Abstract
Purpose
We designed this retrospective study to identify predictive value of prognostic nutritional index (PNI) and albumin–globulin ratio (AGR) in nasopharyngeal cancer patients (NPC).
Methods
95 non-metastatic NPC patients were included in the study. AGR was calculated as the absolute counts between albumin and globulin measurements. (Globulin values were obtained via excluding albumin counts from total protein counts). PNI was calculated using the following formula: [10 × serum albumin value (g/dL) + 0.005 × total lymphocyte count] in the peripheral blood (per mm3).
Results
The statistically significant cutoff value of PNI was identified as 45.45 (area under the curve (AUC): 0.636, p = 0.03) for overall survival. The 5-year OS rate for patients with PNI ≤ 45.45 and PNI > 45.45 were 52.9% and 79.0%, respectively. There were statistically significant difference between groups (p = 0.03).The statistically significant cutoff value of AGR was identified as 1.19 (AUC: 0.689, p < 0.01) for overall survival. The 5-year OS rate for patients with AGR ≤ 1.19 and AGR > 1.19 were 57.7% and 82.0%. There were statistically significant differences between the groups (p = 0.04). 5-year OS rate was 42.9% in the high-risk group (low-PNI and low-AGR patients), it was 80.3% in the intermediate group (low PNI and high AGR or high PNI and low AGR) and it was 80.9% in low-risk group (high PNI and high AGR) (p = 0.004). In the multivariate analysis, age and PNI were independent prognostic factors for poorer OS (HR 2.70, 95% CI 1.091–6.719, p = 0.32 and HR 2.44, 95% CI 1.009–5.940, p = 0.48).
Conclusions
Low PNI is independent prognostic factor for poorer OS. Patients with low-PNI and low-AGR have worse survival than patients with high PNI and high AGR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is the common malignancies in Southeast Asia [1], and treatment of choice is radiotherapy-based combination treatments [2]. In the recent years, intensity-modulated radiotherapy (IMRT) has replaced two-dimensional conventional radiotherapy as the first choice for the treatment of NPC. So many studies have shown that the 5-year loco-regional control rate has increased substantially to reach approximately 90% in NPC patients treated by IMRT with or without chemotherapy [3,4,5], but the distant metastasis rate remains high (14–26%) with no clear improvement in OS (77–84%) [6].
Malnutrition is frequently observed at the time of diagnosis in head and neck cancer due to dysphagia, anorexia and mechanical obstruction. In the literature, malnutrition has been estimated in 30–50% in patients with head and neck cancer [7]. Malnutrition may causes immuno-depression [8], reduced vitality, reduced resistance to the disease and decrease wound healing [9]. Recently, so many studies have focused on influence of nutrition and immune status on the prognosis of cancer patients. Prognostic nutritional index (PNI) was defined as first by Onedera et al., gastrointestinal cancer patients [10]. PNI is calculated based on the serum albumin concentration and total lymphocyte count in the peripheral blood and it is also known to be an indicator of both the nutritional and immune status of cancer. Many studies have shown that the PNI could be used as a prognostic marker in patients with various malignancies consisting of small cell lung cancer [11], renal cell carcinoma [12] and digestive tract tumors [13, 14]. However, the predictive value of PNI has rarely been investigated in NPC patients. The heterogeneity of patients with different risk factors in the same stage has limited the ability of TNM staging to distinguish patients with different prognoses and make accurate treatment choices. In the last decades, it was suggested that systemic inflammatory response was important prognostic predictive value for overall survival independent of disease stage [15,16,17]. The systemic inflammatory response of patients can be assessed by examining changes in the circulating concentrations of acute-phase reactants and hematological cellular components [18]. The decrease in albumin synthesis during inflammation can probably be partially ascribed to the effect of monocyte products such as interleukin-1 (IL-1), interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α). Hypoalbuminemia is frequently observed during acute disease states as albumin is a negative acute-phase protein [19]. In pathological conditions such as sepsis, infection or trauma, or after major surgery, the level of serum albumin is reduced by about 10–15 g/L within 1 week of the event. Cirrhosis, malabsorption syndromes, diabetes mellitus, nutritional deficiencies, increased catabolism, infection, nephrotic syndrome and cancer may cause hypoalbuminemia [19]. Albumin has been widely used to evaluate the nutritional status and to predict the prognosis of cancer patients. Albumin has reported various anticancer capabilities such as managing cell growth and DNA replication, buffering many biochemical alterations, and its antioxidant effects against carcinogens [20]. Malnutrition and inflammation may could prevent the synthesis of albumin. While IL-6 set the regulation of the synthesis of the albumin by the liver cells, the TNF-α regulate the gene transcription of the albumin downwards. In addition, IL-6 can promote to production of globulins. Therefore, albumin–globulin ratio may change due to high levels of globulins [21].
