Abstract
Objectives
In understanding early disturbances in the mother–child relationship, maternal–fetal attachment has become an important concept. To date no study has investigated the reliability and validity of the German version of the Maternal Fetal Attachment Scale (MFAS). The present study aimed to close this gap.
Methods
Questionnaires were completed in a sample of 324 women [third trimester (T1), first week postpartum (T2), and 4 months postpartum (T3)]. In addition to the MFAS (T1), the following measures were assessed: the questionnaire of partnership (T1), the postpartum bonding questionnaire (T2), the Edinburgh Postnatal Depression Scale (T1–T3), the State Trait Anxiety Inventory (T1–T3), and the pregnancy related anxiety questionnaire (T1–T3). Factor structure was analyzed using a principal component analysis (PCA) with varimax rotation. Internal and convergent validities were calculated.
Results
In contrast to the original version with five subscales, PCA yielded a three-factor solution, consisting of the three independent dimensions “anticipation”, “empathy”, and “caring”, explaining 34.9% of the variance together. Good internal reliabilities were found for the total MFAS scale. Maternal–fetal attachment showed a significant negative correlation with postpartum bonding impairment. While no correlations were found with depression, general anxiety and pregnancy-related anxiety during pregnancy, maternal–fetal attachment was significantly related to aspects of partnership quality. In the postpartum period, maternal attachment showed a strong negative correlation with maternal anxiety.
Conclusions
Our results suggest that the German version of the MFAS is a reliable and valid questionnaire to measure the emotional relationship of the mother to the unborn child during pregnancy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pregnancy is characterized by biological, psychological, and social changes in a woman’s life [34]. Additionally, the foundation of the mother–child relationship takes root in this period [5, 10, 54, 59]. These first important maternal feelings towards the unborn child are termed maternal–fetal attachment or bonding [12, 16, 45] and represent the basis of the attachment theory [6].
This relationship between a mother and her unborn child has been associated with different important outcomes, including not only the woman, her well-being, and mental health during pregnancy [36], but also parent–child interaction postpartum [55], infant mood [64] and psychopathological disorders, especially anxiety disorders, in the offspring [8, 23, 53].
Understanding the roots of the early mother–child relationship and its influencing factors has therefore recently not only been the subject of many studies, but has also formed the basis for risk assessment and prenatal educational interventions [63].
Most longitudinal studies on maternal antenatal attachment reported a gradual increase in attachment feelings [5, 54, 63]. As the pregnancy progresses, the connection with the fetus is favored due to actual experiences, such as the quickening of the fetus and visualizing it through ultrasound scans [19, 28, 31].
Several factors play an important role in maternal–fetal attachment [3, 40, 63]. Maternal perinatal mental health problems such as anxiety, low self-esteem, and depression were found to be related to postnatal parenting stress [42, 47]. Furthermore, poor relationship functioning in mid-pregnancy was found to predict vulnerability to postnatal distress [43]. Therefore, maternal–fetal attachment, the couples’ relationship quality, bonding, and postnatal parenting stress seem to be closely linked, but studies examining these links together are sparse in the current literature.
When it comes to attempting to quantify attachment, the Maternal Fetal Attachment Scale (MFAS) was the first self-report questionnaire developed to measure the extent of the attachment between a mother and her unborn child [16]. The MFAS has been widely used to assess maternal–fetal attachment [20, 44, 61]. However, the German version has not been validated yet. Therefore, this study aimed to investigate the psychometric properties of the German version of the MFAS. In addition, we analyzed both the internal and the convergent validity of the German version of the MFAS by assessing associations with construct-related and construct-unrelated psychometric measures. We hypothesized that the construct of maternal–fetal attachment suggests a strong relation with postpartum bonding and relationship skills, but not with measurements of depression and anxiety in peripartum women.
Methods
Participants and study design
The present study is part of a prospective study that was conducted at a perinatal center of maximum care between January and August 2014. Screening procedure is described elsewhere in detail [62] and is briefly summarized here. Participants were at least 18 years old, in the third trimester of pregnancy, and fluent in the German language. Informed consent was obtained from all participants. Questionnaires were completed at three different time points: third trimester (T1, N = 330), first week postpartum (T2, N = 247), and 4 months postpartum (T3, N = 154). In all, six women were excluded from data analysis as they did not complete the MFAS at TI. Due to scale- and time-specific amounts of missing values, the valid number of cases n varied depending on the data subsets. Ethical approval was granted by the Ethical Committee of the University of Heidelberg.
