Abstract
Purpose
To clarify the prognostic value of the number of metastatic lymph nodes (mLNs) in squamous and non-squamous histologies among women with node-positive cervical cancer.
Methods
One hundred ninety-one node-positive cervical cancer patients who had undergone radical hysterectomy plus systematic pelvic and para-aortic lymphadenectomy followed by concurrent radiochemotherapy were retrospectively reviewed. The prognostic value of the number of mLNs was investigated in squamous cell carcinoma (SCC) v (n = 148) and non-SCC (n = 43) histologies separately with univariate log-rank test and multivariate Cox regression analyses.
Results
In SCC cohort, mLNs > 2 was significantly associated with decreased 5-year disease-free survival (DFS) [hazard ratio (HR) = 2.06; 95% confidence interval (CI) 1.03–4.09; p = 0.03) and overall survival (OS) (HR = 2.35, 95% CI 1.11–4.99; p = 0.02). However mLNs > 2 had no significant impact on 5-year DFS and 5-year OS rates in non-SCC cohort (p = 0.94 and p = 0.94, respectively). We stratified the entire study population as SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups. Thereafter, we compared survival outcomes. The non-SCC group had worse 5-year OS (46.8% vs. 85.3%, respectively; p < 0.001) and 5-year DFS rates (31.6% vs. 82.2%, respectively; p < 0.001) when compared to those of the SCC group with mLNs ≤ 2. However, the non-SCC group and the SCC group with mLNs > 2 had similar 5-year OS (46.8% vs. 65.5%, respectively; p = 0.16) and 5-year DFS rates (31.6% vs. 57.5%, respectively; p = 0.06).
Conclusion
Node-positive cervical cancer patients who have non-SCC histology as well as those who have SCC histology with mLNs > 2 seem to have worse survival outcomes when compared to women who have SCC histology with mLNs ≤ 2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymph node (LN) metastasis is an important adverse prognosticator for cervical cancer and detected in 15.3–25.5% of patients who have 2009 International Federation of Gynecology and Obstetrics (FIGO) stage IB-IIA disease [1, 2]. Nevertheless, the status of the LNs was not considered in the FIGO staging system till 2018. In 2018 the staging system for cervical cancer was revised by the FIGO Committee and LN metastasis was defined as stage IIIC disease [3].
Previous studies reported that women with node-positive cervical cancer had 5-year overall survival (OS) rates between 62.0 and 81.9% [4, 5]. It was argued that these patients were a heterogeneous group with certain clinic-pathologic risk factors for relapse and survival [5,6,7]. Tumor histology is among one of the most important risk factors considered. It is well-known that squamous cell carcinoma (SCC) and adenocarcinoma (AC) histologies exhibit similar prognosis in node-negative patients, whereas AC histology is related with worse prognosis in patients who are node-positive [8, 9]. Additionally, the number of metastatic lymph nodes (mLNs) has been proposed as a prominent prognostic factor in patients who have node-positive cervical cancer [5, 7, 10]. However, the prognostic significance of the number of mLNs has not been delineated in specific histologic types of cervical cancer.
This retrospective dual-institutional study presents the experience in patients who uniformly received radical hysterectomy plus systematic pelvic and para-aortic LN dissection followed by concurrent radiochemotherapy. The purpose of this study is to clarify the prognostic value of the number of mLNs in various histological types of node-positive cervical cancer. Therefore, the prognostic significance of the number of mLNs was investigated in stage IIIC patients with SCC histology and stage IIIC patients with non-SCC histology separately.
Methods
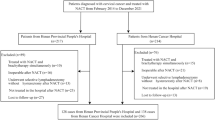
The cervical cancer patients who were subjected to radical hysterectomy with bilateral pelvic and para-aortic lymphadenectomy between January 1st, 2006 and May 6th, 2019 at two gynecologic oncology centers in Ankara, Turkey were retrospectively reviewed after the approval of Institutional Review Board (Başkent University Institutional Review Board Approval Number: KA 19/427).
We included women who met the following criteria: (1) FIGO stage IIIC (p) cervical cancer, (2) SCC, AC or adenosquamous carcinoma, (3) no neo-adjuvant therapy, (4) no synchronous malignancy. Women who had no complete medical records, those who had less than 10 pelvic LNs and less than five para-aortic LNs on their final pathology reports, and those who did not complete standard adjuvant radiochemotherapy were excluded.