Hypoalbuminemia is an independent predictive prognostic factor of worse overall survival in several types of cancer including ovarian, breast, lung and gastrointestinal additionally NPC. Therefore, albumin deficit is related with poor response to treatment, increased treatment toxicity, worse quality of life [22,23,24,25]. Therefore, identifying other prognostic factors may help select patients who will benefit from more aggressive treatment. We designed this retrospective study in NPC patients who received IMRT (chemoradiotherapy or without) to identify predictive value of pretreatment PNI and AGR.
Materials and methods
Patient’s features
Between 2010 and 2018 years, pathologically diagnosed and non-metastatic NPC patients treated with IMRT were evaluated for this trial, at the Erciyes University Oncology Hospital. 95 of 108 patients were enrolled this trial. All patients were screened in terms of pretreatment complete medical history, physical examination, magnetic resonance imaging (MRI) and computed positron emission tomography (PET-CT) as well as pretreatment complete blood count, hepatic and renal functions as biochemistrical. 95 of 110 patients were eligible and included in the study. The eligibility criteria were: (1) patients with age of 16 years and above; (2) primary diagnosed NPC patients with biopsy-confirmed World Health Organization (WHO) type II or III; (3) treated with definitive intensity-modulated radiotherapy (IMRT) at our hospital; (4) complete pre- and post-treatment data. The exclusion criteria were: (1) the presence of distant metastasis at diagnosis; (2) underwent neck nodal dissection prior to radiotherapy; (3) irradiation of head and neck before or recurrence in nasopharyx; (4) confirmed hematological disorders or even with a single episode of systemic infection before or at diagnosis because that effect to PNI and AGR; (5) Karnofsky Performance Status (KPS) < 70; (6) confirmed diseases with high or low albumin–globulin levels such as immunological disorders, chronic malnutrition, protein-losing enteropathies, several liver (cirrhosis) and kidney (nephritic syndromes) disorders.
This study was conducted in compliance with the postulates of Declaration of Helsinki and was approved by local ethical committee and all patients provided written informed consent.
Clinical data collection
Pretreatment peripheral blood count and biochemistry tests were collected and data from the most recent tests in a week before the treatment were based on. In according to these blood checks and clinical symptoms, infection statement was excluded in patients. Biochemistrical and hematological parameters were collected from patient’s charts, which were recorded by medical staff during the treatment. Pretreatment biochemistry values of albumin (ALB), alkaline phosphatase (ALP), lactate dehydrogenase (LDH) were measured using (Roche Hitachi Cobas 8000, Rotkreuz, Switzerland) automatized chemistry analyzer. Hematological values of hemoglobin (hb), lymphocyte (lymp), neutrophil (neu), platelet (plt) were measured using hematology analyzer (Sysmex SE-9000, Kobe, Japan).
Peripheral albumin/globulin ratio (AGR) was calculated as the absolute counts between albumin and globulin measurements. (Globulin values were obtained via excluding albumin counts from total protein counts). PNI was calculated using the following formula: 10 × serum albumin value (g/dL) + 0.005 × total lymphocyte count in the peripheral blood (per mm3).
Clinical staging
Staging was determined by clinical examination of head and neck, naso-endoscopy with direct fiber optic, magnetic resonance imaging (MRI) and positron emission computed tomography (PET-CT). All patients were restaged according to 8th edition of the International Union against Cancer/American Joint Committee on Cancer (UICC/ AJCC) system [26].
