Abstract
Introduction
In athletes, acromioclavicular joint disruptions account for up to 50% of all shoulder injuries. In high-grade injuries, surgery is favored to ensure a correct restoration of the joint, especially in young athletes. The aim of this study was to compare the clinical, radiological and sport related outcomes of the arthroscopic stabilization with the fixation of the AC joint in a mini-open approach.
Materials and methods
19 patients treated arthroscopically (ASK) and 26 patients with an acute AC-joint dislocation Rockwood V who had undergone the mini-open (MO) surgery were included. Constant Murley Score (CMS), Taft Score (TS) and the Simple Shoulder Tests (SST) were evaluated. The sports activity level was determined according to Valderrabano and the athlete’s recovery of their athletic activity level after surgery according to Rhee. Furthermore, all available X-ray images were analyzed.
Results
Patients in the ASK group achieved an average score of 11.7 ± 0.6 points in the SST, 10.3 ± 1.8 points in the TS and 91.2 ± 11.8 points in the CMS. On average, patients in the MO group achieved results of 10.5 ± 1.4 points in the SST, 11.7 ± 0.7 points in the TS and 91.6 ± 9.8 points in the CMS. The ASK group showed significant difference regarding the CC distance in side comparison (Δ = 3.6 mm), whereas no significant difference was found in the MO group (Δ = 0.8 mm). In comparison of both groups, the posterior as well as the combined translation were significantly greater in the ASK group than in the MO group (posterior: ASK: 24.8 mm, MO: 19.3 mm, combined: ASK: 29.1 mm, MO: 20.9 mm). Residual horizontal instability was greater in the ASK group (43%) than in the MO group (32%). Similar results were achieved in sports activity and the recovery of athletic activity (Valderrabano: ASK: 2.8, MO: 2.6; Rhee: ASK: 1.6, MO: 1.5).
Conclusions
Both techniques prove to be effective for the stabilization of high-grade AC-joint disruptions in athletes and showed excellent clinical results. From a radiographic standpoint, the mini-open procedure appears superior to the arthroscopic technique. After mini-open surgery postoperative loss of correction is less common and greater horizontal stability is achieved. The results also suggest the mini-open technique is superior to the arthroscopic procedure when aiming to restore the athlete’s original level of sports activity.
Level of evidence
1.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Injuries of the acromioclavicular joint are considered common injuries, accounting for 12% of all injuries of the shoulder girdle [1]. Furthermore, 50% of athletic injuries to the shoulder region are attributed to injuries of the acromioclavicular (AC) joint. Injuries of the AC joint are approximately 5–10 times more common in males than in females [1, 2]. Depending on the force applied to the AC joint, the extent of the injury can vary from a sprain of the AC joint’s capsule to a complete rupture of all coracoclavicular ligaments as well as a detachment of the delta-trapezial fascia. As a result of such an injury, one to three dimensional instabilities of the AC joint can occur. Cadaver studies have shown that forces as of 500–700 N result in traumatic injury of the AC joint [3, 4]. In a biomechanical study conducted by Mazzocca et al., findings show that the correct reconstruction of the AC joint demonstrates an important factor when ensuring both horizontal and vertical stability of the AC joint under stress [5]. Therefore, surgical treatment of AC-joint injuries, especially in young athletes, is the therapy of choice. Though a variety of surgical procedures exist, a gold standard has not yet been established. Findings of the studies conducted to analyze the various surgical techniques show comparable clinical as well as radiological results in the medium term [2, 6,7,8,9,10,11,12,13,14,15,16]. Significant advances have been made to optimize minimally invasive surgery in recent years. For example, by applying a twin-tailed double TightRope © implant, the failure rate of the previously applied single TightRope © implant was significantly improved. Furthermore, this approach provides the possibility of an exact reconstruction of the AC joint with good vertical stability [16,17,18,19,20,21]. Surgical attempts described by Berthold et al. in 2019, comprising of a combination of both the CC reconstruction and transarticular cerclage, promise an additional increase in horizontal stability [22]. Alternatively, improved horizontal stability is also achieved by the reconstruction of both the delta-trapezial-fascia and the dorsal AC-joint capsule, which in contrast to the arthroscopic technique, is made possible by application of the TwinTail © implant in a mini-open surgical procedure.
