Abstract
Purpose
There are numerous methods for cervical ripening although not all of them are indicated in women presenting a higher risk of uterine hyperstimulation. To compare the efficacy and security of the two methods for cervical ripening in the induction of labor in these pregnancies.
Methods
Retrospective analysis of two cohorts consisting of pregnant women who gave birth from 2016 to 2019 (112 inductions with dinoprostone and 112 with intracervical double- balloon).
Results
There are statistically significant differences in favor of dinoprostone in deliveries that occurred before 12 h since the start of the induction (28.6% vs 13.4%, p = 0.005) and a higher rate of cervical ripening (55.4% vs 33.9%; p = 0.001). There were no statistically significant differences in induction time, the percentage of women delivering within 24 h or beyond, nor in the type of delivery. Additionally, a decreased need of oxytocin (60.7% vs 42.9%; p = 0.001) and a lower dose when used has been observed in the dinoprostone group. However, Dinoprostone also has a higher rate of minor maternal complications as uterine hyperstimulation (18.8% vs 3.6%; p = 0.001) and altered cardiotocography (26.8% vs 4.5%; p = 0.001). No significant difference has been found between the two groups regarding severe complications.
Conclusions
Dinoprostone presents a greater efficacy for cervical ripening and delivery in ≤ 12 h, with less need of oxytocin perfusion than inductions using an intracervical double-balloon. There is no significant difference in severe maternal complications between the two groups. In conclusion, Dinoprostone could be an effective and safe option for patients at risk of uterine hyperstimulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Labor induction is a frequent obstetrical procedure which takes place when the risk of continuing with the pregnancy is greater than that of ending it. Over the last few years, the number of inductions has increased, reaching up to 25% of all pregnancies [1, 2]. However, data varies between countries and even different hospitals, ranging from 22% in the United States [3] (reaching its highest rates in 2010 with 23.8% [4]) to 1.4% in Nigeria [5]. Nevertheless, labor induction has been associated with increased complications in comparison with spontaneous deliveries, especially when facing an unfavorable cervix, with a greater risk of failed labor induction, longer labor and more deliveries by cesarean section [6, 7]. Labor induction can be carried out via mechanical or pharmacological procedures. Mechanical techniques were the first to be developed to help cervical ripening and trigger delivery. In theory they have the same indications as pharmacological methods, although they require a certain degree of cervical dilation and the presence of intact membranes. On the other hand, pharmacological methods are associated with a higher frequency of side effects due to prostaglandin administration, the most common being uterine hyperstimulation.
There is not a single exact definition for uterine hyperstimulation. In fact, it is a concept that includes terms such as tachysystole and hypertonia, without a consensus regarding its precise meaning. The American College of Obstetricians and Gynecologists (ACOG) defines tachysystole as the presence of six or more contractions per 10 min, over an average of 30 min, in combination with fetal heart rate alterations or not [8]. Similarly, the NICE Guide defines uterine hypertonia as contractions persisting over 60 s, or tachysystole as more than five contractions in 10 min [9].
Uterine rupture is the most severe complication of uterine hyperstimulation, and the chances of it happening are significantly increased in patients with previous caesarean section or uterine surgeries. Likewise, uterine hyperstimulation involves a greater risk in cases of intrauterine growth restriction, prematurity, severe preeclampsia or oligohydramnios, as well as instances of uterine hyperdistention (multiple pregnancies, polyhydramnios, great multiparity or macrosomia). Labor induction in these patients is a valid procedure, although there is no consensus as to which method is optimal due to the limited evidence available from randomized clinical trials [10]. Therefore, if the induction of labor is indicated in a pregnant woman of the previously described characteristics, treatment with prostaglandins, oxytocin, elective caesarean section or induction with mechanical methods are all acceptable options.
Until 2017, prostaglandin E2 or dinoprostone 10 mg with a vaginal liberation system (Propess®, Ferring Pharmaceuticals, Saint-Prex, Switzerland [11]) was the only method used in pregnant women with a high risk of uterine hyperstimulation in our clinical unit. Since then, the protocol has been reviewed to include the use of the double-balloon (Intracervical double-balloon catheter for cervical ripening, Cook®, Cook OB/GYN, Spencer, IN, USA [12]) as an alternative for these patients. After two years of use in our hospital, we have compared its results to those of the previous protocol using dinoprostone. Thus, the objective of this paper is to evaluate the differences in labor induction between patients treated with intracervical double-balloon and dinoprostone in women with a high risk of uterine rupture, as well as studying and comparing maternal and neonatal safety profiles in both methods.
