Abstract
Purpose
To evaluate the efficacy and safety of induction in women with a single prior Caesarean section.
Methods
This was a cohort study in which we included all singleton pregnancies in patients with a single prior Caesarean who delivered between 2007 and 2012. Methods of induction were ocytocic infusion plus amniotomy (if Bishop score ≥6) or insertion of a Foley catheter (Bishop <6).
Results
Of the 2,075 patients included, 806 (38.8 %) had an elective repeat Caesarean, 1,045 (50.4 %) went into spontaneous labour, 89 (4.3 %) were induced by artificial rupture of the membranes and infusion of ocytocics and 135 (6.5 %) were induced using a Foley catheter. Rates of vaginal delivery were 79.2, 79.8 and 43.7 %, respectively. Six cases of uterine rupture were reported in the group of patients who went into spontaneous labour. There was no difference between groups with regard to neonatal morbidity. On multivariate analysis, risk factors for Caesarean delivery were macrosomia (OR 2.04, 95 % CI 1.31–3.18) and induction by Foley catheter (OR 3.73, 95 % CI 2.47–5.62); protective factors were previous vaginal delivery (OR 0.41, 95 % CI 0.29–0.57) and cervical dilatation (OR 0.84, 95 % CI 0.78–0.91).
Conclusions
Uterine induction after a single Caesarean section with ocytocic infusion and amniotomy where the cervix is favourable does not appear to entail any significant added risk in terms of maternal or foetal morbidity. Foley catheter induction is a reasonable option if the cervix is not ripe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In France, the rate of Caesarean section is approximately 21 %. We are currently observing a rise in the rate of first Caesareans as well as a rise in the rate of repeat Caesareans [1]. The mean rate of Caesarean section varies considerably from country to country: from 13 % in northern Europe to 32 % in the United States and 48 % in Brazil [2, 3].
After a first Caesarean, a trial of labour is usually proposed [3–5]. For women with a single uterine scar, vaginal delivery enables a significant reduction in maternal morbidity, with a lower rate of transfusions, haemostatic hysterectomies and infectious complications. In addition, there is a better obstetrical prognosis for subsequent pregnancies [6]. In fact, Caesarean delivery carries a greater risk of maternal mortality, and infantile and maternal morbidity as well as complications for subsequent deliveries [7–9].
The principal risk of a trial of labour is uterine rupture [10], which complicates 1 % of attempted vaginal deliveries in developed countries [11]. Moreover, a Caesarean performed during labour is at greater risk of maternal and foetal complications than a repeated elective Caesarean [12, 13].
Some situations demand induction: rupture of the amniotic sac, post-term pregnancy, maternal or foetal disorder. Uterine induction after previous Caesarean section is an acceptable option for the leading learned societies [3–5] but data on efficacy and safety are controversial.
The principal objective of this study was to evaluate the efficacy and safety of induction, by amniotomy and ocytocic infusion or using Foley catheter, in women with a single prior Caesarean section. The secondary objective was to evaluate factors predictive of Caesarean during trial of labour on a uterus scarred from a previous Caesarean.
Methods
This was an observational cohort study conducted in the gynaecology-obstetric hub of Strasbourg, France, which consists of a level 2 maternity and a level 3 maternity hospitals. We included all singleton pregnancies in patients with a single prior Caesarean section, who delivered between 1 October 2007 and 1 May 2012. Data were collected prospectively in the computerized medical dossier.
After evaluating the criteria for a successful vaginal delivery and discussion with the patient [14], it was decided whether to perform a repeat Caesarean or initiate a trial of labour. Where induction was necessary, it was proposed to the patient as an alternative to an immediate Caesarean either by ocytocic infusion plus amniotomy or by inserting a Foley catheter, depending on their Bishop score.
When the Bishop score was ≥6, induction was initiated by ocytocics in accordance with the following protocol: Syntocinon® infusion in an initial dose of 2 mIU per minute for 15 min followed by an incremental step-up every 30 min, without exceeding 20 mIU per minute; amniotomy was performed when contractions were regular and the infant had begun to present [15].
