Abstract
Purpose
To investigate the correlation between the time to locoregional recurrence and survival in T1–T2 oropharyngeal squamous-cell carcinoma (OPSCC) patients.
Methods
A retrospective, single-site study of patients with T1–T2 OPSCC treated with curative intent between 2000 and 2015 who had a locoregional recurrence without distant metastases. Patients without a disease-free interval (i.e., persistent macroscopic disease after the end of treatment and a time to locoregional recurrence of less than 3 months) were excluded. The endpoint considered was overall survival (OS).
Results
Out of 602 T1–T2 OPSCC patients, 121 patients had a locoregional recurrence and they were, hence, analyzed. All of the patients were heavy-smokers, with a consumption of more than 20 pack-years. The recurrence was local in 59.5%, regional in 27.3%, and both local and regional in 13.2% of the patients. The median time to locoregional recurrence and median OS was 15 months and 44 months, respectively. The time to locoregional recurrence was correlated with OS (p < 0.0001). In multivariate analyses, factors associated with survival were an initial N0–N2a versus N2b–N3 nodal staging and a 12-month threshold for the time to locoregional recurrence.
Conclusions
Locoregional control in T1–T2 OPSCC is not only a qualitative prognostic factor but also a quantitative prognostic factor of survival. A time to locoregional recurrence of less than 12 months was correlated with an unfavorable prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous-cell carcinoma is the sixth most common cancer worldwide, with an incidence of 650,000 new cases per year [1]. Among the various forms of head and neck cancer, oropharyngeal squamous-cell carcinoma (OPSCC) is the most frequent site for pharyngeal cancer [2]. Due to the high density of lymphatic vascularisation and frequent bilateral drainage at oropharyngeal subsites, OPSCCs have a high tropism for lymphovascular invasion and regional metastasis. Therefore, neck lymph-node invasion at the initial presentation is more frequent than with localizations such as oral cavity and larynx neoplasms, and it leads to the neck mass being a more of a complaint than a sore throat [3]. This is even more significant in papillomavirus-related OPSCC than in tobacco-related cancer, and it explains why T1–T2 OPSCCs are the most common local stage at diagnosis, accounting for up to 87% of cases in some series [3]. Current treatments comprise concurrent chemoradiotherapy and primary surgery with adjuvant postoperative radiotherapy, according to surrounding tissue invasion and local standards [4]. As adverse pathological features such as lymph-node extracapsular extension in OPSCC are common, the addition of chemotherapy to postoperative concurrent radiotherapy is often called for [4]. There has, therefore, been a historical paradigm shift towards concurrent chemoradiotherapy in primary treatment to limit the toxicity of cumulative treatments, with surgery being used in salvage treatment of locoregional failures [5]. However, when it is feasible, salvage surgery for locoregional failure results in a high rate of postoperative complications, ranging from 27 to 53%, and limited functional results with 40–56% persistent enteral nutrition at 1 year [6,7,8,9]. Moreover, due in part to the limited feasibility of such complex procedures, 5-year OS rates in OPSCC patients with locoregional recurrence have been reported to range from 13 to 28% [10, 11]. Individual prognostic criteria are key factors that assist with the multidisciplinary team decision-making process, and they have been described in numerous retrospective studies [6, 9, 11,12,13,14,15].
Although the impact of the time to locoregional recurrence has been explored in global cohorts of head and neck cancer patients and in other head and neck localizations such as laryngeal cancer, it has not been assessed to date in T1–T2 OPSCC patients [16, 17]. The aim of our study was, hence, to investigate the correlation between the time to locoregional recurrence and survival in T1–T2 OPSCC patients. Our initial hypothesis was that locoregional control is not only a qualitative prognostic factor but also a quantitative prognostic factor of survival in patients with this more frequent presentation.
Materials and methods
This study was undertaken once approval was received from the local Research Committee. We retrospectively reviewed data of patients treated between 2000 and 2015 at our Cancer Centre for an oropharyngeal squamous-cell carcinoma (OPSCC) who were stages T1 or T2 according to the seventh edition of the American Joint Committee on Cancer. The patients included in this study met the following criteria: no distant metastases at presentation; no previous history of head and neck cancer; primary treatment with curative intent; a histologically proven locoregional recurrence, and without metastasis at the time of diagnosis of the recurrence. Patients with persistent macroscopic disease after the end of the treatment and with a time to locoregional recurrence of less than 3 months were excluded from the analysis due to the lack of disease-free interval.
