Abstract
Purpose
Adequate iron transportation from the mother across the placenta is crucial for fetal growth and establishing sufficient iron stores in neonates at birth. The past decade has marked significant discoveries in iron metabolism with the identification of new players and mechanisms. Immunohistochemical studies rendered valuable data on the localization of substantial iron transporters on placental syncytiotrophoblasts. However, the function and regulation of maternal-placentofetal iron transporters and iron handling is still elusive and requires more attention.
Methods
A thorough literature review was conducted to gather information about placental iron transfer, the role of regulators and maintenance of iron homeostasis.
Results
The role of classical and new players in maternal-fetal iron transport and the regulation in the placenta has been addressed in this review. Animal and human studies have been discussed. The role of placental iron regulation in thalassemia and hemochromatosis pregnancies has been reviewed.
Conclusions
The current advances that highlight the mechanisms of placental iron regulation and transport in response to maternal and fetal signals have been presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Iron is a primary trace element in many biological processes and homeostasis of iron is tightly balanced as either overload or deficiency has adverse effects. During pregnancy, physiological anemia results from blood volume expansion and increased demands from the growing placenta and fetus. To accommodate these physiological needs in an early gestation phase, a pregnant woman requires an increased iron supply from stores. But many women enter pregnancy with inadequate iron stores. Global estimates show that 33% of non-pregnant women, 40% of pregnant women, and 42% of children are vulnerable to iron deficiency anemia (IDA) [1]. Neurodevelopment deficit, cognitive deficit, delayed behavioral and mental development persist among infants with IDA [2]. In developing countries, iron deficiency in neonates before six months of age indicates that many neonates may not have adequate iron stores at birth [3]. Studies on placental iron transport have produced noticeable results over the past decade, yet substantive and transformative evidence remains elusive. Hence more detailed studies are essential to understand the specific pathways and molecular mechanisms triggered upon iron depletion and its influence on placental iron regulation. This review will discuss how iron is trafficked across the placenta and transported to the fetus at the mother’s expense and the interplay between iron regulators and transporters in the common maternal–placental–fetal pathway.
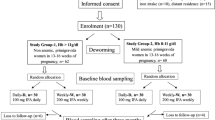
Placenta: maternal–fetal interface
The placenta is a vital interface between mother and fetus which helps transport nutrients, excretion of fetal wastes, prevention of immune rejection, and supports pregnancy by hormone secretions [4, 5]. It is one of the first fetal organs that develop during the implantation period around 6th day after conception. Cytotrophoblast and multinucleated syncytiotrophoblasts are types of trophoblast cells located among mesenchymal cells and vasculature, which collectively form the placenta [6]. At the end of the 5th week of conception, the developing placenta establishes complete maternal–fetal blood circulation and is shown by the developing placenta [7]. At the end of the 12th week of conception, the trophoblast differentiates and forms a villous tree-like structure where the maternal blood flushes into the intervillous space. Villous tree comprises floating villi (FV), drifts into inter villous space and anchoring villi (AV) towards the endometrium. The villous branches bathed in the maternal blood provide more prominent space for trans-placental exchange via active or passive transport where syncytiotrophoblasts lines villi. From this period onwards, the placenta establishes an exchange of nutrients, gases, and waste products between mother and fetus [7]. The placenta takes up an adaptive response in regulating rates of nutrients to be transported [8]. A brief illustration of the placental development is depicted in Fig. 1.
Schematic representation of placental development: Blastocyst implants inside maternal uterus endometrium and its development progress until it reaches the basement membrane. Inner cell mass of blastocyst develops into yolk sac protected by the amniotic sac and chorionic cavity, which allows gas exchange. Trophoblasts (outer layer of blastocyst) proliferate and differentiate into villous cytotrophoblasts, which develop into syncytiotrophoblasts (outer cellular layer) and extravillous cytotrophoblasts (inner cellular layer). Spiral arterioles erode the uterine wall, maternal arteries and enter the intervillous space. The villi-like structures are bathed in maternal blood and provide ample space for trans-placental exchange. Fetal and maternal vascularization completes within early placental development (20th day of conception). Villous branches continue to grow along the expanding intervillous space until the fourth month of gestation
Syncytiotrophoblasts consist of two plasma membranes: microvillus plasma membrane inclined towards maternal circulation and basal plasma membrane facing the stromal core of the villi. The stromal core comprises fetal blood vessels separated by fetal endothelial cells and other cell types, including macrophages and fibroblasts. Nutrients pass through the microvillous plasma membrane and enter fetal circulation after crossing fetal endothelial cells and villous stroma [9]. Several transporters expressed in these plasma membranes regulate maternal–fetal signals. A study on the systems biology approach illustrated the functional gene networks of the placenta, which could help uncover the molecular underpinnings of placental dysfunction with fetal growth abnormalities [10]. Embryonically lethal mouse cell lines derived from CRISPR/Cas9-mediated knockout of trophoblast stem cell line yielded mutant embryos due to molecular defects in placental morphology [11]. These findings suggest that delineating the placenta function helps to understand its association with maternal function and fetal development.
Iron: primary nutrient in pregnancy
Elemental iron (Fe) is essential for many biological processes where it acts as a cofactor for numerous enzymes and other molecules. Dietary iron absorption takes place in the duodenum (1–2 mg/day), where iron is stored in a ferritin reservoir and transported to bone marrow (erythropoiesis), liver (iron storage), reticuloendothelial spleen (iron recycling), and other tissues. Systemic iron homeostasis is tightly regulated by hepcidin, a master regulator synthesized in the liver [12].
Iron has an essential part in placental–fetal development and fetal survival. Failing to meet the demands of such physiological adaptation causes adverse outcomes such as premature birth, low birth weight, cognitive abnormalities in the offspring, and risk of maternal death. Hence, optimal iron availability is crucial and needs to be maintained throughout the gestational period [13]. At birth, the neonate body comprises 1 g of iron derived from the mother, of which 600 mg Fe is from maternal diet and menstrual cessation, and around 400 mg Fe comes from maternal iron stores [14]. However, the mechanism of iron mobilization towards the fetus and iron balance between mother and fetus is not well understood.
Iron demand in pregnancy
Throughout the gestational period, demand for iron is not evenly distributed as there is an increased iron requirement during the second and third trimesters [15]. Bothwell et al. estimated a total need of around 1190 mg Fe during the gestational period as it is necessary for the development of the placental–fetal compartment (360 mg), erythrocyte mass expansion (450 mg), basal losses (230 mg), and compensate the maternal iron loss incurred during delivery (150 mg) [15]. In the first trimester, demand for iron is ~ 0.56 mg/d as menstruation stops and gradually elevates to 4 mg/d and 6 mg/d in subsequent trimesters, respectively [16]. During the 2nd and 3rd trimesters, maternal iron stores are depleted to accommodate fetal growth and survival. Nearly 20% of pregnant women have around 500 mg of iron reserve, which is essential for pregnancy. In contrast, 40% of women of reproductive age proceed to gestation with depleted iron stores [17].
Response to iron supplementation
The World Health Organization (WHO) has suggested the supplementation of 30–60 mg of iron for all reproductive-aged women in all countries. In high-risk populations, prophylaxis for IDA was recommended at a dose of 120 mg/day of elemental iron till hemoglobin level reaches the expected value, after which a regular dose of 30 mg/day was prescribed to prevent anemia [18]. Based on data, 30 mg/day of elemental iron ameliorates maternal iron deficiency and protects their neonates [19]. In contrast, some studies have reported poor outcomes, including no improvement in iron status, increased oxidative stress, gastrointestinal side effects in higher dosage of iron supplementation [20, 21]
WHO conducted a study trial in India revealed that 25% of pregnant women continued to be anemic despite iron supplementation and concluded that iron dosage was not influencing anemia [22]. Data from a national family health survey in India (1998–2016) showed only 30% of pregnant women had responded to iron-folic acid supplementation [23]. Thus, anemia remains a severe health problem in pregnant women despite several measures taken over the last three decades [24].