Treatment
All patients were treated with definitive chemoradiotherapy. The radiotherapy was given in the form of IMRT with simultaneous integrated boost technique. It was performed in a daily fraction of 1.65–2.12 Gy, 5 days per week for 6–7 weeks. The total radiation dosage was 66 or 70 Gy to primary lesion of nasopharynx (66 Gy for T1–2, 70 Gy for T3–4), 66 or 70 Gy to metastatic lymph nodes of the neck, 60 Gy to the regions of high-risk micro-invasive lymphatic drainage areas (clinical target volume 1, CTV 1) and 54 Gy to low-risk areas (clinical target volume 2, CTV 2). Chemotherapy was started in the first radiation treatment day in the all patients. Cisplatin regimen consists of intravenous infusion of 100 mg/m2 every 3 weeks or 50 mg/m2 intravenous infusions weekly.
Follow-up
Patient follow-up was defined from the first day of treatment to last examination or death. Both MRI and PET-CT was performed to evaluate treatment response on third month after the last treatment day. Treatment response evaluation was made according to Response Evaluation Criteria in Solid Tumors (RECIST criteria) [27]. The response to treatment was classified as complete response (CR), partial response (PR), stable disease (SD) or progression disease (PD). If they were accepted as completed response, they were monitored every 3 months for the first 2 years with MRI and follow-up examinations of patients continued every 6 months thereafter until death. The location of first clinical relapse was accepted as local failure, if relapse side was in nasopharynx. The location of first clinical relapse was accepted as regional failure, if relapse side was in the nodal area. If the relapse side was beyond above-mentioned areas, we accepted it as distant failure. The time to loco-regionally failure (LRRFS) and time to distant failure (DMFS) were calculated from day 1 of treatment until documented treatment failure. Overall survival (OS) was calculated from day 1 of the treatment until death or the date of last follow-up.
Statistical analysis
All data were expressed as means ± SD unless otherwise stated and controlled for normality using Shapiro–Wilk test. A receiver-operating characteristic (ROC) curve analysis was performed to determine the optimal cutoff value. Chi square and Fisher exact tests were used to compare categorical variables such as different age, gender, T stage, N stage, AGR and PNI. To clarify the prognostic factors of survival, a Cox regression model was applied to identify the best predictor variables using univariate and multivariate analysis. The predictors were estimated with relative risk and 95% CI in the regression model. The log-rank test was used for comparing between groups for LRRFS, DMFS and OS. Differences were considered significant at p < 0.05. The statistical analysis of the data was performed using IBM SPSS Statistics 22.0 (IBM Corp., Armonk, New York, USA).
Results
Patient characteristics
The median age was 50 years (range 16–70 years). 28 (29.5%) patients were female while 67 (70.5%) patients were male.Of the 95 patients, 14 (14.7%), 28 (29.5%), 20 (21.1%) and 33 (34.7%) had T1, T2, T3, and T4 stage cancers, respectively. Of the 95 patients, 19 (20%), 28 (29.5%), 36 (37.9%) and 12 (12.6%) had N0, N1, N2, and N3 stage cancers, respectively. Of the 95 patients, 18 (18.9%), 34 (35.8%) and 43 (45.3%) had stage II, stage III and stage IVA cancers, respectively. The median follow-up time was 41.0 months (range 2–91 months). At the date of last follow-up, 24 (25.3%) patients had loco-regional recurrence, 17 (17.9%) patients had distant metastasis, and 21 (22.1%) patients died.
Cutoff values of parameters
The median of PNI was 52.5 (range 34.75–127.5). The statistically significant cutoff value of PNI was identified as 45.45 (area under the curve (AUC): 0.636, p = 0.03) for overall survival. The patients divided two groups (PNI ≤ 45.45 and PNI > 45.45) according to cutoff values. The median of AGR was 1.34 (range 0.26–2.18). The statistically significant cutoff value of AGR was identified as 1.19 (area under the curve: 0.689, p < 0.01) for overall survival. The patients divided two groups (AGR ≤ 1.19 and AGR > 1.19) according to cutoff values. We compared that according to clinical and demographic features such as age, gender, T stage, N stage, socioeconomic level, place of residence, educational level, marital status, smoking habits, exposure to pesticides, TNM stage, loco-regional recurrence and distant metastasis. There were no statistically significant difference between groups in terms of PNI and AGR, but the rate of death was statistical significantly higher in patients with PNI < 45 and AGR < 1.19 (p = 0.01). Patient’s clinical and demographical features are summarized in Table 1.
