Abstract
Research investigating maternal bonding and parenting stress in the course of postpartum depression is lacking. Aim of the study was to investigate the development and potential mediation of both constructs in the course of postpartum depression. n = 31 mothers with postpartum depression according to DSM-IV and n = 32 healthy controls completed the German version of the Postpartum Bonding Questionnaire and the Parenting Stress Index at two measuring times: acute depression (T1) and remission (T2). At T1, the clinical group reported lower bonding and higher parenting stress. Bonding was found to partially mediate the link between maternal diagnosis and parenting stress. Furthermore, the clinical group reported lower bonding and higher parenting stress averaged over both measurement times. However, at T2, the clinical group still differed from the controls even though they improved in bonding and reported less parenting stress. A significant increase of bonding was also observed in the control group. Maternal bonding seems to buffer the negative impact of postpartum depression on parenting stress. The results emphasize the need for interventions focusing on maternal bonding and mother-infant interaction in order to prevent impairment of the mother-child relationship.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Maternal bonding reflects the first emotional bond a mother gradually develops within the first weeks postpartum toward her infant and is characterized by positive feelings, emotional warmth, affection, and maternal behaviors such as cuddling or smiling at the infant (Klaus et al. 1995). This process, often described as “falling in love with the baby” in literature ensures that the mother puts great efforts into meeting the infant’s needs by taking over the demanding chores of child rearing.
Postpartum psychiatric disorders pose the developing bond between mother and infant at risk and can lead to bonding impairment or bonding disorders. Impaired bonding is characterized by a lack of “maternal feeling”, accompanied by feelings of irritability, hostility, aggressive impulses, or rejection toward the infant (Brockington 2004; Brockington et al. 2001). The detrimental effect of postpartum depression being one of the most frequent psychiatric disorders in the postpartum period with prevalence rates ranging between 6 and 15 % (O’Hara and Swain 1996; Reck et al. 2008) on maternal bonding is well documented. Research has consistently linked postpartum depression to bonding impairment (Brockington et al. 2001; Loh and Vostanis 2004; Moehler et al. 2006; Reck et al. 2006). Between 17 and 31.7 % of postpartum depressed mothers experience an impaired bonding (Brockington et al. 2001; Loh and Vostanis 2004). The severity of depressive symptoms plays a crucial role in this, with more severe depressive symptoms going hand in hand with a more negative perception of maternal bonding (Reck et al. 2006). But even subclinical depressive symptoms negatively affect the developing bond during the first 4 months postpartum (Moehler et al. 2006). One explanation could be, that mothers with postpartum depression often experience feelings of inadequacy, negative cognitions, and self-doubts, that can result in a negative perception of their relationship and bonding to their infant (Brockington 2004; Brockington et al. 2001; Hornstein et al.2006).
Although the link between bonding impairment and acute depressive symptomatology has been demonstrated, little is known about the development of bonding in the course of postpartum depression, especially regarding remission of depressive symptomatology and compared to healthy controls. Studies with samples of inpatients of mother-infant units have shown that at release from psychiatric treatment postpartum depressed mothers perceived their bonding to their infant more positively than at the beginning of hospitalization (Hornstein et al. 2009; Noorlander et al. 2008). However, in none of these studies, inpatients were remitted at release of hospitalization, the authors describe that patients had sufficiently recovered. Therefore, it is yet unclear how maternal bonding develops beyond remission of affective symptoms.
Despite knowledge about the importance of a buffering effect of maternal bonding for successfully mastering the demanding chores of child rearing as it is physically and psychologically exhausting, the link between maternal bonding and parenting stress has not been explored in detail. Parenting stress is defined as the perceived distress or discomfort a mother experiences in the relationship with her infant resulting from the perceived demands associated with the task of providing care and interaction with her infant (Abidin 1995; Deater-Deckard et al. 1998). In this study, we used the Parental Stress Index-Short Form (Abidin 1995), which assesses three aspects of perceived parental stress: maternal distress due to personal factors, how the infant meets maternal expectations, and behavioral characteristics of the infant that makes him either easy or difficult to manage.
A better understanding of possible links between maternal bonding and parenting stress is particularly important in the context of postpartum depression as research suggests that postpartum depressive symptoms are linked not only to maternal bonding but also parenting stress. Higher maternal depressive symptoms have been shown to be associated to higher parenting stress in various studies (Gelfand et al. 1992; Gerdes et al. 2007; Sidor et al. 2011). Cornish et al. (2006) report that briefly and chronically depressed mothers experience more parenting stress than mothers never having had depression. Depressive symptoms affect the perceived parental stress not only in the postpartum period but also during pregnancy. Misri et al. (2010) could show that depression during pregnancy was a significant predictor of parenting stress at 3 to 6 months postpartum. Vice versa, a recent study by Thomason et al. (2014) revealed that parenting stress predicted later depressive symptoms within the first 14 months postpartum.
High parenting stress negatively affects the mother-infant relationship by influencing the mother’s ability to appropriately assess infant signals and to react sensitively to them (Mills-Koonce et al. 2011) resulting in dysfunctional mother-infant interaction (Abidin 1995) which in turn could negatively impact child socio-emotional development (Tharner et al. 2012). Moreover, mothers reporting higher parenting stress perceive their infants as more difficult to care for (Mulsow et al. 2002), report less optimal parenting behaviors and higher rates of child maltreatment and abuse (Holden and Banez 1996).