Iron status during pregnancy
One of the primary maternal adaptations during pregnancy is accelerated erythropoiesis [25]. Erythropoiesis expansion causes an increase in red blood cell mass and plasma volume during the second and third trimesters and peaks at term owing to physiological anemia [26]. Maternal iron status indicators such as hemoglobin(Hb), hematocrit (HCT), serum ferritin (SF), and serum soluble transferrin receptor (sTfR) were commonly used for evaluating the characteristic changes of iron status occurred due to physiologic anemia [27].
IDA is defined as hemoglobin < 11 g/dL or hematocrit < 33% and serum ferritin < 12 µg/L, respectively [28]. Most often, hemoglobin and hematocrit are used as indicators for anemia in pregnancy [28, 29]. Besides Hb/HCT values, specific indicators such as SF act as sensitive markers for maternal and fetal iron status; sTfR identifies iron demand in cellular iron homeostasis [30]. During the gestational period, sTfR concentration remains constant in the first trimester and gradually increases during the second and third trimesters [31]. Hepcidin, a systemic regulator of iron homeostasis, may act as a diagnostic marker for iron deficiency in pregnant women. Longitudinal studies have depicted lower hepcidin levels in pregnancy were likely to promote increased iron absorption [29]. A recent study detected hepcidin range of 0.49–0.76 ng/ml in iron-deficient pregnant women with good sensitivity (80.6–83.3%) and specificity (76.2%) in diagnosing IDA [32]. Thus, pregnant women with lower hepcidin level could transfer higher amount of maternal iron to the fetus, suggesting that maternal hepcidin could acts as better indicator of bioavailability of iron to fetus. Therefore, serum hepcidin would be a better indicator for diagnosis of IDA in pregnancy as compared to other iron indicators.
Iron regulation in pregnancy
Cellular iron regulation
Iron homeostasis at cellular levels is regulated by a post-transcriptional mechanism that controls the production of critical proteins involved in iron uptake, storage, and release (Fig 2). Iron-regulatory proteins IRP1 and IRP2 are two major proteins in the post-transcriptional regulation of cellular iron homeostasis. At low iron levels, IRPs binds to iron responsive element (IREs) located at the 5ʹ untranslated region (UTR) of RNA stem loops of ferritin FT (iron storage)/ ferroportin FPN (iron exporter) and inhibits their translation. In contrast, 3ʹ UTR binding to transferrin receptor 1 (TFR1) mRNA and divalent metal transporter 1 (DMT1) (iron uptake) stabilizes them [33]. Because of cellular iron deficiency, increased expression of TFR1 and reduced ferritin allows more iron acquisition and mobilization from the iron stores. Whereas at high iron levels, IRPs do not bind to IREs, causing increased ferritin and ferroportin synthesis and degradation of TFR1 and DMT1 [34].
Cellular iron regulation under physiological condition: Iron acquisition depends on endocytosis of diferric transferrin (TF-Fe (III)2) through transferrin receptor (TFR1) on the cell surface. Acidified endosome causes the release of Fe3+ (blue balls) from TF. Fe3+ is transported by divalent metal transporter 1 (DMT1) into the cytoplasm after Fe3+ is reduced to Fe2+ (yellow balls) by STEAP3 (transmembrane epithelial antigen of prostate). Iron-regulatory proteins 1/2 (IRP 1/2) sense the amount of iron present in the cytosol and regulate post-transcriptional modification of iron uptake proteins (DMT1, TFR1), iron storage protein ferritin (FT), and iron exporter ferroportin (FPN). In iron-deficient cells, IRPs stabilize mRNAs of DMT1 and TFR1 by binding to 3′ UTR (untranslated region) iron responsive element (IRE) and allowing increased iron uptake. IRPs bind to 5′. UTR IREs in FT and FPN mRNAs and represses their translation, reducing iron storage and export. In iron replete cells, IRPs do not bind to IREs and increase FT and FPN synthesis while promoting degradation of TFR1 and DMT1
To examine the association of IRPs with placental iron transporters such as TFR1, FPN and FT, Bradley and co-workers analyzed 22 pregnant women's placental tissues at different gestational ages [35]. They demonstrated that IRP1 and IRP2 activity is present throughout gestation and responds to fetal iron status. IRP1 activity was the mainstay for post-transcriptional regulation of FT and FPN in the placenta [35]. Chong’s immunohistochemical study exhibited isoforms of DMT1 such as DMT1A containing IRE in its 3′ UTR and DMT1B without IRE. DMT1 isoforms were expressed in syncytiotrophoblasts and were responsible for cellular iron transport in the placenta [36]. A recent study using IRP1 knockout iron-deficient mice illustrated that placental iron regulators FPN, and transferrin receptor (TFRC) function is regulated by IRP1 activity in response to maternal iron deficiency. Thus placental iron regulation is mediated by IRP1 and the expression of placental IRP2 is much lower than the IRP1 [37].
Systemic iron regulation
Hepcidin, a small peptide hormone, is the systemic regulator of iron absorption, binds to ferroportin and regulates iron entry into the circulation [38]. In the liver, hepcidin synthesis is increased in iron overload or inflammation and suppressed in iron-deficient or hypoxic conditions. Hepcidin in circulation modulates iron absorption and mobilization from iron stores [39].
Insights into hepcidin in pregnancy
Hepcidin concentration decreases throughout the gestational period with increased iron absorption from diet and mobilization from maternal iron stores towards maternal bone marrow for increased erythropoiesis [40]. Studies have reported that hepcidin regulates the iron endowment to placental–fetal unit [41, 42]. Using choriocarcinoma cell line, Jeg 3, as invitro trophoblast model, exogenous hepcidin treatment resulted in decreased expression of ferroportin and transferrin receptor in trophoblast cells [43]. In addition to the effects of maternal hepcidin on iron regulation, fetal hepcidin synthesized by the fetal liver also contributes to the regulation of placental iron transfer towards fetal circulation by regulating the expression of placental transferrin receptor [44]. In a rat model study, fetal hepcidin levels became much lower in an iron-deficient fetus, where fetal liver iron levels strongly correlated with placental transferrin receptor (TFRC) expression, indicating the regulation of placental iron absorption towards fetus by fetal hepcidin [45]. Hence, the question arises of how fetal hepcidin regulates placental TFRC levels. On the other side, studies have shown that fetal hepcidin regulates placental ferroportin expressed on the basolateral side of syncytiotrophoblasts. Together these data provide evidence that fetal hepcidin can have direct influence at the rate of iron delivered to the fetus [27, 44]. In addition, transgenic overexpression of fetal hepcidin in mice had severe iron deficiency and led to spontaneous abortion in utero [46]. Besides in vivo studies have observed lower fetal hepcidin levels in normal pregnancy [45, 47].
In humans, hepcidin levels have been measured only in cord blood at delivery, where fetal hepcidin levels were significantly higher than maternal hepcidin [14, 42, 48]. Basu et al. observed a significant association between maternal and cord blood hepcidin concentration (r = 0.717, p ≤ 0.001) [48]. In contrast, other studies have shown no association of cord blood hepcidin with maternal hepcidin and iron status [14, 42, 49]. Of interest, the authors studied the conceptual link between maternal and fetal iron status and found the association of maternal hepcidin with iron parameters of neonates [14, 50]. In a study by Young, Griffin et al., nineteen pregnant women had ingested intrinsically labeled non-heme and heme iron sources, where iron status was inversely correlated with maternal hepcidin and directly associated with neonatal hemoglobin [51]. Thus, downregulation of maternal hepcidin increases iron absorption and direct delivery to the fetus, establishing adequate iron stores in neonates at birth.
