Abstract
Purpose
To compare the effectiveness of cervical ripening by a mechanical method (double-balloon catheter) and a pharmacological method (prostaglandins) in women with one previous cesarean delivery, an unfavorable cervix (Bishop score < 6), and a singleton fetus in cephalic presentation.
Methods
This retrospective study, reviewing the relevant records for the years 2013 through 2017, took place in two French university hospital maternity units. This study included women with one previous cesarean delivery, a liveborn singleton fetus in cephalic presentation, and intact membranes, for whom cervical ripening, with unfavorable cervix (Bishop score < 6) was indicated for medical reasons. It compared two groups: (1) women giving birth in a hospital that uses a protocol for mechanical cervical ripening by a double-balloon catheter (DBC), and (2) women giving birth in a hospital that performed pharmacological cervical ripening by prostaglandins. The principal endpoint was the cesarean delivery rate. The secondary outcome measures were maternal and neonatal outcomes.
Results
We compared 127 women with prostaglandin ripening to 117 women with DBC. There was no significant difference between the two groups for the cesarean rate (42.5% in the prostaglandin group and 42.7% in the DBC group; p = 0.973; crude OR 1.01 [0.61–1.68]; adjusted OR 1.55 [0.71–3.37]). The median interval between the start of ripening and delivery did not differ between the groups (28.7 h in the prostaglandin group vs 25.6 h in the DBC group; p = 0.880). Neonatal outcomes did not differ between the groups, either. There was one case of uterine rupture in the prostaglandin group, with no associated maternal or neonatal morbidity. There were no neonatal deaths. The postpartum hemorrhage rate was significantly higher in the DBC group.
Conclusion
For cervical ripening for women with one previous cesarean, the choice of a pharmacological or mechanical protocol does not appear to modify the mode of delivery or maternal or neonatal morbidity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The objective of cervical ripening is to modify the cervix to enable vaginal delivery for women whose cervix is unfavorable. The alternative is a planned cesarean delivery, which is associated with recognized risks of both short- and long-term neonatal and maternal morbidity [1, 2]. In women with a uterine scar, trial of vaginal delivery (VBAC, vaginal birth after cesarean) exposes the mother to the risk of uterine rupture and the fetus to the ensuing neonatal consequences [3]. Because of the rarity of this complication, however, trial of vaginal delivery is a reasonable option that is encouraged by various professional societies [4,5,6,7]. Although VBAC rates have dropped over time, the rates of successful trials of labor have remained constant, around 75% [3]. Accordingly, simultaneously increasing VBAC rates and decreasing complications related to multiple cesareans requires a reduction in the rates of planned cesarean and higher rates of planned vaginal deliveries. One step toward achieving these goals might be the planning of vaginal delivery even in cases of an unfavorable cervix, when fetal or maternal conditions indicate the need for delivery. Debate about the use of prostaglandins in women with a previous cesarean and an unfavorable cervix focuses around the risk of uterine rupture [8,9,10,11]. Methods of mechanical cervical ripening are a potential alternative as they result in fewer abnormalities in uterine dynamics. Nonetheless, the studies assessing mechanical methods have several biases that limit the interpretation of their results [12,13,14,15,16].
The objective of this study was to compare the effectiveness of cervical ripening by a mechanical method (double-balloon catheter) and by a pharmacological method (prostaglandins) in women with one previous cesarean delivery, an unfavorable cervix (Bishop score < 6), and a singleton fetus in cephalic presentation.
Materials and methods
Population
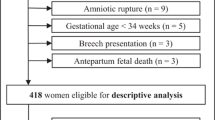
This retrospective study took place in two French university hospital maternity units (level III) and covered all women who met the inclusion criteria in 2014–2017, that is, if they had a history of one cesarean delivery and a subsequent live birth of a singleton fetus in cephalic presentation, regardless of term, after undergoing cervical ripening for a medical indication and an unfavorable cervix (Bishop score < 6). Accordingly, women were excluded if they had two or more previous cesareans, an in utero fetal death before labor, spontaneous rupture of the membranes, presentations other than cephalic, or multiple pregnancies, or when vaginal delivery was contraindicated (placenta previa, dystocic presentation). Because one maternity ward used a protocol for mechanical cervical ripening by a double-balloon catheter (DBC), and the other a protocol for pharmacological cervical ripening by prostaglandins, we compared the groups of women giving birth in each hospital.
