Abstract
Objective
To determine the accuracy of uterine corpus invasion (UCI) diagnosis in patients with cervical cancer and identity risk factors for UCI and depth of invasion.
Methods
Clinical data of patients with cervical cancer who underwent hysterectomy between 2004 and 2016 were retrospectively reviewed. UCI was assessed on uterine pathology. Independent risk factors for UCI and depth of invasion were identified using binary and ordinal logistic regression models, respectively.
Results
A total of 2,212 patients with cervical cancer from 11 medical institutions in China were included in this study. Of these, 497 patients had cervical cancer and UCI, and 1,715 patients had cervical cancer and no UCI, according to the original pathology reports. Retrospective review of the original pathology reports revealed a missed diagnosis of UCI in 54 (10.5%) patients and a misdiagnosis in 36 (2.1%) patients. Therefore, 515 patients with cervical cancer and UCI (160 patients with endometrial invasion, 176 patients with myometrial invasion < 50%, and 179 patients with myometrial invasion ≥ 50%), and 1697 patients with cervical cancer without UCI were included in the analysis. Older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, resection margin involvement, and lymph node metastasis were independent risk factors for UCI. These risk factors, except resection margin involvement, were independently associated with depth of UCI.
Conclusions
UCI may be missed or misdiagnosed in patients with cervical cancer on postoperative pathological examination. Older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, resection margin involvement, and lymph node metastasis were independent risk factors for UCI and depth of UCI, with the exception of resection margin involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the fourth most common cancer in women [1]. Globally, in 2018, there were an estimated 569,847 new cases of cervical cancer and 311,365 deaths from the disease [2]. Most new cases and deaths occur in low-income and middle-income countries [3].
Uterine corpus invasion (UCI) occurs when cervical cancer extends upwards into the uterine corpus [4]. Currently, the International Federation of Gynecology and Obstetrics (FIGO) staging system disregards UCI. However, increasing evidence shows that UCI is associated with decreased survival in patients with cervical cancer [5,6,7,8,9,10,11]. Previous studies estimate the incidence of UCI at 4.9–26.2%, showing great variability. An important limitation of these studies is the lack of a consistent diagnostic and pathological definition of UCI [5,6,7,8,9,10,11].
The objectives of this multicenter retrospective case–control study were to determine the accuracy of UCI diagnosis in patients with cervical cancer and identify the risk factors for UCI and depth of invasion. UCI was identified from a retrospective review of uterine pathology.
Methods
Patients
Patient data were extracted from a multicentre clinical diagnosis and treatment database of cervical cancer in China (International Clinical Trials Registry Platform Search Port, http://apps.who.int/trialsearch/; CHiCTR1800017778). The database included 46,313 patients with cervical cancer admitted for surgery or radiotherapy to 37 medical institutions in mainland China between January 1, 2004 and December 31, 2016 [12,13,14].
Approval for the use of patient pathology data was obtained from 11 of the 37 medical institutions. Patients from these 11 institutions were included in the present study if they met the following criteria: (1) histological diagnosis of cervical cancer according to the 2009 FIGO staging system; (2) had undergone hysterectomy; and (3) postoperative pathological reports showing presence or absence of UCI were available. Patients with no hematoxylin-and-eosin-stained pathology specimens were excluded.
Patients were divided into two groups according to the original pathology reports: cervical cancer with UCI, and cervical cancer without UCI. To eliminate the influence of year on the diagnosis of UCI, patients diagnosed in the same year were allocated to the two groups in a 1:3 ratio, and the extent of UCI found on hematoxylin-and-eosin-stained pathology specimens was reviewed.
This study was approved by the Institutional Review Board of Nanfang Hospital Affiliated with Southern Medical University (NFEC-2017-135). The study was conducted in accordance with the 1964 Declaration of Helsinki and its subsequent revisions. The study used previously collected clinical data. Therefore, the need for informed consent was waived.
Definition and pathology review
Retrospective review of hematoxylin-and-eosin-stained uterine tissue specimens was performed independently by two pathologists who were blinded to the original pathology reports, and a consensus diagnosis was reached.