Erythroid derived cytokines like growth differentiation factor 15 (GDF15), twisted gastrulation homolog 1 (TWSG1) and erythroferrone (ERFE) are considered hepcidin suppressors in the setting of increased erythropoiesis [52,53,54]. The suppressive effect of these erythroid regulators on hepcidin regulation during pregnancy needs to be studied extensively. A study on possible hepcidin inhibitors in healthy pregnant women suggested that maternal iron stores, soluble hemojuvelin, and erythropoietin (EPO) suppress hepcidin transcription while GDF15 has no suppressive effects on hepcidin [55].
Animal and human studies have recognized erythroferrone as the main erythroid regulator for hepatocyte hepcidin suppression. ERFE secreted by erythroblasts specifically in response to erythropoietin and it helps in accumulating iron for erythropoiesis [56]. Delany et al. have shown increased ERFE levels in neonates in comparison to mother. In these neonates, ERFE increased in response to erythropoietin and had inverse association with cord blood hepcidin. Besides neonatal hepcidin and the hepcidin/erythropoietin ratio were the strongest determinants of neonatal Fe and hematological status [57]. Data from current studies on erythroferrone, erythropoietin and hepcidin in pregnant women at mid-gestation and delivery have not found significant association between maternal hepcidin and erythroferrone [57,58,59]. These data suggest that erythroferrone might not be a main driver for hepcidin suppression.
Hormonal regulation of iron metabolism
Several hormones act as checkpoints for placentation and fetal progression during pregnancy. The chief hormones produced during pregnancy are estrogen and progesterone, where estrogen and its relation to iron status were primarily studied in the non-pregnant state [60]. In pregnancy, estrogen is produced in the placenta at the rate of 100–120 mg/24 h, which enables nutrient transfer and helps in vascularization [61]. In vivo studies have reported EPO production was inhibited by increased estrogen levels in pregnant mice models [62]. Horiguchi et al. described the suppressive effect of 17β-estradiol (E2) administration on EPO induction in iron-deficient pregnant rats and the subsequent restoring effect of EPO during iron availability [63]. Endogenous 17β-estradiol also inhibits hepatic hepcidin expression by binding to estrogen responsive element (ERE) at the promoter region of the hepcidin gene and increases iron absorption [60, 64, 65].
Cortisol is a stress hormone released by adrenal glands in the anabolic phase of pregnancy [66]. In young guinea pigs, cortisol levels were increased in response to maternal iron deficiency owing to increased stress levels [66]. Cortisol could be used as a stress biomarker to measure maternal iron deficiency's impact.
Iron trafficking in placenta
Fetal iron source
The transition of iron to the fetus is pooled from sources such as maternal dietary and supplementary iron and maternal iron stores. Chang Cao reported that a pregnant woman consumes bioavailable iron around ~13 mg/day at the onset of pregnancy, of which ~12 mg was non-heme and ~1mg heme iron [67]. Nearly 3–4 mg of dietary iron is loaded onto transferrin. Erythrophagocytosis of senescent red blood cells (RBC) affords ten times more iron into the system. In extravascular RBC catabolism, approximately 20 mg of Fe is released into the plasma iron pool. Besides, 1–2 mg of Fe is discharged by intravascular RBC catabolism as heme and Hb and transported towards the placenta [68].
The placenta employs a distinct cellular iron homeostasis pattern that exclusively responds to systemic and local maternofetal regulatory signals [8]. Restricted rates of iron uptake are facilitated by syncytiotrophoblasts and delivered to the fetus to avoid the excess iron transfer. Earlier studies had suggested that iron flows unidirectionally between maternal and fetal circulation [69, 70].
Non-heme iron transport
From maternal circulation, non-heme iron acquisition takes place through the diferric transferrin (TF-Fe (III)2) bound transferrin receptor 1 (TFR1) complex located on the apical side of syncytiotrophoblasts. Early kinetic studies on the term human placenta demonstrated the higher expression of TF and TFR1 in the placental microvillus surface, which confirms increased iron absorption in the placental apical membrane facing the maternal side [71, 72].
Unlike human placenta, mouse has two syncytiotrophoblasts layers I and II. Transferrin receptor localized to the intracellular vesicles in syncytiotrophoblast I was involved in iron acquisition from maternally injected transferrin iron, suggesting iron trafficking takes place in different placental cells. And it is obscure whether transferrin bound iron travels from syncytiotrophoblast I to II [73].
After non-heme iron uptake, acidification of the endocytosed vesicle assists in the detachment of iron from transferrin. Here iron is reduced to the ferrous state by ferric reductases of Six-Transmembrane Epithelial Antigen of Prostate (STEAP) family members. Notably, STEAP 3, 4 are expressed in the placenta [74, 75]. Further, the reduced form of iron is egressed into the cytoplasm by potential transporters such as DMT1 and Zrt and Irt-like protein 14 (ZIP14) [76]. In the cytoplasm, iron is either incorporated into ferritin, which is strongly expressed in stroma [77] or it is transported to the basal side of syncytiotrophoblasts through the concerted action of FPN, where FPN acts as an iron efflux pump. Subcellular location of FPN in mouse placenta was recently found to be localized to the basal membrane of syncytiotrophoblast II and not present in the fetal endothelium [73].
Ferroxidases such as zyklopen (Zp), hephaestin (HEPH), ceruloplasmin (Cp) are localized to the placenta. Hephaestin expression in placenta was detected in BeWo cell line [78] and mice model lacking hephaestin were survived, indicating absence of its role in placental iron oxidation. Recent investigation on hephaestin knockout mice had fetus with abnormal red cell indices causing fetal anemia. Placental HEPH gene disruption in this mice model had uneven distribution of iron to the fetus, implying essential role of hephaestin in correct distribution of iron and not require for the placental iron export [79]. Earlier animal study observed ceruloplasmin in fetal circulation in early gestation and increase in Cp levels as gestation advances [80]. Using zyklopen knockout mice, author demonstrated that Zp localizes to maternal decidua and not required for the placental iron transfer, rather it is involved in the placental development [81]. Collectively these data implies that unknown ferroxidase involve in iron oxidization in the placenta.
Fe transport across fetal capillary endothelium needs to be characterized, while there is some evidence of transferrin receptor expression in fetal capillary endothelium, suggesting the possibility of endocytosis activity in iron transfer [82]. The probable mechanism of iron transport across the placenta is depicted in Fig. 3.
Iron trafficking in the placenta: Maternal diferric transferrin (TF-Fe (III)2) binds to the transferrin receptor (TFR1) present on the apical plasma membrane of syncytiotrophoblasts and gets internalized by endocytosis. In acidified endosomes, ferric iron is dissociated from the TF-TFR1 complex and reduced to the ferrous state by ferrireductase STEAP3 (transmembrane epithelial antigen of prostate). Then ferrous iron is exported into the cytoplasm by DMT1 (Divalent metal transporter 1) or ZIP 14 or ZIP 8 (Zrt and Irt-like protein). Maternal heme is bound to hemopexin and scavenged via placental LRP1-mediated endocytosis. Heme iron is freed from hemopexin in the lysosome. It is exported to the maternal circulation via FLVCR1 or degraded by heme oxygenase to release iron into the labile iron pool (LIP). LIP incorporates Fe2+ into the ferritin reservoir or iron efflux from syncytiotrophoblasts via ferroportin (FPN). Released Fe2+ is oxidized by unknown ferroxidase and exported into the fetal circulation and transported possibly by fetal transferrin (TF) to the fetus
Gambling and his colleagues demonstrated the rate of iron transfer using a rat model. They suggested that pregnant rats up to 12.5 days of gestation could maintain their hematocrits despite being iron depleted for about five weeks. However, in the second half of pregnancy, hematocrit became low to compensate for high fetal demand. Fetal iron levels were shown to regulate placental transferrin receptor and maternal hepcidin levels, thereby determining the iron supply rate to the fetus [45].
