Abstract
Purpose
To identify prognostic factors of early-stage cervical adenocarcinoma in patients with FIGO IB–IIA, who were treated with radical surgery.
Materials and methods
Clinical data of 64 patients with stage IB–IIA cervical adenocarcinoma who underwent radical hysterectomy and lymphadenectomy with or without adjuvant therapy between 1993 and 2019 were retrospectively reviewed. The clinicopathologic factors that affect the oncological outcomes were evaluated. The Kaplan–Meier method was used for the assessment of survival outcomes. Survival curves were compared using the log-rank test.
Results
The 5-year recurrence-free survival and 5-year disease-specific survivals were 83% and 98%, respectively. Tumor size, stage of disease and uterine spread were significantly related prognostic factors for shorter recurrence-free survival. During the follow-up, nine (14.1%) patients recurred. Five of them were extrapelvic recurrence. No correlation was identified between histopathologic subtype and extrapelvic recurrence (p = 0.265). There was no difference between adjuvant only radiotherapy and concurrent chemoradiotherapy on recurrence-free survival in a univariate analysis adjusting for prognostic factors.
Conclusion
It is important to determine the prognostic factors that predict disease outcome in surgically treated cervical adenocarcinoma for tailored adjuvant treatment. Tumor size, stage and uterine spread are determinant factors for recurrence. Risk stratifications, including uterine spread may especially be useful for patients with AC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cancer of the uterine cervix is the fourth most common cancer worldwide. In 2018, there were an estimated 570,000 new cases that were diagnosed and 310,000 women who died of cervical cancer [1]. Squamous cell cancer (SCC) constitutes the majority of cervical cancer and adenocancer (AC), constituting 10–25% of all cervical cancer cases [2]. In recent years, while SCC incidence has decreased due to the wider implementation of cytological screening and increases in detection rates of premalignant lesions, the relative and absolute rates of AC have increased, especially among young women [2, 3]. The reason for the increase in AC is multifactorial [2, 4]. AC often shows an endophytic growth pattern in the endocervical canal, making it challenging to detect lesions by cytology [3,4,5].
Surgicopathologic factors are important for personalizing postoperative management and predicting prognosis in patients with early-stage cervical cancer who have undergone surgery [6,7,8,9,10]. Although AC has different characteristics concerning epidemiological, prognostic, clinicopathological, molecular features and treatment response, it is treated in the same way as SCC [11]. Several studies reported that AC exhibits more aggressive behavior and could independently influence survival outcomes and had poor prognosis than SCC, implying that histopathologic type was a potential risk factor for cervical cancer and patients with AC should be treated more aggressively [12,13,14,15,16]. Additionally, AC is a very heterogeneous disease and has several subtypes with different histopathological characteristics [2, 4, 17].
In this study, we aimed to identify the clinical, surgicopathological characteristics of cervical AC in patients with the International Federation of Gynecology and Obstetrics (FIGO) IB to IIA who underwent radical hysterectomy and lymphadenectomy and determine the factors predicting survival.
Materials and methods
We reviewed the medical records of 64 patients with cervical AC who had undergone Piver–Rutledge type II or type III radical hysterectomy and lymphadenectomy in our institution between January 1993 and June 2019. This study was approved by the institutional review board (Decision No: 2019-11). Patients with SCC, non-epithelial cervical cancer, cervical neuroendocrine cancer, synchronized cancer or micro-invasive cancer, and patients who had not undergone radical hysterectomy were excluded from this study. Histopathological classification of the tumors was carried out according to 2014 World Health Organization (WHO) criteria [18]. Cervical AC was categorized as endocervical AC–usual type, mucinous, endometrioid, clear cell, serous, mesonephric or villoglandular.
The patients were clinically staged according to FIGO 2014 criteria. All patients underwent a pretreatment staging workup that consisted of pelvic examinations under general anesthesia, cervical tumor biopsy, chest radiography, abdominal and pelvic magnetic resonance imaging (MRI) and/or computerized tomography (CT) and/or positron emission tomography–computerized tomography (PET–CT). All operations were performed by gynecologic oncologists and all pathologic specimens were evaluated by gynecopathologists.