The aim of this study was to compare the clinical and radiological outcomes of the arthroscopic Double AC TightRope © stabilization with the Twin Tail TightRope fixation, using a mini-open surgical approach, as methods of surgical treatment of coracoclavicular instability in athletes. While conducting this study, the athlete’s ability of being able to return to their previous athletic activity and the possible differences regarding dynamic translation, were especially taken into consideration. It was expected that the mini-open Twin Tail TightRope © reconstruction would provide at least equivalent functional results in comparison to the frequently investigated arthroscopic technique and that it would be superior to the arthroscopic technique in terms of dynamic posterior translation. Both surgical techniques were expected to prove successful in regard to the patient’s recovery of their athletic ability.
Materials and methods
Patients included in the study were athletes who had received surgical treatment due to an acute injury of the acromioclavicular joint throughout the previous 2 years at the Sportklinik in Stuttgart, Germany. The patients were divided into two groups, depending on the applied operative procedure and according to the inclusion and exclusion criteria. Additionally, a retrospective examination of the patient was conducted postoperatively. All patients bearing German citizenship and of the ages 18–60 who had received surgical treatment due to the dislocation of the AC joint, classified as a Rockwood type V injury, were included. Exclusion criteria for the participation in this study were chronic dislocations of the AC joint, severe cardiac or kidney disease, and pregnancy. Additionally, patients who had received previous surgical treatment in another healthcare institution were excluded from the study.
The postoperative follow-up examination (ASK 19.3 ± 2.1 months, MO 20.4 ± 1.9 months) contained a standard clinical assessment of both shoulders as well as the evaluation of the Taft Score (TS), the Simple Shoulder Test (SST) and the Constant Murley Score (CMS). Muscle strength was determined by using standardized isometric dynamometry (Isobex TM Dynamometer, Medical Device Solutions AG, Burgdorf, Switzerland) in 90° abduction and 30° anteversion of the shoulder and pronation of the hand. The sports activity level was determined according to Valderrabano (Table 1) and the athlete’s recovery of their athletic activity before surgery according to Rhee (Table 2).
Postoperative radiological imaging, carried out at the same time as the follow-up examination, included projections of both shoulders in the Alexander view and weighted panoramic view (5 kg), the non-operative shoulder serving as a reference. The coracoclavicular distance as well as the width of the acromioclavicular joint were measured in the panoramic view (Fig. 1). Dynamic stability (dt), posterior and superior translation, as well as the combined posterior–superior translation, were determined by measurement in the Alexander view projection (Figs. 2 and 3). Furthermore, radiological findings such as signs of osteoarthritis, subluxations and dislocations of the AC joint were gathered from the radiograph. The measurements were carried out by the senior author.
Surgical techniques
Arthroscopic double TightRope technique
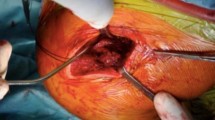
The patient is positioned in the beach chair position and the operative arm is placed onto an armrest (Fig. 4a, b). After completing the diagnostic arthroscopy through a dorsal portal, an additional anterior and anterior–superior portal are created. The coracoid is then located (from the inferior perspective) using electrical ablation. Afterward, approximately 4 cm medial to the AC joint, an incision, 2 cm long is made above the clavicle. Under fluoroscopic guidance, a drill guide pin is positioned above the acromion and coracoid before a 4 mm-cannulated drill is advanced over the pin through the clavicle and coracoid process. The TightRope is then positioned using a suture shuttle system and the button of the TightRope is flipped under fluoroscopic guidance below the coracoid process. A second implant is then secured lateral to the first in the same technique. The implants are positioned along the anatomical alignment of the coracoclavicular ligaments. After arthroscopic documentation of the graft position, the anatomical position of the AC joint is adjusted under fluoroscopic guidance. Knots above the clavicle, under constant axial adjustment, then secure the sutures. The wound is closed in layers (Fig. 5a–c).
Mini-open Twin Tail tight-rope technique
The patient is positioned in the beach chair position. A vertical incision is made, approximately 3 cm medial to the AC joint, along the anterior border of the clavicle in the direction of the coracoid process. After exposure of the delta-trapezial fascia, the fascia is split lengthwise, and the clavicle is dissected. An incision is made lengthwise through the deltoid muscle to expose the base of the coracoid process. This is followed by the insertion of the Twin Tail system after a 4.5 mm drill incision is made through the coracoid and the inserted button is flipped below the coracoid. After two additional 4.0 mm drill incisions are made, positioned 2 cm and 4 cm medial to the AC joint, the anchors of the suture system are channeled outwards (caudal-cranial). The two buttons, cranial to the clavicle are flipped and loosely tightened. Under fluoroscopic guidance, the buttons are repositioned and tightened by the pulley system and the sutures secured by knots. The dorsal segments of the joint capsule are sutured, and the fascia is repaired (Fig. 6a–d).