Statistical design and analysis
Locoregional recurrence was defined as disease recurrence at the primary tumor site and/or a neck lymph node. Persistent disease after the end of the treatment was excluded. Time to locoregional recurrence (DLR) was defined as the time between the multidisciplinary consultation prior to the beginning of the treatment and the diagnosis of a locoregional recurrence. The endpoint considered was overall survival (OS), defined as the time from the initial multidisciplinary consultation to death or the last follow-up.
The descriptive analysis characterized the studied population in terms of frequencies, percentages, medians, and ranges. Correlations in patients followed until death were assessed with Spearman’s test. We evaluated the association between DLR and survival by testing DLR cut-off values of 6, 12, and 24 months. Patients were divided into two groups for each value: patients with a DLR greater than the tested cut-off value and patients with a DLR equal to or less than the cut-off value. The Kaplan–Meier survival curves of the two groups for each test were compared with the log-rank test. The patient, tumor, and treatment characteristics were assessed for their influence on the endpoint using Kaplan–Meier estimates and the log-rank test for the equality of survivor functions. Variables with p values < 0.2 were included in a multivariate analysis using a Cox proportional hazard model. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 23 software (IBM Corp., Armonk, NY, USA). The reported p values were two-sided when available, and p values below 0.05 were considered significant.
Results
Between 2000 and 2015, there were 2,057 patients who presented with an OPSCC at our head and neck oncology department, of whom 602 where stage T1 or T2 that was treated with curative intent. There were 121 patients who met the inclusion criteria and who were hence included in the analysis as they had a locoregional recurrence after a disease-free interval and without concurrent distant metastases, 98 of whom were followed until death. The characteristics of the patients, initial tumor staging, initial treatment strategies, and the patterns of recurrence are presented in Table 1. Notably, all of the patients in our series were heavy-smokers with a consumption of more than 20 pack-years. Determination of p16 expression by immunohistochemistry has been performed at our Cancer Centre since 2012 for all oropharyngeal tumors, with determination of the presence of viral DNA using in-situ hybridization in p16-positive tumors. Retrospective p16 expression based on immunohistochemical staining had been performed for a limited number of tumors originating from lymphoid oropharyngeal sites, i.e., the tonsils and the base of the tongue. Therefore, only 36 patients had been analyzed for tumor p16 status: 8 were p16-positive, of whom 6 were positive for viral DNA. Nine patients received induction chemotherapy for N3 disease prior to definitive treatment, which was primary surgery and postoperative radiotherapy for three patients and definitive radiotherapy for six patients. For the 121 patients, the recurrence was local in 59.5% of the cases, regional in 27.3%, and both local and regional in 13.2%.
The median durations for locoregional control (LRC) and overall survival (OS) were 15 months and 44 months, respectively. The median survival after locoregional recurrence was 15 months.
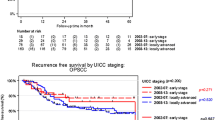
The AJCC/UICC stage prior to the initial treatment influenced OS and LRC. Since we focused our study on T1–2 OPSCC patients, endpoints were associated with the N classification as a surrogate of the global disease stage. The N0–N2a patients had similar OS and LRC rates, and they had better OS and LRC than N2b–N3 patients (p = 0.008 and p = 0.006, respectively). However, in the standard stage stratification, the stage was not a statistically significant factor for OS or LRC (p = 0.078 and 0.185, respectively). Decreased OS or LRC of stages III–IV (locally advanced) as compared to stages I–II (early stage) were not significant (p = 0.069 and p = 0.216, respectively). Yet, as could be expected, stages I–III had similar OS or LRC rates, while stage IV patients had decreased OS and LRC (p = 0.015 and p = 0.032, respectively). Therefore, real-life stratification in T1–2 OPSCC in our experience was not between early stage versus locally advanced, but between stages I–III versus stage IV. When looking only at the N classification, real-life stratification was between N0–N2a versus N2b–N3.
Correlation between the DLR and OS was tested in the 98 patients who were followed until death. OS correlated strongly with the DLR (r = 0.77, p < 0.0001, Fig. 1). A significant difference in OS was associated with a DLR cut-off value of 12 months (p < 0.0001, Fig. 2). Of note, a DLR cut-off value of 6 months did not correlate with OS (p = 0.164). The initial treatment with either primary surgery or radiotherapy was not associated with a difference in OS or LRC (p = 0.232 and p = 0.584, respectively). A recurrence at both local and regional sites was not associated with decreased survival compared to recurrence at a single site only (p = 0.195). In multivariate analyses, factors associated with overall survival were an initial N2b–N3 versus N0–N2a nodal staging (p = 0.033, HR 1.655, 95% CI 1.040 to 2.633) and a DLR longer than 12 months (p = 0.001, HR 2.102, 95% CI 1.350 to 3.274).