Tumor size was defined as the largest tumor diameter in the uterine cervix after fixation in paraffin block and defined as the largest tumor diameter determined during pelvic examination for patients who received neoadjuvant chemotherapy. The deep stromal invasion was defined as a tumor invading the outer half of the cervical stroma. Lymphovascular space invasion (LVSI) was defined as the presence of tumoral cells or cell clusters within a luminal space of lymphatic channels or a vascular space that was stained with hematoxylin and eosin (H&E) in the pathologic sections containing both tumor and the surrounding healthy tissue. Tumor positivity within a 0.5 cm border of the pathological specimen was acknowledged as surgical border involvement. Vaginal involvement was identified based on the detection of a tumor elsewhere in the vaginal region. All these definitions were made according to the final paraffin section. Uterine invasion was defined as the endometrial and/or myometrial spread of the disease above the internal cervical ostium. Decisions regarding postoperative adjuvant therapy were taken by the tumor board.
Follow-up after adjuvant therapy was performed every 3 months for the first 2 years, then every 6 months until 5 years, then annually after 5 years, entering a routine surveillance program. When recurrence was suspected, patients underwent advanced imaging techniques (MRI, CT and PET–CT).
Statistical analysis
The time from surgery to the first recurrence of the disease or last contact was defined as recurrence-free survival (RFS). Disease-specific survival (DSS) was calculated from the date of surgery to the date of disease-specific death or last contact. RFS and DSS estimates were determined using the Kaplan–Meier method. Survival curves were compared using the log-rank test. Multivariate analysis could not be performed due to an insufficient number of patients in the sample. Statistical analyses were performed using SPSS version 20.0 (SPSS Inc, Chicago IL, USA). The cut-off for statistical significance was set at p-value < 0.05.
Results
Patient’s characteristics
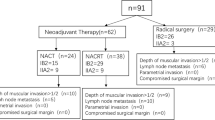
The mean age of the study group was 53.5 ± 11.595 years. The most histopathological type was endocervical AC–usual type in 36 (56.2%) patients. The median tumor size was 30 mm (range 8–72 mm). According to the FIGO 2014 criteria, 44 (68.8%) patients were at stage IB1, 13 (20.3%) patients were at stage IB2, six (9.4%) patients were at stage IIA1, and one (1.6%) patient was at stage IIA2. Only one (1.6%) patient received neoadjuvant chemotherapy. Sixty-one (95.3%) patients underwent type III radical hysterectomy. Parametrial involvement was seen in 14 (21.9%) patients, surgical border involvement in 14 (21.9%) patients, lymphovascular space invasion in 27 (42.2%) patients, deep cervical stromal invasion in 44 (68.8%) patients and uterine spread in 16 (25%) patients. Ovarian metastases were detected in four (6.2%) patients. The clinicopathological and surgical characteristics are presented in Table 1.
The median number of removed lymph nodes was 54 (range 13–113). Lymph node metastasis was detected in 20 (31.2%) patients. Thirteen patients had only pelvic lymph node metastasis, whereas both pelvic and paraaortic metastases were seen in seven patients. None of the patients had isolated paraaortic lymph node metastasis. The median number of metastatic lymph nodes was 4 (range 1–19) (Table 1).
Thirty-four (53.1%) patients received adjuvant radiotherapy, 18 patients underwent concurrent chemoradiotherapy, and two patients received curative-intent chemotherapy followed by radiotherapy. Twelve patients underwent only radiotherapy. For two patients who received adjuvant radiotherapy, there were insufficient clinical data regarding the type of radiotherapy.
Survival analysis
The median follow-up period was 41 months (range 1–235 months). During this period, recurrence was seen in nine (14.1%) patients and two (3.1%) patients died of the disease. The 5-year RFS and 5-year DSS rates were 83% and 98%, respectively. Single-site recurrence was detected in six patients, whereas three patients had multiple-site recurrence. Recurrences were limited to only within the pelvic region in four patients. Five patients had recurrences in extrapelvic regions, which were pulmonary and upper abdomen recurrences in all cases. Extrapelvic recurrence rate was 11% in endocervical type–usual type and 3.6% across the other types; however, this difference was not statistically significant (p = 0.265). Data on histopathology and recurrence patterns are shown in Table 2.
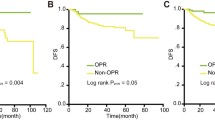
Since only two patients died because of disease, univariate analysis could not be performed to define the factors that affect DSS. Survival analysis was performed only for RFS. Univariate analysis showed that tumor size, stage and uterine spread were significantly related to RFS, whereas age, histopathologic subtype, adjuvant therapy and type of adjuvant radiotherapy, parametrial involvement, surgical border invasion, deep cervical stromal invasion, lymphovascular space invasion, lymph node metastasis and number of removed lymph nodes were not (Table 3).
An increase in tumor size was associated with a decrease in RFS. The 5-year RFS rate was 100% for patients with tumor size < 20 mm, but decreased to 88% for tumor sizes ≥ 20 mm– < 40 mm and 60% in patients with a tumor size of ≥ 40 mm (p = 0.017) (Fig. 1). The 5-year RFS rates for stages IB1 and IB2 were 91% and 65%, respectively (p = 0.022). The uterine invasion was significantly related to RFS. The 5-year RFS rate was 90% in patients without uterine spread but declined to 62% in the presence of uterine tumor spread (p = 0.034) (Table 3).
Discussion
In this study, we aimed to describe the clinical, pathological and surgical characteristics that affect survival in early-stage (IB1–IIA2) cervical AC patients who had undergone Piver–Rutledge type II/III radical hysterectomy and lymphadenectomy. Our results show 5-year RFS and DSS rates of 83% and 98%, respectively. Due to the low number of deaths in our cohort, no information could be given about prognostic factors affecting DSS. Recurrence was observed in 14.1% of the patients. More than half of the recurrences in our study were in the extrapelvic region (56%; n:5/9), including pulmonary and upper abdominal sides. Tumor size, stage and uterine spread were identified as prognostic factors for RFS in the univariate analysis.
In patients who undergo surgery at an early stage of cervical AC, studies have identified 5-year RFS rates of 50.2% in the presence of any one of the following prognostic factors; parametrial invasion, pelvic lymph node metastasis, a positive surgical margin, deep stromal invasion, lymphovascular space invasion, or large tumor size (˃ 4 cm) and 93.5% in patients without any risk factors [19]. Different prognostic factors for RFS were described in surgically treated cervical AC [12, 20, 21]. Mabuchi et al. reported that stage, tumor size and lymphovascular space invasion were significantly associated with a progression-free survival at stage IB–IIB AC subgroup, Park et al. found that parametrial involvement and lymph node metastasis were significant factors for RFS in AC at stage IA2–IIA and Kasamatu et al. suggested that infiltration to the vagina and lymph node metastasis could represent independent factors for relapse in patients with AC at stage I–IIB [12, 20, 21]. In our study, RFS was significantly affected by tumor size, stage and uterine spread, based on univariate analysis and the 5-year RFS rate was 83% for the entire cohort. The determination of different prognostic factors in each study may be due to the different clinical characteristics of the study cohorts as well as the fact that heterogeneous nature of the AC with different subgroups. However, the increasing incidence of AC makes the effects of histopathological type on prognosis important, whereas the same treatment algorithm has been applying with SCC [11]. Therefore, determining the clinicopathological factors specific to AC may be useful in guiding histology-based treatment.
Most authors have concluded that increased tumor size and advanced stages are related to reduced RFS rates in early-stage surgically treated AC and different survival outcomes were reported [20, 22, 23]. Baek et al. reported a 5-year RFS rate of 89% at stage 1B1 and found that tumor size was significantly associated with RFS in univariate analysis. They also identified 5-year RFS rates of 92% and 83% in patients with tumor sizes of ≤ 2 cm and > 2 cm, respectively [22]. Similar results were confirmed in our study, RFS significantly decreases as tumor size increases: whereas the 5-year RFS rate in our sample was 91% in patients with tumor size ≤ 4 cm (stage 1B1), it was only 65% in patients with tumor size > 4 cm (stage 1B2). Additionally, we identified a 5-year RFS rate of 100% with tumor size ˂2 cm. Better RFS in cases with tumor size < 2 cm in early-stage AC may be evaluated together with other surgicopathological factors, allowing establishing a nomogram for the patient and histology-based conservative treatment.