When the Bishop score was <6, Foley catheter induction was proposed unless the following specific contraindications were present: low-lying placenta, hydramnios and suspected chorioamnionitis. The induction protocol was as follows: introduction of an 18-gauge Foley past the internal cervical os after disinfection with an iodine-containing solution; filling of the catheter balloon with 30 cc saline; clamping of the distal extremity of the probe and tension-free attachment to the patient’s thigh; withdrawal of the catheter after 24 h and re-evaluation of the Bishop score; continuing induction by infusion of ocytocics and amniotomy if the Bishop score was ≥6, repeat Caesarean if not.
Assessment criteria were vaginal delivery (with or without instrumental manoeuvre) or Caesarean, occurrence of uterine rupture and neonatal morbidity (pH and Apgar score at 5 min).
A successful outcome for trial of labour was defined as a vaginal delivery with or without instrumental manoeuvre.
Descriptive data were presented as mean and standard error for continuous variables and as numbers and percentages for categorical variables. Comparisons between groups were carried out using ANOVA analysis, Student’s t tests and χ 2 tests. Univariate analysis was performed to identify variables which might account for the occurrence of a Caesarean section. An ascending stepwise multivariate logistic regression model was then constructed. Odds ratio (OR) and their associated confidence interval were computed for each predictor. A p value <0.05 was considered as statistically significant. The statistical software package SAS 9.3 (SAS Institute Inc., Cary, NC, USA) was used for all data analyses.
The study was registered under No. 1656665 with the French data privacy organization CNIL (Commission Nationale de l’Informatique et des Libertés).
Results
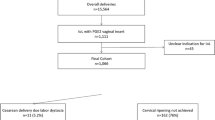
Our study population consisted of 2,075 singleton pregnancies in patients with a single prior Caesarean section: 806 patients (38.8 %) had an immediate repeat Caesarean, 1,045 (50.4 %) went into spontaneous labour, 89 (4.3 %) were induced by artificial rupture of the membranes and ocytocic infusion and 135 (6.5 %) were induced by Foley catheter. The characteristics of these patients as well as data on the newborn are displayed in Table 1. Delivery methods are reported in diagram 1 (Fig. 1). Among patients who had an immediate repeat Caesarean section, 234 were emergency Caesareans (93 cases of preeclampsia, 41 pathological cardiotocography, 26 intra-uterine growth retardation, 20 chorioamnionitis, 19 placenta praevia, 11 abruptio placentae, 24 others) and 572 were planned Caesareans (382 maternal request, 68 breech presentation, 67 diabetes mellitus and/or foetal macrosomia, 39 maternal disease, 16 others).
Comparisons between the group of patients who went into spontaneous labour and the induction group are reported in Table 2. With regard to maternal characteristics, there was no significant difference between the two groups for maternal age, height and previous history of at least one vaginal delivery. Patients who went into spontaneous labour had a significantly lower weight and BMI although this difference did not appear to be clinically relevant. There were significantly more Caesareans in the induction group: 42.0 versus 20.8 % (p < 0.0001). On the other hand, there was no significant difference for the rate of instrumental extractions. Six cases of uterine rupture were observed in the group of patients who went into spontaneous labour, whereas there was no case in the induction group. With regard to neonatal data, the proportion of infants with macrosomia was comparable and there was no significant difference with regard to the neonatal condition between the two groups (pH and Apgar score at 5 min).
Comparisons between the group of patients induced by artificial rupture of the membranes and ocytocic infusion and those induced by Foley catheter are shown in Table 3. There was no difference between the two groups for maternal anthropometric characteristics. In the Foley catheter induction group, significantly fewer patients had had a previous vaginal delivery (23.7 versus 47.2 %, p = 0.0003); they also showed a significantly lower Bishop score (2.1 versus 5.4, p < 0.0001) and smaller degree of cervical dilatation (1.0 versus 2.2 cm, p < 0.0001). There were significantly more Caesareans in the Foley catheter induction group: 56.3 versus 20.2 %, p < 0.0001. This difference persisted even on exclusion of the 41 patients in whom insertion of the Foley catheter had not given rise to a Bishop score ≥6 after 24 h: 37.2 versus 20.2 %, p = 0.01. Indications for Caesarean delivery in the spontaneous labour group were: 104 cases of prolonged labour (48 %), 81 cases of pathological cardiotocography (37 %) and 32 other cases (15 %). Indications for Caesarean delivery in the Foley group were: 41 unsuccessful inductions of labour (54 %), 23 cases of prolonged labour (30 %), 11 cases of pathological cardiotocography (15 %) and one other cases (1 %). For the ocytocic group: three unsuccessful inductions of labour (17 %), eight cases of prolonged labour (44 %), five cases of pathological cardiotocography (28 %) and two other cases (11 %). There was no significant difference with regard to the rate of instrumental extractions. There was no case of uterine rupture among the inductions. There was no significant difference between the two groups with regard to neonatal data.