Heme iron transport
Until now, sources have not provided clear evidence on whether transferrin bound iron is solely responsible for the fetal iron transfer. In an animal study, despite transferrin receptor allele (TfR1) disruption in mice causing defective erythropoiesis in embryos, TfR1-/- embryos were able to generate substantial red blood cells, which suggests that an alternative iron uptake mechanism could occur in early embryogenesis. Total deletion of TfR1 in the placenta could solve this controversy [83]. Nevertheless, the hemochorial placenta highly expresses heme transporters, including low density lipoprotein receptor related protein 1 (LRP1), Felin Leukemic virus subgroup C receptor 1 (FLVCR1), and proton coupled folate transporter (PCFT) also known as heme carrier protein 1 (HCP1).
Besides the placental lipid transport, LRP1 is involved in heme uptake from maternal circulation [84]. In systemic heme recycling, LRP1 is identified as a primary receptor of the heme–hemopexin complex, where plasma protein hemopexin (Hx) has a higher affinity for heme and mediates heme delivery to liver storage. Consistent findings revealed that an increased number of LRP1 in hepatoma cells of iron deprived mice had increased heme iron uptake. In iron-deficient conditions, a similar fashion of heme uptake was noticed in the placenta favoring the fetal iron demand [85]. Besides FLVCR1, a heme exporter that regulates intracellular heme content, and PCFT, a folate transporter engaged in intestinal heme absorption, could be utilized for placental iron transport [86]. Association of LRP1 and FLVCR1 with serum Hx concentration in 57 pregnant women have confirmed that placental heme uptake is mediated by LRP1 and exported via FLVCR1. These findings suggest that heme iron transporters co-ordinately regulate heme iron clearance to prevent the piling of intracellular heme [87]. Another heme transporter, heme oxygenase 1 (HO-1) was detected in trophoblast cells in first trimester and increases, as pregnancy progresses. It was speculated that HO-1 has a role in regulating intracellular iron levels by increasing iron export to fetal side via ferroportin. This relationship was confirmed in the human placenta with fetal death (miscarriage) in first and second trimester, where ratio of HO-1 with FPN-1 was significantly elevated [88].
Coordinated regulation of heme and non-heme transporters with maternal iron status was significantly higher in iron-deficient pregnant women [89]. Furthermore, studying the association of heme transporters with fetal iron demand would help to understand the rate of iron utilized in placental iron transfer.
NTBI transport
Non-transferrin bound iron (NTBI) is another form of iron species that exists in circulation when transferrin saturation and is not commonly present in the serum of healthy subjects [90]. Several authors reported that newborns were the most vulnerable to the disorders caused by NTBI [91, 92]. Higher NTBI concentration was detected in cord blood of newborns with central nervous damage and premature infants. Interestingly, a study using high performance liquid chromatography (HPLC) method found the levels of NTBI ranging from 1.6 to 9.8µM in human term placenta [91]. Consistency with this finding, a first-trimester gestational sac survey confirmed the presence of NTBI in fetal circulation, where transferrin saturation was elevated [93]. Reinforcing the dependence of the fetus on NTBI, several in vivo studies reported that TfR1 deleted mice were born alive despite having severe anemia, suggesting NTBI could be a potential source of iron for the fetus [94, 95]. Additionally, ZIP 8 and ZIP 14, zinc transporters belonging to the solute carrier family 39A, enable the transport of non-transferrin and transferrin bound iron in the mouse placenta [96]. Nevertheless, the precise contribution of NTBI to fetal development in normal and complicated pregnancies would help in understanding placental iron metabolism.
Utilization of iron on fetal side
Many studies have strongly proposed that placental FPN is mainly involved in exporting iron into the fetal circulation [97, 98]. A complete FPN knockout in mice was embryonically lethal, whereas the selective inactivation of FPN in all tissues except the placenta has spared embryonic development and birth [97, 98]. In a recent study, Cao et al. developed mouse model using CRISPR/Cas9 for trophoblast subtype (syncytin b (Synb) Cre line (SynbCre) mice), targeting syncytiotrophoblast facing towards fetal side; demonstrated that conditional knockout of placental Fpn1 in late gestation was embryonically fatal [99]. Collectively these data suggest essential role of ferroportin in placental iron transfer.
Whether the exported iron via FPN is loaded onto transferrin or unknown transporter remains a mystery. Direct transportation of NTBI to fetal circulation is still not elucidated [94]. Ganz et al. reported that fetal hepcidin regulates maternal iron transport towards fetal circulation [100]. In affirmation, rat model studies have evidenced that fetal liver iron has a physiological relationship with maternal transferrin receptor expression [45]. In addition, overexpressed fetal hepcidin in transgenic mice regulated placental ferroportin levels and increased iron export into the fetal circulation [50]. Thus, the fetal liver could control the maternal iron supply to the fetus.
Interestingly, Gunshin and his group developed a SLC11A2-/- (Solute carrier family 11, member 2 or DMT1) mice model and demonstrated that neonates of knockout mice had excess liver iron stores at birth and regular iron stores even in the absence of SLC11A2. Suggesting that fetal SLC11A2 is indispensable for iron acquisition after birth but not required for placental iron transfer [101]. Fundamental questions remain regarding different forms of iron species across the fetal endothelium and its regulation by fetal iron regulators.
Placental iron transport in dysregulated iron homeostasis
Many pregnant women in developing countries develop IDA during gestation, a significant public health concern [18]. During pregnancy, RBC mass expansion and placenta–fetal growth and development impose primary demand for iron from the mother; when the requirement is not met, it results in anemia due to iron deficiency [15]. Maternal iron deficiency causes a severe risk of anemia and affects the developing fetus. In a longitudinal study of 225 pregnant women, iron-deficient pregnant women had a significant association of maternal iron status indicators with placental heme and non-heme transporters, indicating increased iron transfer from mother to fetus [89]. Decreased iron stores and high transferrin receptor levels in pregnant women at mid-gestation were consistently related to the abundance of placental TFR1. In addition, the fetal iron stores indicated by cord blood ferritin levels were negatively associated with placental FLVCR1 expression [89]. Data suggest that the fetus gets priority according to the hierarchical usage of iron, but how the exact mechanism of this priority is regulated remains unclear.
Gestational diabetes mellitus (GDM) is another common disorder in pregnancy caused by glucose intolerance in the second and third trimester [102]. Hemoglobin and iron levels are higher in GDM pregnant women than in healthy pregnant controls [103]. A strong positive relationship between ferritin levels and GDM in pregnant women has also been shown. [103,104,105]. In another study, elevated ferritin [Ferritin—94.5 (67.9–133.5) pmol/l] and hepcidin levels [6.4 (4.6–8.3) ng/ml] had a significant association with increased GDM risk at the second trimester (95% CI: 1.07, 6.36) [105]. Further, FPN expression was higher in GDM pregnant women, while hepcidin expression was lower, indicating an active transport of iron to the fetus in GDM pregnant women compared to normal [106]. Thus, the placenta dynamically participates in the surplus amount of iron transfer to the fetus from iron overloaded GDM mother. However, detailed research is required to predict iron status in the fetus by determining fetal iron parameters in GDM pregnant women.
Iron overload was observed in pregnant women with hereditary hemochromatosis (HH). HH patients carry a mutation in the homeostatic iron regulator (HFE) gene involved in the hepcidin transcription. Pregnant women with HH had higher ferritin levels than their normal counterparts (Table 1) [107]. Thus far, no studies have assessed hepcidin levels in HH pregnant women. In a single case study on HH pregnant women, the fetus had increased ferritin levels (250µg/L) and transferrin saturation (88%) [108]. Nonetheless, the exact mechanism of iron regulation in HH pregnant women and their fetuses remains speculative.