In cervical cancer, invasion of parametrium, upper vagina, bladder or rectum is associated with the FIGO stage. Loco-regional tumor extension to the adjacent organs is associated with decreased survival in cervical cancer. Cervical cancer may spread to the uterine corpus via direct invasion, and women in whom the tumors extended to the uterine corpus show significantly worse survival outcomes than their counterparts without corpus invasion [24, 25]. However, the FIGO staging system disregard the extension of the uterine corpus. Matsuo et al. reported that the 5-year DSS rate of patients with uterine invasion was 75% in stage 1B1 and 67% in 1B2. Additionally, they found that non-squamous histology, including AC, was an independent risk factor for uterine corpus tumor invasion [24]. A further study has also identified AC was an independent risk factor for uterine corpus invasion, revealed that AC is more likely to extend upward to the uterine corpus [26]. In another study, the distant recurrence was common in patients with myometrial invasion ≥ 50% [25]. In our study, uterine involvement was shown to be related to poor 5-year RFS rates of 62% and 90% in patients with and without uterine spread, respectively. Although uterine corpus invasion not included in surgicopathologic factors that are used for the decision of postoperative adjuvant therapy, results from our study and the other reported studies support the inclusion of the uterine invasion as a prognostic factor in cervical AC [9, 24,25,26].
AC predominantly disseminates hematogeneously; thus, it tends to involve higher rates of distant metastasis in a patient with cervical cancer [27]. Lee et al. reported that patients with stage IB–IIA cervical AC treated with radical hysterectomy with or without adjuvant radiotherapy, the recurrence rate was 14.4%, and the distant recurrence rate was 45% in recurrent patients [28]. In our study, tumors recurred 14% of patients and 56% of them were distant metastasis, including pulmonary and upper abdominal sides. Due to the rarity of AC, studies involving adenocarcinomas have not analyzed the different histological subtypes separately, so there were few available data of compared survival findings [9]. Although the number of patients per subgroup in our study was quite low, no association was identified between histologic subtypes and recurrences.
Radical hysterectomy and pelvic lymphadenectomy with definitive radiotherapy or concurrent chemoradiotherapy are recommended in the treatment guidelines for early-stage cervical cancer [11]. Regardless of histological subtype, radiotherapy and CCRT are used as adjuvant therapy for cervical cancer according to pathological risk factors. However the role of adjuvant therapy on survival in early cervical cancer and optimal treatment approaches are still debated and some studies recommended adjuvant treatment according to risk groups [29]. Many studies have reported that AC is more radioresistant than SCC [15, 30, 31]. Landoni et al. reported that patients with AC treated with radical hysterectomy had better survival than those treated with radiotherapy [30]. In our study, adjuvant therapy was not shown to have any effect on RFS rates, and also, the type of adjuvant radiotherapy was not shown to have an effect on RFS rates. These findings suggest that AC is resistant to postoperative radiotherapy. A study conducted by Huang et al. showed that 5-year RFS rates were not different between adjuvant concurrent chemoradiotherapy and radiotherapy group in high-risk AC group [31]. Seki et al. reported that adjuvant radiotherapy/concurrent chemoradiotherapy was ineffective for patients with AC at stage IB–IIB and offers adjuvant systemic chemotherapy [32].
The main limitations of our study were its retrospective design and a limited number of patients from a single center. On the other hand, uniform study cohort was created with the inclusion of only surgically treated patients with cervical AC. Histopathological evaluation was performed by a single team of experienced gynecologic pathologists. All operations were performed by an experienced gynecologist oncologist team, and comprehensive surgical staging procedure performed in a standard way in all study cases are the strong aspects of this study.
In conclusion, stage, tumor size and uterine spread are prognostic factors for recurrences in our study. AC has distinctive characteristics; thus, risk stratifications, including uterine spread, in addition to other risk factors may especially be useful for patients with AC who underwent radical hysterectomy. Prognostic factors should be determined to tailor the histology-based treatment in AC and to define the efficacy of histopathological subtypes on prognosis. To clarify this, further multicentric prospective studies are needed.
Data availability
Data will be provided if asked.
References
The online GLOBOCAN database is accessible at http://gco.iarc.fr/, as part of IARC’s Global Cancer Observatory. 2018. Accessed 17 Mar 2021
Gadducci A, Guerrieri ME, Cosio S (2014) Adenocarcinoma of the uterine cervix: pathologic features, treatment options, clinical outcome and prognostic variables. Crit Rev Oncol Hematol 135:103–114
Gien LT, Beauchemin MC, Thomas G (2010) Adenocarcinoma: a unique cervical cancer. Gynecol Oncol 116(1):140–146
Stolnicu S, Hoang L, Soslow RA (2019) Recent advances in invasive adenocarcinoma of the cervix. Virchows Arch 475(5):537–549
Vandenbroucke L, Robert A-L, Lavoué V, Foucher F, Henno S, Levêque J (2013) L’adénocarcinome du col utérin: particularités diagnostiques et thérapeutiques. J Gynecol Obstet Biol Reprod 42(3):207–216
Kim H, Cho WK, Kim YJ, Kim YS, Park W (2020) Significance of the number of high-risk factors in patients with cervical cancer treated with radical hysterectomy and concurrent chemoradiotherapy. Gynecol Oncol 157(2):423–428
Gülseren V, Kocaer M, Çakır İ, Özdemir İA, Sancı M, Güngördük K (2020) Postoperative nomogram for the prediction of disease-free survival in lymph node-negative stage I-IIA cervical cancer patients treated with radical hysterectomy. J Obstet Gynaecol 40(5):699–704
Singh P, Tripcony L, Nicklin J (2012) Analysis of prognostic variables, development of predictive models, and stratification of risk groups in surgically treated FIGO early-stage (IA-IIA) carcinoma cervix. Int J Gynecol Cancer 22(1):115–122
Kato T, Watari H, Takeda M, Hosaka M, Mitamura T, Kobayashi N, Sudo S, Kaneuchi M, Kudo M, Sakuragi N (2013) Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy. J Gynecol Oncol 24(3):222–228
Widschwendter P, Janni W, Scholz C, De Gregorio A, De Gregorio N, Friedl TWP (2019) Prognostic factors for and pattern of lymph-node involvement in patients with operable cervical cancer. Arch Gynecol Obstet 300(6):1709–1718
Abu-Rustum NR, Yashar CM, Bean S, Bradley K, Campos SM, Chon HS, Chu C, Cohn D, Crispens MA, Damast S, Fisher CM, Frederick P, Gaffney DK, Giuntoli R, Han E, Huh WK, Lurain Iii JR, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Sisodia R, Tillmanns T, Ueda S, Urban R, Wyse E, McMillian NR, Motter AD (2020) NCCN guidelines insights: cervical cancer, version 1.2020. J Natl Compr Canc Netw 18(6):660–666
Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH (2010) Outcomes after radical hysterectomy in patients with early-stage adenocarcinoma of uterine cervix. British J Cancer 102:1692–1698
Galic V, Herzog TJ, Lewin SN, Neugut AI, Burke WM, Lu YS, Hershman DL, Wright JD (2012) Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol Oncol 125(2):287–291
Cao L, Wen H, Feng Z, Han X, Wu X (2019) Distinctive clinicopathologic characteristics and prognosis for different histologic subtypes of early cervical cancer. Int J Gynecol Cancer 29(8):1244–1251
Zhou J, Zhang WW, Wu SG, He ZY, Sun JY, Yang GF, Li FY (2017) The prognostic value of histologic subtype in node-positive early-stage cervical cancer after hysterectomy and adjuvant radiotherapy. Int J Surg 44:1–6
Aslan K, Haberal A, Akıllı H, Meydanli MM, Ayhan A (2021) Prognostic value of the number of the metastatic lymph nodes in locally early-stage cervical cancer: squamous cell carcinoma versus non-squamous cell carcinoma. Arch Gynecol Obstet 304(5):1279–1289
Roma AA, Fadare O (2018) The pattern is the issue: recent advances in adenocarcinoma of the uterine cervix. Virchows Arch 472(6):897–905
Kurman RJ, Carcangiu ML, Herrington CS, Young RH (eds) (2014) WHO classification of tumours of female reproductive organs, 4th edn. Lyon, International Agency for Research on Cancer
Mabuchi S, Okazawa M, Kinose Y, Matsuo K, Fujiwara M, Suzuki O, Morii E, Kamiura S, Ogawa K, Kimura T (2012) Comparison of the prognoses of FIGO stage I to stage II adenosquamous carcinoma and adenocarcinoma of the uterine cervix treated with radical hysterectomy. Int J Gynecol Cancer 22(8):1389–1397
Mabuchi Y, Yahata T, Kobayashi A, Tanizaki Y, Shiro M, Ota N, Yagi S, Minami S, Ino K (2015) Clinicopathologic factors of cervical adenocarcinoma stages IB to IIB. Int J Gynecol Cancer 25(9):1677–1682