On multivariate analysis after exclusion of the repeat Caesareans, risk factors for Caesarean delivery proved to be macrosomia (OR 2.04, 95 % CI 1.31–3.18) and Foley catheter induction (OR 3.73, 95 % CI 2.47–5.62). Protective factors were previous vaginal delivery (OR 0.41, 95 % CI 0.29–0.57) and cervical dilatation (OR 0.84, 95 % CI 0.78–0.91). Induction with ocytocic infusion and amniotomy did not appear to present more of a risk for Caesarean than spontaneous labour. All of these results can be found in Table 4. The neonatal status (pH and Apgar score at 5 min) was not affected by the way in which labour was initiated.
Discussion
This study shows that uterine induction by ocytocic infusion and amniotomy after a single prior Caesarean in patients with a favourable Bishop score enabled vaginal delivery to be accomplished in almost 80 % of cases. Foley catheter induction for less favourable Bishop scores enabled vaginal delivery to be attained in 44 % of cases.
Comparable results are found in the literature, with a vaginal delivery rate of between 73.9 and 77.9 % following induction with ocytocics [16, 17], and of between 50.9 and 55.7 % following induction with Foley catheter [16–18]. The vaginal delivery rate following uterine induction with prostaglandins after a single prior Caesarean appears to be almost identical to that for Foley catheter induction [18].
In our study, there was no case of uterine rupture in the induction group, regardless of how labour was induced. Moreover, there was no difference in the neonatal status, regardless of whether labour was induced or spontaneous. The small number in the induction group in our study did not enable an evaluation of the risk of uterine rupture in the event of induced labour, but the fact that we did not observe a single case of rupture among the 225 induced patients is in itself reassuring. This could be due to our small patient cohort size or selection of those undergoing induction of labour. In our entire study population, there were six cases of uterine rupture, a finding which is comparable to published data. The report of the Agency for Healthcare Research and Quality on deliveries after a single prior Caesarean suggests a rate of uterine rupture of 3 per 1,000. This report also indicates a rise in this risk when a trial of labour is attempted after a single prior Caesarean section: 4.7/1,000 versus 0.3/1,000 [19].
It should be noted that the frequency of uterine rupture is highly variable from study to study. This is partly due to a problem in defining uterine rupture, which can be classified into two categories: complete rupture, corresponding to a tear extending across the entire thickness of the uterine wall (myometrium and peritoneum with tearing of the membranes), and incomplete rupture or detachment where only the myometrium tears, while the peritoneum and membranes remain intact. In the latter case, these tears may go unnoticed and are usually without maternal or foetal impact [20]. In addition, since rupture is fortunately a rare phenomenon, studies are often faced with a problem of statistical power. Lastly, analysis of the literature on this topic is made difficult because of the heterogeneity of the studies: there may be differences in the study populations, in the acceptation criteria for vaginal delivery, in induction methods and even in the ways in which trial of labour is conducted.
For single prior Caesarean section, the reported incidence of uterine rupture during spontaneous labour ranges between 0.30 and 0.52 %, between 0.74 and 3.01 % for induction with ocytocics, between 0.76 and 2.48 % for induction using mechanical methods, and between 0.30 and 3.95 % for induction with prostaglandins [10, 11, 15, 21–27]. All the results for data in the literature are reported in Table 5. It may be noted that the risk of uterine rupture is never zero, even for elective Caesarean section: 0.16–0.25 % [11–24].