Kaplan–Meier curves for overall survival of the 121 T1–T2 oropharyngeal squamous-cell carcinoma patients who developed a locoregional recurrence without distant metastases. Cumulative and overall survivals are reported according to a time to locoregional recurrence cut-off of 12 months. The log-rank test was significant (p < 0.0001)
The patients with a time to locoregional recurrence of less than 12 months did not differ from patients with a time to locoregional recurrence longer than 12 months (Fig. 3) in terms of age (p = 0.1475), gender (p = 0.2426), initial T classification (p = 0.1629), initial N classification (p = 0.3055), subsites (p = 0.2784), and patterns of recurrence (p = 0.3354).
Discussion
Our results show that the time to locoregional recurrence correlates with overall survival (OS) in T1–T2 oropharyngeal squamous-cell carcinoma (OPSCC) patients. Thus, we were able to confirm our hypothesis that locoregional control in T1–T2 oropharyngeal squamous-cell carcinoma (OPSCC) is not only a qualitative prognostic factor but also a quantitative prognostic factor of survival, and we found that a cut-off time to locoregional recurrence of 12 months was significant.
Correlation between locoregional control and overall survival in head and neck cancer was first described by Stell et al. in 1991 [16]. Since then, the disease-free interval has been shown to be associated with the outcomes of salvage treatments in series of patients with several head and neck localizations [8, 12,13,14, 17,18,19]. However, very few studies have reported the prognostic importance of the disease-free interval in OPSCC, and to the best of our knowledge, no study to date has addressed this question specifically in T1–T2 OPSCC. This is, nonetheless, a very important issue given the high rate of T1–T2 stage at the initial presentation of OPSCC patients, and the high morbidity and poor outcomes associated with the available salvage treatments in case of locoregional failure of the first treatment, particularly in p16-negative cases. In our study, both nodal staging and a time to locoregional recurrence cutoff of 12 months were associated with a difference in survival. Our cut-off value was comparable to the results of Agra et al. who found that a locoregional control of less than 12 months was a prognostic factor associated with a lower OS in 246 patients after salvage surgery for recurrent oral (n = 176) and oropharyngeal (n = 70) cancer [12]. Most of the patients had advanced stage III/IV disease at presentation by the time of first treatment, but details of the T stage were not reported. In another series, Kostrzewa et al. described the outcomes for 72 recurrent oral or oropharyngeal cancer patients who underwent salvage surgery with free flap reconstruction [8]. Patients with a disease-free interval of less than 6 months had an estimated 5-year survival of 11.4%, compared to a 5-year survival of 54.4% for patients with a disease-free interval between 6 and 24 months and a 5-year survival of 63.8% for patients with a disease-free interval of more than 24 months. Details of the disease staging at the time of the first treatment were not reported either. However, the prognostic influence of the disease-free interval for recurrent oropharyngeal cancer is a very important issue in patients with a T1–T2 primary tumor at the time of the first treatment. Due to the very limited local extensions of the disease in deep soft tissues, the limited local effects of treatments, and the ease of access to the oropharynx for clinical examination, disease persistence or progression after the end of the treatment can be more readily assessed during the early follow-up than for most of T3–T4 tumors. Indeed, most authors have indicated that disease persistence or progression after the end of treatment versus recurrence is a critical factor in predicting salvage treatment outcomes [18]. In a series of 41 patients who underwent salvage oropharyngeal surgery, Zafereo et al. found that the absence of a disease-free interval very much correlated with a worse prognosis [13]. This is consistent with the consensual hypothesis of a correlation with an aggressive phenotype and biological behavior [18]. In our study, we chose to exclude patients without a disease-free interval, only including patients with disease recurrence and not patients with macroscopic disease persistence or progression. Nonetheless, our results confirmed that time to macroscopic recurrence, which is the definition of cancer recurrence, of a probably microscopically persistent disease, is associated with cancer aggressiveness and with consecutive spreading of the disease and patient survival.