The emotional bond toward the infant is linked to mother-infant interaction. Results of a study by Mason et al. (2011) suggest that the link between maternal depressive symptoms at 2 months postpartum and maternal report about interaction with the infant at 6 months was mediated by maternal feelings of attachment. Depressed mothers are at risk to be impaired in their emotional bond toward their infant (Brockington et al. 2001; Loh and Vostanis 2004), and research shows that exclusive disorder specific treatment of depression is linked to decreasing parenting stress, but not to a better quality of mother-infant relationship (Forman et al. 2007).
In order to extend existing work that has sought to investigate the link between maternal bonding and parenting stress, the present study jointly examines associations between and the development of both constructs in the course of postpartum depression. It was hypothesized, that at time of acute depression (T1) both, maternal bonding and parenting stress in the clinical group significantly differ from the control group and that the clinical group would perceive significantly lower bonding and higher parenting stress compared to the control group. Furthermore, after remission of depressive symptoms (T2), we expected that mothers of the clinical group would report better bonding and lower parenting stress compared to T1.
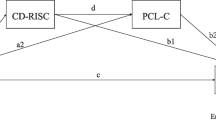
As the links between postpartum depression, maternal bonding, and parenting stress so far have not been explored in detail, we wanted to test two different mediation models: The first one hypothesized that maternal bonding could buffer the effect of postpartum depression on parenting stress and therefore function as a mediator between both constructs. The second one postulated that parenting stress would mediate the relationship between postpartum depression and maternal bonding. This assumption is based on results underlining that postpartum depressed mothers report higher parenting stress (Sidor et al. 2011), and this significantly increases the infant’s risk of being perceived as difficult (Mäntymaa et al. 2006) which in turn could influence the developing bond to the infant. Exploratively, it was tested if found associations out of the main analyses applied longitudinally in our sample.
Methods
Participants
Data was collected during an acute depressive episode (T1) as well as after remission of depressive symptoms (T2). The sample (N = 63) is composed of n = 31 women with postpartum depressive disorders and n = 32 controls without current or previous mental health disorders. The absolute age of the infants could not be kept constant due to the acute phase of the mother’s depressive episode. At T2, the initial sample size was reduced because only n = 26 of women with remitted postpartum depression and n = 24 of controls were available for participation. Subjects were recruited between September 2001 and December 2008 in local maternity hospitals and from a mother-infant unit (for further details see Reck et al. 2011). 95.2 % (n = 60) of the sample (N = 63) were interviewed with the Structured Clinical Interview for DSM-IV (Wittchen et al. 1997) and 4.8 % (n = 3) of the sample, all inpatient depressed mothers, were diagnosed based on a 1-h diagnostic session and the criteria of the ICD-10 (World Health Organization (WHO) 1992). ICD-10 diagnoses of depression are considered to be comparable to the diagnoses of the DSM-IV (Wittchen et al. 1997), especially for the ICD-10 diagnoses depressive episode (F32) and receding depressive episode (F33) and the DSM-IV diagnosis major depression episode, relevant to our study (Mombour W. et al. 1990). 80.6 % (n = 25) of the women in the clinical subsample were recruited from the mother-infant unit of the Psychiatric University Hospital Heidelberg, where they received inpatient treatment, 9.7 % (n = 3) were outpatients and 9.7 % (n = 3) had no treatment and were recruited from local maternity hospitals. Inclusion criterion for the clinical group was a depressive episode according to DSM-IV during the first 3 months postpartum, and women in this group were excluded if they had any acute or history of psychosis or bipolar disorder and current substance abuse/dependence.
The healthy control sample was recruited from local maternity hospitals. All mothers in the control group were diagnosed using the SCID-I. Healthy controls needed to have no current or life time diagnoses in the Structured Clinical Interview for DSM-IV Disorders Axis-I (SCID-I; Wittchen et al. 1997) and should not have received psychotherapy at any time of their life. Infants needed to have a gestational age of no less than 37 weeks and had no congenital abnormalities. Infant’s mean age was 3.9 (T1) and 6.3 (T2) months, respectively. Full demographic statistics are demonstrated in Table 1.
Study design
Overview of procedures
Data was collected during an acute depressive episode (T1) as well as after remission of depressive symptoms (T2). Eligible women from the mother-infant unit were approached by their therapist or the study staff and informed about the present study. Healthy controls were recruited in local maternity hospitals. As described above, women were interviewed and diagnosed either based on a 1-h diagnostic session and the criteria of the ICD-10 (World Health Organization (WHO) 1992) or by carrying out a full version of the SCID-I (Wittchen et al. 1997) by trained and reliable interviewers. In the clinical group, the Beck Depression Inventory (BDI; Beck and Steer 1995) was administered every 2 weeks and T2 took place as soon as the value of the BDI was <11, indicating that women were no longer clinically depressed. Healthy controls were invited to the second measurement time according to infant’s age of the clinical group to ensure comparability between both groups. At both measurement times two questionnaires, the German version of the Postpartum Bonding Questionnaire (PBQ-16; Reck et al. 2006) and the Parenting Stress Index-Short Form (PSI-SF; Abidin 1995) were administered. Sociodemographic data was collected at first assessment. The study protocol had been approved by the independent Ethics Committee of the Medical Faculty of Heidelberg University Hospital. Written informed consent was obtained from every participating woman after the study procedures had been fully explained.
Measures
Assessment of postpartum depression
Postpartum depression was measured either with the German version of the Structured Clinical Interview for DSM-IV Axis I (Wittchen et al. 1997) by trained and reliable SCID-I interviewers or the ICD-10 (World Health Organization (WHO) 1992) during a 1-h diagnostic interview session by an experienced psychiatrist or psychologist who worked in the mother-infant unit. However, the diagnoses of these standard diagnostic instruments are considered to be comparable, especially for ICD-10 diagnoses depressive episode (F32) and receding depressive episode (F33) and the DSM-IV diagnosis major depression episode, relevant to our study (Mombour W. et al. 1990).
Assessment of depressive symptoms
Beck depression inventory
The Beck Depression Inventory (Beck and Steer 1995) is a widely used self-report questionnaire to measure severity of depression consisting of 21 items, each assessing a unique category of depressive symptoms and with total scores ranging from 0 to 63. The BDI has been used in both nonclinical and clinical samples. A higher score indicates a higher severity of depression, BDI-scores <11 indicate normal mood.
Assessment of maternal bonding
Postpartum bonding questionnaire-16
Brockington developed the Postpartum Bonding Questionnaire (Brockington et al. 2001) as a screening tool for impaired bonding. This self-report instrument consists of 25 items to be rated on a scale of 0 (“never”) to 5 (“always”) and is based on four factors. In this study, we used an abridged 16-item version of the PBQ translated in German (Reck et al. 2006) as a principal component analysis did not confirm the original four factor structure but suggested a single factor solution with “bonding impairment.” The PBQ-16 has an internal consistency of Cronbach’s α = 0.85 (Reck et al. 2006). Higher values on the PBQ-16 indicate lower maternal bonding. Items of the PBQ-16 are e.g. “I feel close to my baby.”; “My baby is the most beautiful baby of the world.”; “I wish the old days when I had no baby would come back.”; “I feel distant from my baby.”
Assessment of parenting stress
Parenting stress index-short form (PSI-SF)
Parenting stress was assessed by means of the short form of the Parenting Stress Index (Abidin 1995). The PSI-SF consists of 36 items which are rated on a 5-point Likert scale from SA/1 (“strongly agree”) to SD/5 (“strongly disagree”). The 36 items represent three subscales with 12 items each of the following: “Parental Distress” which measures the level of distress due to personal factors (e.g., “I often have the feeling that I cannot handle things very well.”; “I find myself giving up more of my life to meet my children’s needs than I ever expected.”). “Parent–Child Dysfunctional Interaction” which reflects how the child meets the expectations of the mother (e.g., “When I do things for my child, I get the feeling that my efforts are not appreciated very much.”; “Sometimes my child does things that bother me just to be mean.”; “I expected to have closer and warmer feelings for my child than I do and this bothers me.”). “Difficult Child” which assesses behavioral characteristics of the infant that makes him/her either difficult or easy to manage (e.g., “My child turned out to be more of a problem than I had expected.”; “My child makes more demands on me than most children.”; “My child reacts very strongly when something happens that my child doesn’t like.”). Furthermore, a total stress score can be summed up by adding the scores of the three subscales. In this study, the total stress score was used for the analyses. The reported internal reliability coefficient for the total stress score is 0.91, while those for the subscales range from 0.80 to 0.87 (Abidin 1995).
Data analyses
We used the Statistical Package for Social Sciences (IBM® SPSS® v. 23.0.0.0) and the statistical software “R” v. 3.2.1 (R Development Core Team 2011) in combination with RStudio v. 0.99.467. Power-estimations for the main analyses were computed using G-Power v. 3.1.9.2 (Faul et al. 2007, 2009).
The initial sample sizes were reduced due to incomplete response behavior at T1 (n = 50) and at T2 (n = 35). Thus, before carrying out the main analyses, we ran Little’s MCAR test (Little 1988). The MCAR test evaluates if the missing-completely-at-random-condition (MCAR) is fulfilled. If non-significant, differences between the missing cases due to drop-out or incomplete data and the remaining sample are unlikely. Furthermore, differences related to maternal and infant age, number of children, maternal education, infant sex, and partnership status between controls and their clinical counterparts were explored (via t tests, U tests, and χ 2 tests) to ensure comparability between the groups.
Linear mixed models were used to evaluate the hypotheses. As there were more than 40 error degrees of freedom (df) and the groups were equally sized for the main analyses, the general linear model is assumed to be sufficiently robust against the violation of mathematical assumptions (e.g., normal distribution) (Bortz 2005). The main analysis should evaluate if there were associations between maternal diagnosis, maternal bonding, and parenting stress. Furthermore, it was evaluated, if maternal bonding or parenting stress was mediating the effects of maternal diagnosis on parenting stress and maternal bonding, respectively. Mediation analyses were carried out according to the suggestions of Baron and Kenny (1986). Consequently, four models were created. Since we chose full factorial models in order to test the interaction terms and thus potential moderation effects as well, in sum, eight beta weights were tested for significance. The critical α-errors of the main analyses (global α-error was α = 0.05) were Bonferroni-adjusted yielding a critical α-error of α = 0.00625 for each beta weight test. Empirical p values were two-tailed.
The additional analyses were carried out without correction for multiple testing and thus serve in an explorative hypotheses-generating manner. The Parenting Stress Index (SF) consists of three subscales which can be summed up to a total stress score. In our analyses, we used the total stress score. Using Pearson correlations, we tested for associations of the subscales with maternal bonding. This should guarantee that the found associations were not only due to a single PSI subscale which contains items that potentially overlap with items of the PBQ. Furthermore, these analyses should guarantee that all scales were associated to maternal bonding in the same direction. Furthermore, it was tested if the found associations of the main analyses applied longitudinally in our sample. Additionally, the within-effect of and interaction terms with measurement time were evaluated.
For the linear mixed models, parametric variables were z-standardized to receive standardized β-weights in regressions where parametric variables were independent and dependent parameters. Nominal variables were dummy-coded. For group and measurement time comparisons, effect sizes are reported as partial η 2, which is a sample-based estimator of explained variance. According to Cohen (1988), η 2 = 0.01 are small, η 2 = 0.06 are medium-sized, and η 2 = 0.14 are large effects. Model fit was quantified by the −2 log likelihood χ 2.
Results
Preliminary data analyses
For the MCAR test, we considered the following variables: maternal and infant age, number of children, maternal education, infant sex, partnership status, group (clinical vs. control), maternal bonding, parenting stress, and parameters that were not used for the analyses and therefore were not described here, but might explain missing values. The test was non-significant (χ 2 = 378.86, df = 1178, p > 0.99); the case-exclusions (due to drop-outs and missing data) were valid for our sample and the subpopulation at T2 is representative for the larger sample. In order to ensure comparability between the clinical and the control group, we compared the distribution of demographic variables at T1 using t, U, and χ 2 tests. As demonstrated in Table 1, no differences were found between the groups.
Main analyses
Maternal bonding and parenting stress during acute depression
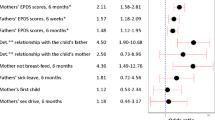
At T1, group was a significant predictor for parenting stress (β = 1.58, SE = 0.17, lower 95 % CI bound = 1.24, upper 95 % CI bound = 1.92, t = 9.33, p < 0.001, −2 log likelihood = 90.45), as well as for maternal bonding (β = 1.21, SE = 0.21, lower 95 % CI bound = 0.79, upper 95 % CI bound = 1.63, t = 5.72, p < 0.001, −2 log likelihood = 129.39). Women with acute depression experienced more parenting stress (M = 88.78, SE = 2.83) and a lower bonding quality (M = 18.56, SE = 1.70) than controls (parenting stress: M = 53.58, SE = 2.61; maternal bonding: M = 5.14, SE = 1.67). For parenting stress (η 2 = 0.64) and maternal bonding (η 2 = 0.37), the effect was large.
Next, full factorial models were created to determine if, and how these effects were mediated. One model regressed onto parenting stress (model 1) with maternal bonding as potential mediator and one model regressed onto maternal bonding with parenting stress as potential mediator (model 2). As can be taken out of Table 2, model 1 has a lower −2 log likelihood estimate and thus better explains our data. Additionally, the p values of parenting stress (p = 0.0065) exceeded the Bonferroni-adjusted critical α-error (α = 0.00625). Consequently, though just slightly more adequate than Model 2, we further focused model 1 only.
In model 1, both group and maternal bonding were significant predictors of parenting stress. The interaction between group and bonding was not significant (Table 2). The model significantly improved by considering maternal bonding as additional predictor as revealed by χ 2 test for the model comparison (Δ−2 log likelihood χ 2 = 39.04, Δdf = 2, p < 0.001). In order to test, if the effect of “group” on parenting stress (β = 1.583) significantly decreased by considering maternal bonding (β = 0.772), the procedure of Cumming (2009) was applied. Thus, beta weights can be considered as statistically different from each other (p < 0.05) if their confidence intervals overlap less than 50 %. Half of the average of the overlapping confidence intervals was calculated (0.176) and added to the group beta weight lower bound estimate out of the plain model (where only group is a predictor for parenting stress; 1.242), which yielded 1.418. As this value exceeded the value of the group upper bound value out of the more complex model (with maternal bonding as predictor; 1.133), the difference between the both beta weights (Δβ = 0.816) was considered statistically significant from zero. Additionally the Sobel test (Sobel 1982) indicated a significant mediation effect of maternal bonding between group and parenting stress (z = 2.73, p = 0.006). Thus, maternal bonding is considered a partial mediator between group and parenting stress, given the fact that group remained a significant predictor in the model.
The power to discover large effects (f 2 = 0.35) in the full factorial model for our analyses reached 1-β = 0.94. Medium-sized effects (f 2 = 0.15) could be revealed with a power of 56 %. Small effects (f 2 = 0.02) can definitely not be ruled out, as the β-error was 94 %.
Additional analyses
Correlations of maternal bonding (PBQ-16) with parenting stress (PSI-SF) sum score and subscales
As demonstrated in Table 3, at both assessments, the sum scale showed the highest correlations with maternal bonding at T1 followed by the subscales “difficult child,” “dysfunctional interaction,” and “parental distress”. At T2, the sum scale was followed by “parental distress,” “dysfunctional interaction,” and “difficult child”. All associations exceeded an association strength of r > 0.69. The correlation coefficients were tested on significant differences between each other at the respective measurement point with z tests (Eid et al. 2011). For T1, it was revealed that the total score was significantly higher associated to maternal bonding than the subscales “parental distress” (z = 3.79, p < 0.01) and “dysfunctional interaction” (z = 2.07, p = 0.02). For T2, it was revealed that the total score was significantly higher associated to maternal bonding than the subscale “difficult child” (z = 2.454, p = 0.01). No other comparisons of correlation coefficients with the total score and among the subscales were significant (│z│ < 1.51, p > 0.07).
Development of maternal bonding and parenting stress in the course of postpartum depression
As the variances of parenting stress (T1 483.98, T2 341.01) and maternal bonding (T1 107.34, T2 40.18) differed but were highly correlated between the measurement times (parenting stress: r = 0.91, p < 0.001; maternal bonding: r = 0.78, p < 0.001), we assumed a diagonal covariance structure for the repeated measure analyses with linear mixed models. For these analyses, the single repeated measures (level 1) were nested in the subjects (level 2) and an additional dummy-coded variable “time” was created.
Table 4 shows the regressions onto parenting stress (model 3) and maternal bonding (model 4) with group, time, and their interaction term as predictors. For model 3, only group was a significant predictor. Depressive women generally experienced more parenting stress averaged over both measurement times (M = 82.56, SE = 3.08) in comparison to controls (M = 51.26, SE = 3.08, η 2 = 0.65). In model 4, it was revealed that depressed mothers generally experienced a lower bonding averaged over both measurement points (M = 14.05, SE = 1.54) in comparison to controls (M = 4.55, SE = 1.54, η 2 = 0.37). Additionally, the “group × time” interaction term was revealed significant (η 2 = 0.20): Besides, the group difference at T1 (reported in the main analyses) post hoc t tests revealed that at T2, groups significantly differed (clinical group: M = 10.31, SE = 1.33; control group: M = 3.77, SE = 1.33; t = 3.48, p = 0.001, η 2 = 0.28). Additionally, patients significantly improved their bonding (t = 3.75, p = 0.002, η 2 = 0.47) from T1 (M = 17.79, SE = 2.65) to T2 (M = 10.31, SE = 1.71) as did controls (T1: M = 5.33, SE = 1.07; T2: M = 3.77, SE = 0.79; t = 2.40, p = 0.03, η 2 = 0.26), however, to a smaller degree. Thus, patients generally experienced lower bonding during acute depression as well as after remission. However, their bonding improves more from T1 to T2 than in controls.
Next, in line with the findings of the main analyses, we explored if maternal bonding mediated the relationship between group and parenting stress in a full factorial model (model 5, Table 5). Effects of time and their interaction terms were additionally evaluated. A comparison between model 5 and model 3 revealed that the model improved by considering maternal bonding as additional predictor in the full factorial model (Δ−2 log likelihood χ 2 = 70.10, Δdf = 4, p < 0.001). In model 6, a random intercept and a random slope for maternal bonding on the individual level (level 2) were assumed (maximum likelihood estimation, variance component covariance structure). A comparison between model 5 and model 6 revealed no statistical significant decrease in the −2 log likelihood χ 2 by the random effects (Δ−2 log likelihood χ 2 = 3.99, Δdf = 2, p = 0.14). Thus, only the less complex model (model 5) was further investigated.
As demonstrated in Table 5, model 5, only group and maternal bonding had significant effects on parenting stress. Neither time nor interaction terms were significant. The procedure of Cumming (2009) was repeated, to evaluate if the effects of group on parenting stress (model 3, β = 1.130) significantly decreased by considering maternal bonding as mediator (model 5, β = 0.542). Half of the average of the overlapping confidence intervals was calculated (0.216) and added to the group beta weight lower bound estimate out of model 3 (without PBQ as mediator; 0.684), which yielded 0.900. As the group upper bound value out of model 5 (with maternal bonding as predictor; 0.960) slightly exceeded this value, the difference between the both beta weights (Δβ = 0.588) was not considered statistically significant from zero (p > 0.05). However, the Sobel test (Sobel 1982) indicated a significant mediation effect of maternal bonding between group and parenting stress (z = 2.44, p = 0.01).
Discussion
The aim of this study was to investigate the link between and the course of maternal bonding and parenting stress during postpartum depression and after remission compared to healthy controls. During acute depressive episode, mothers in the clinical group reported significantly lower bonding and higher parenting stress compared to healthy controls. This is in line with literature reporting a significant link between postpartum depression and maternal bonding (Loh and Vostanis 2004; Moehler et al. 2006; Reck et al. 2006) as well as perceived parenting stress (Gerdes et al. 2007; Sidor et al. 2011).
Regarding links between maternal diagnosis at T1, maternal bonding and parenting stress full factorial models suggested that maternal bonding partially mediates the link between maternal diagnosis and parenting stress as this model fits best with the data. This result indicates that maternal diagnosis as well as maternal bonding are independent predictors of parenting stress but a higher bonding can partially buffer the effect of maternal diagnosis on parenting stress. A diagnosis of postpartum depression and a lower bonding seem to be a cumulative risk to experience high parenting stress.