We obtained the following data from medical records of patients; age at diagnosis, 2009 FIGO stage, 2018 FIGO stage, lymphovascular space invasion (LVSI) (absent/present), stromal invasion depth, vaginal involvement (absent/present), microscopic parametrial involvement (absent/present), primary tumor size (cm), positive surgical margin (absent/present), number of LNs removed, location of LNs involved, size of the mLNs > 1 cm (yes/no) and number of mLNs. The number of mLNs was categorized as mLNs ≤ 2 and mLNs > 2 according to previously published studies [5, 10, 11]. Also, the date of surgery, type of adjuvant therapy, the recurrence status, and the date of last visit or death, were abstracted.
Cervical biopsy and pelvic examination were the essential components of the pre-operative work-up. A pelvic ultrasound or MRI (Magnetic Resonance Imaging) was applied to all women in order to guide the treatment plan. Cystoscopy and rectoscopy were performed when clinically indicated. A radical hysterectomy with pelvic and para-aortic lymphadenectomy was planned for the women with 2009 FIGO stage IB-IIA disease [12]. After the emerging of the 2018 FIGO staging system, we routinely used MRI or PET-CT (positron-emission tomography) to assess LNs [3]. Thereafter, primary chemoradiation was planned for women with positive nodes on imaging.
All the patients underwent abdominal Piver type III hysterectomy with bilateral pelvic and para-aortic LN dissection. Pelvic and para-aortic lymphadenectomy was performed as we described in our previous study [13]. Intraoperative frozen section examination for detecting nodal disease was not routinely requested. The attending surgeon decided whether to request a frozen section examination for suspicious LNs or not. In the case of a frozen-section analysis indicating positive nodal disease, radical hysterectomy was abandoned. Additionally, the surgical procedure was terminated if intra-peritoneal disease was detected during surgery.
Gynecological pathologists examined the surgical specimens and used conventional pathology for diagnosis. The data regarding the histopathological features were extracted from the original pathology reports and central pathology review was not performed. LVSI was described as the existence of tumor cells inside the lumen of the lymphatics or capillaries [14]. The histologic subtype of cervical cancer was determined according to the World Health Organization (WHO) classification system [15]. The patients were allocated to the FIGO 2018 stages based on their final pathology reports.
Adjuvant treatment of the patients was decided by the multidisciplinary tumor board at each institution. Whole pelvic external beam radiation therapy (EBRT) was administered at a dose of 45–50 Gy to the patients who had pelvic LN metastasis. During course of EBRT patients received systemic cisplatin (40 mg/m2) weekly. Chemoradiation was administered to all cases those who had para-aortic LN metastasis on final pathology. By employing a four field arrangement in the pelvis and, anterior and posterior fields in the para-aortic area, extended-field radiotherapy delivered 45–50 Gy to the pelvis and para-aortic area over 5 weeks at 1.8–2 Gy per fraction. During the period of extended-field radiotherapy, cisplatin (40 mg/m2) infusion was applied once-weekly. If there was vaginal involvement, vaginal brachytherapy was administered to the patients. Cylinders were employed to deliver vaginal brachytherapy to the upper 4 cm of the residual vagina. Three fractions of high dose rate brachytherapy of 7 Gy every other day, was prescribed to 0.5 cm from the surface of the applicator.
Recurrence was defined as pathological or radiological confirmation of tumor metastasis after three months disease-free period following primary surgery. Disease-free survival (DFS) was defined as the period between the date of initial surgery and first recurrence, death from any cause, or the date of last follow-up for women without any event. The duration between the date of initial surgery and death, or the last visit was regarded as OS. The women were categorized into two cohorts according to tumor histology as patients with SCC or patients with non-SCC. The non-SCC cohort consisted of adenosquamous carcinoma and AC histologies. The prognostic value of mLN count was determined in each of the cohorts separately.
We carried out the statistical analysis by employing the SPSS version 23.0 statistical software (IBM Corp., Armonk, NY, USA). Continuous variables were given as medians and ranges and categorical variables were reported in terms of counts and percentages. The continuous variables were compared with student’s t test whereas Chi-square test was utilized to compare the categorical variables. Furthermore, we employed Kaplan Meier method to form survival curves and the long-rank test to document the difference between survival curves. Multivariate analysis was applied to each variable which exhibited p value of less than 0.05 in the univariate analysis. Multivariate analysis was performed by using the Cox proportional hazard model. For all analysis p < 0.05 was regarded as statistically significant.