Measurements
Maternal Fetal Attachment Scale (MFAS)
For the MFAS [16], Cranley defined six aspects of early bonding that were used as labels for the subscales. The content was obtained by consulting with other clinicians and a group of Lamaze teachers. After subsequent validation analyses in a sample of women in the third trimester of pregnancy, the final version consisted of 24 items organized into five subscales corresponding to five aspects of the relationship between mother and fetus: (1) differentiation of self from the fetus; (2) interaction with the fetus; (3) attributing characteristics and intentions to the fetus; (4) giving of self; and (5) roletaking. The 24 items are scored on a 7-point Likert scale (1 ‘definitely no’ to 7 ‘definitely yes’). A higher sum score is associated with a greater extent of prenatal maternal attachment to the fetus. The original version was translated into German and back translated into English by the first and the last authors and a team of psychologists, including an independent scientific translator, and piloted in a previous study [21].
Postpartum bonding questionnaire (PBQ)
Postpartum bonding disorders of the mother to her child were assessed by the abridged German version of the postpartum bonding questionnaire (PBQ-16) [7, 49]. The response categories range from ‘always’ to ‘never’ on a 6-point Likert scale, with a higher sum score indicating lower bonding. The sum scores range between 0 and 80 points. The PBQ score reached a good internal consistency of Cronbach’s α = 0.82 (T2) and α = 0.85 (T3).
Edinburgh Postnatal Depression Scale (EPDS)
The EPDS was originally developed by Cox et al. [15] and translated into German by Bergant et al. [4]. It consists of 10 items scored from 0 to 3 (normal response 0 and severe response 3) assessing depressive symptoms during the past 7 days [38]. Internal consistency was good for our sample (T1: α = 0.87, T2: α = 0.86, T3: α = 0.90).
State-Trait Anxiety Inventory (STAI)
The STAI was developed by Spielberger et al. [57] and translated into German by Laux et al. [33]. Based on Cattell’s theory of anxiety [11], the STAI consists of two scales (STAI-S and STAI-T) with 20 items each, to separately assess anxiety as a general characteristic (= trait) or as a temporary condition (= state). Items are coded with points (1–4), which are added to a total value. A total value of 20 means absolute absence of anxiety whereas 80 points means highest level of anxiety. The STAI was validated for pregnancy by Grant el al. [25]. Internal consistency was shown to be excellent (STAI-S T1: α = 0.93, T2: α = 0.91, T3: α = 0.94; STAI-T T1: α = 0.92, T2: α = 0.91, T3: α = 0.94).
Questionnaire on partnership (PFB)
The questionnaire on partnership (PFB) assesses general aspects of partnership, consisting of 30 four-point items which are categorized into three scales: conflict behavior, tenderness, and communication [26]. Previous analyses have confirmed adequate scale reliability [29]. In our sample, Cronbach’s α was excellent (α = 0.92).
Salmon’s items list (SIL-17)
The Salmons items list (SIL) assesses the birth experience in mothers, consisting of a 20-item questionnaire developed from terms and expressions used by women spontaneously after birth to describe their experience [52]. Items are rated on a numerical scale from 1 to 7. Scores > 70 suggest a positive birth experience [58].
Statistical analyses
We used the Statistical Package for Social Sciences (IBM® SPSS® v. 24.0.0.0) for all analyses conducted. Little’s MCAR test confirmed equality between excluded cases and the remaining sample (χ2 = 8092.11, df = 7949, p = 0.13) [37]. A principal component analysis (PCA) was carried out in order to assess whether the original five-scale structure of the MFAS could be validated on the basis of our data. Loadings of each item on each factor were then calculated using varimax rotation. Cronbach’s alpha was calculated to evaluate internal consistency. The relationship between MFAS scores and both sociodemographic and questionnaire scores was examined using Pearson correlation coefficients. Two-sided statistical significance was evaluated at the 5% level.
Results
Descriptive characteristics
Sample characteristics are demonstrated in Table 1. Valid cases (N), minimum (Min) and maximum (Max) values, means (M), and standard deviations (SD) of the questionnaire data are displayed in Table 2.
