Abstract
Background
Maternal–fetal attachment has not been formally studied among pregnant Indian women using Cranley’s 24-item maternal–fetal attachment scale.
Objective
The purpose of this study was to validate the Cranley’s 24-item maternal–fetal attachment scale (MFAS-24).
Methods
Consecutive pregnant Indian women of all trimesters were studied in Pondicherry, India.
Statistical Analysis
The mean, standard deviation (SD), Cronbach’s alpha, content validity index (CVI), correlation coefficient, and simple correlation analyses were calculated.
Results
230 pregnant women of various sociodemographic, religious and educational background formed the sample. Mean age of sample was 23 (SD ± 3) years, mean MFAS scores was 87.4 (SD ± 10), mean GHQ scores was 14 (SD ± 1.2), and mean gestational age was 27.2 (SD ± 7) weeks. Cronbach’s reliability alpha of MFAS was high (0.71). There was no correlation between MFAS scores and gestational age or the pregnancy trimester. CVI of the scale, for the Tamil version was 0.72 and for the English version was 0.78.
Conclusions
This study shows applicability of MFAS-24 in Indian settings also for measuring maternal–fetal attachment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Globally, common to all pregnant mothers, irrespective of their cultural or ethnic background, diverse and unique experiences tend to develop during the period of pregnancy between the pregnant mother and her future child. Researchers have quantified these antenatal experiences as “maternal–fetal attachment” (MFA) using John Bowlby and Mary Ainsworth’s attachment theories [1–8]. Similarly, “prenatal attachment” refers to the affective investment that parents develop toward the unborn baby during the gestation period. Cognitively, it may be the imagined scenarios between mother and child, as well as a mother’s attribution of physical and emotional characteristics to the fetus [9].
According to Cranley [5], MFA can be subjectively measured using her maternal–fetal attachment scale (MFAS) that includes 24 items under five behavior domains which are Role taking (e.g., I picture myself feeding the baby; I am eagerly waiting to see how my baby will look like after birth; I picture myself taking care of my baby after birth), Differentiation of self from fetus (I enjoy watching my tummy jiggle as the baby kicks inside; I dream about what my baby thinks and feels from inside my stomach), Interaction with the fetus (I poke the baby to get him/her to poke back, I talk to my unborn baby from outside; I try to grab the feet of my baby seen on my tummy and move it around), Attributing characteristics to fetus (It seems the baby kicks and moves just to remind me that it is my feeding time; If my baby is a boy, I have chosen a name for him already), and Giving of self (I feel that all the trouble of being pregnant is worth it; because I am pregnant, I do things to improve my well-being and of the baby inside, which I will not do if I was not pregnant). MFA has been found to increase with advancing gestational age, particularly after quickening at approximately 18–22 weeks of gestation [10]. The rate and degree of MFA development appears to be influenced by amount of fetal movement, pregnancy history, and the mother’s own attachment history [11, 12].
MFA research began only in the 1970s. The declining mortality rate and technological developments in western nations over the past 30–40 years have changed conceptions about pregnancy and the fetus. Women can detect pregnancy earlier and are able to view high resolution images of their fetus at earlier dates. In a recent integrative review of MFA literature completed by Cannella [13], factors associated with higher levels of MFA included family support, greater psychological well-being, and an ultrasound having been performed. Factors such as depression, substance abuse, and higher anxiety levels were associated with lower levels of MFA. The implications of MFA for maternal and fetal health are now studied in other countries, and across cultures of developed nations, including China, Germany, Sweden, Israel, and Japan [14].
Despite a few researches on MFA worldwide, there has been ambiguity on findings drawn on the concept of MFA especially due to lack of similar evidence reported from other parts of the world in terms of cultural, ethnic, educational, and religious backgrounds.
In this context, India, being a multiethnic, highly culturally diverse country in South Asia offers an ideal location for conducting research on the above concept. Although India has recently risen economically from a global perspective, a great social and economic divide still exists between the rich and poor. Stereotypes and traditions still prevail in most of the Indian societies even today and when it comes to women and pregnancy, many would immediately assume that the concept of attachment between mother and child begins invariably only after delivery and is greatly influenced by many variables such as social, educational, economic, religious, and health, unlike the Western world, where women consider pregnancy an equally important period that initiates and leads into a healthy maternal–child attachment after birth. Environmental- and health-related factors that affect the antenatal phase of pregnancy have been clearly shown to impact the process of normal delivery, and mental and physical health of the mother and the child postnatally.
Unfortunately, MFA has not been studied in developing nations, including India, in which the mortality rate for women and infants remains at or above 40 %. One-third babies born in India are of low birth weight (<2.5 kg) [15, 16], in addition to high infant mortality rates and childhood growth failure among survivors. Low birth weight in India has been attributed to widespread maternal undernutrition. We hypothesize that healthy MFA may serve to allow women to adopt optimal health practices earlier, thereby on a larger scale contribute toward reduction of obstetric maternal and child morbidity.
This absolute lack of research on MFA in India prompted us to conduct the first ever Indian study to validate the 24-item MFAS of Cranley among pregnant Indian mothers to assess the levels of attachment that could exist across different socioeconomic, religious, and cultural background.
Methods
Research Design
A Cross-sectional Observational study (Survey) was considered, and consecutive pregnant Indian women were recruited for the study irrespective of their trimester of pregnancy; attention was paid to include subjects from all sociodemographic, culturally diverse, and ethnic Indian communities. The reading ability of the subjects was also noted to enable uniformity in the procedure of assessment procedure, as the primary measure was a self-report scale.
Setting
The study was done in the Department of Psychiatry & Department of Obstetrics & Gynaecology, Indira Gandhi Government Medical College & Research Institute, Kathirkamam, Puducherry, India.
Ethical Clearance
The study protocol was prepared in keeping with the ethical guidelines of the Indian Council of Medical Research and was presented to an independent ethics committee at Jipmer, Pondicherry.
Sample
230 subjects were included from the following sites for sample collection after obtaining permission:
-
Antenatal Clinic, Department of Obstetrics & Gynaecology, Mahatma Gandhi Medical College & Research Institute, Puducherry, India.
-
Antenatal Clinic, Ashwini Maternity Nursing Home, Puducherry, India.
-
Antenatal Clinic, Department of Obstetrics and Gynaecology, Indira Gandhi Medical College & Research Institute, Puducherry, India.
-
Antenatal Clinic, Primary Health Centre, Mettupalayam, Puducherry, India.
The following criteria were used to recruit the study sample.
Inclusion Criteria
-
1.
Pregnant women of any age group.
-
2.
Women of all ethnic, religion, caste, income, and residential status.
-
3.
Prior written informed consent to participate in the study.
Exclusion Criteria
-
1.
Refusal to give written informed consent.
Measures
Primary Measure
Maternal–Fetal Attachment Scale (MFAS)
MFAS was the first tool developed by Cranley, 1981 to measure MFA in pregnant women. It is a 24-item, Likert type, self-rated scale with five subscales and was developed and tested on 71 pregnant women in the third trimester of pregnancy. The MFAS items each consist of responses from 1 (Definitely No), 2 (No), 3 (Uncertain), 4 (Yes), and 5 (definitely yes). Negative items namely item numbers 9 and 24 will be reverse scored. The total score ranges from 24 to 120. The Tamil version of the scale was used here. Five subscales consisted of (i) Differentiation of self; (ii) Interaction with the fetus; (iii) Attributing characteristics and intentions; (iv) Giving of Self; (v) Role taking.
Procedure
The MFAS was initially translated back-to-back into Tamil language by two other health professionals who were proficient in Tamil and English. The vernacular version obtained was then back-translated to English by two bilingual health professionals. The final version was arrived at based on a consensus decision by all the four translators with due attention being paid to the content, semantic, technical, and conceptual equivalence of the Tamil version.
All participants were interviewed to obtain written informed consent, and for those who were illiterate, the accompanying person signed the consent form after verbal approval by the participant. As there were many participants who were not literate with the ability of reading and signing the informed consent, rating instruments, the Tamil version of MFAS was read to all the participants to ensure commonality of the procedure. The participants were asked to tick the response that they felt most appropriate to them after they fully understood the question.
Waltz and Bausell’s [17] method of estimating content validity index (CVI) was used (8). For the purpose of estimating the CVI of the Tamil translated version of the scale, 10 trained maternal healthcare nurses from the nearest primary healthcare centers were selected, and 10 experienced consultant obstetricians were selected for the English version. Both these groups were asked to rate the MFAS scales, based on the following five criteria, relevance, clarity, simplicity, and ambiguity; each was further rated on a 4-point scale.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) Trial version 18 (SPSS South Asia Pvt Ltd., Bangalore, India), was used for all statistical analysis. Descriptive statistics included calculating mean, standard deviation of MFAS scores. The Cronbach’s alpha was obtained to know the reliability of the scale. CVI was calculated based on the total score obtained on the 5-point validity scale and its likert rating. The correlation coefficient was calculated for both the Tamil and the English version of the MFAS based on the 5-domain criteria. Simple correlation analyses were performed to identify any association between MFAS scores and gestational age or the trimester of pregnancy.
Results
Overall Group Statistics
230 pregnant women in various trimesters of their pregnancy formed the overall sample. The overall mean age in years was 22.9 (SD ± 2.7) and ranged from 18 to 32 years. 180 (78 %) of mothers were of 16–25 years in age and 50 (22 %) were of 26–35 years. 50 % (116) had done primary schooling, 45 (20 %) finished the 10th standard, 40 (17 %) were illiterate, 17 (7 %) finished the 12th standard, and 12 (5 %) had finished graduation. 177 (77 %) mothers were housewife; 49 (21 %) were housewife and doing family job, such as agriculture; and 4 (2 %) were employed before their conception. 115 (50 %) belonged to middle socioeconomic status, 111 (48 %) from low SES, and 4 (2 %) were from upper middle class family. 115 (50 %) were from rural background, 62 (27 %) from urban setting, and 53 (23 %) from semi-urban residential setting. 84 % were Hindu by religion, 12 % were Christians, and 4 % were Muslims.
Obstetric Findings
Mean gestational age of the entire sample was 27.23 (SD ± 7) and ranged from 14 to 38. 121 (52 %) mothers were in the third trimester, and 109 (47 %) were in the second trimester. 174 (76 %) mothers were primigravida, and 28 (12 %) each were second and third gravida. 32 (14 %) mothers were para 1, and 24 (10 %) were para 2. 56 (24 %) mothers had one living child from previous pregnancies. 28 (12 %) mothers had no past obstetric complications. 58 (25 %) had abortions in the past due to various reasons, 10 (4 %) had death of infant due to unknown reasons. 44 (19 %) had 2 abortions and 14 (6 %) had 1 abortion in the past. In terms of obstetric risk, 176 (76 %) mothers had low risk and 54 (23 %) mothers had high risk. 115 subjects from urban and semi-urban background had undergone at least one antenatal sonogram for this pregnancy whereas only 43 % of 115 mothers from rural background had at least one antenatal sonogram.
Reliability
The Cronbach’s alpha scale reliability coefficient was 0.72 for the 24 items of the MFAS, which was well within the reported range by Cranley’s scale in various studies worldwide.
CVI
The CVI ratings obtained for the two different language versions of MFAS showed a rating of 0.72 for the Tamil version and 0.78 for the English version.
MFAS and Correlation Analyses
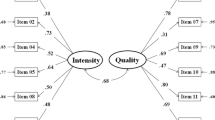
Mean MFAS score was 87.43 (SD ± 10) which is on the lower end of the range of scores (Table 1). Further, there was no statistical association between MFAS and gestational age and trimester of pregnancy (Table 2). The higher MFAS scores were noted around the 28–34 weeks of pregnancy and lower scores noted in early second trimester of pregnancy (Fig. 1).
Discussion
We had chosen the MFA scale for validation, since it was Cranley [18, 19], who had pioneered research in MFA and had also produced the first validated measuring tool for MFA based on the literature review and discussion with experts within antenatal care clinicians and Lamaze teacher’s literature.
The initial version of MFAS consisted of six subscales, with “Nesting” as an additional item. However, after following scrutiny by experts (content validity) and pregnant women (face validity), a 24-item instrument, representing five subscales with a Cronbach’s alpha coefficient of 0.85, demonstrating good internal reliability was established.
Our study had showed a good reliability score of 0.72, which compares well with Cranley’s coefficient of reliability of 0.85. However, CVIs of 0.72 for the Tamil version and 0.78 for the English version were below that of 0.83 as reported by Cranley for the entire scale, leading to doubts on what was initially a criticism of Cranley’s MFAS, which claimed that the information in the scale is based on expert’s interpretation of pregnant women’s emotions and behaviors, but not exactly on the women’s own experiences. The resulting definition underpinning the tool is “the extent to which women engages in behaviours that represent affiliation and interaction with their unborn child.” However, although problems exist in the utilization of the MFAS for research, it has proved to be a catalyst for research and development in the field of maternal/fetal attachment. The five subscales suggest a hierarchy of behaviors, which can be useful in assessing a woman’s attachment behaviors throughout pregnancy. The tool measures a developmental sequence of behaviors, which can be useful in assessing a woman’s progress through pregnancy and patterns of lower scores can alert the researcher to potential attachment problems.
Among various possible reasons for this cross-cultural variation in MFA could be the lack of perception of antenatal maternal–fetal relationship as a form of attachment in Indian settings. Interestingly, rural Indian pregnant women tend to consider the period of pregnancy less precious than the process of delivery. Also living in a socially and economically depraved environment and continuing to do the household, and often the family’s job outside home, throughout the pregnancy leaves little time and scope for these women to cherish antenatal period as a special time for any sort of relationship to develop between the mother and fetus. Another remaining fact is that until the pregnancy results in healthy delivery of the child, women in India are not considered socially competent to behold motherhood. Many such stereotypes and traditional belief systems exist in Indian setting and could explain the low content validity of MFA scale and the limited generalizability of MFA findings from the Western countries.
To conclude, our study proves that cross-cultural research is highly essential to develop a comprehensive understanding of the concept of antenatal MFA.
Implications for Practice
Cranley’s MFAS shows reasonable utility in Indian setting, but additional analyses of various factors that could influence the MFAS scores in any population need to be performed extensively before we can draw further conclusions on the presence or the absence of MFA.
References
Condon JT. The prenatal–foetal relationship—a comparison of male and female expectant parents. J Psychosom Obstet Gynaecol. 1985;4:271–84.
Condon JT, Dunn DJ. The nature and determinants of parent-to-infant attachment in the early postnatal period. J Am Acad Child Adolesc Psychiatry. 1988;27:293–9.
Condon JT. The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol. 1993;66:167–83.
Condon JT, Corkindale CJ. The assessment of parent–infant attachment: development of a self-report questionnaire instrument. J Reprod Infant Psychol. 1997;16:57–76.
Cranley MS. Social support as a factor in the development of parent’s attachment to their unborn. Birth Defects Orig Artic Ser. 1984;20:99–124.
Lester BM, LaGasse LL, Seifer R, et al. The Maternal Lifestyle Study (MLS): effects of prenatal cocaine and/or opiate exposure on auditory brain response at one month. J Pediatr. 2003;142(3):279–85.
Low J. Unstructured interviews and health research. In: Saks M, Allsop J, editors. Researching health: qualitative, quantitative and mixed methods. London: Sage Publications Ltd; 2007.
Salisbury A, Law K, LaGasse L, et al. Maternal–fetal attachment. J Am Med Assoc. 2003;289(13):1701.
Rubin R. Maternal tasks in pregnancy. Matern Child Nurs J. 1975;4:143–53.
Grace JT. Development of maternal–fetal attachment during pregnancy. Nurs Res. 1989;38:228–32.
Lerum CW, LoBiondo-Wood G. The relationship of maternal age, quickening, and physical symptoms of pregnancy to the development of maternal–fetal attachment. Birth. 1989;16:13–7.
LoBiondo-Wood G. The progression of physical symptoms in pregnancy and the development of maternal–fetal attachment. Diss Abstr Int. 1985;46:2625B.
Cannella BL. Maternal–fetal attachment: an integrative review. J Adv Nurs. 2005;50(1):60–8.
Narita S, Maehara S. The development of maternal–fetal attachment during pregnancy. Nihon Kango Kagakkaishi. 1993;13:1–9.
Gopalan C. Low birthweight: significance and implications. In: Sachdev HPS, Chaudhury P, editors. Nutrition in children: developing country concerns. New Delhi, India: Imprint; 1994.
UNICEF. The state of the world’s children. New York: UNICEF; 1998.
Waltz CF, Bausell RB. Nursing research: design, statistics and computer analysis. 2nd ed. Philadelphia: FA Davis Company; 1983.
Cranley MS. Roots of attachment: the relationship of parents with their unborn. Birth Defects Orig Artic Ser. 1981;XVII(6):59–83.
Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res. 1981;30:281–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lingeswaran, A., Bindu, H. Validation of Tamil Version of Cranley’s 24-Item Maternal–Fetal Attachment Scale in Indian Pregnant Women. J Obstet Gynecol India 62, 630–634 (2012). https://doi.org/10.1007/s13224-012-0175-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-012-0175-3