Survival analysis
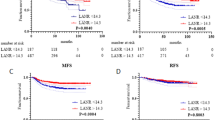
The 5-year loco-regional recurrence-free survival (LRRFS), distant metastasis-free survival (DMFS) and overall survival (OS) rate were 68.5%, 80.5% and 74.6%, respectively. The 5-year DMFS rate for patients with PNI ≤ 45.45 vs. PNI > 45.45 was 71.5% and 80.6%, respectively. There were no statistically significant difference between the groups (p = 0.58). The 5-year LRRFS rate for patients with PNI ≤ 45.45 vs. PNI > 45.45 was 56.4% and 71.4%, respectively. There were no statistically significant difference between the groups (p = 0.26). The 5-year OS rate for patients with PNI ≤ 45.45 vs. PNI > 45.45 was 52.9% and 79.0%, respectively. There were statistically significant differences between the groups (p = 0.03). The 5-year DMFS rate for patients with AGR ≤ 1.19 vs. AGR > 1.19 was 74.3% and 80.2%, respectively. There were no statistically significant differences between the groups (p = 0.71). The 5-year LRRFS rate for patients with AGR ≤ 1.19 vs. AGR > 1.19 was 65.6% and 69.3%, respectively. There were no statistically significant differences between the groups (p = 0.84). The 5-year OS rate for patients with AGR ≤ 1.19 vs. AGR > 1.19 was 57.7% and 82.0%, respectively. There were statistically significant differences between the groups (p = 0.04) (Fig. 1).
Kaplan–Meier curves for patients PNI ≤ 45.45 vs. PNI > 45.45 and AGR ≤ 1.19 vs. AGR > 1.19. a Loco-regional recurrence-free survival between groups for PNI. b Loco-regional recurrence-free survival between groups for AGR. c Distant metastasis-free survival curve between groups for PNI. d Distant metastasis-free survival curve between groups for AGR. e Overall survival curve between groups for PNI. f Overall survival curve between groups for AGR
Univariate and multivariate analyses
In the univariate analysis, gender, T stage, N stage, TNM stage, lymphocyte counts, albumin and AGR were not associated with DMFS, LRRFS and OS (Tables 2, 3). Age (≥ 50 years) (HR 2.77, 95% CI 1.120–6.885, p = 0.02) and low pretreatment PNI (HR 2.53, 95% CI 1.045–6.144, p = 0.04) were found as predictive for only OS, not DMFS and LRRFS. Likewise, in the multivariate analysis, both age and pretreatment PNI were independent prognostic factors for worse OS (HR 2.70, 95% CI 1.091–6.719, p = 0.32 and HR 2.44, 95% CI 1.009–5.940, p = 0.48, respectively) (Table 3).
Combined prognostic value of PNI and AGR
The patients were assessed by dividing into the three groups for the combined prognostic value of pretreatment PNI and AGR: with low-PNI and low-AGR patients defined as group high risk, with low-PNI and high-AGR or high-PNI and low-AGR patients defined as intermediated group, with high-PNI and high-AGR patients defined as low-risk group. The data showed high-risk group had the worst overall survival compared with low-risk group and intermediated-risk group. While 5-year OS rate in the high-risk group was 42.9, in intermediate group, it was 80.3% and in low risk group it was 80.9%. Differences between the groups were statistical significantly (for intermediate group vs. high-risk group p = 0.28; for low-risk group vs. high-risk group p = 0.004) (Fig. 2).