While the retrospective nature of our study was not a limitation for the analysis of survival in a single cohort, our study, nonetheless, has a number of limitations that warrant being pointed out. The low number of cases with available p16 status was a limitation, but p16 positivity has already been shown to be between 27 and 40% in France. This is probably due to high tobacco consumption in the general population and, therefore, a persistently high incidence of tobacco-related OPSCC [20]. Even in p16-positive OPSCC patients, smoking history has been shown to be a major prognostic factor and an independent survival predictor with an adverse effect on tumor control in HPV-related patients. In our series, all of the patients were heavy-smokers [21,22,23,24,25]. Another limitation is that we did not analyze salvage treatments. Our main objective, however, was to analyze the impact of the time to locoregional recurrence on survival in a cohort of patients who initially had small primary tumors. Since the time to locoregional recurrence is a follow-up surrogate for tumor aggressiveness, it is not surprising that it correlates with the feasibility of salvage surgery. Due to obvious circular biases, we did not intend to address this issue in our analyses. We believe that this particular issue requires a specific study methodology. Our objective was not to consider salvage treatments after a diagnosis of recurrence but to focus on the prognostic quantitative importance of locoregional control in the initial treatment.
Conclusion
Locoregional control in T1–T2 oropharyngeal squamous-cell carcinoma (OPSCC) is not only a qualitative prognostic factor but also a quantitative prognostic factor of survival. A time to locoregional recurrence of less than 12 months is associated with an unfavorable prognosis.
References
Hunter KD, Parkinson EK, Harrison PR (2005) Profiling early head and neck cancer. Nat Rev Cancer 5(2):127–135. https://doi.org/10.1038/nrc1549
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Khalid MB, Ting P, Pai A, Russo JL, Bakst R, Chai RL, Teng MS, Genden EM, Miles BA (2018) Initial presentation of human papillomavirus-related head and neck cancer: a retrospective review. Laryngoscope. https://doi.org/10.1002/lary.27296
Turner MT, Byrd JK, Ferris RL (2016) Current role of surgery in the management of oropharyngeal cancer. J Oncol Pract 12(11):1176–1183. https://doi.org/10.1200/JOP.2016.015263
Chen AY, Zhu J, Fedewa S (2014) Temporal trends in oropharyngeal cancer treatment and survival: 1998–2009. Laryngoscope 124(1):131–138. https://doi.org/10.1002/lary.24296
Goodwin WJ (2000) Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means?. Laryngoscope 110(93):1–18. https://doi.org/10.1097/00005537-200003001-00001
Agra IM, Carvalho AL, Pontes E, Campos OD, Ulbrich FS, Magrin J, Kowalski LP (2003) Postoperative complications after en bloc salvage surgery for head and neck cancer. Arch Otolaryngol Head Neck Surg 129(12):1317–1321. https://doi.org/10.1001/archotol.129.12.1317
Kostrzewa JP, Lancaster WP, Iseli TA, Desmond RA, Carroll WR, Rosenthal EL (2010) Outcomes of salvage surgery with free flap reconstruction for recurrent oral and oropharyngeal cancer. Laryngoscope 120(2):267–272. https://doi.org/10.1002/lary.20743
Philouze P, Peron J, Poupart M, Pujo K, Buiret G, Ceruse P (2017) Salvage surgery for oropharyngeal squamous cell carcinomas: a retrospective study from 2005 to 2013. Head Neck 39(9):1744–1750. https://doi.org/10.1002/hed.24827
Jayaram SC, Muzaffar SJ, Ahmed I, Dhanda J, Paleri V, Mehanna H (2016) Efficacy, outcomes, and complication rates of different surgical and nonsurgical treatment modalities for recurrent/residual oropharyngeal carcinoma: a systematic review and meta-analysis. Head Neck 38(12):1855–1861. https://doi.org/10.1002/hed.24531
Kao SS, Ooi EH (2018) Survival outcomes following salvage surgery for oropharyngeal squamous cell carcinoma: systematic review. J Laryngol Otol 132(4):299–313. https://doi.org/10.1017/S0022215117000998
Agra IM, Carvalho AL, Ulbrich FS, de Campos OD, Martins EP, Magrin J, Kowalski LP (2006) Prognostic factors in salvage surgery for recurrent oral and oropharyngeal cancer. Head Neck 28(2):107–113. https://doi.org/10.1002/hed.20309
Zafereo ME, Hanasono MM, Rosenthal DI, Sturgis EM, Lewin JS, Roberts DB, Weber RS (2009) The role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx. Cancer 115(24):5723–5733. https://doi.org/10.1002/cncr.24595
Kim J, Kim S, Albergotti WG, Choi PA, Kaplan DJ, Abberbock S, Johnson JT, Gildener-Leapman N (2015) Selection of ideal candidates for surgical salvage of head and neck squamous cell carcinoma: effect of the Charlson-Age Comorbidity Index and oncologic characteristics on 1-year survival and hospital course. JAMA Otolaryngol Head Neck Surg 141(12):1059–1065. https://doi.org/10.1001/jamaoto.2015.2158
Hamoir M, Holvoet E, Ambroise J, Lengele B, Schmitz S (2017) Salvage surgery in recurrent head and neck squamous cell carcinoma: oncologic outcome and predictors of disease-free survival. Oral Oncol 67:1–9. https://doi.org/10.1016/j.oraloncology.2017.01.008
Stell PM (1991) Time to recurrence of squamous cell carcinoma of the head and neck. Head Neck 13(4):277–281
Liu SA, Wong YK, Lin JC, Poon CK, Tung KC, Tsai WC (2007) Impact of recurrence interval on survival of oral cavity squamous cell carcinoma patients after local relapse. Otolaryngol Head Neck Surg 136(1):112–118. https://doi.org/10.1016/j.otohns.2006.07.002
Ho AS, Kraus DH, Ganly I, Lee NY, Shah JP, Morris LG (2014) Decision making in the management of recurrent head and neck cancer. Head Neck 36(1):144–151. https://doi.org/10.1002/hed.23227
Omura G, Saito Y, Ando M, Kobayashi K, Ebihara Y, Yamasoba T, Asakage T (2014) Salvage surgery for local residual or recurrent pharyngeal cancer after radiotherapy or chemoradiotherapy. Laryngoscope 124(9):2075–2080. https://doi.org/10.1002/lary.24695
Lacau St Guily J, Rousseau A, Baujat B, Perie S, Schultz P, Barry B, Dufour X, Malard O, Pretet JL, Clavel C, Birembaut P, Franceschi S, Papillophar G (2017) Oropharyngeal cancer prognosis by tumour HPV status in France: the multicentric Papillophar study. Oral Oncol 67:29–36. https://doi.org/10.1016/j.oraloncology.2017.01.012
Huang SH, Xu W, Waldron J, Siu L, Shen X, Tong L, Ringash J, Bayley A, Kim J, Hope A, Cho J, Giuliani M, Hansen A, Irish J, Gilbert R, Gullane P, Perez-Ordonez B, Weinreb I, Liu FF, O’Sullivan B (2015) Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus-related oropharyngeal carcinomas. J Clin Oncol 33(8):836–845. https://doi.org/10.1200/JCO.2014.58.6412
Liskamp CP, Janssens GO, Bussink J, Melchers WJ, Kaanders JH, Verhoef CG (2016) Adverse effect of smoking on prognosis in human papillomavirus-associated oropharyngeal carcinoma. Head Neck 38(12):1780–1787. https://doi.org/10.1002/hed.24516
Hong AM, Martin A, Chatfield M, Jones D, Zhang M, Armstrong B, Lee CS, Harnett G, Milross C, Clark J, Elliott M, Smee R, Corry J, Liu C, Porceddu S, Rees G, Rose B (2013) Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int J Cancer 132(12):2748–2754. https://doi.org/10.1002/ijc.27956
Maxwell JH, Kumar B, Feng FY, Worden FP, Lee JS, Eisbruch A, Wolf GT, Prince ME, Moyer JS, Teknos TN, Chepeha DB, McHugh JB, Urba SG, Stoerker J, Walline HM, Kurnit DM, Cordell KG, Davis SJ, Ward PD, Bradford CR, Carey TE (2010) Tobacco use in human papillomavirus-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res 16(4):1226–1235. https://doi.org/10.1158/1078-0432.CCR-09-2350
Lin BM, Wang H, D’Souza G, Zhang Z, Fakhry C, Joseph AW, Drake VE, Sanguineti G, Westra WH, Pai SI (2013) Long-term prognosis and risk factors among patients with HPV-associated oropharyngeal squamous cell carcinoma. Cancer 119(19):3462–3471. https://doi.org/10.1002/cncr.28250
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Formal consent for participation has been given by patients.
Rights and permissions
About this article
Cite this article
Caula, A., Boukhris, M., Guerlain, J. et al. Correlation between the duration of locoregional control and survival in T1–T2 oropharyngeal cancer patients. Eur Arch Otorhinolaryngol 276, 1161–1166 (2019). https://doi.org/10.1007/s00405-019-05293-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05293-z