Neonatal hemochromatosis is characterized by fetal liver cirrhosis and marked by increased expression of TFR1, transferrin, hepcidin, ferritin, and DMT1 in microvilli surface and cytoplasm of syncytiotrophoblasts [109, 110]. Decreased fetal hepcidin levels are observed in this rare neonatal disorder. To counterbalance fetal hepcidin deficiency, ferroportin was sustained on the surface of syncytiotrophoblasts and thereby helps in iron transfer from mother to fetus at a higher level.
Yet another iron disorder is beta thalassemia major and intermedia marked by maternal iron overload secondary to stress erythropoiesis [111]. The absence or decreased production of hemoglobin tetramer beta globin chains causes beta thalassemia (BT). BT is characterized by ineffective erythropoiesis, splenomegaly, extramedullary expansion, apoptosis of erythroid precursors, and shortened mature RBC survival [112].
Two cases of pregnant women with β-thalassemia major and intermedia had 50% iron deposition in placental villi at the 38th gestational week [113]. In another case report on neonates born to β-thalassemia major pregnant women, the fetus had lower ferritin and serum iron levels compared to maternal iron indicators [114]. This suggests that neonates born to thalassemic women were not affected by iron overload in mothers. In thirty-six non-transfusion dependent beta thalassemic pregnant women, ferritin levels were not exacerbated at pre and post pregnancy (409.35 ug/L and 418.18 ug/L, respectively), and they had successful delivery [115]. Ferritin (p = 0.0137) and liver iron levels (p = 0.006) increased in the third trimester in eleven pregnant women with β-thalassemia major who received chelation therapy either before or during pregnancy, and the iron levels were monitored using MRI (Magnetic resonance) [116]. Substantially, iron overload in beta thalassemia might result in maternal and fetal complications [116]. In contrast to GDM and HH, the amount of iron transferred from beta thalassemic mother to fetus is not in excess despite the placenta loaded with iron.
Although iron deficiency or iron overload has been extensively studied in the above disorders, a more detailed understanding of maternal and fetal signaling is needed to minimize iron dysregulation. Fetal iron homeostasis in these high-risk pregnant women is unexplored so far. Identifying essential iron regulatory genes associated with these disorders would substantially prevent adverse outcomes in the mother and the fetus.
Conclusion and future directions
The placental iron trafficking mechanisms and regulation from the studies reported so far have critically elucidated factors, including hepcidin, DMT1, and FPN. During the pre-gestational period, many women entered with reduced iron stores. Maternal iron absorption is regulated by systemic iron regulatory hormone hepcidin, which declines throughout gestation and facilitates increased iron mobilization to meet the iron demand. The placenta regulates and ensures optimal iron transfer from mother to fetus and assists in having sufficient iron stores in neonates at birth.
In the placenta, the transferrin receptor helps in non-heme iron uptake from the maternal iron-transferrin complex and gets endocytosed. Cellular iron transporter DMT1 transports iron from endosome to cytoplasm in syncytiotrophoblasts, and FPN effluxes iron from syncytiotrophoblasts to fetal circulation. On the other hand, heme iron acquisition occurs through heme receptor LRP1. Fetus utilizes maximum iron from mother as per hierarchical usage and benefits from adequate iron stores at birth. But the mechanism of maternal and fetal regulation in determining the rate of iron transfer across the placenta raises many unanswered questions.
Understanding the importance of iron regulators in the placenta using animal models is well appreciated. Some studies suggested that fetal iron is regulated independently of maternal support. Hepcidin levels decline throughout the gestational period, ascertaining that an unknown mechanism exerts a suppressive effect. Molecular details of cellular iron transporters highly expressed in the placenta are poorly characterized; identifying the function of normal and alternative isoforms of cellular iron transporters would help to understand prioritized iron transport for the fetal need. Hence, detailing mechanistic insights of placental dynamic regulation of maternofetal signals and fetal iron homeostasis using animal models and a larger cohort of human pregnancies will elucidate the gap in iron regulation during pregnancy.
Data availability
This is a review article and no data was generated or analyzed. Further enquiries can be directed to the corresponding author.
References
“WHO guidance helps detect iron deficiency and protect brain development.” https://www.who.int/news/item/20-04-2020-who-guidance-helps-detect-iron-deficiency-and-protect-brain-development (accessed Dec. 23, 2022).
Georgieff MK (2020) Iron deficiency in pregnancy. Am J Obstet Gynecol 223(4):516–524. https://doi.org/10.1016/j.ajog.2020.03.006
Yang Z et al (2009) Prevalence and predictors of iron deficiency in fully breastfed infants at 6 mo of age: comparison of data from 6 studies. Am J Clin Nutr 89(5):1433–1440. https://doi.org/10.3945/ajcn.2008.26964
H. Kay, D. M. Nelson, and Y. Wang, The Placenta: From Development to Disease. Wiley, 2011.
Roberts H, Bourque SL, Renaud SJ (2020) Maternal iron homeostasis: effect on placental development and function. Reproduction 160(4):R65–R78. https://doi.org/10.1530/REP-20-0271
Soares MJ, Varberg KM, Iqbal K (2018) Hemochorial placentation: development, function, and adaptations. Biol Reprod 99(1):196–211. https://doi.org/10.1093/biolre/ioy049
Polin RA, Fox WW, Abman SH (2011) Fetal and neonatal physiology e-book, 4th edn. Elsevier Health Sciences, Philadelphia, PA
McArdle HJ, Lang C, Hayes H, Gambling L (2011) Role of the placenta in regulation of fetal iron status. Nutr Rev 69(s1):S17–S22. https://doi.org/10.1111/j.1753-4887.2011.00428.x
“Estrogen-enhanced apical and basolateral secretion of apolipoprotein B-100 by polarized trophoblast-derived BeWo cells - ScienceDirect.” https://www.sciencedirect.com/science/article/abs/pii/S0300908417301189?via%3Dihub (accessed Jun. 15, 2022).
Deyssenroth MA, Peng S, Hao K, Lambertini L, Marsit CJ, Chen J (2017) Whole-transcriptome analysis delineates the human placenta gene network and its associations with fetal growth. BMC Genom 18(1):520. https://doi.org/10.1186/s12864-017-3878-0
Perez-Garcia V et al (2018) Placentation defects are highly prevalent in embryonic lethal mouse mutants. Nature 555(7697):463–468. https://doi.org/10.1038/nature26002
Edison ES, Bajel A, Chandy M (2008) Iron homeostasis: new players, newer insights. Eur J Haematol 81(6):411–424. https://doi.org/10.1111/j.1600-0609.2008.01143.x
Cao C, Fleming MD (2016) The placenta: the forgotten essential organ of iron transport. Nutr Rev 74(7):421–431. https://doi.org/10.1093/nutrit/nuw009
Gunes T et al (2016) Maternal and cord blood hepcidin levels based on gestational weeks in term and preterm infants. Pediatr Hematol Oncol J 1(2):23–27. https://doi.org/10.1016/j.phoj.2016.07.007
Bothwell TH (2000) Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr 72(1 Suppl):257s–264s. https://doi.org/10.1093/ajcn/72.1.257S
Gassmann B (1991) Requirements of Vitamin A, iron, folate and Vitamin B12. report of joint FAO/WHO expert consultation. 107 Seiten, 5 Abb., 24 Tab. food and agriculture organization of the United Nations; Rome 1988. Food Nahr 35(1):20–20. https://doi.org/10.1002/food.19910350104
Sharma MSJB (2010) “Anemia in Pregnancy,”. JIMSA, 23(4)
WHO, 2012 “WHO Guidelines Approved by the Guidelines Review Committee,” in Guideline: Daily Iron and Folic Acid Supplementation in Pregnant Women, Geneva: World Health Organization World Health Organization.