Material and methods
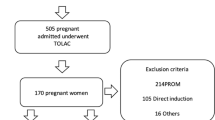
We have compared two cohorts derived from the protocol change in our department. The first cohort was made up of 112 pregnant women with risk factors for uterine hyperstimulation (Table 1) who met the inclusion criteria, had no exclusion criteria and were induced with an intracervical double-balloon for a maximum of 12 h between May 2017 and September 2019. The second group was a retrospective cohort of 112 pregnant women who fulfilled the same inclusion and exclusion criteria but were induced with dinoprostone for up to 24 h according to the previous protocol between January 2016 and April 2017. The data was obtained from the labor registry of the University Hospital of Fuenlabrada by reviewing medical records on Selene SP12, Cerner Health Services, Inc. No information was introduced, modified or suppressed.
Inclusion criteria were: women with singleton pregnancy and a high risk of uterine hyperstimulation (Table 1), cephalic presentation and Bishop test < 6 upon admission to the hospital [13]. Exclusion criteria included patients with Bishop ≥ 6, symptomatic or suspected chorioamnionitis, vaginal bleeding, multiple pregnancies, non-cephalic presentations, placenta previa or premature placenta detachment, alterations in uterine contraction, and hepatic, renal or cardiovascular alterations. Also, two women with a stillbirth and premature rupture of membranes were excluded from this trial to avoid possible bias, as placement of a double-balloon is not recommended in the technical specifications of the product in these cases [12]. All patients signed an informed consent form for the induction of labor.
Prior to the induction of labor, fetal wellbeing was assessed via a 20 to 30-min cardiotocography (CTG). In the group assigned to mechanical ripening a double-balloon catheter was placed. Said catheter consists of a single use latex free silicone device which is placed in the lower extraamniotic space under direct vision with a Sim’s sterile speculum, without cervical traction. Once both balloons are inside the cervical canal, the first one (uterine) is filled with 80 ml of saline solution (maximal capacity), slightly pulling until it rests on the internal cervical os. Next, the second balloon (vaginal) is also filled with 80 ml of saline solution. After setting the catheter, an external fetal monitor was placed for 30 min, continuing with the usual induction protocol once fetal wellbeing was verified.
The double-balloon catheter was left in place a maximum of 12 h as per the manufacturer’s recommendation [12]. The catheter was removed if spontaneous rupture of membranes, expulsion of the catheter or beginning of labor occurred, as well as in cases with signs of fetal distress. In the dinoprostone groups, the vaginal liberation system was placed in the posterior vaginal fornix a maximum of 24 h according to the product’s technical specifications and CTGs were done before and after its placement [11].
After having completed the maximum recommended time, the device was removed (either catheter or dinoprostone), and after an hour, oxytocin perfusion was started if labor had not set on before. A low dose oxytocin protocol was used, beginning at 0.5–2 mU/min with an increment of 1–2 mU/min every 15 to 60 min until effective uterine contractions were achieved, followed by controlled amniotomy when possible [14, 15].
Once labor was established (3–4 cm dilated cervix) we proceeded with the hospital’s usual protocol.
A failed induction was diagnosed when active labor was not accomplished despite of regular uterine dynamics, after amniotomy and a minimum of 12 h of oxytocin infusion. Failure in labor progression was defined as the absence of change in cervical dilation in a 4-h interval after increasing oxytocin and achieving regular uterine dynamics.
Bishop’s Test was performed at the beginning of induction and immediately after removal of the chosen device (balloon or dinoprostone), prior to oxytocin infusion. Cervical ripening was considered complete with a Bishop score ≥ 6.
Induction time was categorized in the following way:
-
Time until cervical ripening: time from the placement of the device until reaching a Bishop score ≥ 6.
-
Time of labor: time from the beginning of the active phase of labor (> 3–4 cm of cervical dilation) until birth.
-
Time of induction: time from the placement of the device until birth.
Our main variable was vaginal birth in the first 24 h after induction (and within the first 12 h after the placement of the device). The secondary variables were caesarean rate, oxytocin use -and the highest dose reached-, intrapartum complications due to the ripening method and perinatal results.
Statistics Process Social Sciences (SPSS) 20.0 version for Windows (SPSS Inc, Chicago, IL, USA) was used for statistical analysis. For qualitative variables, frequency (n) and percentages (%) were calculated. Quantitative variables were expressed with means of average and standard deviation. The Chi-squared test was used to analyze the relationship between two qualitative variables (or Fisher’s test if the sample was small). Quantitative variables were compared using Student’s T-test. Statistical significance level was stablished as p < 0.05.