Principal component analysis (PCA)
The Kaiser–Meyer–Olkin measure of sampling was KMO = 0.762, indicating a substantial amount of linear relationships between the items. Bartlett’s test of sphericity was significant (χ2 = 1606.610, df = 276, p < 0.001), indicating that the item-intercorrelation matrix is different from the identity matrix and, thus, data are appropriate for conducting a factor analysis. The measures of sample adequacy were MSA > 0.640 for the items, indicating substantial linear relationships of each item to the remaining ones except for item 22 (MSA = 0.577). However, to evaluate the factor structure as a whole and for reasons of face validity, this single item was not excluded initially.
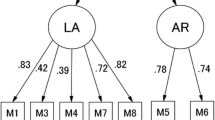
In the beginning, a visual analysis of the scree plot (see Fig. 1) was generated in order to get an idea of the number of expected factors. It suggested a four-factor solution. Horn’s parallel analysis [48] and Velicer’s original and revised minimum average partial (MAP) test [48] suggested a three-factor solution. Thus, we decided to extract three factors. Factor loadings are shown in Table 3. The cumulative variance accounted for by the model was 34.9%. After rotation, factor 1 had an eigenvalue of 3.3 and explained 13.9% of variance (initial eigenvalue = 4.8; explained variance = 19.9%). Factor 2 had an eigenvalue of 3.0 and explained 12.6% of variance (initial eigenvalue = 2.0; explained variance = 8.5%). Factor 3 had an eigenvalue of 2.0 and explained 8.4% of variance (initial eigenvalue = 1.6; explained variance = 6.5%).
In a next step, the item loadings on the three factors of the rotated solution were analyzed: item loadings of a < 0.20 were neglected. Items were assigned to the factor they loaded the most and if the Fürntratt criterion (a2 > h2/2) was fulfilled. Only two items (9 and 13) did not meaningfully load onto any of the extracted factors.
Reliability
The MFAS reached a good internal consistency, with an ICC = 0.772 [95% CI (0.732; 0.810)] and a Cronbach’s α = 0.806 (standardized items). The reliability was not enhanced by excluding any of the items (Cronbach’s α if items deleted < 0.781). The three-factor solution yielded the following values: factor 1 α = 0.747, factor 2 α = 0.684, and factor 3 α = 0.53. As only factor 1 had an acceptable internal consistency, we decided to continue the analyses only with the factor values. Analyzing the item contents for each factor, factor 1 might reflect “anticipation”, while factor 2 might reflect “empathy” and factor 3 “caring”.
Sociodemographic and obstetric correlates
The correlative associations of the MFAS sum score are depicted in Table 4a. There were no significant associations between the MFAS sum score and sociodemographic or obstetric variables. Regarding the subscales, factor 1 “anticipation” was negatively associated with maternal age (p = 0.020), income (p = 0.009), and maternal education (p = 0.014).
“Empathy” was also negatively associated with maternal education (p = 0.003). “Caring” was negatively associated with gravidity (p = 0.033) and c-section (p = 0.005); and positively associated with maternal education (p < 0.001) and infant gender (p = 0.001; if women reported more caring, they more likely gave birth to a girl).
Convergent and predictive validity
The associations of the MFAS to related constructs are demonstrated in Table 4b. There were small to moderately negative associations between the MFAS sum score and low maternal bonding (PBQ-16) at T2 (p < 0.001) and T3 (p = 0.03) as well as a positive association to partnership satisfaction (PFB sum score; p = 0.005) at T1. Of the PFB subscales, “tenderness” (p < 0.001) and “communication” (p = 0.002) were positively associated with the MFAS sum score. Furthermore, there were positive associations to a positive birth experience (SIL-17 sum score; p = 0.026) and the subscale “fulfillment” (p = 0.001) at T2.
The factor “anticipation” was negatively associated with low maternal bonding (PBQ-16) at T2 (p < 0.001) and T3 (p = 0.001) as well as positively to general partnership satisfaction at T1 (PFB sum score; p < 0.001) and all PFB subscales (p < 0.038). Furthermore, there was a positive association to the SIL sub scale “fulfillment” (p = 0.015). The factor “caring” was negatively related to low maternal bonding at T2 (p = 0.044), positively to general partnership satisfaction (PFB sum score; p = 0.009), “tenderness” (p = 0.038), “communication” (p = 0.001) at T1, and the SIL subscale “negative experience”.
Maternal mental health
In order to determine the relationship between fetal attachment and maternal mental health, MFAS, EPDS, and STAI scores were subjected to correlational analysis (Table 4b). Fetal attachment was not associated with maternal depressive symptoms (EPDS) as all p values were above 0.143. Surprisingly, mothers who experienced less anxiety at T2 had significantly higher fetal attachment scores at T1, as maternal state (p = 0.003) and trait anxiety (p = 0.021) showed a significant negative association to fetal attachment (Table 5).