Rioux FM, LeBlanc CP (2007) Iron supplementation during pregnancy: what are the risks and benefits of current practices? Appl Physiol Nutr Metab Physiol Appl Nutr Metab 32(2):282–288. https://doi.org/10.1139/H07-012
Ramakrishnan U et al (2004) Multiple micronutrient supplements during pregnancy do not reduce anemia or improve iron status compared to iron-only supplements in Semirural Mexico. J Nutr 134(4):898–903. https://doi.org/10.1093/jn/134.4.898
Milman N (2012) Oral iron prophylaxis in pregnancy: not too little and not too much! J Pregnancy 2012:514345. https://doi.org/10.1155/2012/514345
Mathan VI, Baker SJ, Sood SK, Ramachandran K, Ramalingaswami V (1979) WHO sponsored collaborative studies on nutritional anaemia in India. The effects of ascorbic acid and protein supplementation on the response of pregnant women to iron, pteroylglutamic acid and cyanocobalamin therapy. Br J Nutr 42(3):391–398
Rai R, Fawzi W, Barik A, Chowdhury A (2018) The burden of iron-deficiency anaemia among women in India: how have iron and folic acid interventions fared? WHO South-East Asia J Public Health 7(1):18–23. https://doi.org/10.4103/2224-3151.228423
Gautam CS, Saha L, Sekhri K, Saha PK (2008) Iron deficiency in pregnancy and the rationality of iron supplements prescribed during pregnancy. Medscape J Med 10(12):283
Lurie S, Mamet Y (2001) Red blood cell survival and inetics during pregnancy. Eur J Obstet Gynecol Reprod Biol 93:185–192. https://doi.org/10.1016/S0301-2115(00)00290-6
Vricella LK (2017) Emerging understanding and measurement of plasma volume expansion in pregnancy. Am J Clin Nutr 106(Suppl 6):1620S-1625S. https://doi.org/10.3945/ajcn.117.155903
Fisher AL, Nemeth E (2017) Iron homeostasis during pregnancy. Am J Clin Nutr 106(Suppl 6):1567s–1574s. https://doi.org/10.3945/ajcn.117.155812
Suominen P, Punnonen K, Rajamaki A, Irjala K (1998) Serum transferrin receptor and transferrin receptor-ferritin index identify healthy subjects with subclinical iron deficits. Blood 92(8):2934–2939
WHO/UNICEF/UNU, 2001 “Iron Deficiency Anemia: Assessment,Prevention and Control. A Guide for Programme Managers.Geneva, World Health Organization,”
Daru J, Colman K, Stanworth SJ, De La Salle B, Wood EM, Pasricha SR (2017) Serum ferritin as an indicator of iron status: what do we need to know? Am J Clin Nutr 106(Suppl 6):1634S-1639S. https://doi.org/10.3945/ajcn.117.155960
Choi JW, Im MW, Pai SH (2000) Serum transferrin receptor concentrations during normal pregnancy. Clin Chem 46(5):725–727
Zaman B, Rasool S, Jasim S, Abdulah D (2019) Hepcidin as a diagnostic biomarker of iron deficiency anemia during pregnancy. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1635112
Torti SV, Torti FM (2013) Iron and cancer: more ore to be mined. Nat Rev Cancer 13(5):342–355. https://doi.org/10.1038/nrc3495
Georgieff MK, Berry SA, Wobken JD, Leibold EA (1999) Increased placental iron regulatory protein-1 expression in diabetic pregnancies complicated by fetal iron deficiency. Placenta 20(1):87–93. https://doi.org/10.1053/plac.1998.0339
Bradley J et al (2004) Influence of gestational age and fetal iron status on IRP activity and iron transporter protein expression in third-trimester human placenta. Am J Physiol Regul Integr Comp Physiol 287(4):R894-901. https://doi.org/10.1152/ajpregu.00525.2003
Chong WS, Kwan PC, Chan LY, Chiu PY, Cheung TK, Lau TK (2005) Expression of divalent metal transporter 1 (DMT1) isoforms in first trimester human placenta and embryonic tissues. Hum Reprod 20(12):3532–3538. https://doi.org/10.1093/humrep/dei246
Sangkhae V et al (2019) Effects of maternal iron status on placental and fetal iron homeostasis. J Clin Invest. https://doi.org/10.1172/jci127341
Silvestri L, Nai A, Dulja A, Pagani A (2019) Hepcidin and the BMP-SMAD pathway: an unexpected liaison. Vitam Horm 110:71–99. https://doi.org/10.1016/bs.vh.2019.01.004
Tandara L, Salamunic I (2012) Iron metabolism: current facts and future decisions. Biochem Med Zagreb 22(3):311–328. https://doi.org/10.11613/bm.2012.034
Mégier C, Peoch K, Puy V, Cordier AG (2022) Iron metabolism in normal and pathological pregnancies and fetal consequences. Metabolites 12(2):129. https://doi.org/10.3390/metabo12020129
Guo Y et al (2019) Iron homeostasis in pregnancy and spontaneous abortion. Am J Hematol 94(2):184–188. https://doi.org/10.1002/ajh.25341
Kulik-Rechberger B, Kosciesza A, Szponar E, Domosud J (2016) Hepcidin and iron status in pregnant women and full-term newborns in first days of life. Ginekol Pol 87(4):288–292. https://doi.org/10.17772/gp/62202
McDonald EA, Gundogan F, Olveda RM, Bartnikas TB, Kurtis JD, Friedman JF (2022) Iron transport across the human placenta is regulated by hepcidin. Pediatr Res 92(2):396–402. https://doi.org/10.1038/s41390-020-01201-y
Kammerer L, Mohammad G, Wolna M, Robbins P, Lakhal-Littleton S (2019) Fetal liver hepcidin supports acquisition of iron stores in utero. Biorxiv. https://doi.org/10.1101/799304
Gambling L et al (2009) Fetal iron status regulates maternal iron metabolism during pregnancy in the rat. Am J Physiol Regul Integr Comp Physiol 296(4):R1063–R1070. https://doi.org/10.1152/ajpregu.90793.2008
Nicolas G et al (2002) Severe iron deficiency anemia in transgenic mice expressing liver hepcidin. Proc Natl Acad Sci U A 99(7):4596–4601. https://doi.org/10.1073/pnas.072632499
Willemetz A et al (2014) Matriptase-2 is essential for hepcidin repression during fetal life and postnatal development in mice to maintain iron homeostasis. Blood 124(3):441–444. https://doi.org/10.1182/blood-2014-01-551150
Basu S, Kumar N, Srivastava R, Kumar A (2016) Maternal and cord blood hepcidin concentrations in severe iron deficiency Anemia. Pediatr Neonatol 57(5):413–419. https://doi.org/10.1016/j.pedneo.2015.09.012
Rehu M et al (2010) Maternal serum hepcidin is low at term and independent of cord blood iron status. Eur J Haematol 85(4):345–352. https://doi.org/10.1111/j.1600-0609.2010.01479.x
Koenig MD, Tussing-Humphreys L, Day J, Cadwell B, Nemeth E (2014) Hepcidin and iron homeostasis during pregnancy. Nutrients 6(8):3062–3083. https://doi.org/10.3390/nu6083062