Results
We analyzed data from 224 pregnant women divided into two homogeneous cohorts according to their general characteristics (Table 2). Only maternal age was slightly higher in the dinoprostone group (p = 0.04), with no clinical relevance. Most women did not have previous births (69.6% in dinoprostone group and 76.8% in the catheter group; p = 0.23), there were no differences between the two groups in terms of women with previous caesarean Sect. (35.7% dinoprostone vs 33% catheter groups; p = 0.68) and average gestational age at the time of induction was 38 weeks.
The main reason for induction in both of our cohorts was fetal growth restriction, followed by chronologically prolonged pregnancies and hypertensive disorders in pregnancy. Other medical and obstetrical motives for induction we encountered were thromboembolic and hematologic illness (previous deep venous thrombosis, massive thromboembolism and severe plaquetopenia) as well as previous unfavorable obstetric results (fetal death before or after birth).
Table 3 shows the method of delivery and the indication of caesarean section in both groups, the Bishop Test score before and after the placement of the induction method and the times associated to the induction of labor in its different phases, as well as oxytocin needs.
The type of labor was similar in both groups, with delivery via caesarean section being slightly higher in the intracervical double-balloon cohort (27.7% vs 23.2%) but lacking statistical significance (p = 0.44). For women with vaginal deliveries, the percentage of instrumental delivery was superior in the dinoprostone group (32.6 vs 28.4%; p = 0.56), again without statistical significance. The most common indication of caesarean section or instrumental birth was pathological CTG with risk of loss of fetal well-being.
The rate of cervical ripening was significantly greater in the dinoprostone group (55.4% vs 33.9%; p = 0.001). Initial Bishop Test score was similar in both groups, and after the removal of the device it was significantly higher in the dinoprostone cohort (5.49 vs 4.76; p = 0.03).
We found statistically significant differences in the need of oxytocin use (dinoprostone group 60.7% vs double-balloon group 83.9%; p = 0.001) and in the average maximum dose required (18.82 mU/min dinoprostone group vs 26.45 mU/min double-balloon group; p = 0.006). No statistically significant differences were found between the rest of the studied variables.
Regarding the removal or expulsion of the device, there was a greater rate in the dinoprostone cohort (26.8% vs 4.5%; p = 0.001), the main reason for removal in this group being alterations in CTG whereas in the double-balloon group most were spontaneous expulsions.
No significant differences were found in the achievement of delivery, either in the first 24 h of induction or beyond. However, delivery rates in the first 12 h of induction were significantly higher in the dinoprostone group (28.6% vs 13.4%; p = 0.005). Total induction time since device placement was similar in both groups. When we analyzed the different time slots up to cervical ripening and from the beginning of the active phase of labor until delivery we found that the dinoprostone group needed more time (12.91 h vs 9.42 h in the catheter groups; p = 0.001) but once the active phase of labor was reached, time until delivery was significantly shorter (6.18 h the dinoprostone group vs 13.7 h the double-balloon group; p = 0.001). On the other hand, the duration of cervical ripening was shorter in the double-balloon group, although with this method more time passed from active phase until delivery and these patients had lower Bishop Test scores after removal of the device.
Secondary adverse effects derived from the induction method are described in Table 4. Minor maternal complications including CTG alteration and tachysystole were significantly greater in the dinoprostone group (p = 0.001 in both cases), whereas no statistically significant differences were found in neither meconium liquid nor maternal fever.
We found no differences in severe maternal complications such as uterine rupture (p = 0.5) or postpartum hemorrhage (p = 0.3) between both groups.
Regarding perinatal outcomes, statistically significant differences were only found in admission to the neonatal intensive care unit (NICU), greater for the balloon group (p = 0.01) (Table 5).
Discussion
The present study showed that among this group of women with a high risk of uterine hyperstimulation, cervical ripening with dinoprostone achieved a higher rate of cervical ripening and deliveries before 12 h since the start of induction in comparison to the intracervical double-ballon. Altough dinoprostone may increase the occurrence of uterine hyperstimulation and altered cardiotocography; both without fetal repercussion, this method did not cause severe maternal or neonatal complications.
Due to these results, we propose that both methods can be safely used for the induction of labor in this group of pregnant women.