Postoperative care.
After surgery, a follow-up radiographic examination consisting of a half panoramic projection without weight is performed (Fig. 6).
The postoperative recovery program was identical in both groups. An arm sling (Medi © Armschlinge) was used to ensure stability of the joint and maintain the correct position of the implant, which the patients were to wear throughout the first 4 weeks following the surgical procedure. Additionally, patients received an ossification prophylaxis with celecoxib given at a dose of 200 mg twice daily for 2 weeks after the surgery. Contracture prophylaxis was administered through physiotherapeutic assisted mobilization of the shoulder in abduction and flexion up to 40 degrees until completion of the second postoperative week. Thereafter, passive extension of the mobility range was increased to 90 degrees. Full stress of the joint as well as weight-bearing on the extended arm and rotational movement of the shoulder were to be avoided until after the sixth postoperative week. Neither one of the applied surgical techniques required the removal of materials after recovery.
Statistics
The required number of patients for the study was determined by the GPower 3.1. software. According to the expected mean value applied to the CS with 85 ± 4 points and power of 95%, 18 patients were calculated to be required for the arthroscopy group. Likewise, 18 patients were calculated as the required number of patients for the MO group with an expected mean value applied to the CS of 80 ± 4 points and power of 95%.
Statistical analysis was performed using the IBM© SPSS© Statistics software. The comparison of the individual group values was carried out at a double-sided significance level of 5%. P-values ≤ 0.05 were considered statistically significant. The unconnected samples of the distribution-free interval-scaled data were analyzed using the Mann–Whitney U test. Results were given as an average value ± standard error (minimum–maximum).
A positive vote from the ethics committee of Baden-Württemberg was granted prior to the study (08/15/2013; registry number: F-2013-052).
Results
A follow-up examination was conducted of 19 patients who had received the arthroscopic surgery and of 26 patients who had undergone the surgery in the mini-open technique. The average age of the patients in the ASK group was 33 ± 10 years and 35 ± 10 years in the MO group. The main cause of injury were injuries acquired during athletic activities such as mountain bike riding (n = 12), snowboarding (n = 8), soccer (n = 7), and skiing (n = 5) and in rarer incidents, accidents by falling, handball, rugby, or karate injuries.
Clinical results
Both groups showed good-to-excellent results in the clinical score evaluations with no significant differences between both groups which are shown in Table 3.
Radiological results
Coracoclavicular distance and width of the AC joint
The radiological results concerning the coracoclavicular distance and the width of the AC joint are shown in Table 4. There were significant differences in the ASK group regarding the CC distance, ranging from + 3.6 mm ± 3.5 (− 1.0 to 10.5 mm, p = 0.003), and the width of AC joint, showing + 2.6 mm ± 2.4 (− 0.8 to 8.7 mm, p = 0.006) when compared to the non-operative shoulder. In the MO group, no significant differences were found in the CC distance after comparison of the operative and non-operative shoulder. Considering the mean value, a significant difference in the AC distance of + 1.9 mm ± 2.6 (− 1.8 to 8.3 mm) was also found in the MO group when compared to the non-operative shoulder (p = 0.002).
When comparing both patient groups, no significant differences in measurement of the CC- and AC- distances of the operative shoulder were found (CC distance: p = 0.075, AC distance p = 0.905).
Dynamic translation (DT)
In the ASK group, significant differences were found in the superior (p = 0.053) and the combined translation (p = 0.018). No significant differences were found in the mere posterior translation after comparison of the operative and non-operative shoulder (p = 0.152).
In the MO group, there were no significant differences in either translation when both shoulders were compared (superior: p = 0.317; posterior: p = 0.788; combined: p = 0.772).
In order to offer comparison to similar studies, a difference in the combined translation greater than 5 mm, while comparing the operative with the non-operative shoulder, was counted as a “residual horizontal instability”.
Accordingly, 43% of patients in the ASK group showed a residual horizontal instability, whereas in the MO group, only 31% of patients showed a residual horizontal instability (Table 5).
When comparing the ASK and the MO group, both the posterior and the combined translation were significantly greater in the ASK group than in the MO group (posterior: Δ = 5.5 mm; combined: Δ = 8.2 mm, p = 0.001).