In sum, the risk of uterine rupture is probably slightly increased during induction with a Foley catheter compared to the risk during spontaneous labour, although data in the literature are not conclusive. The option of mechanical induction nevertheless seems reasonable. The use of prostaglandins is probably associated with a higher risk of uterine rupture than mechanical methods such as the Foley catheter. It would not seem reasonable to advocate their use, especially since they are not any more effective in procuring vaginal delivery [17]. A recent review of the literature on the induction of patients with healthy uteruses incidentally showed that mechanical methods are just as effective as prostaglandins while being associated with a lower risk of provoking uterine hypertonus [28]. For the leading learned societies, induction of labour with ocytocics in women with a single uterine scar is permissible and mechanical methods may be an acceptable second choice. All recommendations contraindicate the use of prostaglandins, except for those of the Royal College of Obstetricians and Gynaecologists which provide for their use in a reduced dose [29–34].
The secondary objective of the study was to evaluate the factors predictive of a successful outcome of trial of labour in the uterus after previous Caesarean section. We found that the risk factors for Caesarean delivery were macrosomia and Foley catheter induction, while protective factors were previous vaginal delivery and cervical dilatation. Induction with ocytocics plus amniotomy did not appear to present a greater risk of Caesarean than spontaneous labour. These results are comparable to previously published data [19]. It would seem entirely legitimate to inform patients about these risk factors so that they can be fully informed about their choices when selecting between a repeat Caesarean and trial of labour, in particular in the event of induction with an unfavourable Bishop score.
In conclusion, uterine induction after a single prior Caesarean section with ocytocic infusion and amniotomy where the cervix is favourable does not appear to entail any significant added risk in terms of maternal or foetal morbidity. Foley catheter induction is a reasonable option if the cervix is not ripe.
References
Blondel B, Lelong N, Kermarrec M, Goffinet F, Coordination nationale des Enquêtes Nationales Périnatales (2012) Trends in perinatal health in France between 1995 and 2010: Results from the National Perinatal Surveys. J Gynecol Obstet Biol Reprod (Paris) 41(2):151–166. doi:10.1016/j.jgyn.2011.11.008
Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Kirmeyer S, Osterman MJ (2010) Births: final data for 2007. Natl Vital Stat Rep 58(24):1–85
OCDE (2011) Panorama de la santé 2011: Les indicateurs de l’OCDE, Éditions OCDE. doi:10.1787/health_glance-2011-fr
CNGOF (2012) Conférence de consensus du CNGOF sur l’accouchement en cas d’utérus cicatriciel. http://www.cngof.asso.fr/D_TELE/RPC_uterus_cicatriciel_2012.pdf
American College of Obstetricians and Gynecologists (2010) ACOG Practice bulletin no. 11: vaginal birth after previous cesarean delivery. Obstet Gynecol 116(2 Pt 1):40–63. doi:10.1097/AOG.0b013e3181eeb21
National Institutes of Health Consensus Development Conference Panel (2010) Vaginal birth after cesarean: new insights. Obstet Gynecol 115(6):1279–1295. doi:10.1097/AOG.0b013e3181e459e5
Rossi AC, D’Addario V (2008) Maternal morbidity following a trial of labor after cesarean section versus elective repeat cesarean delivery: a systematic review with metaanalysis. Am J Obstet Gynecol 199:224–231
Minkoff H, Chervenak FA (2003) Elective primary cesarean delivery. N Engl J Med 348:946–950
Bewley S, Cockburn J (2002) The unfacts of ‘request’ Caesarean section. BJOG 109(6):597–605
Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A, Shah A, Campodónico L, Bataglia V, Faundes A, Langer A, Narváez A, Donner A, Romero M, Reynoso S, de Pádua KS, Giordano D, Kublickas M, Acosta A (2006) Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet 367(9525):1819–1829
Macones GA, Peipert J (2005) Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol 193(5):1656–1662
Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 345(1):3–8
McMahon MJ, Luther ER, Bowes WA Jr, Olshan AF (1996) Comparison of a trial of labor with an elective second cesarean section. N Engl Med 335:689–695
Rosen MG, Dickinson JC, Westhoff CL (1991) Vaginal birth after cesarean: a meta-analysis of morbidity and mortality. Obstet Gynecol 77:465–470
Rozenberg P (2005) The counselling of patient with prior C-section. Gynecol Obstet Fertil 33(12):1003–1008
Collège national des gynécologues et obstétriciens français (1995) Conférence de consensus sur le déclenchement, Paris. http://www.gyneweb.fr/sources/obstetrique/consens.htm
Bujold E, Blackwell SC, Gauthier RJ (2004) Cervical ripening with transcervical foley catheter and the risk of uterine rupture. Obstet Gynecol 103(1):18–23
Landon MB, Leindecker S (2005) The MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean delivery. Am J Obstet Gynecol 193(3 Pt 2):1016–1023
Ben-Aroya Z, Hallak M, Segal D, Friger M, Katz M, Mazor M (2002) Ripening of the uterine cervix in a post-cesarean parturient: prostaglandin E2 versus Foley catheter. J Matern Fetal Neonatal Med 12(1):42–45
Agency for Healthcare Research and Quality (03) Vaginal birth after cesarean. http://archive.ahrq.gov/downloads/pub/evidence/pdf/vbac/vbac.pdf
D’ercole C, Bretelle F (2007) Modalités d’accouchement en cas d’utérus cicatriciel, mécaniques et techniques obstétricales, 3rd edn. Sauramps Médical, Montpellier, France, pp 753–764
Ravasia DJ, Wood SL, Pollard JK (2000) Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am J Obstet Gynecol 183(5):1176–1179
Landon MB, Hauth JC et al (2004) Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 351(25):2581–2589
Blanchette H, Blanchette M, McCabe J, Vincent S (2001) Is vaginal birth after cesarean safe? Experience at a community hospital. Am J Obstet Gynecol 184(7):1478–1484 (discussion 1484-7)
Wen SW, Rusen ID et al (2004) Comparison of maternal mortality and morbidity between trial of labor and elective cesarean section among women with previous cesarean delivery. Am J Obstet Gynecol 191(4):1263–1269
Sanchez-Ramos L, Gaudier FL, Kaunitz AM (2000) Cervical ripening and labor induction after previous cesarean delivery. Clin Obstet Gynecol 43(3):513–523
Yogev Y, Ben-Haroush A, Lahav E, Horowitz E, Hod M, Kaplan B (2004) Induction of labor with prostaglandin E2 in women with previous cesarean section and unfavorable cervix. Eur J Obstet Gynecol Reprod Biol 116(2):173–176
Locatelli A, Regalia AL, Ghidini A, Ciriello E, Biffi A, Pezzullo JC (2004) Risks of induction of labour in women with a uterine scar from previous low transverse caesarean section. BJOG 111(12):1394–1399
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M (2012) Mechanical methods for induction of labour. Cochrane Database Syst Rev 3:CD001233
Carbonne B, Frydman R, Goffinet F, Pierre F, Subtil D (2000) Recommandations pour la pratique Clinique du CNGOF : Cesariennes conséquences et indications. http://www.cngof.asso.fr/D_PAGES/PURPC_08.HTM
Haute autorité de santé (2008) Recommandations pour la pratique clinique de la Haute autorité de santé sur le déclenchement artificiel du travail à partir de 37 semaines d’aménorrhée. http://www.has-sante.fr/portail/upload/docs/application/pdf/declenchement_artificiel_du_travail_-_recommandations.pdf
SOGC clinical practice guidelines (2005) Guidelines for vaginal birth after previous caesarean birth. Int J Gynaecol Obstet 89:319–331
ACOG (2010) Practice bulletin no. 115. Vaginal birth after previous cesarean delivery. Obstet Gynecol 116:450–463
Royal College Of obstetricians and gynecologists (2007) Birth after previous Caesarian birth. Green-Top Guideline. http://www.rcog.org.uk/files/rcog-corp/GTG4511022011.pdf
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sananès, N., Rodriguez, M., Stora, C. et al. Efficacy and safety of labour induction in patients with a single previous Caesarean section: a proposal for a clinical protocol. Arch Gynecol Obstet 290, 669–676 (2014). https://doi.org/10.1007/s00404-014-3287-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3287-4