Induction of labor is one of the most common procedures in obstetrics [3, 16,17,18]. This procedure must be carried out when the benefits of delivery exceed the risks of continuing the pregnancy, and although there are many indications that justify it, there are only a few absolute indications, including: maternal medical causes such as chronic arterial hypertension, pregestational diabetes mellitus or hypertensive disorders of pregnancy. Fetal pathology such as growth restriction, amniotic fluid alterations or multiple pregnancies can also lead to terminating the pregnancy once a viable gestational age is reached. Rising causes of induction include premature rupture of membranes, chronologically prolonged pregnancies and those where previous obstetrical history is taken into account (antepartum or fetal death during labor, malformations or previous adverse obstetric outcomes among others [17,18,19,20,21]).
There are numerous scientific papers comparing every ripening method, recommending different doses and usage times, evaluating secondary effects and possible maternal and fetal complications. Liu’s meta-analysis comparing double-ballon with dinoprostone obtained similar results to our study [22]. This review showed that the efficacy of both methods is similar. No differences were found regarding vaginal delivery in the first 24 h (relative risk (RR) 1.21 confidence interval of 95% (CI) 0.93–1.59) nor the incidence of caesarean section (RR 0.99, 95% CI 0.77 – 1.21). Dinoprostone was associated with less oxytocin use (RR 1.95, 95% CI 1.45–2.62), a greater incidence of excessive uterine activity (RR 0.17, 95% CI 0.06–0.54) and neonatal arterial blood pH < 7.1 (RR 0.36, 95% CI 0.15–0.84). No differences were found in the other neonatal parameters studied. Unlike our study, none of the articles included in the meta-analysis analyze the deliveries which occurred within the first 12 h or describe maternal complications.
One of the main concerns in pregnant women with previous caesarean section that undergo an induction is the risk of uterine rupture. However, the incidence of this event in this group was low, ranging from 0.32 to 0.47% [23], and it varied depending on the type of hysterotomy performed in the caesarean section (low transverse incisions carried a risk of 0.2–1.5% while uterine rupture occurred in 1–1.6% of the patients with a vertical incision [24]). Risk of uterine rupture is greater in women with previous caesarean section if labor is induced rather than spontaneous (0.15–0.4% vs 0.54–1.4%) [25]. In a multicenter trial including over 33,000 pregnant women attempting vaginal delivery after caesarean section, the induction of labor carried an increase in uterine rupture compared to spontaneous beginning of labor. However, a secondary analysis concluded that the rate of uterine rupture increased only in those women without previous vaginal deliveries in addition to a caesarean Sect. (1.5% vs. 0.8%, p = 0.02) [26].
In our sample there were only two registered cases of uterine rupture (1.8%), both associated with dinoprostone use in women with previous caesarean section (one of them with a previous complex surgery due to hysterotomy tearing) and without previous vaginal deliveries. There were no significant differences with the double-balloon group (0 vs 1,8%, p = 0.5).
Prostaglandins are one of the most used methods for cervical ripening in women without previous uterine scars. Since they usually provoke uterine contractions in addition to cervical ripening, their use is not recommended in women with a previous caesarean section [27,28,29]. However, the induction of labor with prostaglandins has been associated with lower oxytocin needs when compared with mechanical methods, as we also found in our results (dinoprostone group 60.7% vs double-balloon group 83.9%; p = 0.001) [30].
There are no quality studies that show the effectiveness and safety of the various induction methods in women with previous cesarean section. In a recent systematic review, the evidence from studies on methods of induction of labor for women with a prior caesarean section is not adequate and said studies are not powerful enough to detect clinically relevant differences for many outcomes.[10].
As we found in our study, severe complications such as uterine rupture are rare and most of the studies about pregnancy outcomes in women with previous cesarean section are also retrospective studies [31,32,33,34].
There are several types of prostaglandins used for inducing labor. Prostaglandin E1 is contraindicated in women with a history of cesarean section because its use can lead to uterine rupture due to the hyperstimulation it produces. [35, 36]. Prostaglandin E2 may be used for cervical ripening in case of unfavorable cervical dilation in women who have undergone a previous caesarean section with a transverse segmentary incision. The Society of Obstetricians and Gynecologists of Canada (SOGC) endorses the use of prostaglandin E2 in inductions of women with a previous caesarean section after proper counselling. On top of that, commercial preparations of dinoprostone (Propess®) offer a posology of 10 mg with prolonged release, with an average release rhythm of 0.3 mg/hour, more convenient than the intracervical gel format. Once the device is placed it can remain in the vagina for up to 24 h, and it can be removed via its string [11]. In case of hyperdinamia or alterations in fetal cardiac frequency directly derived from the drug, the vaginal device can be easily and quickly removed, making dinoprostone the first choice for many authors. The patient must always be informed of the increased risk of uterine rupture with the use of prostaglandins even though the absolute risk is very low [37], although it increases when oxytocin is added. Personalized informed consent must always be obtained in these cases.