Regarding the subscales, the factor “anticipation” was negatively related to trait anxiety (STAI-T) at T1 (p = 0.010) and T2 (p = 0.024). “Empathy” was positively associated with maternal depressive symptoms (EPDS; p < 0.001) and trait anxiety (STAI-T; p = 0.002) at T1, while “caring” was negatively associated with maternal depressive symptoms (EPDS) at T1 (p = 0.004) as well as state anxiety (STAI-S) at T1 (p < 0.001), T2 (p = 0.040), and T3 (p = 0.046). Furthermore, it was negatively related to trait anxiety (STAI-T) at T1 (p < 0.001) and T2 (p = 0.017).
Discussion
Reliability and construct validity of the MFAS
This study represents the first analyses of the psychometric characteristics of the German version of the MFAS. In summary, our results appeared to be most reliable with a three-factor solution, consisting of the independent dimensions “anticipation”, “empathy”, and “caring”, with a cumulative variance of 34.9% and with a good internal consistency of Cronbach’s α = 0.806. This is in line with other validation studies reporting Cronbach’s alpha values for the total scale between 0.72 and 0.92 [1, 9, 61]. We further discovered that two items [9 (“I can almost guess what my baby’s personality will be from the way he moves around” and 13 “I have decided on a name for a girl (a boy) baby”)] had no meaningful loading on any of these factors. However, as excluding any of the items did not enhance the reliability, we do not recommend the use of an abridged version.
Widely criticized for the problematic validity of the subscales [44], a problem that potentially derives from the fact that the construction of the subscales was not based on any statistical technique [61], many factor analyses on MFAS items were conducted. None of the studies could fully support Cranley’s five subscales: Muller and Ferketich [44] reported two and three factors, Sjögren et al. [56] and Van den Bergh and Simons [61] revealed four factors, while Busonera et al. [9], in line with our findings, described a three-factor solution. The latter identified the dimensions “future parental roletaking”, “present interaction with the baby”, and “giving of self and responsibility” (2016). The distribution of the other items mostly resembles the distribution of our analysis with comparable Cronbach’s alpha for the subscales factor 1 α = 0.77 (good), factor 2 0.64 (acceptable), and factor 3 0.56 (poor).
Our results underline that the items belonging to factor 1 “anticipation” indicate all coherent statements concerning the mothers’ expectations and future parental role taking, proven by an acceptable internal consistency of Cronbach’s α = 0.747. Furthermore, the internal consistency of the items attributed to factor 2 “empathy” was quite acceptable (0.684). Only the statements attributed to factor 3 “caring” seem to be very heterogeneous, which is represented by a Cronbach’s α = 0.537.
However, having explained 34.9% of the variance, our findings seem to be a promising model. Overall, the original version of the MFAS was shown to be a reliable and valid instrument.
Sociodemographic determinants of maternal–fetal attachment
Our study results showed no significant relationship between maternal–fetal attachment and age, parity, gravidity, or socioeconomic status. Consistent with previous findings [32, 65], parity had no relationship with maternal–fetal attachment. Also in line with previous research, the correlation between education and maternal–fetal attachment was only moderately significant and therefore negligible [36]. While some authors found that age contributed significantly to maternal–fetal attachment (the younger, the higher the attachment) [32, 36], others confirmed our results and found no significant influence [9, 16].
Regarding the subscales, factor 1 “anticipation” was negatively associated with maternal age, income, and maternal education. According to Damato et al. [18], older women are possibly more aware of the changes that come with pregnancy and a child in contrast to younger women, who are assumed to attribute more value to the pregnancy in terms of role fulfillment. These findings are also in line with a study examining the psychometric properties of a similar construct, the Maternal Antenatal Attachment Scale (MAAS) [60]. Consistent with the findings of the latter report, which describes that higher educated and multiparous women were less preoccupied with their fetuses [60], we could show that factor 2 “empathy” was negatively associated with maternal education and factor 3 “caring” was negatively associated with gravidity and having a c-section. Furthermore, maternal education was significantly and positively associated with factor 3 “caring”. This underlines the importance of the difference between “empathy” in the sense of “to empathize with the unborn child”, influenced by intrinsic factors, and “caring” in the sense of “worrying” or “being anxious”, influenced more by external factors such as history of preterm birth. Interestingly, we found that the factor “caring” was also positively related to the inverted SIL sub scale “negative experience”, which points out the potentially negative influence of worrying on the birth experience.