Results
Patient characteristics
This study includes a total of 191 women with FIGO stage IIIC (p) cervical cancer. Among these women 148 (77.5%) had SCC and 43 (22.5%) had non-SCC histology. The SCC and non-SCC cohorts were well balanced with regard to median age at diagnosis, 2018 FIGO stages, 2009 FIGO stages, LVSI, depth of cervical stromal invasion, vaginal involvement, microscopic parametrial involvement, tumor size, positive surgical margin, and the duration of median follow-up. The median number of removed pelvic, para-aortic and total lymph node numbers was similar between the groups. The two cohorts were also comparable in terms of parametrial, obturator, common iliac, presacral and external iliac LN metastasis. Sixty-five patients (43.9%) in the SCC cohort had mLNs > 2, and 24 (55.8%) patients in the non-SCC cohort had mLNs > 2 (p = 0.22). Table 1 demonstrates the clinical and pathological characteristics of the patients. We analyzed the prognostic value of the number of mLNs for patients with SCC histology and non-SCC histology separately.
SCC cohort
In the SCC cohort, we compared the baseline characteristics of women with mLNs ≤ 2 and mLNs > 2. The women with mLNs > 2 were more likely to have FIGO stage IIIC2 disease (27/65 vs .7/83, respectively; p < 0.01), external iliac LN metastasis (48/65 vs . 30/83, respectively; p < 0.01), common iliac LN metastasis (13/65 vs .1/83, respectively; p < 0.01) and presacral LN metastasis (6/65 vs .0/83, respectively; p < 0.01) than those with mLNs ≤ 2.
Univariate analysis revealed that the FIGO stage IIIC2 disease (p = 0.04), tumor size ≥ 4 cm (p = 0.04) and mLNs > 2 (p = 0.005) were significantly related with decreased 5-year DFS. On multivariate analysis, mLNs > 2 remained as the only factor that was significantly associated with decreased 5-year DFS (hazard ratio [HR] = 2.06; 95% confidence interval [CI] 1.03–4.09; p = 0.03) (Table 2).
Univariate analyses revealed that there was no factor other than mLNs > 2 that significantly related to decreased 5-year OS (HR = 2.35, 95% CI 1.11–4.99; p = 0.02). As there was only one factor related to decreased 5-year OS, we did not perform multivariate analysis (Table 3).
Non-SCC cohort
In the non-SCC cohort, we compared the baseline characteristics of women with mLNs ≤ 2 and mLNs > 2. The women with mLNs > 2 were more likely to have FIGO stage IIIC2 disease (14/24 vs.1/19, respectively; p < 0.01), LVSI (24/24 vs.15/19, respectively; p = 0.03), external iliac LN metastasis (17/24 vs.11/19, respectively; p < 0.01), obturator LN metastasis (21/24 vs.10/19, respectively; p = 0.01) and size of the mLNs > 1 cm (24/24 vs.9/19, p < 0.01) than those patients with mLNs ≤ 2.
Univariate analysis revealed that vaginal involvement (p = 0.02), microscopic parametrial involvement (p = 0.001), primary tumor size ≥ 4 cm (p = 0.02) and 2009 FIGO stage II disease (p = 0.03) were significantly associated with decreased 5-year DFS. However, on multivariate analysis, no independent prognostic factor was defined (Table 4).
Univariate analysis revealed that vaginal involvement (p = 0.006), presacral LN metastasis (p = 0.01) and FIGO stage II disease (p = 0.01) were significantly related with decreased 5-year OS. However, on multivariate analysis, no independent prognostic factor was defined (Table 5).
Effect of tumor histology and number of mLNs on survival for the whole study population
We grouped the patients with SCC histology based on the number of mLNs as mLNs ≤ 2, and mLNs > 2. However, we did not stratify the patients with non-SCC histology because the number of mLNs was not a prognostic factor for survival outcome in non-SCC cohort according to the results of our study. Thereafter we analyzed the baseline characteristics and survival outcomes of SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups.
There was no statistically significant difference between the groups in terms of age at diagnosis, LVSI, depth of cervical stromal invasion, vaginal involvement, microscopic parametrial involvement, tumor size, positive surgical margin, parametrial LN metastasis, obturator LN metastasis and the duration of median follow-up. However, the SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups were significantly different with regard to FIGO stage IIIC2 disease (27/65, 7/83, 15/43, respectively; p < 0.01), external iliac LN metastasis (48/65, 30/83, 28/43, respectively; p < 0.01) common iliac LN metastasis (13/65, 1/83, 8/43, respectively; p < 0.01), presacral LN metastasis (6/65, 0/83, 3/43, respectively; p = 0.02) and size of the mLNs > 1 cm (48/65, 48/83, 33/43, respectively; p = 0.04).