Other obstetric and gynecological scientific institutions [35, 38, 39] have not directly advised against the use of prostaglandin E2 in women with prior cesarean delivery yet they recommend induction of labor with a Foley catheter in these patients [40].
The risk of uterine rupture is greater when oxytocin is used for induction as opposed to spontaneous onset of labor. However, there is insufficient evidence to conclude that the use of prostaglandin E2 also increases the risk of uterine rupture [31,32,33].
Mechanical methods for induction were the first to be developed for cervical ripening in unfavorable cases but have since been mostly replaced with pharmacological methods, apparently more effective and convenient. However, mechanical methods have the advantage of presenting a low rate of uterine hypercontractility, which makes them of special interest in the group we are studying. They also show a low side effect rate in most studies. Nonetheless, two recent randomized trials suggest an increase in the risk of chorioamnionitis when two Foley catheters are used to induce labor in patients with premature rupture of membranes [41, 42]. Consequently, premature rupture of membranes is one of the contraindications for induction via intracervical double-balloon (Cook double-balloon®), as included in its technical specifications [12]. In our study, significantly more newborns were admitted to the NUCI in the ballon group vs dinoprostone (p = 0.01). However, we did not place double-balloons when there was a premature rupture of membranes and thus found no causality for this event.
The use of combined pharmacological and mechanical methods has been studied to no avail. A trial carried out by Letailleur [43] comparing dinoprostone with sequential administration of double-balloon followed by dinoprostone found that double cervical ripening allowed for a better Bishop test score without increasing the rate of vaginal deliveries nor presenting statistical differences concerning maternal or neonatal complications.
We proposed a change in the induction of labor protocol used in our hospital, adding the use of mechanical methods as an alternative to dinoprostone in cases with a high risk of uterine hyperstimulation. Although most studies are based on the Foley catheter as a mechanical dilator due to its widespread availability, price and years in use, we chose the double-balloon catheter as it was the first device specifically created and commercialized for this purpose.
The main variable in our study was time elapsed from the beginning of induction until delivery. Our results don't show significant differences between the use of dinoprostone or double-balloon catheter as far as vaginal deliveries in the first 24 h of induction are concerned, similar to previous studies [22]. However, there was a difference when delivery took place within the first 12 h after starting the induction, where dinoprostone produced a greater rate of vaginal labor, fact not found in previous studies.
The rate of caesarean sections was slightly increased in the double-balloon catheter group, although without statistical significance, matching these results with those of previous controlled trials comparing intracervical catheters and vaginal prostaglandins [44, 45]. In the meta-analysis published in 2016 by Du, both the double-balloon catheter and prostaglandins had similar rates of caesarean section and vaginal delivery in the first 24 h, as well as adverse maternal outcomes. However, the risk of excessive uterine activity and the need of neonatal ICU increased significantly in the prostaglandin group when compared to the double-balloon catheter group [46]. In the recent systematic review by Vaan MDT et al. concerning the induction of labor with mechanical methods, they compared these with prostaglandin E2 (PGE2), a low misoprostol dose or oxytocin. They reached similar conclusions to our study: no differences were found in the rate of vaginal delivery in the first 24 h with PGE2 or double-balloon catheter (risk ratio (RR) 1.01; CI 95%: 0.92–1.09). Similarly to our findings, they also concluded that the double-balloon catheter probably reduced the risk of uterine hyperstimulation, although they chose not to differentiate double or single-balloon catheters [47]. Generally, the evidence found across several studies is of moderate quality and the estimates of the effect too imprecise to allow a valid judgment.
As to neonatal results, no significant differences were found in our study. This seems to be in the same line as what is found in literature, save for Pennel’s meta-analysis, the first study to include neonatal blood gases in the results. They found a greater rate of respiratory acidosis with dinoprostone use, probably secondary to uterine hyperstimulation. Still, further studies are needed to support this hypothesis [48].
When it comes to the strengths of our study, we must point out that, within our knowledge, this is the first trial that analyses labor induction in pregnant women with high risk of uterine hyperstimulation. On top of that, it is the first one to demonstrate an increase in vaginal deliveries within the first 12 h of induction in patients treated with dinoprostone. In addition, we found no differences in severe maternal complications and neonatal outcomes between both groups.
On the other hand, our study’s main weakness is its retrospective nature, leading to a lower quality of data when compared to a prospective study. Nonetheless, the focus on women at risk of hyperstimulation has provided interesting and detailed data concerning a relatively homogeneous group of women where labor induction means a greater challenge. The relative absence of data found in previous studies and the heterogenous definitions and procedures used for labor induction show the need for further investigation with high quality trials focusing on the comparison between the different methods for labor induction.
On the subject of cervical ripening produced by the two methods, we reached an important conclusion: dinoprostone takes longer to attain a higher score in the Bishop test, and more time is needed from the beginning of the active phase until delivery with the use of the double-balloon catheter. When using dinoprostone, cervical ripening is a lengthier process, but once the cervix is ripened less time passes until delivery due to its stimulating effect on the uterus.
On the other hand, cervical ripening is quickly achieved with the double-balloon, albeit with a lower final Bishop test score. This lower score might stem from the subjective nature of cervical evaluation. We have clearly observed how lack of experience with the double-balloon can lead to underestimating cervical modifications after its use when compared to pharmacological methods. Thus, it is crucial that personnel in hospital units where double-balloons are used for cervical ripening receive appropriate training to perform an adequate cervical evaluation and Bishop test score after device removal in these cases. This could improve the development of the technique as well as induction results.
Conclusion
Both the intracervical double-balloon catheter and dinoprostone are effective techniques for cervical ripening in the induction of labor in women at a high risk of uterine hyperstimulation with an unfavorable cervix. However, our study shows a higher rate of delivery within the first 12 h and lower oxytocin need with the use of dinoprostone. We have also proven a similar safety profile in both methods for patients and newborns. In conclusion, dinoprostone is more effective than the double-balloon for induction in these patients whilst remaining equally safe.
References
Murthy K, Grobman WA, Lee TA, Holl JL (2011) Trends in induction of labor at early-term gestation. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2010.12.023
Sciscione AC, Ruhstaller K (2013) Double-balloon catheter results in higher rate of vaginal delivery within 24 h when compared with dinoprostone vaginal insert. Evid Based Med 18(4):140–141. https://doi.org/10.1136/eb-2012-101021
Committee ACOG, on Practice Bulletins – Obstetrics, (2009) ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol 114:386–397. https://doi.org/10.1097/AOG.0b013e3181b48ef5
Osterman MJ, Martin JA (2014) Recent declines in induction of labor by gestational age. NCHS Data Brief 155:1–8
Bukola F, Idi N, M’Mimunya M, Jean-Jose WM, Kidza M, Isilda N, Faouzi A, Archana S, Paulo SJ, Matthews M, Metin G (2012) Unmet need for induction of labor in Africa: secondary analysis from the 2004–2005 WHO Global Maternal and Perinatal Health Survey (A cross-sectional survey). BMC Public Health 12:722. https://doi.org/10.1186/1471-2458-12-722
Vahratian A, Zhang J, Troendle JF, Sciscione AC, Hoffman MK (2005) Labor progression and risk of cesarean delivery in electively induced nulliparas. Obstet Gynecol 105(4):698–704. https://doi.org/10.1097/01.AOG.0000157436.68847.3b
Cocks DP (1955) Significance of initial condition of cervix uteri to subsequent course of labour. BMJ 1(4909):327–328. https://doi.org/10.1136/bmj.1.4909.327
American College of Obstetricians and Gynecologists (2009). ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstetrics and gynecology, 114(1), 192–202. https://doi.org/https://doi.org/10.1097/AOG.0b013e3181aef106
National Collaborating Centre for Women's and Children's Health (UK). (2007). Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. RCOG Press.
West HM, Jozwiak M, Dodd JM (2017) Methods of term labour induction for women with a previous caesarean section. The Cochrane database of systematic reviews. https://doi.org/10.1002/14651858.CD009792.pub3
Propess 10 mg sistema de liberación vaginal ® (2020) Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). http://www.aemps.gob.es/cima/pdfs/ es/ft/62088/FT_62088.pdf. Accessed 16 April 2019.
Cook cervical ripening balloon with adjustable stylet (2019). Cook medical. https://www.cookmedical.com/data/IFU_PDF/T_J-CCRBS_REV2.PDF. Accessed 16 April 2019.
Bishop EH (1964) Pelvic scoring for elective induction. Obstet Gynecol 24:266–268
Budden A, Chen LJ, Henry A (2014) High-dose versus low-dose oxytocin infusion regimens for induction of labour at term. The Cochrane database of systematic reviews. https://doi.org/10.1002/14651858.CD009701.pub2
Patka JH, Lodolce AE, Johnston AK (2005) High- versus low-dose oxytocin for augmentation or induction of labor. Ann Pharmacother 39(1):95–101. https://doi.org/10.1345/aph.1E037
Osterman MJK, Martin JA. Recent declines in induction of labor by gestational age. (2014). NCHS data brief, no 155. Hyattsville, MD: National Center for Health Statistics. http://www.cdc.gov/nchs/data/databriefs/db155.htm. Accessed 20 May 2019.
WHO recommendations: induction of labour at or beyond term. (2018) Geneva: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/277233/9789241550413-eng.pdf. Accessed 20 may 2019.
World Health Organization Recommendations for Induction of labour. http://apps.who.int/iris/bitstream/10665/44531/1/9789241501156_eng.pdf. Accessed 20 May 2019.
American College of Obstetricians and Gynecologists, & Task Force on Hypertension in Pregnancy (2013). Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstetrics and gynecology, 122(5), 1122–1131. https://doi.org/https://doi.org/10.1097/01.AOG.0000437382.03963.88
WHO recommendations for Prevention and treatment of pre-eclampsia and eclampsia (2011). https://apps.who.int/iris/bitstream/handle/10665/44703/9789241548335_eng.pdf?sequence=1. Accessed 20 May 2019
Caughey AB, Stotland NE, Washington AE, Escobar GJ (2007) Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2006.08.040
Liu YR, Pu CX, Wang XY, Wang XY (2019) Double-balloon catheter versus dinoprostone insert for labour induction: a meta-analysis. Arch Gynecol Obstet 299(1):7–12. https://doi.org/10.1007/s00404-018-4929-8
Guise JM, Berlin M, McDonagh M, Osterweil P, Chan B, Helfand M (2004) Safety of vaginal birth after cesarean: a systematic review. Obstet Gynecol 103(3):420–429. https://doi.org/10.1097/01.AOG.0000116259.41678.f1
Shipp TD, Zelop CM, Repke JT, Cohen A, Caughey AB, Lieberman E (1999) Intrapartum uterine rupture and dehiscence in patients with prior lower uterine segment vertical and transverse incisions. Obstet Gynecol 94:735–740. https://doi.org/10.1016/s0029-7844(99)00398-1
Fitzpatrick KE, Kurinczuk JJ, Alfirevic Z, Spark P, Brocklehurst P, Knight M (2012) Uterine rupture by intended mode of delivery in the UK: a national case-control study. PLoS Med 9(3):e1001184. https://doi.org/10.1371/journal.pmed.1001184
Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O’Sullivan MJ, Sibai B, Langer O, Thorp JM, Ramin SM, Mercer BM, Institute N, of Child Health and Human Development Maternal-Fetal Medicine Units Network, (2004) Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 351(25):2581–2589. https://doi.org/10.1056/NEJMoa040405
Alfirevic Z, Aflaifel N, Weeks A (2014) Oral misoprostol for induction of labour. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001338.pub3
Hofmeyr GJ, Gülmezoglu AM, Pileggi C (2010) Vaginal misoprostol for cervical ripening and induction of labour. The Cochrane database of systematic reviews. https://doi.org/10.1002/14651858.CD000941.pub2
Committee ACOG, Opinion. American College of Obstetrician and Gynecologist, (2003) ACOG Committee Opinion. Number 283, May 2003. New U.S. Food and Drug Administration labeling on Cytotec (misoprostol) use and pregnancy. Obstet Gynecol 101:1049–1050. https://doi.org/10.1016/s0029-7844(03)00396-x
Vaknin Z, Kurzweil Y, Sherman D (2010) Foley catheter balloon vs locally applied prostaglandins for cervical ripening and labor induction: a systematic review and metaanalysis. Am J Obstet Gynecol 203(5):418–429. https://doi.org/10.1016/j.ajog.2010.04.038
Ravasia DJ, Wood SL, Pollard JK (2000) Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am J Obstet Gynecol 183(5):1176–1179. https://doi.org/10.1067/mob.2000.109037
Zelop CM, Shipp TD, Repke JT, Cohen A, Caughey AB, Lieberman E (1999) Uterine rupture during induced or augmented labor in gravid women with one prior cesarean delivery. Am J Obstet Gynecol 181(4):882–886. https://doi.org/10.1016/s0002-9378(99)70319-4
Delaney T, Young DC (2003) Spontaneous versus induced labor after a previous cesarean delivery. Obstet Gynecol 102(1):39–44. https://doi.org/10.1016/s0029-7844(03)00355-7
Al-Zirqi I, Stray-Pedersen B, Forsén L, Vangen S (2010) Uterine rupture after previous caesarean section. BJOG 117(7):809–820. https://doi.org/10.1111/j.1471-0528.2010.02533.x
ACOG Practice Bulletin No (2019) 205 Summary: Vaginal Birth After Cesarean Delivery. Obstet Gynecol 133(2):393–395. https://doi.org/10.1097/AOG.0000000000003079
Wing DA. Techniques for ripening the unfavorable cervix prior to induction (2020). http://uptodate.com/contents. Accesed 24 June 2020.