Discussion
Different treatment outcomes of patients at the same TNM stage are required by the investigators to identify other prognostic factors.Therefore, different biological and hematological markers were studied which are related to either tumour or host. The serum albumin concentration is organized by nutritional status and immuno-response of organism. In addition, albumin organizes cellular growth and DNA stabilization. It works like buffer in biochemical reactions. Besides, it keeps up regularity of sex hormones against cancer. Low serum albumin level is related to poor prognosis and worse survival in patients with cancer [25]. Additionally lymphocytes are an important part of adaptive immunity, it is called as cellular immunity, which battles against cancer cells. It was reported that lymphocyte infiltration is associated with anti-tumour immunity. Therefore, low lymphocyte levels indicate that poor immuno-response and that can be related to worse prognosis. On the contrary, in the studies, they were associated with better prognosis and immuno-response that include high lymphocyte levels [28]. PNI which is one of these markers, first was used to asses postoperative complications in patients with gastrointestinal surgery in 1984 by Onodera et al. [10] Until the recent years, the value of the use of PNI in the oncology practices has been neglected but studies in the last years have shown that PNI is closely to associated with survival in many types of cancer [11,12,13,14]. However, there are limited trials in patients with NPC, which were related to PNI. The cutoff value of PNI is in the range 40 and 52 in the literature. We found the statistically significant cutoff value of PNI as 45.45 for OS, but no relation was found in terms of DMFS and LRFS. There have been 7 published studies in the literature for PNI in NPC patients. One of them is prospective and others are retrospective trials. In addition, one of these six retrospective studies has been performed in patients with metastatic NPC. In two studies (one of them prospective), studies have not been designed to predict PNI and survival, and these trials had been intended to evaluate toxicity [7, 29]. Low PNI level was found as predictive in terms of worse DMFS in the four studies [30,31,32,33]. Similarly, three of these studies reported that NPC patients with low PNI had poor OS than patients with high PNI [30,31,32]. In this current retrospective study, we found that patients with low PNI have shorter survival (55.52 months) than patients with high PNI (77.94 months). According to this current study, pretreatment low PNI (< 45.45) is independent prognostic factor for OS. However, prediction of prognosis between PNI and DMFS has not been found, in contrast to studies in the literature.
There are two published studies in the literature for AGR in NPC.One of these trials, Du et al. showed that patients with low AGR had shorter survival than patients with high AGR in terms of OS, DMFS and PFS [34]. In another trial with Li A et al. reported that low AGR was predictive for distant metastasis [35]. In this current trial, we observed that between groups for AGR values > 1.19 and < 1.19, there were statistically significant difference for OS (p = 0.04), but there was no statistically significant difference between the groups in terms of DMFS and LRFS. Especially, both in the low AGR and low PNI group had worst overall survival. According to this current outcome, pretreatment determination of AGR and PNI levels is very important for NPC patients. In this group, patients with both nutritional and immunological conditions were supported carefully.
Conclusion
We reported that pretreatment low PNI is independent prognostic factor for poorer OS. Patients with low PNI and low AGR have worse survival than patients with high PNI or high AGR. Therefore, pretreatment evaluation of PNI and AGR may be an important parameter who chose different treatment strategy. Finally, we need prospective randomized studies to determine the importance of PNI and AGR in NPC patients.
References
Wee JT, Ha TC, Loong SL, Qian CN (2010) Is nasopharyngeal cancer really a “Cantonese Cancer”? Chin J Cancer 29:517–526
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and future of TNM. Ann Surg Oncol 17:1471–1474
Su SF, Han F, Zhao C et al (2011) Treatment outcomes for different subgroups of nasopharyngeal carcinoma patients treated with intensity-modulated radiation therapy. Chin J Cancer 30:565–573
Lee AW, Ng WT, Chan LL et al (2014) Evolution of treatment for nasopharyngeal cancer-success and setback in the intensity-modulated radiotherapy era. Radiother Oncol 110:377–384
Wang W, Feng M, Fan Z, Li J, Lang J (2014) Clinical outcomes and prognostic factors of 695 nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy. BioMed Res Int 2014:814948