On pathology, UCI was defined as the extension of the primary cervical cancer above the anatomical internal os of the cervix with endometrial glands and stroma clearly visible in the area invaded by the tumor [4, 15, 16].
Depth of UCI was classified as endometrial invasion, myometrial invasion < 50%, or myometrial invasion ≥ 50%, according to the deepest point of invasion within the uterine corpus.
Variables
In addition to the presence/absence of UCI and depth of UCI, the following clinical and pathological covariates were recorded: age, stage, tumor size, histologic type, histologic grade, neoadjuvant therapy, surgical approach, stromal invasion depth, lymphovascular space invasion (LVSI), parametrial involvement (PMI), resection margin involvement (RMI), and lymph node (LN) metastasis.
Statistical analysis
Statistical analyses were performed using SPSS v24.0 (IBM Inc, Chicago, IL, USA). Comparisons were made between patients with cervical cancer with and without UCI. Categorical variables were compared with the chi-squared test. Independent risk factors for UCI were identified using multivariate forward stepwise logistic regression models. Covariates were clinical and pathological variables with P < 0.1 on univariate analysis. Clinicopathological variables were selected a priori on the basis of their potential for affecting UCI. Independent risk factors for depth of UCI were identified using ordinal logistic regression models.
A subgroup analysis that included patients who had not received neoadjuvant therapy was performed to clarify the association between neoadjuvant therapy and UCI.
Two-sided p-values < 0.05 were considered statistically significant.
Results
Patient characteristics
Patient selection is shown in Fig. 1. A total of 46,313 patients were identified by the multicenter clinical diagnosis and treatment database of cervical cancer in China. Among the 11 institutions that provided approval for the use of patient pathology data, 17,508 patients underwent hysterectomy and 630 (3.6%) patients had cervical cancer with UCI, according to the original pathology reports. Patients were allocated to two groups in a 1:3 ratio (n = 630, cervical cancer with UCI: n = 1,890, cervical cancer without UCI). Subsequently, 133 patients with cervical cancer with UCI and 175 patients with cervical cancer without UCI were excluded due to missing data. Ultimately, a total of 2,212 patients met the criteria for inclusion in this study. The original pathology reports revealed that 497 patients with cervical cancer had UCI, and 1,715 patients with cervical cancer had no UCI. Subsequent review of hematoxylin-and-eosin-stained uterine tissue specimens was performed by two pathologists according to our prespecified definition of UCI. Compared to the original pathology reports, a second review of uterine corpus and cervix pathology showed that missed diagnosis of UCI occurred in 54/1,715 (10.5%) patients with cervical cancer without UCI, according to the original pathology reports, and misdiagnosis of UCI occurred in 36/497 (2.1%) patients with cervical cancer with UCI, according to the original pathology reports. This revealed that 515 patients with cervical cancer had UCI, and 1,697 patients with cervical cancer had no UCI (Table 1).
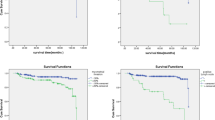
The detailed characteristics of the 2,212 patients included in this study are summarized in Supplementary Table 1. According to uterine corpus pathology, 515 patients had UCI, including 160 (31.0%) patients with endometrial invasion, 176 (34.2%) patients with myometrial invasion < 50%, and 179 (34.8%) patients with myometrial invasion ≥ 50% (Fig. 2). Compared to patients with cervical cancer and no UCI, those with UCI were significantly older (p < 0.001), had a significantly larger tumor size (p < 0.001), and were significantly more likely to have advanced stage disease (p < 0.001), adenocarcinoma (p < 0.001), Grade 1 or 2 disease (p = 0.009), stromal invasion depth > 1/2 (p = 0.001), PMI (p < 0.001), RMI (p = 0.001), or LN metastasis (p < 0.001) (Table 2).
Hematoxylin–eosin staining of uterine tissue specimens. Arrows represent infiltrate related to cervical carcinoma in different parts of the uterine corpus. a cervical squamous cell carcinoma; b cervical adenocarcinoma; c uterine corpus without tumor invasion; d endometrial invasion; e myometrial invasion < 50%; f myometrial invasion ≥ 50%
Risk factors for UCI and invasion depth
On multivariate binary logistic regression analysis, older age (50–59 versus < 50 years, aOR 1.681; ≥ 60 versus < 50 years, aOR 2.670), advanced stage (IIB versus ≤ IA2-IB, aOR 1.576; III-IV versus ≤ IA2-IB, aOR 3.458), tumor size (unknown versus ≤ 2, aOR 2.500), adenocarcinoma (aOR 2.271), parametrial involvement (aOR 2.078), resection margin involvement (aOR 1.840), and lymph node metastasis (aOR 1.647) were independent risk factors for UCI (Table 3).
On ordinal logistic regression analysis, these risk factors, except RMI, were independently associated with depth of UCI (Table 4).
Subgroup analysis
A total of 1,848 patients did not receive neoadjuvant therapy, including 434 patients with cervical cancer and UCI and 1414 patients with cervical cancer and no UCI. Among the women with UCI, 136 (31.3%) patients had endometrial invasion, 156 (36.0%) patients had myometrial invasion < 50%, and 142 (32.7%) patients had myometrial invasion ≥ 50%. On multivariate binary logistic regression analysis, older age (50–59 versus < 50 years, aOR 1.535; and ≥ 60 versus < 50 years, aOR 2.377), advanced stage (IIB versus ≤ IA2-IB, aOR 1.904; III–IV versus ≤ IA2-IB, aOR 15.541), tumor size (unknown versus ≤ 2, aOR 2.451), adenocarcinoma (aOR 2.040), parametrial involvement (aOR 1.876), and lymph node metastasis (aOR 1.562) were independent risk factors for UCI (Supplementary Table 2).
On ordinal logistic regression analysis, these risk factors were independently associated with depth of UCI (Supplementary Table 3).
A total of 1,267 patients diagnosed at stages IA2, IB1 and IIA1 did not receive neoadjuvant therapy, including 270 patients with cervical cancer and UCI and 997 patients with cervical cancer and no UCI. Among the women with UCI, 97 (35.9%) patients had endometrial invasion, 98 (36.3%) patients had myometrial invasion < 50%, and 75 (27.8%) patients had myometrial invasion ≥ 50%. On multivariate binary logistic regression analysis, older age (50–59 versus < 50 years, aOR 1.529; and ≥ 60 versus < 50 years, aOR 2.456), tumor size (unknown versus ≤ 2, aOR 3.399), histologic type (adenocarcinoma versus squamous cell carcinoma, aOR 1.782; and others or unknown versus squamous cell carcinoma, aOR 2.851), parametrial involvement (aOR 3.018), and lymph node metastasis (aOR 1.422) were independent risk factors for UCI (Supplementary Table 4).
On ordinal logistic regression analysis, these risk factors were independently associated with depth of UCI (Supplementary Table 5). Findings from the subgroup analyses were consistent with the primary analysis.
Discussion
This multicentre retrospective case–control study determined the accuracy of UCI diagnosis and the risk factors associated with the presence and depth of UCI in patients with cervical cancer. Presence and depth of UCI were identified from a retrospective review of hematoxylin-and-eosin-stained uterine tissue specimens. Retrospective review of the original pathology reports according to our prespecified definition of UCI revealed a missed diagnosis of UCI in 54 (10.5%) patients and a misdiagnosis in 36 (2.1%) patients.
Previous studies have described UCI in cervical cancer, estimating the incidence at 4.9–26.2% [5,6,7,8,9,10,11]. These studies were limited as the estimates were not based on pathological criteria. In clinical practice, tumor extension to the uterine corpus is likely missed or misdiagnosed by pathologists as it is disregarded by the FIGO staging system.