During the study period, 41 (21.4%) women had recurrent disease. In the SCC group with mLNs ≤ 2, there were three (3.6%) vaginal vault, two (2.4%) pelvic, three (3.6%) lymphatic, two (2.4%) distant relapses. In the SCC group with mLNs > 2, there were four (6.2%) vaginal vault, two (3.1%) pelvic, six (9.2%) lymphatic, three (4.6%) distant and one (1.5%) vaginal vault plus pelvic relapses. The recurrence locations in the non-SCC group as follows; three (7.0%) vaginal vault, four (9.3%) pelvic, three (7%) lymphatic, four (9.3%) distant, one (2.3%) lymphatic plus distant. At the time of reporting 142 women were alive and 49 were dead.
The 5-year DFS rates were 82.2% for the SCC group with mLNs ≤ 2, 57.5% for the SCC group with mLNs > 2 and 31.6% for non-SCC group (Fig. 1). The results of pairwise comparisons revealed that the SCC group with mLNs ≤ 2 had better 5-year DFS rate when compared to the SCC group with mLNs > 2 (82.2% vs. 57.5%, respectively; p = 0.005), and the non-SCC group (82.2% vs. 31.6%, respectively; p < 0.001). Nevertheless, the SCC group with mLNs > 2 and the non-SCC group were comparable in terms of 5-year DFS rates (57.5% vs. 31.6%, respectively; p = 0.06).
Kaplan–Meier curves for DFS according SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups (SCC with mLNs ≤ 2 vs. SCC with mLNs > 2, p = 0.005; SCC with mLNs ≤ 2 vs. non-SCC, p < 0.001; SCC with mLNs > 2 vs. non-SCC, p = 0.06) DFS disease-free survival, mLNs metastatic lymph nodes, SCC squamous cell carcinoma
The 5-year OS rates were 85.3% for the SCC group with mLNs ≤ 2, 65.5% for the SCC group with mLNs > 2 and 46.8% for the non-SCC group (Fig.2). The results of pairwise comparisons revealed that the SCC group with mLNs ≤ 2 had a better 5-year OS rate when compared to the SCC group with mLNs > 2 (85.3% vs. 65.5%, respectively; p = 0.02), and the non-SCC group (85.3% vs. 46.8%, respectively; p < 0.001). Nevertheless, the SCC group with mLNs > 2 and the non-SCC group were similar in terms of 5-year OS rates (65.5% vs. 46.8%, respectively; p = 0.16).
Kaplan–Meier curves for OS according SCC with mLNs ≤ 2, SCC with mLNs > 2, and non-SCC groups (SCC with mLNs ≤ 2 vs. SCC with mLNs > 2, p = 0.02; SCC with mLNs ≤ 2 vs. non-SCC, p < 0.001; SCC with mLNs > 2 vs. non-SCC, p = 0.16) OS overall survival, mLNs metastatic lymph nodes, SCC squamous cell carcinoma.
Discussion
Our study revealed that mLNs > 2 was not a prognostic factor in the non-SCC cohort, whereas it was independently associated with decreased 5-year DFS and 5-year OS rates in the SCC cohort. Furthermore, when the study population was classified as SCC with mLNs ≤ 2, SCC with mLNs > 2 and non-SCC, the SCC group with mLNs ≤ 2 had better survival outcomes when compared to the other two groups. To our knowledge, this study is the first to investigate the prognostic value of metastatic LN count with regard to histologic subtype in a node-positive cervical cancer population who underwent standard surgical and adjuvant treatment.
However, there are some shortcomings in the current study. The retrospective design makes the study susceptible to selection and referral bias and the absence of central pathologic review limits the data integrity between the participating centers. Small sample size of the non-SCC group is another limitation of our study.
Lymphadenectomy is a component of the surgical management of cervical cancer. Systematic lymphadenectomy is useful for tailoring adjuvant treatment and predicting prognosis [3]. Therefore, the thoroughness of lymphadenectomy is crucial for decreasing the risk of occult lymphatic metastasis. The total LN count was proposed as an indicator of quality control for pelvic LN dissection procedure in the surgical management of cervical cancer [16]. However, the minimum number of LNs for considering lymphadenectomy as adequate is still debatable. European Organization for Research and Treatment of Cancer–Gynecological Cancer Group has indicated that resection of more than 11 pelvic LNs as one of the quality indicators of surgical treatment for cervical cancer [17]. Very recently, European Society of Gynaecological Oncology quality indicators for surgical management of cervical cancer have been published [18]; however, there was no information regarding the number of LNs to be harvested for describing a lymphadenectomy as systematic. In this study, we included only patients with more than 10 pelvic and five para-aortic LNs on their final pathology report in order to maintain a minimum standard for surgical quality.