Coherence of clinical and radiological results
Overcorrection of the AC joint did not result in any functional deficits in athletes in reference to the Constant Murley Score (CMS). In both cases with the greatest overcorrection of 1.8 and 1.5 mm of the AC joint, 94 and 96 points were achieved in the CMS score. In the cases of overcorrection of the CC distance of 3.8 and 2.4 mm, scores of 95 and 98 points were achieved in the CMS.
In the ASK group, three subluxations and three dislocations showed heterogeneous score results (subluxations: 53, 96 and 97 points; dislocations: 74, 96 and 97 points). Likewise, four patients (15.4%) from the MO group showed heterogeneous results in their CMS score with 81, 89, 94 and 96 points.
Return to sports and the level of sports activity
Patients of the ASK group showed an average level of sports activity of 2.8 according to Valderrabano. This was equivalent to a weekly amount of 5 h of sports. Sports activity on a competitive level (Valderrabano level 4) was practiced by five patients of the ASK group. Athletes in this group reported to have been able to achieve average results in their return to their athletic activity with a result of 1.6 points according to Rhee, which is equivalent to 90–100% of their previous athletic capacity. One patient was reported not being able to return to his athletic activity, achieving five points in the Rhee score and continued to experience difficulties during regular day-to-day routines. All in all, 13 of 19 patients were able to completely recover their previous athletic activity.
In the MO group, a similar average level of sports activity of 2.6 points according to Valderrabano was found. Upon average with a point score of 1.5 according to Rhee, likewise a 90–100% recovery of the patient’s athletic capacity was achieved. One patient recovered only 50% of his previous athletic capacity claiming four points in the Rhee score. 20 of 26 patients within the MO group achieved a full recovery to their previous level of sports activity.
Complications
Out of 19 patients, 6 showed a relevant increase of the coracoclavicular distance postoperatively in the ASK group, whereas three of these were to be classified as subluxations. Re-dislocation of the AC joint occurred in three cases postoperatively due to the dislocation of the TightRope button. In 4 of 26 cases postoperative loss of reduction was found within the MO group, showing a subluxation of the AC joint in the follow-up examination. A complete loss of correction of the AC joint was not found throughout this group (Figs. 7 and 8).
Discussion
The aim of this study was to compare the clinical and radiological results of both surgical techniques when treating athletes practicing sports on a high or competitive level. The athlete’s ability to return to their previous sports activity and possible differences in dynamic posterior translation (DPT) received special consideration. The most important finding of this study is that the mini-open technique provides better radiological results with a significantly lower dynamic posterior translation than the comparable arthroscopic method. An explanation for this outcome is most likely found in the additional reconstruction of the fascia and dorsal joint capsule. Both surgical techniques proved successful in restoring athletic capacity after acute AC-joint injuries. However, the results suggest that the mini-open technique is mild superior to the arthroscopic procedure regarding the recovery of the athlete’s original level of sporting activity. Nevertheless, the arthroscopic procedure in cases of AC-joint injuries can be helpful to detect concomitant injuries to the shoulder joint [23].
Throughout the previous years, various surgical techniques have been developed for the treatment of high-grade acromioclavicular joint disruptions. A study conducted by Bahlke et al. in the year 2015 showed that at the time, stabilization of the acromioclavicular joint was most commonly performed by hook plate fixation. Arthroscopic or mini-open techniques for surgical coracoclavicular stabilization using the TightRope were the second most conducted operative procedures [24]. A gold standard for surgical treatment of AC-joint disruptions has not yet been established. A prospective level II study, conducted by Stein et al. [25], demonstrated that the arthroscopic stabilization is superior to the hook plate fixation. Nevertheless, various studies on the implementation of the hook plate fixation as well as on the TightRope procedure and the PDS cerclage technique show good-to-excellent clinical results [2, 6,7,8,9,10,11,12,13,14,15,16]. Likewise, the surgical techniques observed in the course of this study show comparable excellent results in the evaluation of the Constant Murley Score (ASK: 91.2 points, MO: 91.6 points), as well as very good results in the Taft Score and the Simple Shoulder Test (Taft: ASK: 10.3 points, MO: 10.5 points; SST: ASK: 11.7 points, MO: 11.7 points).
Despite the excellent clinical results, a postoperative increase in the CC distance as well as a residual horizontal instability are often found in the Alexander view. Studies have shown that neither a narrowing of the AC joint nor an increase in the CC distance correlate with poor clinical outcomes. When observing the width of the AC joint of the non-operative shoulder in comparison to the operative shoulder, a significant increase in the width of the AC joint was found in both groups (MO: p = 0.002, ASK: p = 0.006), which, however, did not affect the clinical outcome.