Kasamatsu T, Onda T, Sawada M, Kato T, Ikeda S, Sasajima Y, Tsuda H (2009) Radical hysterectomy for FIGO stage I-IIB adenocarcinoma of the uterine cervix. British J Cancer 100(9):1400–1405
Baek MH, Park JY, Kim D, Suh D-S, Kim J-H, Kim Y-M, Kim Y-T, Nam J-H (2014) Comparison of adenocarcinoma and adenosquamous carcinoma in patients with early-stage cervical cancer after radical surgery. Gynecol Oncol 135(3):462–467
Chargui R, Damak T, Khomsi F, Hassouna JB, Chaieb W, Hechiche M, Gamaudi A, Boussen H, Benna F, Rahal K (2006) Prognostic factors and clinicopathologic characteristics of invasive adenocarcinoma of the uterine cervix. Am J Obstet Gynecol 194(1):43–48
Matsuo K, Machida H, Blake EA, Takiuchi T, Mikami M, Roman LD (2017) Significance of uterine corpus tumor invasion in early-stage cervical cancer. Eur J Surg Oncol 43(4):725–734
He F, Li W, Liu P, Kang S, Sun L, Zhao H, Chen X, Yin L, Wang L, Chen J, Fan H, Li P, Yang H, Wang F, Chen C (2020) Influence of uterine corpus invasion on prognosis in stage IA2-IIB cervical cancer: A multicenter retrospective cohort study. Gynecol Oncol 158(2):273–281
Li W, He F, Liu P, Duan H, Ni Y, Wang S, Lin L, Yin Z, Chen X, Yin L, Wang L, Liu Y, Luan Z, Chen C (2021) Uterine corpus invasion in cervical cancer: a multicenter retrospective case-control study. Arch Gynecol Obstet 303(3):777–785
Jung EJ, Byun JM, Kim YN, Lee KB, Sung MS, Kim KT, Jeong DH (2017) Cervical adenocarcinoma has a poorer prognosis and a higher propensity for distant recurrence than squamous cell carcinoma. Int J Gynecol Cancer 27(6):1228–1236
Lee YY, Choi CH, Kim TJ, Lee JW, Kim BG, Lee JH, Bae DS (2011) A comparison of pure adenocarcinoma and squamous cell carcinoma of the cervix after radical hysterectomy in stage IB-IIA. Gynecol Oncol 120(3):439–443
Scharl S, Becher C, Gerken M, Scharl A, Anapolski M, Ignatov A, Inwald EC, Ortmann O, Kölbl O, Klinkhammer-Schalke M, Papathemelis T (2021) Is there a benefit for adjuvant radio(chemo)therapy in early cervical cancer? Results from a population-based study. Arch Gynecol Obstet 304(3):759–771
Landoni F, Maneo A, Zapardiel I, Zanagnolo V, Mangioni C (2012) Class I versus class III radical hysterectomy in stage IB1-IIA cervical cancer. A prospective randomized study. Eur J Surg Oncol 38(3):203–209
Huang YT, Wang CC, Tsai CS, Lai CH, Chang TC, Chou HH, Lee SP, Hong JH (2012) Clinical behaviours and outcomes for adenocarcinoma or adenosquamous carcinoma of cervix treated by radical hysterectomy and adjuvant radiotherapy or chemoradiotherapy. Int J Radiat Oncol Biol Phys 84(2):420–427
Seki T, Tanabe H, Nagata C, Suzuki J, Suzuki K, Takanao H, Isonishi S, Ochiai K, Takakura S, Okamoto A (2017) Adjuvant therapy after radical surgery for stage IB-IIB cervical adenocarcinoma with risk factors. Jpn J Clin Oncol 47(1):32–38
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
YD: project development, data collection, manuscript writing/editing,surgical and medical practices; CC: data collection or processing, surgical and medical practices; KF: data collection, literature search; UM: data collection, literature search; KC: data collection, literature search, surgical and medical practices; KCG: analysis and interpretation, surgical and medical practices; KV: analysis and interpretation,literature search, surgical and medical practices; TO: surgical and medical practices, analysis and interpretation; TT: project development, surgical and medical practices, analysis and interpretation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
Local Committee of Ethics of Etlik Zubeyde Hanim Women’s Health Care, Training and Research Hospital, University of Health Sciences approved the study with the number of 11/2019.
Informed consent
Written informed consent was obtained from all patients on admission for medical information to be used anonymously for academic purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yüksel, D., Çakır, C., Kılıç, F. et al. Oncologic outcomes of patients with FIGO 2014 stage IB-IIA cervical adenocarcinoma who underwent radical surgery. Arch Gynecol Obstet 306, 1657–1664 (2022). https://doi.org/10.1007/s00404-022-06507-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06507-2