Adjuvant chemoradiation following radical hysterectomy and systematic lymphadenectomy is currently recommended in women with positive LN, microscopic parametrial involvement, or a positive surgical margin [19]. However, combined treatment with radical hysterectomy and radiotherapy was associated with increased morbidity [20]. The European Society of Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology Guidelines for the Management of Patients with Cervical Cancer recommended intraoperative assessment of LN status with a frozen section [21]. If mLN is detected, they have recommended abandoning radical hysterectomy to avoid morbidity [21]. However, there are only a few retrospective studies that directly compared the outcomes of women in whom radical hysterectomy was aborted or completed in early-stage node-positive cervical cancer [22,23,24,25]. In a Surveillance Epidemiology and End Results (SEER) analysis, Richard et al. [26] included 218 stage IB cervical cancer patients who received pelvic and para-aortic lymphadenectomy and reported positive LN. Among these patients, 163 had undergone radical hysterectomy while radical hysterectomy was abandoned in 55 women. The results of this study revealed that the radical hysterectomy completed and abandoned groups had similar five-year survival (69% vs. 71%, respectively, p = 0.46). Phanedra et al. [27] assessed the value of a routine intraoperative frozen section examination of pelvic LNs in early-stage cervical cancer and reported 86.7% sensitivity and 100% specificity. Despite the success rates, the authors did not suggest a routine frozen section examination of LNs as it was time-consuming, expensive, and not available in all centers.
On the other hand, clinical management of LNs in early-stage cervical cancer varies widely among gynecologic oncologists. A survey study evaluated the practice patterns of Society of Gynecologic Oncology (SGO) members concerning intraoperative management of LNs in early-stage cervical cancer [28]. It has been reported that only 38.6% of the responders preferred routine intraoperative frozen section examination for LNs. Of those, only 21% preferred to cancel radical hysterectomy when an isolated metastatic microscopic LN detected. In another survey study, Gubbala et al. [29] addressed the approach of the British Gynaecological Cancer Society (BGCS) members to intraoperative frozen section examination of LNs in patients with cervical cancer. Only 12.5% of the responders stated that they routinely perform frozen examination. Similarly, in our study, the decision to perform a frozen section examination in an attempt to identify positive nodes was at the discretion of the attending surgeon. The radical hysterectomy was abandoned in the event of metastatic LN. In order to standardize the study population, we did not include women whose radical hysterectomy was canceled as a result of the frozen section analysis.
The LN status was incorporated into the recently revised FIGO staging system in order to emphasize the importance of the nodal metastasis [3]. Patients with metastatic LN either detected by imaging (r) or histopathology (p) were classified as stage IIIC [3]. The 2018 FIGO staging system permits to perform any of CT (computed tomography), MRI, or PET-CT to detect nodal disease [3]. However, both CT and MRI suffer from low sensitivity. In a meta-analysis [30] that evaluated the diagnostic performances of imaging modalities, it was reported that CT had a sensitivity of 57% and a specificity of 91%. MRI showed a sensitivity of %52 and a specificity of 94% [30]. The PET-CT is more accurate than CT or MRI in the detection of mLNs with a sensitivity of 66% and specificity of 97% [30]. Although the diagnostic performance of the imaging modalities is sufficient to spare many patients from an unnecessary lymphadenectomy, histology-proven LN metastasis still seems to be the gold standard in assessing nodal status [31]. Avoiding the double morbidity of radiation and surgery in the case of positive LNs should be the main goal of gynecologist oncologists while managing locally-early stage cervical cancer. It is clear that a Piver III operation followed by chemoradiation carries high morbidity without any survival benefit. However, it should be emphasized that most of the patients in the current study had undergone surgery before the 2018 FIGO staging system was introduced. The low sensitivity of the imaging techniques [30] as well as the lack of stage IIIC (r) in the previous FIGO staging system resulted in inappropriately staged lymph nodes in the pre-operative setting which seems to be the major limitation of our study.
The prognostic significance of mLN count, in different histologic subtypes of cervical cancer has been questioned in a limited number of studies. Liu et al. [10] analyzed the prognostic value of the number of mLNs in 60 pelvic LN positive SCC cases. They found out that the women with positive pelvic nodes ≤ 2 had better 5-year OS rates when compared to women with positive pelvic nodes > 2 (76% and 35%, respectively). However, it must be noted that the cases in this study underwent only pelvic lymphadenectomy. The omission of para-aortic lymphadenectomy might have resulted in underestimation of metastatic nodal disease. Furthermore, the Liu study represented the results of a heterogeneous population because neoadjuvant chemotherapy was administered to 50% of the study population.