Radiological analysis showed three subluxations (15.8%) and three dislocations (15.8%) with very heterogeneous CMS results in the ASK group. The three patients of the MO group who experienced subluxations (15.4%) achieved good-to-excellent CMS results (81, 89, 94, and 96 points). These results are comparable to those gathered in other studies conducted on coracoclavicular stabilization using the PDS cerclage technique. In these studies, the authors reported an average subluxation rate of 14.3% and mean dislocation rate of 5.3% with likewise consistent excellent functional results [7, 14, 26]. Patients who had received an overcorrection of the AC joint showed no functional deficits according to the CMS results. Outcomes of this study as well as those of other studies suggest that overcorrection of the AC joint is to be preferred over a remaining subluxation of the AC joint. Therefore, under consideration of this aspect, the mini-open procedure proved superior to the arthroscopic technique. In summary, occurrences of loss of correction in the MO group were less relevant, and more overcorrections were observed in the MO group than in the ASK group.
In contrast to this, increased DPT has been repeatedly associated with poorer functional results, whereas improvement of the horizontal stability coincides with better clinical results [18, 27, 28]. The correct placement of the coracoidal drill channel has already been identified as a key variable for improving horizontal stability [29]. It has also been shown that the now common use of two coracoidal sutures is superior to the use of only one suture connection [16, 17]. Despite the implementation of these findings, a high rate of residual horizontal instability of 48% on average remains in many studies (42.9–53.3%) [16, 19, 20, 27]. In this study, in the ASK group, a residual horizontal instability was found in 43% of cases, while this was only the case in 31% of the MO group. It should also be emphasized in the analysis of these results that none of the measurements in the group MO showed a significant difference in dynamic instability between the non-operative and operative shoulder. Additionally, the posterior and combined translation of both the non-operative and operated shoulder were significantly lower in the MO group than in the ASK group (posterior: p = 0.037, combined: p = 0.001).
The results of this study show that the mini-open implantation of the TwinTail Tight-Rope implant provides better results concerning dynamic posterior translation than a mere arthroscopic approach with a comparable implant. The additional fascial suture and reconstruction of the dorsal joint capsule are most likely responsible for the increase in horizontal stability. Whether this hypothetically more stable construct of soft tissue reconstruction and twin-tailed implant provide better clinical and radiological results in the long term remains to be investigated in further studies and compared with additional possibilities of horizontal stabilization.
Return to sports and level of sports activity
Through both of the applied surgical techniques, this demanding patient population achieved a high rate-of-return to their original level of sports activity. With an average level of sports activity of 2.8 according to Valderrabano, 69% of the patients in the ASK group were able to recover their full athletic capacity. In the MO group, 77% of the patients were able to fully recover their previous athletic capacity with an average level of sports activity of 2.6 according to Valderrabano. 20 of 26 patients within the MO group achieved a full recovery to their previous level of sports activity.
The results of this study suggest that more sportsmen achieved a full recovery to their previous level of sports activity when the mini-open procedure was used. Even if this not significant. Therefore, these are consistent with the findings of Faggiani et al. in 2016 which demonstrated that patients receiving the mini-open procedure showed significantly better results in the SPORTS score than those who had been treated arthroscopically [30].
Studies on the return to sporting activities after twin-tailed coracoclavicular stabilization using comparable implants show an average recovery rate of the previous level of sports activity of 80.4% (62–92%) [11, 31,32,33,34]. In the MO group, a similar outcome was achieved. However, in these studies, none or no comparable classifications of the level of sports activity were applied. Therefore, the results are to be considered critically and an absolute comparison is difficult.
Nevertheless, it should be noted that despite good functional results, an average of one quarter of all patients in this study and about one fifth of the patients in comparable studies were unable to return to their initial sporting level. As in the studies mentioned above, the functional results of this study are essentially based on the Constant Murley Score. However, remaining residual instability or limitations under maximum load, as is often the case in sports, are insufficiently evaluated.
Due to the described clinical and functional relevance of dynamic posterior instability, a standardized assessment of dynamic posterior translation should be established in the future. Scheibel et al. provide a possible approach for this with their Acromioclavicular Joint Instability Score which, however, is hardly applied [27]. Likewise, Kraus et al. proposed the introduction of a new classification of AC-joint disruptions, which not only includes the consideration of vertical instability, but also dynamic posterior translation [35]. In order to improve the functional comparison and evaluation of AC-joint treatment, a uniform methodology should be established for the conduction of future studies.