Studies suggest that mothers reporting high parenting stress show less optimal parenting behaviors (Mulsow et al. 2002) which not only affects mother-infant relationship but also child development (Tharner et al. 2012) due to dysfunctional interaction patterns which are linked to developmental problems (Murray and Cooper 1997a, b). Research consistently reports that depressed mothers interact less sensitive with their infants and show less positive, more intrusive behaviors or withdrawal (Field 2010; Field et al. 2006; Tronick and Reck 2009). In a recent study submitted for publication by our research group, we found significant links between maternal bonding and positive interaction behaviors, indicating that the emotional bond toward the infant is also expressed on behavioral level. Furthermore, lower maternal bonding was linked to higher rates of infant self-comforting behaviors which in turn correlated with higher infant salivary cortisol reactivity (Müller et al. 2015). Therefore, infant self-comforting behavior might be seen as an indicator for infant stress and an expression of insufficient dyadic regulation due to impairment of maternal sensitivity and positive affect. Interacting with an unregulated infant put the mother under stress and can affect the developing bond. Vice versa, as our results suggest, if mothers reported to be well bonded to their infant, the vicious circle of perceived parenting stress and dysfunctional interaction patterns might be broken and transformed into a circle of mutual positive reinforcement. Therefore, interventions focusing on maternal bonding as well as maternal sensitivity are clearly needed. In a video-feedback intervention to enhance parent-infant relationship with parents of pre-term infants, bonding increased over the course (Hoffenkamp et al. 2015) showing that such interventions are useful and effective.
Regarding the development of bonding and parenting stress in the course of postpartum depression, postpartum depressed mothers experienced significantly more parenting stress and lower bonding averaged over both measurement times compared to healthy controls. Interestingly, after remission of the depressive symptomatology, mothers in the clinical group still differed significantly from the control group regarding maternal bonding even though they had improved significantly in the emotional bond to their child. This result could be a hint that postpartum depression has potential long-term effects on mother-infant relationship even beyond acute depressive episode. Therefore, mothers remitted from postpartum depression should be supported over a considerable period of time to prevent potential impairment of mother-infant relationship and child development. This result is in line with results of Reck et al. (2012) indicating that mothers who had life time diagnoses of depression but were not affected by depression at time of assessment reported impaired maternal self-efficacy.
Regarding parenting stress, which was assessed with the PSI, the sum scale had the strongest association to maternal bonding (PBQ) on a descriptive as well as on an inferential level in comparison to the PSI subscales throughout both assessment times. Consequently, the found associations between maternal bonding and parenting stress were not due to a single PSI subscale. It should be mentioned that some items of the PSI may reflect certain aspects of maternal bonding but not in its entity.
Another central concept in mother-infant research is maternal attachment. Mothers with postpartum depression are often insecurely attached (McMahon et al. 2008) which goes along with lower maternal sensitivity and lower quality of mother-child relationship. Wilkinson and Mulcahy (2010) could show that independent of a postpartum depression insecurely attached mothers reported lower bonding to their infants. Therefore, maternal attachment representations should be taken into account in future studies.
A significant increase in maternal bonding was observed in the control group indicating that maternal bonding gradually develops over the first months. This is in line with results of a study by Moehler et al. (2006) reporting that maternal bonding increased over the first months postpartum with a moderate stability after 4 months.
In sum, the present findings shed light on the link between maternal bonding and perceived parenting stress in the course of postpartum depression. Our finding that maternal bonding partially mediates the relationship between maternal diagnosis and perceived parenting stress is indicative for the development of interventions focusing on mother-infant interaction and maternal bonding problems in order to reduce parental stress and to prevent developmental problems in infants. A promising technique could be video-feedback interventions in which mother-infant interaction is recorded and then micro-analyzed with respect to certain positive affective and behavioral components. Especially, mothers with postpartum depression and low bonding could benefit from such interventions with the aim to (re-)discover intuitive parenting behaviors (Papoušek and Papoušek 1995) and enhance positive interactive feedback leading to mutual positive reinforcement between mother and infant. This might prevent regulatory problems in infancy and childhood.
Limitations
Firstly, besides a rather small sample size, a great variation of infant age due to the mother’s state of acute depression characterizes our sample. Secondly, women in our study over proportionally held academic degrees. This surely is not representative for the overall population. Thirdly, the PBQ-16 is a self-report questionnaire. A standardized interview assessing maternal attitude and behavior with respect to maternal bonding in German language is still missing. It should also be noted that other variables apart from maternal bonding could have an effect on parenting stress, e.g., maternal attachment representations (Main et al. 1985; Main 2000) which influence early mother-infant interaction and parenting behaviors (Riva Crugnola et al. 2013). For future studies, these parameters should also be taken into account.
Finally, as our study is the first one evaluating links between maternal bonding and parenting stress in the course of postpartum depression, further support for this finding in larger samples with longitudinal study designs is needed.