Aslan H, Unlu E, Agar M, Ceylan Y (2004) Uterine rupture associated with misoprostol labor induction in women with previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol 113(1):45–48. https://doi.org/10.1016/S0301-2115(03)00363-4
Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Birth after previous caesarean section (2019). https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Birth-after-previous-Caesarean-Section-(C-Obs-38)Review-March-2019.pdf?ext=.pdf Accessed 24 June 2020
Birth after previous caesarean birth (2015) Green top bulletin No.45. London: RCOG. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_45.pdf Accesed 20 May 2019
Jozwiak M, van de Lest HA, Burger NB, Dijksterhuis MG, De Leeuw JW (2014) Cervical ripening with Foley catheter for induction of labor after cesarean section: a cohort study. Acta Obstet Gynecol Scand 93(3):296–301. https://doi.org/10.1111/aogs.12320
Amorosa J, Stone J, Factor SH, Booker W, Newland M, Bianco A (2017) A randomized trial of Foley Bulb for Labor Induction in Premature Rupture of Membranes in Nulliparas (FLIP). Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2017.04.038
Mackeen AD, Durie DE, Lin M, Huls CK, Qureshey E, Paglia MJ, Sun H, Sciscione A (2018) Foley plus oxytocin compared with oxytocin for induction after membrane rupture: A randomized controlled trial. Obstet Gynecol 131(1):4–11. https://doi.org/10.1097/AOG.0000000000002374
Letailleur M, Mathieu N, Dietrich G et al (2015) Double-balloon device and intravaginal dinoprostone for cervical ripening in women with unfavourable cérvix. Gynecol Obstet Fertil 43:424–430
Boulvain M, Kelly A, Lohse C, Stan C, Irion O (2001) Mechanical methods for induction of labour. The Cochrane database of systematic reviews. https://doi.org/10.1002/14651858.CD001233
Prager M, Eneroth-Grimfors E, Edlund M, Marions L (2008) A randomised controlled trial of intravaginal dinoprostone, intravaginal misoprostol and transcervical balloon catheter for labour induction. BJOG 115(11):1443–1450. https://doi.org/10.1111/j.1471-0528.2008.01843.x
Du YM, Zhu LY, Cui LN, Jin BH, Ou JL (2017) Double-balloon catheter versus prostaglandin E2 for cervical ripening and labour induction: a systematic review and meta-analysis of randomised controlled trials. BJOG 124(6):891–899. https://doi.org/10.1111/1471-0528.14256
de Vaan MD, Ten Eikelder ML, Jozwiak M, Palmer KR, Davies-Tuck M, Bloemenkamp KW, Mol B, Boulvain M (2019) Mechanical methods for induction of labour. The Cochrane database of systematic reviews. https://doi.org/10.1002/14651858.CD001233.pub3
Pennell CE, Henderson JJ, O’Neill MJ, McChlery S, Doherty DA, Dickinson JE (2009) Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG 116(11):1443–1452. https://doi.org/10.1111/j.1471-0528.2009.02279.x
Funding
None.
Author information
Authors and Affiliations
Contributions
JVC and RMM: project development, data analysis, manuscript writing and editing; MSA and MGLP: data collection; MTG, NPL and RCR: manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no conflict of interests.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes.
Research involving Human/animal participants
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
All patients signed an informed consent form for the induction of labor. All women whose data were analyzed gave their written informed consent to study participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cañadas, J.V., González, M.T., Limón, N.P. et al. Intracervical double‐balloon catheter versus dinoprostone for cervical ripening in labor induction in pregnancies with a high risk of uterine hyperstimulation. Arch Gynecol Obstet 304, 1475–1484 (2021). https://doi.org/10.1007/s00404-021-06071-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06071-1