Maternal–fetal attachment, postpartum bonding, and relationship quality
Low MFAS scores correlated with a higher frequency of bonding impairment postpartum, proving the consistent, prospective validity of the MFAS. The influence of attitudes towards the unborn baby on the first impression of the newborn [13] and the correlation between antenatal and postnatal bonding [19, 46] have been the topic of many investigations. In line with our findings, these studies showed that the higher the prenatal attachment, the stronger is the bonding postnatally [51, 60].
“Tenderness” and “communication” in the couples’ relationship were also positively associated with the MFAS sum score, which enables us to speculate whether the ability to maintain meaningful relationships with a significant partner constitutes the key-competence for generating maternal–fetal attachment, indicating that representations of other relationships are also important for maternal–fetal attachment. Previous studies reported that relationships with significant others (own partner [30, 63], the father [39], the mother [17]) have a positive association with maternal–fetal attachment. Mikulincer and Florian [41] report an association of romantic attachment security in adult relationships with quality of maternal–fetal attachment and mental health throughout pregnancy. Walsh et al. [63] identified, in addition to the “adult romantic attachment”, the dimension of “caregiving responsiveness to partner” as an important predictor for the maternal–fetal relationship, assuming that this caregiving system may also form the earliest representation of a mother’s relationship with her unborn child.
Recognizing “anticipation” as the idea of future “caregiving”, these findings are in line with our results, as the factor “anticipation” was positively associated with general partnership satisfaction and maternal bonding.
Maternal–fetal attachment and mental health
Maternal–fetal attachment had no significant association with maternal depressive symptoms (EPDS) at any time, thus supporting the discriminant validity of the German version of the MFAS. Furthermore, there was no significant correlation with pregnancy-related anxiety. These results are in line with previous findings, which could not show any correlation between depression [30], general anxiety [39], or pregnancy-related anxiety [2] and maternal–fetal attachment. Condon and Esuvaranathan [14] did not find any association at all between maternal–fetal attachment and maternal mood state. In contrast to the latter, our results discovered a negative association between maternal–fetal attachment and maternal state and trait anxiety in the early postpartum period. The higher the attachment was, the lower the state and trait anxiety.
Considering the subscales, the factor “anticipation” was negatively related to trait anxiety, while “empathy” was positively associated with maternal depressive symptoms and trait anxiety in the third trimester. “Caring”, however, was negatively associated with state anxiety over all time points. These findings underline again the subtle distinction of the subscales: “Anticipation”, in the sense of “future parental role taking”, as a purely intrinsic factor, includes the dimension of “caregiving responsiveness” to the partner and the unborn child, but also to the mother herself, by influencing her trait anxiety and vice versa. “Empathy”, in contrast, indicates the vulnerable characteristics of the mother for developing depressive symptoms or anxiety. “Caring”, the only factor associated with state anxiety, again seems to be influenced by external factors. This is in line with the findings of other authors, who reasoned that the mothers’ preoccupation state seems to be determined more by external factors such as employment or the presence of other children [27, 60].
In contrast to Cranley’s findings, reporting an inverse correlation between perceived prenatal stress and maternal–fetal bonding [16], many studies identified prenatal anxiety [35, 42] and poor relationship functioning at mid-pregnancy [43] as risk factors for postnatal parenting stress, influencing bonding relations [22] as well as behavioral and emotional outcomes in the offspring [25]. Bonding, in turn, was assumed to buffer parenting stress [50].
We were able to demonstrate that the higher the maternal–fetal attachment was influenced by relationship quality, the lower postnatal bonding impairment was, raising the question of whether strengthening maternal–fetal attachment could buffer subsequent parenting stress by reducing maternal trait anxiety and bonding impairment. Therefore, the correlations of prenatal anxiety disorders and potential protective effects of maternal–fetal attachment on relationship quality, anxiety disorders, bonding impairment, and parenting stress should be the subject of future research.
Limitations
Some results should be interpreted with caution. First, most variables of interest were assessed by self-report measurements and, therefore, potentially bear the risk for cognitive biases. For example, patients with depressive symptoms in particular tend to selectively place attention on negative information [24].
Second, data were collected from a highly educated sample of pregnant women rather than from population-based subjects. The results obtained for this specific group, therefore, cannot readily be generalized to broader populations. Furthermore, anxiety disorders and depression were not diagnosed according to DSM-IV or ICD-10 criteria. This could be a limitation, on the one hand, but it also supports the theory that even subclinical symptoms can impair attachment, which, on the other hand, emphasizes the relevance of our findings.
Conclusions
Overall, the original version of the MFAS is a reliable and valid instrument to measure maternal–fetal attachment. Our results emphasize that the MFAS measures aspects of relationship quality to the unborn child, underlined by strong construct-related correlations to bonding and partnership quality. Strengthening maternal–fetal attachment in the prenatal period as an effective prevention of postpartum bonding impairment with its extensive consequences for developmental psychopathology in childhood should be implemented in routine prenatal clinical care and in prenatal classes. The examination of the fascinating association with anxiety, shown in a reduction of postpartum anxiety in women with high prenatal attachment, should be the subject of further research.
References
Anand L, Hima B (2012) Validation of Tamil version of Cranley’s 24-item Maternal fetal Attachment Scale in Indian pregnant women. J Obstet Gynecol India 62:630–634
Armstrong D, Hutti M (1998) Pregnancy after perinatal loss: the relationship between anxiety and prenatal attachment. J Obstet Gynecol Neonatal Nurs 27:183–189
Barone L, Bramante A, Lionetti F, Pastore M (2014) Mothers who murdered their child: an attachment-based study on filicide. Child Abuse Negl 38:1468–1477. https://doi.org/10.1016/j.chiabu.2014.04.014
Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O (1998) German language version and validation of the Edinburgh postnatal depression scale. Dtsch Med Wochenschr 123:35–40. https://doi.org/10.1055/s-2007-1023895
Bicking Kinsey C, Hupcey JE (2013) State of the science of maternal–infant bonding: a principle-based concept analysis. Midwifery 29:1314–1320. https://doi.org/10.1016/j.midw.2012.12.019
Bowlby J (1969) Attachment and loss attachment, vol 1. Basic Books, New York
Brockington IF, Oates J, George S, Turner D, Vostanis P, Sullivan M, Loh C, Murdoch C (2001) A screening questionnaire for mother–infant bonding disorders. Arch Womens Ment Health 3:133–140
Busch AL, Cowan PA, Cowan CP (2008) Unresolved loss in the adult attachment interview: implications for marital and parenting relationships. Dev Psychopathol 20:717–735. https://doi.org/10.1017/S0954579408000345
Busonera A, Cataudella S, Lampis J, Tommasi M, Zavattini GC (2016) Psychometric properties of a 20-item version of the Maternal Fetal Attachment Scale in a sample of Italian expectant women. Midwifery 34:79–87. https://doi.org/10.1016/j.midw.2015.12.012
Castellano R, Velotti P, Crowell JA, Zavattini GC (2014) The role of parents’ attachment configurations at childbirth on marital satisfaction and conflict strategies. J Child Fam Stud 23:1011–1026
Cattell RB, Scheier IH (1961) The meaning and measurement of neuroticism and anxiety. Ronald, Oxford
Condon JT (1993) The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol 66(Pt 2):167–183
Condon JT, Dunn DJ (1988) Nature and determinants of parent-to-infant attachment in the early postnatal period. J Am Acad Child Adolesc Psychiatry 27:293–299. https://doi.org/10.1097/00004583-198805000-00005
Condon JT, Esuvaranathan V (1990) The influence of parity on the experience of pregnancy: a comparison of first- and second-time expectant couples. Br J Med Psychol 63(Pt 4):369–377
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786
Cranley MS (1981) Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res 30:281–284
Curry MA (1987) Maternal behavior of hospitalized pregnant women. J Psychosom Obstet Gynaecol 7:165–182
Damato EG (2004) Predictors of prenatal attachment in mothers of twins. J Obstet Gynecol Neonatal Nurs 33:436–445
Damato EG (2004) Prenatal attachment and other correlates of postnatal maternal attachment to twins. Adv Neonatal Care 4:274–291
Doan HM, Cox NL, Zimerman A (2003) The maternal fetal attachment scale: some methodological ponderings. J Prenat Perinat Psychol Health 18(2):167–188
Dubber S, Reck C, Muller M, Gawlik S (2015) Postpartum bonding: the role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Arch Womens Ment Health 18:187–195. https://doi.org/10.1007/s00737-014-0445-4
Feldman R, Gordon I, Zagoory-Sharon O (2011) Maternal and paternal plasma, salivary, and urinary oxytocin and parent–infant synchrony: considering stress and affiliation components of human bonding. Dev Sci 14:752–761. https://doi.org/10.1111/j.1467-7687.2010.01021.x
Goldberg S, Benoit D, Blokland K, Madigan S (2003) Atypical maternal behavior, maternal representations, and infant disorganized attachment. Dev Psychopathol 15:239–257
Gotlib IH, Joormann J (2010) Cognition and depression: current status and future directions. Annu Rev Clin Psychol 6:285–312. https://doi.org/10.1146/annurev.clinpsy.121208.131305
Grant KA, McMahon C, Reilly N, Austin MP (2010) Maternal sensitivity moderates the impact of prenatal anxiety disorder on infant mental development. Early Hum Dev 86:551–556. https://doi.org/10.1016/j.earlhumdev.2010.07.004
Hahlweg K (1979) Konstruktion und Validierung des Partnerschaftsfragebogens PFB. Z Klin Psychologie 8:17–40 (German)
Hart R, McMahon CA (2006) Mood state and psychological adjustment to pregnancy. Arch Womens Ment Health 9:329–337. https://doi.org/10.1007/s00737-006-0141-0
Heidrich SM, Cranley MS (1989) Effect of fetal movement, ultrasound scans, and amniocentesis on maternal–fetal attachment. Nurs Res 38:81–84
Hinz A, Stöbel-Richter Y, Brähler E (2001) Der Partnerschaftsfragebogen (PFB): Normierung und soziodemographische Einflussgrößen auf die Partnerschaftsqualität. Diagnostica
Hjelmstedt A, Widstrom AM, Collins A (2006) Psychological correlates of prenatal attachment in women who conceived after in vitro fertilization and women who conceived naturally. Birth 33:303–310. https://doi.org/10.1111/j.1523-536X.2006.00123.x
Ji EK, Pretorius DH, Newton R, Uyan K, Hull AD, Hollenbach K, Nelson TR (2005) Effects of ultrasound on maternal–fetal bonding: a comparison of two- and three-dimensional imaging. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 25:473–477. https://doi.org/10.1002/uog.1896
Kemp VH, Page CK (1987) Maternal prenatal attachment in normal and high-risk pregnancies. J Obstet Gynecol Neonatal Nurs 16:179–184
Laux L, Glanzmann P, Schaffner P, Spielberger CD (1981) Das State-Trait-Angstinventar (Testmappe mit Handanweisung, Fragebogen STAI-G Form X 1 und Fragebogen STAI-G Form X 2). Beltz, Weinheim
Lederman RP (1990) Anxiety and stress in pregnancy: significance and nursing assessment. NAACOG’s Clin Issues Perinat Womens Health Nurs 1:279–288
Leigh B, Milgrom J (2008) Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8:24. https://doi.org/10.1186/1471-244X-8-24
Lindgren K (2001) Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health 24:203–217
Little RJ (1988) A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 83(404):1198–1202. https://doi.org/10.1080/01621459.1988.10478722
Matthey S, Barnett B, Kavanagh DJ, Howie P (2001) Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. J Affect Disord 64:175–184
Mercer RT, Ferketich S, May K, DeJoseph J, Sollid D (1988) Further exploration of maternal and paternal fetal attachment. Res Nurs Health 11:83–95
Mikulincer M, Florian V (1999) The association between parental reports of attachment style and family dynamics, and offspring’s reports of adult attachment style. Fam Process 38:243–257
Mikulincer M, Florian V (1999) Maternal–fetal bonding, coping strategies, and mental health during pregnancy—the contribution of attachment style. J Soc Clin Psychol 18:255–276
Misri S, Kendrick K, Oberlander TF, Norris S, Tomfohr L, Zhang H, Grunau RE (2010) Antenatal depression and anxiety affect postpartum parenting stress: a longitudinal, prospective study. Can J Psychiatry 55:222–228
Morse CA, Buist A, Durkin S (2000) First-time parenthood: influences on pre- and postnatal adjustment in fathers and mothers. J Psychosom Obstet Gynaecol 21:109–120