Zhou et al. [7] utilized the database of the SEER and analyzed 2222 cervical cancer patients who had pathologically-confirmed positive LNs. The Zhou study revealed that positive-LNs > 2 was significantly associated with decreased OS and cause-specific survival (CSS) in cases who had SCC histology (CSS, p < 0.001; OS, p = 0.001) or adeno-squamous histology (CSS, p = 0.017; OS, p = 0.045). However, the number of positive-LNs was not a prognostic factor among patients with AC subtype (CSS, p = 0.215; OS, p = 0.184). Nevertheless, it should be emphasized that the SEER database has some limitations such as lack of information about the type of hysterectomy, the extent of lymphadenectomy, the use of neo-adjuvant chemotherapy, adjuvant treatment modalities, and the recurrence of disease.
Previous studies on node-positive cervical cancer have indicated poor prognosis for non-SCC histology when compared to SCC histology. Nakanishi et al. [8] reported that non-SCC histology was significantly related with decreased OS (HR = 2.86, 95% CI 1.60–5.09; p < 0.001) and DFS (HR = 2.33, 95% CI 1.34–4.05; p = 0.003) in the presence of LN metastasis. Similarly, Hosaka et al. [32] evaluated 108 patients with node-positive cervical cancer and showed that pure AC histology was an independent prognostic factor for decreased OS (HR = 4.0, 95% CI 0.11–0.55, p = 0.0005). Also, Zhou et al. [1] analyzed the SEER database and reported that AC histology exhibited a worse OS (HR = 1.474, 95% CI 1.114–1.951; p = 0.001) and CSS (HR = 1.614, 95% CI 1.114–1.951; p < 0.001) when compared to SCC histology in node-positive cervical cancer patients. Our study represents the survival outcomes of a uniform study population who underwent standard surgical and adjuvant treatment. According to our findings, regardless of the number of mLNs, the non-SCC group had worse 5-year OS (46.8% vs. 85.3%, respectively; p < 0.001) and 5-year DFS rates (31.6% vs. 82.2%, respectively; p < 0.001) when compared to those of the SCC group with mLNs ≤ 2. However, the non-SCC group and the SCC group with mLNs > 2 had similar 5-year OS (46.8% vs. 65.5%, respectively; p = 0.16) and 5-year DFS rates (31.6% vs. 57.5%, respectively; p = 0.06).
In the present study, we administered concurrent radiochemotherapy to all patients as the adjuvant therapy. However, our results imply that radiochemotherapy seemed to be insufficient for controlling the disease for the SCC group with mLNs > 2 and the non-SCC group. Therefore, new adjuvant treatment strategies other than concurrent radiochemotherapy may be adopted for the management of those patients. Radiotherapy with concurrent doublet chemotherapy based on cisplatin is one of the alternatives. In a meta-analysis, Petrelli et al. [32] demonstrated that concurrent cisplatin-based doublet chemotherapy was associated with significantly enhanced OS (OR 0.65; 95% CI 0.51–0.81; p = 0.0002) and progression-free survival (PFS) (OR 0.71; 95% CI 0.55–0.91; p = 0.006) when compared to weekly cisplatin plus radiotherapy. Concurrent consolidation chemotherapy after chemo-radiation may be another adjuvant treatment option for those patients. In a phase II study, Mabuchi et al. [33] assessed the prognostic value of the consolidation chemotherapy following concurrent carboplatin and paclitaxel plus pelvic radiotherapy in node-positive cervical cancer patients which were surgically treated. The results of the Mabuchi study revealed that this kind of adjuvant treatment was related with better PFS (p = 0.026) when compared to concurrent radiochemotherapy. Additionally, the authors [33] reported that consolidation chemotherapy following concurrent carboplatin and paclitaxel plus pelvic radiotherapy has resulted in better PFS (p = 0.0004) and OS (p = 0.034) when compared to radiotherapy alone.
In conclusion, we demonstrated that patients node-positive cervical cancer patients who had non-SCC histology, as well as those having SCC histology with mLNs > 2, had worse survival outcomes when compared to women who have SCC histology with mLNs ≤ 2.This new stratification might be helpful in predicting the prognosis and determining the choice of adjuvant treatment in patients with stage IIIC (p) cervical cancer. However, our results need to be validated in a prospective fashion.
Availability of data and material
Available on request of editor or reviewers.
References
Zhou J, Zhang WW, Wu SG et al (2017) The prognostic value of histologic subtype in node-positive early-stage cervical cancer after hysterectomy and adjuvant radiotherapy. Int J Surg 44:1–6. https://doi.org/10.1016/j.ijsu.2017.05.074
Sakuragi N, Satoh C, Takeda N et al (1999) Incidence and distribution pattern of pelvic and paraaortic lymph node metastasis in patients with Stages LB, IIA, and IIB cervical carcinoma treated with radical hysterectomy. Cancer 85:1547–1554. https://doi.org/10.1002/(SICI)1097-0142(19990401)85:7%3c1547::AID-CNCR16%3e3.0.CO;2-2
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R (2018) Cancer of the cervix uteri. Int J Gynecol Obstet 143:22–36. https://doi.org/10.1002/ijgo.12611
Hosaka M, Watari H, Mitamura T et al (2011) Survival and prognosticators of node-positive cervical cancer patients treated with radical hysterectomy and systematic lymphadenectomy. Int J Clin Oncol 16:33–38. https://doi.org/10.1007/s10147-010-0123-0
Yan DD, Tang Q, Tu YQ et al (2019) A comprehensive analysis of the factors of positive pelvic lymph nodes on survival of cervical cancer patients with 2018 FIGO stage IIIC1p. Cancer Manag Res 11:4223–4230. https://doi.org/10.2147/cmar.s204154
Park JY, Kim DY, Kim JH et al (2010) Further stratification of risk groups in patients with lymph node metastasis after radical hysterectomy for early-stage cervical cancer. Gynecol Oncol 117:53–58. https://doi.org/10.1016/j.ygyno.2009.12.006
Zhou J, Wu SG, Sun JY et al (2017) Incorporation of the number of positive lymph nodes leads to better prognostic discrimination of node-positive early stage cervical cancer. Oncotarget 8(16):26057–26065
Nakanishi T, Ishikawa H, Suzuki Y et al (2000) A comparison of prognoses of pathologic stage Ib adenocarcinoma and squamous cell carcinoma of the uterine cervix. Gynecol Oncol 79:289–293. https://doi.org/10.1006/gyno.2000.5935
Kodama J, Seki N, Masahiro S et al (2010) Prognostic factors in stage IB–IIB cervical adenocarcinoma patients treated with radical hysterectomy and pelvic lymphadenectomy. J Surg Oncol 101:413–417. https://doi.org/10.1002/jso.21499
Liu Y, Zhao LJ, Li MZ et al (2015) The number of positive pelvic lymph nodes and multiple groups of pelvic lymph node metastasis influence prognosis in stage IA–IIB cervical squamous cell carcinoma. Chin Med J (Engl) 128:2084–2089. https://doi.org/10.4103/0366-6999.161372
Zhou J, Zhang WW, Wu SG et al (2017) The impact of examined lymph node count on survival in squamous cell carcinoma and adenocarcinoma of the uterine cervix. Cancer Manag Res 9:315–322. https://doi.org/10.2147/CMAR.S141335
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105:103–104
Aslan K, Meydanli MM, Oz M et al (2020) The prognostic value of lymph node ratio in stage IIIC cervical cancer patients triaged to primary treatment by radical hysterectomy with systematic pelvic and para-aortic lymphadenectomy. J Gynecol Oncol. https://doi.org/10.3802/jgo.2020.31.e1
Sakuragi N, Takeda N, Hareyama H et al (2000) A multivariate analysis of blood vessel and lymph vessel invasion as predictors of ovarian and lymph node metastases in patients with cervical carcinoma. Cancer 88:2578–2583
Kurman RJ, Carcangiu ML, Herrington CS (2014) WHO classification of tumours of female reproductive organs. WHO press, 4th edn, vol 6
Pieterse QD, Kenter GG, Gaarenstroom KN et al (2007) The number of pelvic lymph nodes in the quality control and prognosis of radical hysterectomy for the treatment of cervical cancer. Eur J Surg Oncol 33:216–221. https://doi.org/10.1016/j.ejso.2006.09.037
Verleye L, Vergote I, Reed N et al (2009) Quality assurance for radical hysterectomy for cervical cancer: the view of the European Organization for Research and Treatment of Cancer-Gynecological Cancer Group (EORTC-GCG). Ann Oncol 20:1631–1638
Cibula D, Planchamp F, Fischerova D et al (2020) European Society of Gynaecological Oncology quality indicators for surgical treatment of cervical cancer. Int J Gynecol Cancer 30:3–14. https://doi.org/10.1136/ijgc-2019-000878
Peters WA, Liu PY, Barrett RJ et al (2000) Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol 18:1606–1613. https://doi.org/10.1200/JCO.2000.18.8.1606
Barter JF, Soong SJ, Shingleton HM et al (1989) Complications of combined radical hysterectomy-postoperative radiation therapy in women with early stage cervical cancer. Gynecol Oncol 32:292–296. https://doi.org/10.1016/0090-8258(89)90627-6