Young MF et al (2012) Maternal hepcidin is associated with placental transfer of iron derived from dietary heme and nonheme sources. J Nutr 142(1):33–39. https://doi.org/10.3945/jn.111.145961
Tanno T et al (2007) High levels of GDF15 in thalassemia suppress expression of the iron regulatory protein hepcidin. Nat Med 13(9):1096–1101. https://doi.org/10.1038/nm1629
Tanno T et al (2009) Identification of TWSG1 as a second novel erythroid regulator of hepcidin expression in murine and human cells. Blood 114(1):181–186. https://doi.org/10.1182/blood-2008-12-195503
Arezes J et al (2018) Erythroferrone inhibits the induction of hepcidin by BMP6. Blood 132(14):1473–1477. https://doi.org/10.1182/blood-2018-06-857995
Finkenstedt A et al (2012) Hepcidin is correlated to soluble hemojuvelin but not to increased GDF15 during pregnancy. Blood Cells Mol Dis 48(4):233–237. https://doi.org/10.1016/j.bcmd.2012.02.001
Coffey R, Ganz T (2018) Erythroferrone: an erythroid regulator of hepcidin and iron metabolism. HemaSphere 2(2):e35. https://doi.org/10.1097/HS9.0000000000000035
Delaney KM, Guillet R, Pressman EK, Ganz T, Nemeth E, O’Brien KO (2021) Umbilical cord erythroferrone is inversely associated with hepcidin, but does not capture the most variability in iron status of neonates born to teens carrying singletons and women carrying multiples. J Nutr 151(9):2590–2600. https://doi.org/10.1093/jn/nxab156
Delaney KM, Guillet R, Pressman EK, Ganz T, Nemeth E, O’Brien KO (2021) Serum erythroferrone during pregnancy is related to erythropoietin but does not predict the Risk of Anemia. J Nutr 151(7):1824–1833. https://doi.org/10.1093/jn/nxab093
Wei S et al (2021) Disordered serum erythroferrone and hepcidin levels as indicators of the spontaneous abortion occurrence during early pregnancy in humans. Br J Haematol 192(3):643–651. https://doi.org/10.1111/bjh.17049
Dacks PA (2012) Estrogens iron out the details: a novel direct pathway for estrogen control of iron homeostasis. Endocrinology 153(7):2942–2944. https://doi.org/10.1210/en.2012-1480
Morel Y, Roucher F, Plotton I, Goursaud C, Tardy V, Mallet D (2016) Evolution of steroids during pregnancy: Maternal, placental and fetal synthesis. Ann Endocrinol Paris 77(2):82–89. https://doi.org/10.1016/j.ando.2016.04.023
Mukundan H, Resta TC, Kanagy NL (2002) 17Beta-estradiol decreases hypoxic induction of erythropoietin gene expression. Am J Physiol Regul Integr Comp Physiol 283(2):R496-504. https://doi.org/10.1152/ajpregu.00573.2001
Horiguchi H, Oguma E, Kayama F (2005) The effects of iron deficiency on estradiol-induced suppression of erythropoietin induction in rats: implications of pregnancy-related anemia. Blood 106(1):67–74. https://doi.org/10.1182/blood-2004-06-2350
Yang Q, Jian J, Katz S, Abramson SB, Huang X (2012) 17beta-Estradiol inhibits iron hormone hepcidin through an estrogen responsive element half-site. Endocrinology 153(7):3170–3178. https://doi.org/10.1210/en.2011-2045
Hou Y et al (2012) Estrogen regulates iron homeostasis through governing hepatic hepcidin expression via an estrogen response element. Gene 511(2):398–403. https://doi.org/10.1016/j.gene.2012.09.060
Shero N, Fiset S, Plamondon H, Thabet M, Rioux FM (2018) Increase serum cortisol in young guinea pig offspring in response to maternal iron deficiency. Nutr Res 54:69–79. https://doi.org/10.1016/j.nutres.2018.03.017
Hurrell R, Egli I (2010) Iron bioavailability and dietary reference values. Am J Clin Nutr 91(5):1461s–1467s. https://doi.org/10.3945/ajcn.2010.28674F
Cao C, O’Brien KO (2013) Pregnancy and iron homeostasis: an update. Nutr Rev 71(1):35–51. https://doi.org/10.1111/j.1753-4887.2012.00550.x
Harris ED (1992) New insights into placental iron transport. Nutr Rev 50(11):329–331. https://doi.org/10.1111/j.1753-4887.1992.tb07719.x
O’Brien KO (2022) Maternal, fetal and placental regulation of placental iron trafficking. Placenta 125:47–53. https://doi.org/10.1016/j.placenta.2021.12.018
King BF (1976) Localization of transferrin on the surface of the human placenta by electron microscopic immunocytochemistry. Anat Rec 186(2):151–159. https://doi.org/10.1002/ar.1091860203
Parmley RT, Barton JC, Conrad ME (1985) Ultrastructural localization of transferrin, transferrin receptor, and iron-binding sites on human placental and duodenal microvilli. Br J Haematol 60(1):81–89. https://doi.org/10.1111/j.1365-2141.1985.tb07388.x
Cao C, Fleming MD (2021) Localization and kinetics of the transferrin-dependent iron transport machinery in the mouse placenta. Curr Dev Nutr 5(4):25. https://doi.org/10.1093/cdn/nzab025
Afar et al, 2006 “Antibodies immunospecific for STEAP1,” U. S. Pat.,
Ohgami RS, Campagna DR, McDonald A, Fleming MD (2006) The Steap proteins are metalloreductases. Blood 108(4):1388–1394. https://doi.org/10.1182/blood-2006-02-003681
Li YQ et al (2012) Divalent metal transporter 1 expression and regulation in human placenta. Biol Trace Elem Res 146(1):6–12. https://doi.org/10.1007/s12011-011-9214-7
Bastin J, Drakesmith H, Rees M, Sargent I, Townsend A (2006) Localisation of proteins of iron metabolism in the human placenta and liver. Br J Haematol 134(5):532–543. https://doi.org/10.1111/j.1365-2141.2006.06216.x
Li Y-Q, Bai B, Cao X-X, Yan H, Zhuang G-H (2012) Ferroportin 1 and hephaestin expression in BeWo cell line with different iron treatment. Cell Biochem Funct 30(3):249–255. https://doi.org/10.1002/cbf.1843
Helman SL, Frazer DM, Anderson GJ, Wilkins SJ (2022) Disruption of Hephaestin in the Placenta and Fetus Leads to Fetal Anemia. Blood 140(Supplement 1):2196. https://doi.org/10.1182/blood-2022-167810
Fryer AA, Jones P, Strange R, Hume R, Bell JE (1993) Plasma protein levels in normal human fetuses: 13 to 41 weeks’ gestation. Br J Obstet Gynaecol 100(9):850–855. https://doi.org/10.1111/j.1471-0528.1993.tb14313.x
Helman SL et al (2021) The placental ferroxidase Zyklopen is not essential for iron transport to the fetus in mice. J Nutr 151(9):2541–2550. https://doi.org/10.1093/jn/nxab174
“Endocytosis in the placenta: An undervalued mediator of placental transfer - PubMed.” https://pubmed.ncbi.nlm.nih.gov/33994009/ (accessed Dec. 09, 2022).