Muller M, Ferketich S (1993) Factor analysis of the Maternal Fetal Attachment Scale. Nurs Res 42:144–147
Muller ME (1992) A critical review of prenatal attachment research. Sch Inq Nurs Pract 6:5–22
Muller ME (1996) Prenatal and postnatal attachment: a modest correlation. J Obstet Gynecol Neonatal Nurs 25:161–166
Nonnenmacher N, Noe D, Ehrenthal JC, Reck C (2016) Postpartum bonding: the impact of maternal depression and adult attachment style. Arch Womens Ment Health 19:927–935. https://doi.org/10.1007/s00737-016-0648-y
O’Connor BP (2000) SPSS and SAS programs for determining the number of components using parallel analysis and velicer’s MAP test. Behav Res Methods Instrum Comput 32:396–402
Reck C, Klier CM, Pabst K, Stehle E, Steffenelli U, Struben K, Backenstrass M (2006) The German version of the postpartum bonding instrument: psychometric properties and association with postpartum depression. Arch Womens Ment Health 9:265–271. https://doi.org/10.1007/s00737-006-0144-x
Reck C, Zietlow AL, Muller M, Dubber S (2016) Perceived parenting stress in the course of postpartum depression: the buffering effect of maternal bonding. Arch Womens Ment Health 19:473–482. https://doi.org/10.1007/s00737-015-0590-4
Rossen L et al (2016) Predictors of postnatal mother–infant bonding: the role of antenatal bonding, maternal substance use and mental health. Arch Womens Ment Health 19:609–622. https://doi.org/10.1007/s00737-016-0602-z
Salmon P, Miller R, Drew NC (1990) Women’s anticipation and experience of childbirth: the independence of fulfillment, unpleasantness and pain. Br J Med Psychol 63(Pt 3):255–259
Schimmenti A (2013) Linking lack of care in childhood to anxiety disorders in emerging adulthood: the role of attachment styles. Child Adolesc Ment Health 20:41–48
Shieh C, Kravitz M, Wang HH (2001) What do we know about maternal–fetal attachment? Kaohsiung J Med Sci 17:448–454
Siddiqui A, Hagglof B (2000) Does maternal prenatal attachment predict postnatal mother–infant interaction? Early Hum Dev 59:13–25
Sjögren B, Edman G, Widström AM, Mathiesen AS, Uvnäs-Moberg K (2004) Maternal foetal attachment and personality during first pregnancy. J Reprod Infant Psychol 22:57–69
Spielberger CD, Gorsuch RL, Lushene RE (1970) The State-Trait Anxiety Inventory (test manual). Consulting Psychologists Press, Palo Alto
Stadlmayr W et al (2006) Memory of childbirth in the second year: the long-term effect of a negative birth experience and its modulation by the perceived intranatal relationship with caregivers. J Psychosom Obstet Gynaecol 27:211–224
Ustunsoz A, Guvenc G, Akyuz A, Oflaz F (2010) Comparison of maternal– and paternal–fetal attachment in Turkish couples. Midwifery 26:e1–e9. https://doi.org/10.1016/j.midw.2009.12.006
van Bussel JC, Spitz B, Demyttenaere K (2010) Reliability and validity of the Dutch version of the maternal antenatal attachment scale. Arch Womens Ment Health 13:267–277. https://doi.org/10.1007/s00737-009-0127-9
Van den Bergh B, Simons A (2009) A review of scales to measure the mother–foetus relationship. J Reprod Infant Psychol 27:114–126
Wallwiener S et al (2016) Predictors of impaired breastfeeding initiation and maintenance in a diverse sample: what is important? Arch Gynecol Obstet 294:455–466. https://doi.org/10.1007/s00404-015-3994-5
Walsh J, Hepper EG, Marshall BJ (2014) Investigating attachment, caregiving, and mental health: a model of maternal–fetal relationships. BMC Pregnancy Childbirth 14:383. https://doi.org/10.1186/s12884-014-0383-1
White MA, Wilson ME, Elander G, Persson B (1999) The Swedish family: transition to parenthood. Scand J Caring Sci 13:171–176
Zachariah R (1994) Maternal–fetal attachment: influence of mother–daughter and husband–wife relationships. Res Nurs Health 17:37–44
Funding
This study was funded by the German Society of Psychosomatics in Gynecology and Obstetrics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Doster, A., Wallwiener, S., Müller, M. et al. Reliability and validity of the German version of the Maternal–Fetal Attachment Scale. Arch Gynecol Obstet 297, 1157–1167 (2018). https://doi.org/10.1007/s00404-018-4676-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4676-x