The present study revealed that older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, resection margin involvement, and lymph node metastasis were independent risk factors for UCI. Among these, adenocarcinoma is more likely to extend upward to the uterine corpus compared to squamous cell carcinoma. Adenocarcinoma of the cervix originates close to the uterine corpus in the endocervical glands, while squamous cell carcinoma arises in the ectocervix. UCI has been associated with lymph node metastasis in previous studies [11, 17]. Current NCCN guidelines do not recommend routine para-aortic lymphadenectomy as part of radical surgery due to the very low rate of para-aortic lymph node metastasis in early stage cervical cancer [18, 19]. In the current study, only 180 (8.1%) patients underwent para-aortic lymphadenectomy and 10 (0.5%) patients underwent para-aortic lymph node biopsy. Due to the small sample size, data describing pelvic and para-aortic lymph node involvement were analyzed together. Lymph node metastasis was identified as an independent risk factor for UCI, but the effect of para-aortic lymph node metastasis could not be evaluated. The current study also demonstrated that advanced stage, including IIB and III-IVA, were associated with UCI. However, according to the NCCN guideline, radical surgery was not recommended, and the optimal treatment strategy was concurrent chemoradiotherapy [18]. Furthermore, multivariate binary logistic regression analysis revealed that the variable of “unknown tumor size” was an independent risk factor for UCI, but “known tumor size” was not. Therefore, in this model, tumor size would not have practical significance. This result may be due to bias caused by the small sample size. Alternatively, large tumor size may be difficult to measure and prone to missing data.
To the author’s knowledge, the present study is the first to identify older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, and lymph node metastasis as independent risk factors affecting depth of UCI [5, 10, 11]. Several previous studies revealed that cervical cancer extension to the corpus was associated with decreased survival and distant metastasis in patients with early stage cervical cancer, including a large retrospective cohort study involving 17,074 patients [11]. However, one previous study reported no association between UCI and survival in patients with cervical cancer [10]. Previous studies did not consider the effect of depth of tumor invasion within the uterine corpus on survival in cervical cancer, which may explain these inconsistent results. In the present study, among the 11 included institutions, no pathologists reported depth of UCI on their patients’ medical records. Further research on the effect of depth of UCI on patient survival is warranted to inform clinical practice.
Findings from our study revealed that neoadjuvant therapy was not associated with UCI. Cervical cancer involves the uterine corpus by direct extension rather than blood borne or lymphatic metastasis; thus, the effect of neoadjuvant therapy on UCI may not be apparent due to the large quantity of locally spreading tumor cells [20,21,22,23,24]. Our subgroup analysis excluded the influence of preoperative neoadjuvant therapy on postoperative pathological risk factors for UCI. Consistent with the primary analysis, older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, and lymph node metastasis were independent risk factors for UCI in patients who did not receive neoadjuvant therapy. Resection margin involvement was not identified as a risk factor in these patients, possibly due to the limited number of patients with resection margin involvement in this subgroup analysis.
This was a large-scale cohort study that identified risk factors for UCI and depth of invasion in patients with cervical cancer; however, it had several limitations. First, this was a non-randomized retrospective study with potential for patient and institution selection bias. Second, findings from this study may not be generalizable to patients and institutions across China and in other geographical locations. Third, the data should be interpreted with caution as odds ratios exaggerate effect sizes compared to relative risk. Finally, the objective of the current study was to investigate the accuracy of UCI diagnosis and the risk factors for UCI and depth of invasion in cervical cancer. Patient outcomes associated with UCI and depth of invasion were not investigated, but may be studied in future research.
In conclusion, findings from this study reveal UCI may be missed or misdiagnosed in patients with cervical cancer on postoperative pathological examination. Older age, advanced stage, tumor size, adenocarcinoma, parametrial involvement, resection margin involvement, and lymph node metastasis were independent risk factors for UCI and depth of UCI, with the exception of resection margin involvement.
References
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R (2018) Cancer of the cervix uteri. Int J Gynaecol Obstet 143(Suppl 2):22–36. https://doi.org/10.1002/ijgo.12611
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 68 (6):394–424. doi:https://doi.org/10.3322/caac.21492
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393(10167):169–182. https://doi.org/10.1016/S0140-6736(18)32470-X
Hoogduin KJ, Hopman AN, Ramaekers FC, McCluggage WG, Smedts F (2013) BCL2 and keratin 5 define the uterine-cervix-isthmus junction, a transition between endocervical and tubal-like epithelium. Int J Gynecol Pathol 32(1):122–130. https://doi.org/10.1097/PGP.0b013e318253c6f6
Noguchi H, Shiozawa I, Kitahara T, Yamazaki T, Fukuta T (1988) Uterine body invasion of carcinoma of the uterine cervix as seen from surgical specimens. Gynecol Oncol 30(2):173–182. https://doi.org/10.1016/0090-8258(88)90021-2
Perez CA, Zivnuska F, Askin F, Kumar B, Camel HM, Powers WE (1975) Prognostic significance of endometrial extension from primary carcinoma of the uterinecervix. Cancer 35(6):1493–1504. https://doi.org/10.1002/1097-0142(197506)35:6%3c1493::aid-cncr2820350603%3e3.0.co;2-m
Perez CA, Camel HM, Askin F, Breaux S (1981) Endometrial extension of carcinoma of the uterine cervix: a prognostic factor that may modify staging. Cancer 48(1):170–180. https://doi.org/10.1002/1097-0142(19810701)48:1%3c170::aid-cncr2820480128%3e3.0.co;2-0
Grimard L, Genest P, Girard A, Gerig L, Prefontaine M, Drouin P, Nair RC, Stats M (1988) Prognostic significance of endometrial extension in carcinoma of the cervix. Gynecol Oncol 31(2):301–309. https://doi.org/10.1016/s0090-8258(88)80008-8
Boyce J, Fruchter RG, Nicastri AD, Ambiavagar PC, Reinis MS, Nelson JH Jr (1981) Prognostic factors in stage I Carcinoma of the cervix. Gynecol Oncol 12(2 Pt 1):154–165. https://doi.org/10.1016/0090-8258(81)90145-1
Kato T, Watari H, Takeda M, Hosaka M, Mitamura T, Kobayashi N, Sudo S, Kaneuchi M, Kudo M, Sakuragi N (2013) Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy. J Gynecol Oncol 24(3):222–228. https://doi.org/10.3802/jgo.2013.24.3.222
Matsuo K, Machida H, Blake EA, Takiuchi T, Mikami M, Roman LD (2017) Significance of uterine corpus tumor invasion in early-stage cervical cancer. Eur J Surg Oncol 43(4):725–734. https://doi.org/10.1016/j.ejso.2017.01.017
Li W, Liu P, Zhao W, Yin Z, Lin Z, Bin X, Lang J, Chen C (2020) Effects of preoperative radiotherapy or chemoradiotherapy on postoperative pathological outcome of cervical cancer–from the large database of 46,313 cases of cervical cancer in China. Eur J Surg Oncol 46(1):148–154. https://doi.org/10.1016/j.ejso.2019.09.188
Liang C, Liu P, Cui Z, Liang Z, Bin X, Lang J, Chen C (2020) Effect of laparoscopic versus abdominal radical hysterectomy on major surgical complications in women with stage IA-IIB cervical cancer in China, 2004–2015. Gynecol Oncol 156(1):115–123. https://doi.org/10.1016/j.ygyno.2019.10.032
Zhang W, Chen C, Liu P, Li W, Hao M, Zhao W, Lu A, Ni Y (2019) Staging early cervical cancer in China: data from a multicenter collaborative. Int J Gynecol Cancer . https://doi.org/10.1136/ijgc-2019-000263
Standring S (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. In, vol 29. vol 2, 41th edn. Elsevier, London, p 1295
Mills SE (2012) Histology for Pathologists. In., 4th edn. Lippincott williams & Wilkins, Philadelphia, p 1084
Narayan K, Fisher RJ, Bernshaw D (2008) Patterns of failure and prognostic factor analyses in locally advanced cervical cancer patients staged by magnetic resonance imaging and treated with curative intent. Int J Gynecol Cancer 18(3):525–533. https://doi.org/10.1111/j.1525-1438.2007.01050.x
Koh WJ, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, Chon HS, Chu C, Clark R, Cohn D, Crispens MA, Damast S, Dorigo O, Eifel PJ, Fisher CM, Frederick P, Gaffney DK, Han E, Huh WK, Lurain JR, Mariani A, Mutch D, Nagel C, Nekhlyudov L, Fader AN, Remmenga SW, Reynolds RK, Tillmanns T, Ueda S, Wyse E, Yashar CM, McMillian NR, Scavone JL (2019) Cervical Cancer, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network : JNCCN 17 (1):64–84. doi:https://doi.org/10.6004/jnccn.2019.0001
Matsuo K, Shimada M, Saito T, Takehara K, Tokunaga H, Watanabe Y, Todo Y, Morishige KI, Mikami M, Sugiyama T (2018) Risk stratification models for para-aortic lymph node metastasis and recurrence in stage IB-IIB cervical cancer. J Gynecol Oncol 29(1):e11. https://doi.org/10.3802/jgo.2018.29.e11
Katsumata N, Yoshikawa H, Kobayashi H, Saito T, Kuzuya K, Nakanishi T, Yasugi T, Yaegashi N, Yokota H, Kodama S, Mizunoe T, Hiura M, Kasamatsu T, Shibata T, Kamura T, Japan Clinical Oncology G (2013) Phase III randomised controlled trial of neoadjuvant chemotherapy plus radical surgery vs radical surgery alone for stages IB2, IIA2, and IIB cervical cancer: a Japan Clinical Oncology Group trial (JCOG 0102). Br J Cancer 108(10):1957–1963. https://doi.org/10.1038/bjc.2013.179
Zhang H, Peng W, Zhang Y (2014) Detection of cell apoptosis in pelvic lymph nodes of patients with cervical cancer after neoadjuvant chemotherapy. J Int Med Res 42(3):641–650. https://doi.org/10.1177/0300060513506328
Rydzewska L, Tierney J, Vale CL, Symonds PR (2012) Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev 12:CD007406. doi:https://doi.org/10.1002/14651858.CD007406.pub3
de la Torre M (2018) Neoadjuvant chemotherapy in woman with early or locally advanced cervical cancer. Rep Pract Oncol Radiother 23(6):528–532. https://doi.org/10.1016/j.rpor.2018.09.005
Zhang T, Kong W, Li F, Song D, Liu T, Han C, Jiao S, Chen J (2016) Effect of preoperative radiotherapy on stage IB2 and IIA2 cervical cancer: A retrospective cohort study. Int J Surg 30:63–67. https://doi.org/10.1016/j.ijsu.2016.04.001
Acknowledgements
We would like to thank the Department of Pathology at 11 medical institutions in mainland China for their support in this study, including the Second Hospital of ShanXi Medical University, the Second Affiliated Hospital of Zhengzhou University, the Fourth Hospital of Hebei Medical University, Shanxi Cancer Hospital, Anyang Cancer Hospital, Anhui Cancer Hospital, Yuncheng Central Hospital of Shanxi province, People’s Hospital of Guizhou Province, the Affiliated Yantai Yuhuangding Hospital of Qingdao University, the Fifth Affiliated Hospital of Southern Medical University, and Maternal and Child Health Hospital of Guizhou Province. Furthermore, we thank Medjaden Bioscience Limited for scientific editing of this manuscript.
Funding
This study was supported by the National Science and Technology Support Program of China (2014BAI05B03), the National Natural Science Fund of Guangdong (2015A030311024) and the Science and Technology Plan of Guangzhou (158100075).
Author information
Authors and Affiliations
Contributions
WLL: project development, study design and manuscript writing. FJH: project development, study design and manuscript writing. PL: project development, study design and data analysis. HD: project development, study design and data analysis. WLL, FJH, PL and HD are equal first author contribution status. YN: project development. SGW: project development. LHL: project development. ZHY: data collection, management. XLC: data collection, management. LY: data collection, management. LXW: provide clinical expertise and supervision. YPL: provide clinical expertise and supervision. ZHL: provide clinical expertise and supervision. CLC: project development, study design and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, W., He, F., Liu, P. et al. Uterine corpus invasion in cervical cancer: a multicenter retrospective case–control study. Arch Gynecol Obstet 303, 777–785 (2021). https://doi.org/10.1007/s00404-021-05968-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-05968-1