Levy JE, Jin O, Fujiwara Y, Kuo F, Andrews NC (1999) Transferrin receptor is necessary for development of erythrocytes and the nervous system. Nat Genet 21(4):396–399. https://doi.org/10.1038/7727
Hvidberg V, Maniecki MB, Jacobsen C, Hojrup P, Moller HJ, Moestrup SK (2005) Identification of the receptor scavenging hemopexin-heme complexes. Blood 106(7):2572–2579. https://doi.org/10.1182/blood-2005-03-1185
Smith A, Ledford BE (1988) Expression of the haemopexin-transport system in cultured mouse hepatoma cells. Links between haemopexin and iron metabolism. Biochem J 256(3):941–950. https://doi.org/10.1042/bj2560941
Quigley JG et al (2004) Identification of a human heme exporter that is essential for erythropoiesis. Cell 118(6):757–766. https://doi.org/10.1016/j.cell.2004.08.014
Cao C, Pressman EK, Cooper EM, Guillet R, Westerman M, O’Brien KO (2014) Placental heme receptor LRP1 correlates with the heme exporter FLVCR1 and neonatal iron status. Reproduction 148(3):295–302. https://doi.org/10.1530/rep-14-0053
Inoue R, Irie Y, Akagi R (2021) Role of heme oxygenase-1 in human placenta on iron supply to Fetus. Placenta 103:53–58. https://doi.org/10.1016/j.placenta.2020.09.065
Best CM et al (2016) Maternal iron status during pregnancy compared with neonatal iron status better predicts placental iron transporter expression in humans. Faseb J 30(10):3541–3550. https://doi.org/10.1096/fj.201600069R
Garbowski MW, Ma Y, Fucharoen S, Srichairatanakool S, Hider R, Porter JB (2016) Clinical and methodological factors affecting non-transferrin-bound iron values using a novel fluorescent bead assay. Transl Res 177:19-30.e5. https://doi.org/10.1016/j.trsl.2016.05.005
Koba M, Socha E, Słomka A, Żekanowska E, Socha M, Grabiec M (2017) The ability to determine the non-transferrin-bound iron and total iron in the human placenta using high-performance liquid chromatography method. Med Res J 2(4):181–185. https://doi.org/10.5603/MRJ.2017.0026
Kalhan TG, Bateman DA, Bowker RM, Hod EA, Kashyap S (2017) Effect of red blood cell storage time on markers of hemolysis and inflammation in transfused very low birth weight infants. Pediatr Res 82(6):964–969. https://doi.org/10.1038/pr.2017.177
Evans P, Cindrova-Davies T, Muttukrishna S, Burton GJ, Porter J, Jauniaux E (2011) Hepcidin and iron species distribution inside the first-trimester human gestational sac. Mol Hum Reprod 17(4):227–232. https://doi.org/10.1093/molehr/gaq101
Sangkhae V, Nemeth E (2019) Placental iron transport: The mechanism and regulatory circuits. Free Radic Biol Med 133:254–261. https://doi.org/10.1016/j.freeradbiomed.2018.07.001
Cc T 3rd, Dr C, Vm S, Nc A, Md F (2000) The molecular defect in hypotransferrinemic mice. Blood 96(3):1113–1118
Girijashanker K et al (2008) Slc39a14 gene encodes ZIP14, a metal/bicarbonate symporter: similarities to the ZIP8 transporter. Mol Pharmacol 73(5):1413–1423. https://doi.org/10.1124/mol.107.043588
Donovan A et al (2005) The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab 1(3):191–200. https://doi.org/10.1016/j.cmet.2005.01.003
Drakesmith H, Nemeth E, Ganz T (2015) Ironing out Ferroportin. Cell Metab 22(5):777–787. https://doi.org/10.1016/j.cmet.2015.09.006
Cao C, Fleming MD (2022) Loss of the placental iron exporter ferroportin 1 causes embryonic demise in late-gestation mouse pregnancy. Development 149(23):201160. https://doi.org/10.1242/dev.201160
Ganz T (2011) Hepcidin and iron regulation, 10 years later. Blood 117(17):4425–4433. https://doi.org/10.1182/blood-2011-01-258467
Gunshin H, Fujiwara Y, Custodio AO, DiRenzo C, Robine S, Andrews NC (2005) Slc11a2 is required for intestinal iron absorption and erythropoiesis but dispensable in placenta and liver. J Clin Invest 115(5):1258–1266. https://doi.org/10.1172/JCI24356
Panaitescu AM, Peltecu G (2016) Gestational diabetes. obstetrical perspective. Acta Endocrinol Buchar 12(3):331–334. https://doi.org/10.4183/aeb.2016.331
Chen X, Scholl TO, Stein TP (2006) Association of elevated serum ferritin levels and the risk of gestational diabetes mellitus in pregnant women: The Camden study. Diabetes Care 29(5):1077–1082. https://doi.org/10.2337/diacare.2951077
Bowers KA, Olsen SF, Bao W, Halldorsson TI, Strom M, Zhang C (2016) Plasma concentrations of ferritin in early pregnancy are associated with risk of gestational diabetes Mellitus in women in the Danish National Birth Cohort. J Nutr 146(9):1756–1761. https://doi.org/10.3945/jn.115.227793
Rawal S et al (2017) A longitudinal study of iron status during pregnancy and the risk of gestational diabetes: findings from a prospective, multiracial cohort. Diabetologia 60(2):249–257. https://doi.org/10.1007/s00125-016-4149-3
Yang A et al (2016) Expression of hepcidin and ferroportin in the placenta, and ferritin and transferrin receptor 1 levels in maternal and umbilical cord blood in pregnant women with and without gestational diabetes. Int J Env. Res Public Health 13(8):766. https://doi.org/10.3390/ijerph13080766
Sokoloff A, Brook S, Cooper M (2009) Iron Studies in hemochromatosis during pregnancy. Blood 114(22):5099–5099
Baynes RD, Meyer TE, Bothwell TH, Lamparelli RD (1991) Maternal and fetal iron measurements in a hemochromatotic pregnancy. Am J Hematol 36(1):48–49. https://doi.org/10.1002/ajh.2830360110
Feldman AG, Whitington PF (2013) Neonatal hemochromatosis. J Clin Exp Hepatol 3(4):313–320. https://doi.org/10.1016/j.jceh.2013.10.004
Shimono A et al (2016) An immunohistochemical study of placental syncytiotrophoblasts in neonatal hemochromatosis. Placenta 48:49–55. https://doi.org/10.1016/j.placenta.2016.10.005
Petrakos G, Andriopoulos P, Tsironi M (2016) Pregnancy in women with thalassemia: challenges and solutions. Int J Womens Health 8:441–451. https://doi.org/10.2147/IJWH.S89308
R. Origa, “Beta-Thalassemia,” in GeneReviews®, M. P. Adam, H. H. Ardinger, R. A. Pagon, S. E. Wallace, L. J. Bean, K. Stephens, and A. Amemiya, Eds. Seattle (WA): University of Washington, Seattle, 1993. Accessed: Nov. 11, 2020. [Online]. Available: http://www.ncbi.nlm.nih.gov/books/NBK1426/
Artico M et al (2004) Direct demonstration of iron in a term placenta in two cases of beta-thalassemia. Am J Hematol 75(4):241–242. https://doi.org/10.1002/ajh.20005
Pearson HA (2007) Iron studies in infants born to an iron overloaded mother with beta-thalassemia major: possible effects of maternal desferrioxamine therapy. J Pediatr Hematol Oncol 29(3):160–162. https://doi.org/10.1097/MPH.0b013e31803b957d
Lee BS, Sathar J, Sivapatham L, Lee LI (2018) Pregnancy outcomes in women with non-transfusion dependent thalassaemia (NTDT): A haematology centre experience. Malays J Pathol 40(2):149–152
Vlachodimitropoulou E, Thomas A, Shah F, Kyei-Mensah A (2018) Pregnancy and iron status in β-thalassaemia major and intermedia: six years’ experience in a North London Hospital. J Obstet Gynaecol 38(4):567–570. https://doi.org/10.1080/01443615.2017.1342616
Acknowledgements
This work was supported by a grant DST/INT/POL/P-7/2014 from the Department of Science and Technology, Government of India to ES.
Funding
This work was supported by a grant DST/INT/POL/P-7/2014 from the Department of Science and Technology, Government of India to ES.
Author information
Authors and Affiliations
Contributions
SS carried out the research, reviewed the literature, prepared tables, and figures, and wrote the manuscript. ES conceptualized the study, reviewed, and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This is a review article. No ethical approval is required.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santhakumar, S., Edison, E.S. Molecular insights into placental iron transfer mechanisms and maternofetal regulation. Arch Gynecol Obstet 309, 63–77 (2024). https://doi.org/10.1007/s00404-023-07032-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07032-6