Protocols of cervical ripening
The maternity ward using the DBC planned the mode of delivery for women with a previous cesarean during collective obstetric staff meetings at 36 weeks of gestation. A planned cesarean was performed at 39 weeks if estimated fetal weight exceeded 4500 g or if the woman had a history of uterine rupture. Trial of VBAC was proposed in all other situations, with the choice left to the woman, who could refuse it. The balloon used for cervical ripening is a double balloon (cervical ripening balloon, Cook OB/GYN, Spencer, IN, USA). An intern placed the DBC in the morning, in the labor room. Fetal heart rate (FHR) was monitored for 30 min before the placement. Each balloon was inflated with a quantity of sterile water, ranging from 10 to 80 ml as a function of maternal tolerance (pain). FHR was monitored continuously after placement for two hours, and the DBC was left in place for 24 h. FHR was monitored for 30 min that evening and then the next morning, before the DBC was removed.
If the membranes ruptured, the DBC was removed and expectant management adopted until the next morning for women whose 9th-month vaginal sample was negative for streptococci B. In women with streptococci B colonization, the team providing care could choose between immediate induction if the cervix was favorable or expectant management with antibiotic therapy (1 g amoxicillin every 8 h) until the next morning. In the case of poor maternal tolerance, the DBC could be deflated or even removed, but the induction would not continue until the next morning. The team also determined what action to take if the DBC was dislodged or lost. If the woman entered labor, the DBC was removed and she was transferred to the labor room. Otherwise, the DBC was removed the next morning, 24 h after placement, and the cervix was reassessed by digital cervical examination before the staff meeting so that a collective decision could be reached about the next steps. Either the cervix was favorable (that is, Bishop score ≥ 6) and induction continued by oxytocin, or it was unfavorable (Bishop score < 6), in which case there were two possibilities: continuation of induction by oxytocin, if the couple agreed, or immediate cesarean delivery.
The center using cervical ripening by prostaglandins also decided mode of delivery collectively, each morning, at the daily obstetric staff meeting, which considered the files of women between 36 and 38 weeks of gestation. The indications for planned cesareans were a history of uterine rupture, an abnormally narrow pelvis (transverse median < 10.5 cm, median conjugate < 9.5 cm, and interspinous diameter < 8.5 cm), an estimated fetal weight (EFW) of 4250–4500 g associated with abnormal pelvic measurements (transverse median < 11 cm, median conjugate < 10 cm, and interspinous diameter < 9 cm), or an EFW > 4500 g. First-line cervical ripening in this hospital was performed by PGE2 administered as an intracervical gel. The protocol of prostaglandin administration takes into account the fact that the uterus is scarred. Specifically, a dose of prostaglandins was administered daily for up to 7 consecutive days if the cervix remained unfavorable and in the absence of intercurrent events requiring emergency delivery, to aimed at inducing cervical ripening, but not labor at any cost. On days 1, 2, and 3, dinoprostone, 0.5 mg, was administered intracervically (Prepidil®); on day 4, misoprostol (Cytotec®) was administered intravaginally at a dose of 25 μg, and on days 5, 6, and 7, at a dose of 50 μg. Residents placed the prostaglandins in the morning in the labor room. Fetal heart rate was monitored continuously for 30 min before placement and was required to be normal. FHR monitoring continued for 2 h after administration. Thereafter, the woman could return to her hospital room if she had not entered labor and the FHR was normal. FHR was also monitored for 30 min each evening. If the cervix appeared favorable during this process, oxytocin was administered to induce labor.
After 7 days, if the woman had not entered spontaneous labor and the cervix remained unfavorable, the available alternatives were induction by oxytocin with an unripe cervix or an immediate cesarean.