Limitations
Due to the drop out of patients with very good results who did not consider further examination necessary, the size of the groups varies. Nevertheless, the results of the remaining patients provided satisfactory on functionality, stability, and sports level after surgical treatment of AC-joint disruption. An additional limitation of the study is the circumstance that as there was no control group, meaning that only a comparison between the two groups and similar surgical procedures can be drawn. Also, based on this study, further statements on the conservative treatment options cannot be made.
Conclusion
Both surgical procedures observed in this study prove to be effective techniques for the stabilization of high-grade AC-joint injuries in athletes. From a radiographic standpoint, surgical treatment by the mini-open procedure proved superior to the arthroscopic technique. However, a significant correction can be performed using both techniques. Patients undergoing the mini-open procedure are less likely to experience a loss of correction. Additionally, the extent of the loss of correction in this group was less pronounced.
More importantly, the study showed that reconstruction of the AC joint by the mini-open procedure results in a significantly higher horizontal stability in comparison to the arthroscopic technique. It is probable that the further increase in horizontal stability is achieved by the additional reconstruction of the fascia and dorsal joint capsule. Both groups showed excellent clinical results and, therefore, both procedures prove to be effective treatment options for the recovery of athletic capacity on a high to competitive level. The results of the study suggest that the mini-open procedure and the arthroscopic technique aiming almost the same results to restore the previous level of sports activity.
References
Bosch U, Fremerey RW (2003) AC-Gelenkverletzungen. Trauma und Berufskrankheit 5(1):s126–s129. https://doi.org/10.1007/s10039-002-0627-6
Yoon JP, Lee B-J, Nam SJ, Chung SW, Jeong W-J, Min W-K et al (2015) Comparison of results between hook plate fixation and ligament reconstruction for acute unstable acromioclavicular joint dislocation. Clin Orthop Surg 7(1):97–103. https://doi.org/10.4055/cios.2015.7.1.97
Costic RS, Labriola JE, Rodosky MW, Debski RE (2004) Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med 32(8):1929–1936. https://doi.org/10.1177/0363546504264637
Salzmann GM, Walz L, Schoettle PB, Imhoff AB (2008) Arthroscopic anatomical reconstruction of the acromioclavicular joint. Acta Orthop Belg 74(3):397–400
Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA (2006) A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med 34(2):236–246. https://doi.org/10.1177/0363546505281795
Gstettner C, Tauber M, Hitzl W, Resch H (2008) Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg 17(2):220–225. https://doi.org/10.1016/j.jse.2007.07.017
Sandmann GH, Martetschläger F, Mey L, Kraus TM, Buchholz A, Ahrens P et al (2012) Reconstruction of displaced acromio-clavicular joint dislocations using a triple suture-cerclage: description of a safe and efficient surgical technique. Patient Saf Surg 6(1):1–7. https://doi.org/10.1186/1754-9493-6-25
Petersen W, Wellmann M, Rosslenbroich S, Zantop T (2010) Minimalinvasive Akromioklavikulargelenkrekonstruktion (MINAR). Oper Orthop Traumatol 22(1):52–61. https://doi.org/10.1007/s00064-010-3004-4
Di Francesco A, Zoccali C, Colafarina O, Pizzoferrato R, Flamini S (2012) The use of hook plate in type III and V acromio-clavicular Rockwood dislocations: clinical and radiological midterm results and MRI evaluation in 42 patients. Injury 43(2):147–152. https://doi.org/10.1016/j.injury.2011.04.002
Kienast B, Thietje R, Queitsch C, Gille J, Schulz A, Meiners J (2011) Mid-term results after operative treatment of rockwood grade III-V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res 16(2):52–56. https://doi.org/10.1186/2047-783X-16-2-52
De Carli A, Lanzetti RM, Ciompi A, Lupariello D, Rota P, Ferretti A (2015) Acromioclavicular third degree dislocation: surgical treatment in acute cases. J Orthop Surg Res 10(1):13. https://doi.org/10.1186/s13018-014-0150-z
Eschler A, Gradl G, Gierer P, Mittlmeier T, Beck M (2012) Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch Orthop Trauma Surg 132(1):33–39. https://doi.org/10.1007/s00402-011-1399-x
Jensen G, Katthagen JC, Alvarado LE, Lill H, Voigt C (2014) Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg Sports Traumatol Arthrosc 22(2):422–430. https://doi.org/10.1007/s00167-012-2270-5
Greiner S, Braunsdorf J, Perka C, Herrmann S, Scheffler S (2009) