cerebrovascular reactivity to carbon dioxide in humans. Anaesth Intensive Care 38(4):710–7
Gertz K et al (2006) Physical activity improves long-term stroke outcome via endothelial nitric oxide synthase-dependent augmentation of neovascularization and cerebral blood flow. Circ Res 99(10):1132–40
Green DJ et al (2004) Effect of exercise training on endothelium-derived nitric oxide function in humans. J Physiol 561(Pt 1):1–25
Grolimund P, Seiler RW (1988) Age dependence of the flow velocity in the basal cerebral arteries—a transcranial Doppler ultrasound study. Ultrasound Med Biol 14(3):191–8
Gur AY, Bova I, Bornstein NM (1996) Is impaired cerebral vasomotor reactivity a predictive factor of stroke in asymptomatic patients? Stroke 27(12):2188–90
Heckmann JG et al (2003) Delayed cerebrovascular autoregulatory response to ergometer exercise in normotensive elderly humans. Cerebrovas Dis 16(4):423–9
Hellstrom G et al (1996) Carotid artery blood flow and middle cerebral artery blood flow velocity during physical exercise. J Appl Physiol 81(1):413–8
Hooker SP et al (2008) Cardiorespiratory fitness as a predictor of fatal and nonfatal stroke in asymptomatic women and men. Stroke 39(11):2950–7
Hopkins WG (2000) Measures of reliability in sports medicine and science. Sports Med 30(1):1–15
Ito H et al (2002) Effect of aging on cerebral vascular response to PaCO2 changes in humans as measured by positron emission tomography. J Cereb Blood Flow Metab 22(8):997–1003
Ivey FM et al (2011) Improved cerebral vasomotor reactivity after exercise training in hemiparetic stroke survivors. Stroke 42(7):1994–2000
Jorgensen LG et al (1992) Middle cerebral artery flow velocity and blood flow during exercise and muscle ischemia in humans. J Appl Physiol 72(3):1123–32
Kastrup A et al (1998) Changes of cerebrovascular CO2 reactivity during normal aging. Stroke 29(7):1311–4
Kingwell BA et al (1997) Four weeks of cycle training increases basal production of nitric oxide from the forearm. Am J Physiol Heart Circ Physiol 272(3 Pt 2):H1070–7
Krejza J et al (1999) Transcranial color Doppler sonography of basal cerebral arteries in 182 healthy subjects: age and sex variability and normal reference values for blood flow parameters. AJR Am J Roentgenol 172(1):213–8
Lavi S et al (2006) Impaired cerebral CO2 vasoreactivity: association with endothelial dysfunction. Am J Physiol Heart Circ Physiol 291(4):H1856–61
Lee IM, Paffenbarger RS Jr (1998) Physical activity and stroke incidence: the Harvard Alumni Health Study. Stroke 29(10):2049–54
Linkis P et al (1995) Dynamic exercise enhances regional cerebral artery mean flow velocity. J Appl Physiol 78(1):12–6
Liu Y et al. (2011) Arterial spin labeling MRI study of age and gender effects on brain perfusion hemodynamics. Magn Reson Med
Llorens-Martin M, Torres-Aleman I, Trejo JL (2010) Exercise modulates insulin-like growth factor 1-dependent and -independent effects on adult hippocampal neurogenesis and behaviour. Mol Cell Neurosci 44(2):109–17
Markus HS (2004) Cerebral perfusion and stroke. J Neurol Neurosurg Psychiatry 75(3):353–61
Markus H, Cullinane M (2001) Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain 124(Pt 3):457–67
Marsden KR et al. (2011) Aging blunts hyperventilation-induced hypocapnia and reduction in cerebral blood flow velocity during maximal exercise. Age (Dordr)
Moraine JJ et al (1993) Relationship of middle cerebral artery blood flow velocity to intensity during dynamic exercise in normal subjects. Eur J Appl Physiol Occup Physiol 67(1):35–8
Ogoh S, Ainslie PN (2009) Cerebral blood flow during exercise: mechanisms of regulation. J Appl Physiol 107(5):1370–80
Ogoh S et al (2005) Middle cerebral artery flow velocity and pulse pressure during dynamic exercise in humans. Am J Physiol Heart Circ Physiol 288(4):H1526–31
Ogoh S et al (2008) Interaction between the ventilatory and cerebrovascular responses to hypo- and hypercapnia at rest and during exercise. J Physiol 586(Pt 17):4327–38
Ogoh S, Ainslie PN, Miyamoto T (2009) Onset responses of ventilation and cerebral blood flow to hypercapnia in humans: rest and exercise. J Appl Physiol 106(3):880–6
Peebles K et al (2007) Human cerebrovascular and ventilatory CO2 reactivity to end-tidal, arterial and internal jugular vein PCO2. J Physiol 584(1):347–57
Querido JS, Sheel AW (2007) Regulation of cerebral blood flow during exercise. Sports Med 37(9):765–82
Rasmussen P et al (2006) Enhanced cerebral CO2 reactivity during strenuous exercise in man. Eur J Appl Physiol 96(3):299–304
Reich T, Rusinek H (1989) Cerebral cortical and white matter reactivity to carbon dioxide. Stroke 20(4):453–7
Rhyu IJ et al (2010) Effects of aerobic exercise training on cognitive function and cortical vascularity in monkeys. Neuroscience 167(4):1239–48
Schwertfeger N et al (2006) Cerebrovascular reactivity over time course in healthy subjects. J Neurol Sci 249(2):135–9
Seifert T et al (2010) Endurance training enhances BDNF release from the human brain. Am J Physiol Regul Integr Comp Physiol 298(2):R372–7
Silvestrini M et al (2000) Impaired cerebral vasoreactivity and risk of stroke in patients with asymptomatic carotid artery stenosis. JAMA 283(16):2122–7
Swain RA et al (2003) Prolonged exercise induces angiogenesis and increases cerebral blood volume in primary motor cortex of the rat. Neuroscience 117(4):1037–46
Thomas KN et al (2009) Initial orthostatic hypotension is unrelated to orthostatic tolerance in healthy young subjects. J Appl Physiol 107(2):506–17
Thompson PD et al (2001) The acute versus the chronic response to exercise. Med Sci Sports Exerc 33(6 Suppl):S438–45, discussion S452-3
Tinken TM et al (2008) Time course of change in vasodilator function and capacity in response to exercise training in humans. J Physiol 586(Pt 20):5003–12
Tsuda Y, Hartmann A (1989) Changes in hyperfrontality of cerebral blood flow and carbon dioxide reactivity with age. Stroke 20(12):1667–73
Wuyam B et al (1995) Imagination of dynamic exercise produced ventilatory responses which were more apparent in competitive sportsmen. J Physiol 482(Pt 3):713–24
Yamaguchi F et al (1979) Normal human aging and cerebral vasoconstrictive responses to hypocapnia. J Neurol Sci 44(1):87–94
Yamamoto M et al (1980) Aging and cerebral vasodilator responses to hypercarbia: responses in normal aging and in persons with risk factors for stroke. Arch Neurol 37(8):489–96
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Murrell, C.J., Cotter, J.D., Thomas, K.N. et al. Cerebral blood flow and cerebrovascular reactivity at rest and during sub-maximal exercise: Effect of age and 12-week exercise training. AGE 35, 905–920 (2013). https://doi.org/10.1007/s11357-012-9414-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-012-9414-x