In this hospital, an intern performed a routine manual uterine examination after delivery to ensure the integrity of the uterine scar. In the case of scar dehiscence or uterine rupture, surgical revision by laparotomy was considered only in cases of hemorrhage.
In the maternity ward performing mechanical cervical ripening, the women to be included were identified by the PMSI (discharge summary) code O34.2, and data were collected retrospectively from each medical file. All data had initially been collected prospectively at each prenatal visit and at delivery by the healthcare professionals managing the woman. In the department using pharmacological ripening, women were identified from the department's computer database. The entire medical file was computerized and was completed prospectively at each visit, at delivery, and during the postpartum period. All data were verified at the obstetrics staff meeting the day after the delivery. These medical records were reviewed individually and completely for women with uterine rupture, uterine dehiscence, or a pH < 7.0.
Statistical analyses
We collected the following data: the mothers' characteristics, any disease or disorders occurring during pregnancy, the methods used for cervical ripening, characteristics of labor and delivery, any complications of delivery, and neonatal characteristics.
The principal endpoint was the cesarean rate. The secondary outcome measures concerned mothers and babies. The secondary maternal outcomes were: mode of delivery, postpartum hemorrhage (defined by blood loss > 500 cc), time from the start of the cervical ripening procedure to both the start of labor and to delivery, and the occurrence of a uterine rupture, defined by complete rupture of the myometrium and serosa. The secondary perinatal outcome measures were death, FHR abnormalities during labor, umbilical artery pH at birth, the 5-min Apgar score, and intubation in the delivery room.
First, we studied the comparability of the two groups for maternal and obstetric characteristics. Then we conducted univariate analyses to compare the prostaglandin group and the DBC group for the principal endpoint and the secondary outcome measures. Finally we used a logistic regression model to perform a multivariate analysis for the principal endpoint. The model included the variables that differed significantly between the two groups in the univariate analysis (p < 0.2). The analyses were performed with Stata software version 13.0. We used Student’s t, χ2, and Fisher's exact tests for the univariate analyses.
This study was approved by the National Data Protection Authority (Commission Nationale de l’Informatique et des Libertes, CNIL no. 293683). Under French regulations, this study was exempt from Institutional Review Board approval because it was an observational study using anonymized data from medical records. Women were informed that their records could be used for the evaluation of medical practices and were allowed to opt out of these studies.
Results
This study included 244 women: 127 in the prostaglandin group and 117 in the DBC group. Compared with the prostaglandin group, the DBC group contained significantly more women younger than 30 years, who were nulliparous, had a normal body mass index (BMI), and a history of VBAC, and fewer with preexisting diabetes at pregnancy (Table 1). The groups did not differ for pregnancy complications, except that the prostaglandin group had a higher frequency of pregnancy-related hypertension.
The principal indications for this cervical preparation in the prostaglandin group were post-term status (22.0%) and oligohydramnios (22.8%), and in the DBC group post-term status (32.4%) (Table 2). The groups did not differ for mean gestational age at cervical ripening. In the prostaglandin group, 68 women (53.5%) received a single ripening agent, 24 (20.5%) two agents, and 35 (27.5%) at least three. The DBC was successfully placed in every case.
There were significantly more women with a long, closed cervix before cervical preparation in the prostaglandin group, and more improvement in cervical length in the DBC group.
During this procedure, the women in the prostaglandin group required more opioids than those in the DBC group (Table 3). Spontaneous labor occurred significantly more often in the prostaglandin group. The indications for induction of labor after cervical ripening were significantly different between the two groups: for the prostaglandin group, these indications were more often favorable cervix (68.2%) and FHR abnormalities (18.9%) and in the DBC group, favorable cervix (49.1%) and “on maternal request” (20.5%).
One emergency cesarean took place, for bradycardia, during DBC placement. This woman experienced significant pain during the placement and had a vasovagal syncope after inflation of the vaginal balloon; fetal bradycardia was recorded by FHR monitoring during this reaction.