Cibula D, Pötter R, Planchamp F et al (2018) The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer. Radiother Oncol 127:404–416. https://doi.org/10.1016/j.radonc.2018.03.003
Potter ME, Alvarez RD, Shingleton HM et al (1990) Early invasive cervical cancer with pelvic lymph node involvement: to complete or not to complete radical hysterectomy? Gynecol Oncol 37:78–81. https://doi.org/10.1016/0090-8258(90)90312-9
Bremer GL, van der Putten HW, Dunselman GA, de Haan J (1992) Early stage cervical cancer: aborted versus completed radical hysterectomy. Eur J Obstet Gynecol Reprod Biol 47:147–151. https://doi.org/10.1016/0028-2243(92)90045-Z
Suprasert P, Srisomboon J, Charoenkwan K et al (2005) Outcomes of abandoned radical hysterectomy in patients with stages IB–IIA cervical cancer found to have positive nodes during the operation. Int J Gynecol Cancer 15:498–502. https://doi.org/10.1111/j.1525-1438.2005.15315.x
Gray HJ, Seifert E, Saly Rosas VG et al (2010) The abandoned radical hysterectomy for cervical cancer: clinical predictors and outcomes. Obstet Gynecol Int 2010:1–6. https://doi.org/10.1155/2010/743794
Richard SD, Krivak TC, Castleberry A et al (2008) Survival for stage IB cervical cancer with positive lymph node involvement: a comparison of completed vs. abandoned radical hysterectomy. Gynecol Oncol 109:43–48. https://doi.org/10.1016/j.ygyno.2007.12.002
Gubbala PK, Laios A, Wang Z et al (2016) Routine intraoperative frozen section examination to minimize bimodal treatment in early-stage cervical cancer. Int J Gynecol Cancer 26:1148–1153. https://doi.org/10.1097/IGC.0000000000000738
Garg G, Shah JP, Toy EP et al (2011) Intra-operative detection of nodal metastasis in early stage cervical cancer: a survey of the practice patterns of SGO members. Gynecol Oncol 121:143–147. https://doi.org/10.1016/j.ygyno.2010.12.337
Ganesan R, Brown LJR, Kehoe S et al (2013) The role of frozen sections in gynaecological oncology: survey of practice in the United Kingdom. Eur J Obstet Gynecol Reprod Biol 166:204–208. https://doi.org/10.1016/j.ejogrb.2012.10.024
Liu B, Gao S, Li S (2017) A comprehensive comparison of CT, MRI, positron emission tomography or positron emission tomography/CT, and diffusion weighted imaging-MRI for detecting the lymph nodes metastases in patients with cervical cancer: a meta-analysis based on 67 studies. Gynecol Obstet Invest 82:209–222
Zigras T, Lennox G, Willows K et al (2017) Early cervical cancer: current dilemmas of staging and surgery. Curr Oncol, Rep, p 19
Petrelli F, De Stefani A, Raspagliesi F et al (2014) Radiotherapy with concurrent cisplatin-based doublet or weekly cisplatin for cervical cancer: a systematic review and meta-analysis. Gynecol Oncol 134:166–171
Mabuchi S, Isohashi F, Yokoi T et al (2016) A phase II study of postoperative concurrent carboplatin and paclitaxel combined with intensity-modulated pelvic radiotherapy followed by consolidation chemotherapy in surgically treated cervical cancer patients with positive pelvic lymph nodes. Gynecol Oncol 141:240–246. https://doi.org/10.1016/j.ygyno.2016.02.011
Author information
Authors and Affiliations
Contributions
KA protocol/project development,data collection or management, data analysis, manuscript writing/editing, approved the version to be published. AH protocol/project development, manuscript writing/editing, approved the version to be published. HA data collection or management, manuscript writing/editing, approved the version to be published; MMM protocol/project development, data analysis, manuscript writing/editing, approved the version to be published. AA protocol/project development, manuscript writing/editing, approved the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval
The Institutional Review Board of Başkent University approved this study (IRB Approval Number:nKA 19/427).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aslan, K., Haberal, A., Akıllı, H. et al. Prognostic value of the number of the metastatic lymph nodes in locally early-stage cervical cancer: squamous cell carcinoma versus non-squamous cell carcinoma. Arch Gynecol Obstet 304, 1279–1289 (2021). https://doi.org/10.1007/s00404-021-06030-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06030-w