Li AC, Xiao W-W, Shen GZ et al (2015) Distant metastasis risk and patterns of nasopharyngeal carcinoma in the era of IMRT: long-term results and benefits of chemotherapy. Onco-target 6:24511–24521
Kono T, Sakamoto K, Shinden S, Ogawa K (2017) Pre-therapeutic nutritional assessment for predicting severe adverse events in patients with head and neck cancer treated by radiotherapy. Clin Nutr 36:1681–1685
Chandra RK (1997) Nutrition and the immune system: an introduction. Am J Clin Nutr 66:460–463
Magnano M, Mola P, Machetta G et al (2015) The nutritional assessment of head and neck cancer patients. Eur Arch Otorhinolaryngol 272:3793–3799
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon GekaGakkaiZasshi 85:1001–1005
Hong S, Zhou T, Fang W et al (2015) The prognostic nutritional index (PNI) predicts overall survival of small-cell lung cancer patients. Tumor Biol 36:3389–3397
Hofbauer SL, Pantuck AJ, de Martino M et al (2015) The preoperative prognostic nutritional index is an independent predictor of survival in patients with renal cell carcinoma. Urol Oncol 33(2):e1–7
Ikeya T, Shibutani M, Maeda K et al (2015) Maintenance of the nutritional prognostic index predicts survival in patinets with unresectable metastatic colorectal cancer. J Cancer Res Clin Oncol 141:307–313
Jiang N, Deng JY, Ding XW et al (2014) Prognostic nutritional index predicts postoperative complications and long-term outcomes of gastric cancer. World J Gastroenterol 20:10537–10544
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12:223–226
Muliawati Y, Haroen H, Rotty LW (2012) Cancer anorexia-cachexia syndrome. Acta Med Indones 44:154–162
Lis CG, Gupta D, Lammersfeld CA, Markman M, Vashi PG (2012) Role of nutritional status in predicting quality of life outcomes in cancer- a systematic review of the epidemiological literature. Nutr J 11:27
Proctor MJ, Morrison DS, Talwar D et al (2011) The comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer 47:2633–2641
Gatta A, Verardo A, Bolognesi M (2012) Hypoglobulinemia. Intern Emerg Med 7:193–199
Zhou T, Yu ST, Chen WZ et al (2019) Pretreatment albumin globulin ratio has a superior prognostic value in laryngeal squamous cell carcinoma patients: a comparison study. J Cancer 10:594–601
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Ramos Chaves M, Boleo-Tome C, Monterio-Grillo I, Camilo M, Ravasco P (2010) The diversity of nutritional status in cancer: new insights. Oncologist 15:523–530
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
Lien YC, Hsieh CC, Wu YC et al (2004) Preoperative serum albumin level is a prognostic indicator for adenocarcinoma of the gastric cardia. J Gastrointest Surg 8:1041–1048
Gupta D, Lis CG (2010) Pretreatment serum albumin is a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 9:69
Pan JJ, Ng WT, Zong JF et al (2016) Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer 122:546–558
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
He JR, Shen GP, Ren ZF et al (2012) Pretreatment levels of peripheral neutrophils and lymphocytes as independent prognostic factors in patients with nasopharyngeal carcinoma. Head Neck 34:1769–1776
Jin T, Li KX, Li PJ et al (2017) An evaluation of nutrition intervention during radiation therapy in patients with locoregionally advanced nasopharyngeal carcinoma. Oncotarget 8:83723–83733
Du XJ, Tang LL, Mao YP et al (2015) Value of prognostic nutritional index and weight loss in predicting metastasis and long-term mortality in nasopharyngeal carcinoma. J Transl Med 13:364
Oei RW, Ye L, Kong F et al (2018) Prognostic value of inflammation-based prognostic index in patients with nasopharyngeal carcinoma: a propensity score matching study. Cancer Manag Res 10:2785–2797
Miao J, Xiao W, Wang L, Han F, Wu H, Deng X (2017) The value of the prognostic nutritional index (PNI) in predicting outcomes and guiding the treatment strategy of nasopharyngeal carcinoma (NPC) patients receiving intensity-modulated radiotherapy (IMRT) with or without chemotherapy. J Cancer Res Clin Oncol 143:1263–1273
Yang L, Xia L, Wang Y et al (2016) Low prognostic nutritional index (PNI) predicts unfavorable distant metastasis-free survival in nasopharyngeal carcinoma: a propensity score-matched analysis. PLoS ONE 11(7):e0158853
Du XJ, Tang LL, Mao YP et al (2014) The pretreatment albumin to globulin ratio has predictive value for long-term mortality in nasopharyngeal carcinoma. PLoS ONE 9(4):e94473
Li AC, Xiao WW, Wang L et al (2015) Risk factors and prediction-score model for distant metastasis in nasopharyngeal carcinoma treated with intensity-modulated radiotherapy. Tumor Biol 36:8349–8357
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gundog, M., Basaran, H. Pretreatment low prognostic nutritional index and low albumin–globulin ratio are predictive for overall survival in nasopharyngeal cancer. Eur Arch Otorhinolaryngol 276, 3221–3230 (2019). https://doi.org/10.1007/s00405-019-05595-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05595-2