Use of oxytocin was less frequent in the prostaglandin than the DBC group, and its mean duration of use was shorter. The maximum dose administered did not differ.
The principal endpoint did not differ significantly between the groups. The cesarean rate was 42.5% in the prostaglandin group and 42.7% in the DBC group (p = 0.97), crude OR 1.01 [0.61–1.68]. This did not change after adjustment for maternal age, BMI, parity, fetal macrosomia, indication for cervical ripening, cervical length, tone and opening before ripening: adjusted OR 1.56 [0.71–3.41]. However, after adjusting for confounders, although the association is non-significant, there is a higher risk of a cesarean section in the DBC group.
The rate of cesareans during labor was not significantly different between the two groups. But the indications of caesarean during labor significantly differed according to the group. Concerning the indications of caesarean during labor, there were significantly more cesareans for FHR abnormalities in the prostaglandin than in the DBC group. Significantly fewer women in the prostaglandin group went into labor or gave birth on the first day (Table 4). Nonetheless, the median time from the start of the cervical ripening procedure to both entry into labor and delivery did not differ significantly between the groups. The duration of labor was significantly shorter in the prostaglandin than in the DBC group (343 min (5 h 43 min) versus 515 min (8 h 35 min); p = 0.001). The same was true for each of the different phases of labor (Table 4).
There were significantly more postpartum hemorrhages in the prostaglandin than the DBC group.
Two uterine dehiscences were observed in the DBC group during the manual uterine examination performed for bleeding, and no uterine rupture. There was one uterine rupture in the prostaglandin group and two scar dehiscences observed during cesareans. The uterine rupture involved a 24-year-old secundiparous woman, at term. She had a dose of Prepidil® gel placed three times, 24 h apart. On D4, she was induced by oxytocin with a favorable cervix. Labor lasted 5 h 30 min, and she received oxytocin to a maximum dose of 20 ml/h (5 IU/500 cc) for 3 h. Because of fetal bradycardia and sudden pelvic pain at 3 cm, an emergency cesarean was performed. A complete uterine rupture of the entire previous incision scar was observed during this cesarean delivery. She gave birth to a boy weighing 3440 g, with Apgar scores of 2/2/7/8, and a pH of 7.06. He required pediatric management at birth: intubation at 7 min of life for respiratory distress, with extubation at 18 min. He then accompanied his mother to her room.
There were no significant differences between the groups for the secondary neonatal outcome measures (Table 5). No neonatal deaths occurred.
Discussion
This study shows that the effectiveness of cervical ripening for women with a previous cesarean delivery and a singleton live fetus in cephalic presentation was similar whether performed mechanically by a DBC or pharmacologically, by prostaglandins. There was one case of uterine rupture in the prostaglandin group, with no associated maternal or neonatal morbidity.
Interpretation of results
The success rate of trial of labor for vaginal birth after cesarean (VBAC)—57.5% in the prostaglandin group and 57.2% in the DBC group—is similar to rates previously reported by earlier studies of women planning to attempt VBAC and requiring cervical ripening [8, 9, 17,18,19,20,21]. Nonetheless, few studies in the literature have compared prostaglandins and DBC, and their results have been contradictory. The study by Kehl et al. comparing cervical ripening by PGE2 only to ripening by DBC followed by recourse to PGE2 depending on the cervical modifications did not find a significant difference in the cesarean rates [22]. One of the limitations of their study was that it did not explain the basis of its decisions to use PGE2 or DBC. The study by Ben-Aroya et al., comparing cervical ripening by prostaglandins and by a Foley catheter, clearly showed a significantly higher cesarean rate in the Foley catheter group [23]. The limitations of this study were the small number of subjects, the lack of information about cervical characteristics at the start and end of the ripening, and the time until ripening occurred, which was not indicated. Moreover, no information was provided about the indication for the cesareans, and the authors did not explain the basis for the choice of preparation method. The data in the literature are thus sparse and have important limitations. Our study provides supplementary information with methodological strengths and more women.
It nonetheless lacks the power to show a significant difference, if one exists, in the onset of rare and serious events, such as uterine rupture. We note however that a case of uterine rupture did occur in the prostaglandin group—and none in the DBC group. We observed two scar dehiscences in each group; this result must nonetheless be qualified by the fact that a manual uterine examination was routinely performed in the maternity ward using prostaglandins. These are the rates of uterine rupture currently found in the literature and were based on standardized definitions of uterine rupture and scar dehiscence [15, 17, 23,24,25,26,27]. As of now, no study has had the power required to reach a conclusion about the risk of uterine rupture with the use of either DBC or prostaglandins.
Looking at other obstetric complications, we note that the DBC was successfully placed in every case, even though the study began simultaneously with the DBC's initial use in the department; the physicians were therefore inexperienced with it at the start. The placement failure rate reached 0.8% in the study by Cromi et al. [28]. Bradycardia occurred in one fetus during DBC placement and resulted in an emergency cesarean. Contrary to the literature, there were no such cases in the prostaglandin group [28, 29]. Cervical ripening by prostaglandins appeared to be perceived as more painful than that by DBC, consistent with the data in the literature [30]. Finally, we found no difference concerning infectious complications, although the literature on the topic is somewhat controversial [30]; nonetheless, women with preterm rupture of the membranes were excluded from the study.
Consistent with the literature, our study showed a higher rate of spontaneous labor and lower rate of oxytocin use in the prostaglandin group [28]. It appears that mechanical cervical ripening results in most cases in continuation by induction by oxytocin at higher doses and for a longer time than after ripening by prostaglandins, which more often produce spontaneous labor. A high rate of oxytocin use creates a risk of uterine rupture, emergency cesarean delivery, and postpartum hemorrhage [31,32,33].
Strengths and limitations
This study is original in its focus on the comparison between the methods of mechanical and pharmacological cervical ripening in women with a previous cesarean—a topic little studied until now. Although many physicians are beginning to use mechanical methods to prepare the cervix for women with unfavorable local conditions who would previously have had a repeat cesarean delivery, it was necessary to assess these practices. A second originality lies in our principal endpoint. The literature is currently debating the definition of the failure of cervical ripening. Assessments of the effectiveness of agents for this purpose use a variety of principal endpoints, involving mode of delivery, or a time interval, or entry into the active phase of labor. We chose the cesarean rate as our principal endpoint the cesarean rate, because its reduction is the major clinical benefit expected from cervical ripening. It thus appears to us to be the criterion most clinically relevant for assessing protocols intended to accelerate cervical ripening. Our study provides the information often absent from studies of this procedure, including the indications for cesareans, maternal morbidity, postpartum hemorrhage, and neonatal condition—all important elements to consider in assessing protocols for this procedure. Finally, the previous studies comparing mechanical and pharmacological methods of cervical ripening have included small numbers of women, fewer than 100 women in each group. Our study has the advantage of including more women.
The limitations of this study are, first of all, its retrospective character; nonetheless, the data were collected prospectively, with an exhaustive list of data for each woman, verified daily. After adjustment for several factors, the OR for cesarean rate reached no statistical significance but changed obviously from 1.01. to 1.56, suggesting a possible increased risk of cesarean delivery for DBC group. But this result must be interpreted with caution because we have few effective, few cases of cesarean and in comparison several factors of adjustment, so we lacked of statistical power to conclude. It also did not include enough women to provide adequate power to reach conclusions about rare events such as uterine rupture. Protocols of induction used in these two maternities are rather individual and can limit the external validity of this study. But the objective of this study was to compare two policies of practices of induction (mechanical versus pharmacological) and not to compare two different protocols. Finally, women's satisfaction with each of these methods could not be studied.
Conclusion
Our results suggest that DBC and prostaglandins are cervical ripening methods with equivalent effectiveness for women with a previous cesarean delivery and unfavorable local conditions. Both enable vaginal delivery in nearly half of all cases. Our study thus demonstrates that either method can be used for cervical ripening in women with a uterine scar, to avoid systematic realization of planned cesarean delivery. A mechanical cervical ripening by DBC can be a safe option for practitioners not performing, currently, a cervical ripening by prostaglandins. But DBC for cervical ripening in women with previous cesarean still needs to be evaluated and it is necessary to be very careful about the induction of labor with oxytocin, after DBC, when the cervix remained persistently unfavorable, in view of the potential association with increased uterine rupture rates. In the meantime, prostaglandins may be preferred because we have more data on their uses in this indication. A much larger study, such as a multicenter randomized trial of a large number of women, would be necessary to examine rare, serious events.
References
Keag OE, Norman JE, Stock SJ (2018) Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med 15(1):e1002494
Sandall J, Tribe RM, Avery L, Mola G, Visser GH, Homer CS et al (2018) Short-term and long-term effects of caesarean section on the health of women and children. The Lancet 392(10155):1349–1357
Guise JM, Eden K, Emeis C, Denman MA, Marshall N et al. (2010) Vaginal birth after cesarean: new insights. Evidence report/technology assessment No.191. AHRQ Publication No. 10-E003. https://www.ahrq.gov/research/findings/evidence-basedreports/vbacup-evidence-report.pdf. Accessed 21 Oct 2013
Sentilhes L, Vayssière C, Beucher G, Deneux-Tharaux C, Deruelle P, Diemunsch P et al (2013) Delivery for women with a previous cesarean: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol 170(1):25–32
ACOG Practice Bulletin No (2019) 205 Summary: vaginal birth after cesarean delivery. Obstet Gynecol 133(2):393–395
Royal College of Obstetricians and Gynaecologists (2015) Birth after previous caesarean birth. Green-top guideline no. 45
Martel M-J, MacKinnon CJ, Clinical Practice Obstetrics Committee, Society of Obstetricians, and Gynaecologists of Canada (2005) Guidelines for vaginal birth after previous caesarean birth. J Obstet Gynaecol Can 27(2):164–188
Dekker GA, Chan A, Luke CG, Priest K, Riley M, Halliday J et al (2010) Risk of uterine rupture in Australian women attempting vaginal birth after one prior caesarean section: a retrospective population-based cohort study. BJOG Int J Obstet Gynaecol 117(11):1358–1365
Schmitz T, Pourcelot A-G, Moutafoff C, Biran V, Sibony O, Oury J-F (2013) Cervical ripening with low-dose prostaglandins in planned vaginal birth after cesarean. PLoS ONE 8(11):e80903
Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 345(1):3–8
Al-Zirqi I, Stray-Pedersen B, Forsén L, Vangen S (2010) Uterine rupture after previous caesarean section. BJOG Int J Obstet Gynaecol 117(7):809–820
Ravasia DJ, Wood SL, Pollard JK (2000) Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am J Obstet Gynecol 183(5):1176–1179
Kehl S, Weiss C, Rath W (2016) Balloon catheters for induction of labor at term after previous cesarean section: a systematic review. Eur J Obstet Gynecol Reprod Biol 204:44–50
Kruit H, Wilkman H, Tekay A, Rahkonen L (2017) Induction of labor by Foley catheter compared with spontaneous onset of labor after previous cesarean section: a cohort study. J Perinatol 37(7):787–792
Jozwiak M, van de Lest HA, Burger NB, Dijksterhuis MGK, De Leeuw JW (2014) Cervical ripening with Foley catheter for induction of labor after cesarean section: a cohort study. Acta Obstet Gynecol Scand 93(3):296–301
Vital M, Grange J, Le Thuaut A, Dimet J, Ducarme G (2018) Predictive factors for successful cervical ripening using a double-balloon catheter after previous cesarean delivery. Int J Gynaecol Obstet 142(3):288–294
Kwee A, Bots ML, Visser GHA, Bruinse HW (2007) Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands. Eur J Obstet Gynecol Reprod Biol 132(2):171–176
McMahon MJ, Luther ER, Bowes WA, Olshan AF (1996) Comparison of a trial of labor with an elective second cesarean section. N Engl J Med 335(10):689–695
Macones GA, Peipert J, Nelson DB, Odibo A, Stevens EJ, Stamilio DM et al (2005) Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol 193(5):1656–1662
Boujenah J, Fleury C, Tigaizin A, Benbara A, Mounsambote L, Murtada R et al (2019) Déclenchement par ballonnet en cas d’utérus cicatriciel et col défavorable : la tentative en vaut-elle la chandelle ? Gynécol Obstét Fertil Sénol. https://linkinghub.elsevier.com/retrieve/pii/S2468718919300145
Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW et al (2004) Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 351(25):2581–2589
Kehl S, Weiss C, Wamsler M, Beyer J, Dammer U, Heimrich J et al (2016) Double-balloon catheter and sequential vaginal prostaglandin E2 versus vaginal prostaglandin E2 alone for induction of labor after previous cesarean section. Arch Gynecol Obstet 293(4):757–765
Ben-Aroya Z, Hallak M, Segal D, Friger M, Katz M, Mazor M (2002) Ripening of the uterine cervix in a post-cesarean parturient: prostaglandin E2 versus Foley catheter. J Matern-Fetal Neonatal Med 12(1):42–45
Agnew G, Turner MJ (2009) Vaginal prostaglandin gel to induce labour in women with one previous caesarean section. J Obstet Gynaecol 29(3):209–211
Grobman WA, Gilbert S, Landon MB, Spong CY, Leveno KJ, Rouse DJ et al (2007) Outcomes of induction of labor after one prior cesarean. Obstet Gynecol 109(2 Pt 1):262–269
Sananès N, Rodriguez M, Stora C, Pinton A, Fritz G, Gaudineau A et al (2014) Efficacy and safety of labour induction in patients with a single previous caesarean section: a proposal for a clinical protocol. Arch Gynecol Obstet 290(4):669–676
Sarreau M, Leufflen L, Monceau E, Tariel D, Villemonteix P, Morel O et al (2014) Balloon catheter for cervical ripening on scarred uterus with unfavorable cervix: multicenter retrospective study of 151 patients. J Gynecol Obstet Biol Reprod (Paris) 43(1):46–55
Cromi A, Ghezzi F, Uccella S, Agosti M, Serati M, Marchitelli G et al (2012) A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. Am J Obstet Gynecol 207(2):125.e1–7
Vaknin Z, Kurzweil Y, Sherman D (2010) Foley catheter balloon vs locally applied prostaglandins for cervical ripening and labor induction: a systematic review and metaanalysis. Am J Obstet Gynecol 203(5):418–429
Pennell CE, Henderson JJ, O’Neill MJ, McChlery S, McCleery S, Doherty DA et al (2009) Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG Int J Obstet Gynaecol 116(11):1443–1452
Heinemann J, Gillen G, Sanchez-Ramos L, Kaunitz AM (2008) Do mechanical methods of cervical ripening increase infectious morbidity? A systematic review. Am J Obstet Gynecol 199(2):177–187 (discussion 187–188)
Alfirevic Z, Kelly AJ, Dowswell T (2009) Intravenous oxytocin alone for cervical ripening and induction of labour. Cochrane Database Syst Rev 4:CD3246
Weimar CHE, Lim AC, Bots ML, Bruinse HW, Kwee A (2010) Risk factors for uterine rupture during a vaginal birth after one previous caesarean section: a case-control study. Eur J Obstet Gynecol Reprod Biol 151(1):41–45
Funding
None.
Author information
Authors and Affiliations
Contributions
DK: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. SR: Data collection or management, Data analysis, Manuscript writing/editing. CM: Manuscript writing/editing. PM: Manuscript writing/editing. OS: Protocol/project development, Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Korb, D., Renard, S., Morin, C. et al. Double-balloon catheter versus prostaglandin for cervical ripening to induce labor after previous cesarean delivery. Arch Gynecol Obstet 301, 931–940 (2020). https://doi.org/10.1007/s00404-020-05473-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05473-x