References
Abidin RR (1995) Parenting stress index, 3rd edn. Psychological Assessment Resources, Odessa FL
Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182
Beck AT, Steer RA (1995) Beck-Depressions-Inventar: BDI (2., überarb. Aufl. ed.). Huber, Bern; Göttingen
Bortz J (2005) Statistik für Human- und Sozialwissenschaftler: mit … 242 Tabellen (6., vollst. überarb. und aktualisierte Aufl. ed.). Springer, Heidelberg
Brockington I (2004) Postpartum psychiatric disorders. Lancet 363(9405):303–310
Brockington I, Oates J, George S, Turner D, Vostanis P, Sullivan M, Murdoch C (2001) A screening questionnaire for mother-infant bonding disorders. Arch Womens Ment Health 3(4):133–140
Cohen J (1988) Statistical power analysis for the behavioral sciences (2. ed. ed.). Erlbaum, Hillsdale, NJ
Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kowalenko N, Tennant C (2006) Maternal depression and the experience of parenting in the second postnatal year. J Reprod Infant Psychol 24(2):121–132
Cumming G (2009) Inference by eye: reading the overlap of independent confidence intervals. Stat Med 28(2):205–220
Deater-Deckard K, Pickering K, Dunn JF, Golding J (1998) Family structure and depressive symptoms in men preceding and following the birth of a child. The Avon Longitudinal Study of Pregnancy and Childhood Study Team. Am J Psychiatr 155(6):818–823
Eid M, Gollwitzer M, Schmitt M (2011) Statistik und Forschungsmethoden Lehrbuch. Beltz, Weinheim
Faul F, Erdfelder E, Lang A, Buchner A (2007) GPower 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Faul F, Erdfelder E, Buchner A, Lang A (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Field T (2010) Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev 33(1):1–6
Field T, Hernandez-Reif M, Diego M (2006) Intrusive and withdrawn depressed mothers and their infants. Dev Rev 26(1):15–30
Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC (2007) Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Dev Psychopathol 19(2):585–602. doi:10.1017/S0954579407070289
Gelfand DM, Teti DM, Fox CR (1992) Sources of parenting stress for depressed and nondepressed mothers of infants. J Clin Child Psychol 21(3):262–272
Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, Jensen PS (2007) Maternal depressive symptomatology and parenting behavior: exploration of possible mediators. J Abnorm Child Psychol 35(5):705–714. doi:10.1007/s10802-007-9134-3
Hoffenkamp HN, Tooten A, Hall RAS, Braeken J, Eliëns MPJ, Vingerhoets AJJM, Van Bakel HJA (2015) Effectiveness of hospital-based video interaction guidance on parental interactive behavior, bonding, and stress after preterm birth: a randomized controlled trial. J Consult Clin Psychol 83(2):416–429. doi:10.1037/a0038401
Holden EW, Banez GA (1996) Child abuse potential and parenting stress within maltreating families. J Fam Violence 11(1):1–12
Hornstein C, Schenk S, Wortmann-Fleischer S, Downing G, Schwarz M (2006) Videotherapie bei postpartalen Störungen. Ein interaktionales Behandlungskonzept bei Müttern mit Depressionen und Psychosen. Psychotherapeut 51(5):363–368. doi:10.1007/s00278-006-0484-z
Hornstein C, Hohm E, Trautmann-Villalba P (2009) (1995). Bonding: building the foundations of secure attachment and independence. In: Bonding: building the foundations of secure attachment and independence. Addison-Wesley, Massachussetts
Klaus MH, Kennel JH, Klaus P (1995) Symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Arch Womens Ment Health 9(5):273–278. doi:10.1007/s00737-006-0149-5
Little R (1988) A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc 83:1198–1202
Loh C-C, Vostanis P (2004) Perceived mother-infant relationship difficulties in postnatal depression. Infant Child Dev 13(2):159–171. doi:10.1002/icd.347
Main M (2000) The organized categories of infant, child and adult attachment: flexible vs. inflexible attention under attachment-related stress. J Am Psychoanal Assoc 48:1055–1095
Main M, Kaplan N, Cassidy J (1985) Security in infancy, childhood, and adulthood: a move to the level of representation. Monogr Soc Res Child Dev 50:66–104
Mäntymaa M, Puura K, Luoma I, Salmelin RK, Tamminen T (2006) Mother’s early perception of her infant’s difficult temperament, parenting stress and early mother-infant interaction. Nord J Psychiatry 60(5):379–386. doi:10.1080/08039480600937280
Mason ZS, Briggs RD, Silver EJ (2011) Maternal attachment feelings mediate between maternal reports of depression, infant social–emotional development, and parenting stress. J Reprod Infant Psychol 29(4):382–394. doi:10.1080/02646838.2011.629994
McMahon C, Trapolini T, Barnett B (2008) Maternal state of mind regarding attachment predicts persistence of postnatal depression in the preschool years. J Affect Disord 107(1–3):199–203
Mills-Koonce WR, Appleyard K, Barnett M, Deng M, Putallaz M, Cox M (2011) Adult attachment style and stress as risk factors for early maternal sensitivity and negativity. Infant Ment Health J 32(3):277–285. doi:10.1002/imhj.20296
Misri S, Kendrick K, Oberlander TF, Norris S, Tomfohr L, Zhang H, Grunau RE (2010) Antenatal depression and anxiety affect postpartum parenting stress: a longitudinal, prospective study. Can J Psychiatry 55(4):222–228
Moehler E, Brunner R, Wiebel A, Reck C, Resch F (2006) Maternal depressive Die postpartale Bindungsstörung: Eine Risikokonstellation für den Infantizid? Forensische Psychiatrie Psychologie Kriminologie 1:1–8. doi:10.1007/s11757-008-0111-7
Mombour W, Spitzner S, Reger KH, Von Cranach M, Dilling H, Helmchen H (1990) Summary of the qualitative criticisms made during the ICD-10 field trial and remarks on the German translation of ICD-10. Pharmacopsychiatry 23:197–201
Müller M, Zietlow A, Tronick E, Reck C (2015) What dyadic reparation Is meant to do: an association with infant cortisol reactivity. Psychopathology. doi:10.1159/000439225
Mulsow M, Caldera YM, Pursley M, Reifman A, Huston AC (2002) Multilevel factors influencing maternal stress during the first three years. J Marriage Fam 64(4):944–956. doi:10.1111/j.1741-3737.2002.00944.x
Murray L, Cooper P (1997a) Effects of postnatal depression on infant development. Arch Dis Child 77(2):99–101
Murray L, Cooper P (1997b) Postpartum depression and child development. Psycholigal Med 27(2):253–260
Noorlander Y, Bergink V, van den Berg MP (2008) Perceived and observed mother-child interaction at time of hospitalization and release in postpartum depression and psychosis. Arch Womens Ment Health 11(1):49–56
O’Hara MW, Swain AM (1996) Rates and risk of postpartum depression-a meta-analysis. Int Rev Psychiatry 8(1):37–54. doi:10.3109/09540269609037816
Papoušek H, Papoušek M (1995) Intuitive parenting. In: Bornstein MH (ed) Handbook of parenting, vol 2, Biology and ecology of parenting. Lawrence Erlbaum Associates, Inc., Hillsdale, NJ, England, pp 117–136
R Development Core Team (2011) R: a language and environment for statistical computing. the R Foundation for Statistical Computing, Vienna, Austria. Available online at http://www.R-project.org/
Reck C, Klier CM, Pabst K, Stehle E, Steffenelli U, Struben K, Backenstrass M (2006) The German version of the postpartum bonding instrument: psychometric properties and association with postpartum depression. Arch Womens Ment Health 9(5):265–271. doi:10.1007/s00737-006-0144-x
Reck C, Struben K, Backenstrass M, Stefenelli U, Reinig K, Fuchs T, Mundt C (2008) Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatr Scand 118:459–468. doi:10.1111/j.1600-0447.2008.01264.x
Reck C, Noe D, Stefenelli U, Fuchs T, Cenciotti F, Stehle E, Tronick EZ (2011) Interactive coordination of currently depressed inpatient mothers and their infants during the postpartum period. Infant Ment Health J 32(5):542–562. doi:10.1002/imhj.20312
Reck C, Noe D, Gerstenlauer J, Stehle E (2012) Effects of postpartum anxiety disorders and depression on maternal self-confidence. Infant Behav Dev 35(2):264–272. doi:10.1016/j.infbeh.2011.12.005
Riva Crugnola C, Gazzotti S, Spinelli M, Ierardi E, Caprin C, Albizzati A (2013) Maternal attachment influences mother-infant styles of regulation and play with objects at nine months. Attach Hum Dev 15(2):107–131
Sidor, Anna, Kunz, Elisabeth, Schweyer, Daniel, Eickhorst, Andreas, & Cierpka, Manfred. (2011). Links between maternal postpartum depressive symptoms, maternal distress, infant gender and sensitivity in a high-risk population. Child and Adolescent Psychiatry and Mental Health, 5. doi: 10.1186/1753-2000-5-7
Sobel ME (1982) Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S (ed) Sociological methodology. Jossey-Bass, San Francisco, pp 290–312
Tharner A, Luijk MPCM, Van I, Marinus H, Bakermans K, Marian J, Jaddoe VWV, Hofman A, Tiemeier H (2012) Infant attachment, parenting stress, and child emotional and behavioral problems at age 3 years. Parenting Science Practice 12(4):261–281. doi:10.1080/15295192.2012.709150
Thomason E, Volling BL, Flynn HA, McDonough SC, Marcus SM, Lopez JF, Vazquez DM (2014) Parenting stress and depressive symptoms in postpartum mothers: bidirectional or unidirectional effects? Infant Behav Dev 37(3):406–415
Tronick EZ, Reck C (2009) Infants of depressed mothers. Harv Rev Psychiatry 17(2):147–156. doi:10.1080/10673220902899714
Wilkinson RB, Mulcahy R (2010) Attachment and interpersonal relationships in postnatal depression. J Reprod Infant Psychol 28(3):252–265
Wittchen H-U, Wunderlich U, Gruschwitz S, Zaudig M (1997) SKID-I: Strukturiertes Klinisches Interview für DSM-IV. Achse I: Psychische Störungen. Hogrefe, Göttingen
World Health Organization (WHO) (1992) The ICD-10 classification of mental and behavioural disorders, 10th edn. World Health Organization, Geneva
Acknowledgments
We would like to thank the mothers and children participating in the study. Furthermore, we would like to express our thanks to the maternity clinics and their staff for their willingness to cooperate and their support in recruiting patients. The study was supported by a grant from the Program of Research Support of the Medical Faculty (funding period: 2003–2004), Dietmar Hopp as well as by Köhler and Jung foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reck, C., Zietlow, AL., Müller, M. et al. Perceived parenting stress in the course of postpartum depression: the buffering effect of maternal bonding. Arch Womens Ment Health 19, 473–482 (2016). https://doi.org/10.1007/s00737-015-0590-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-015-0590-4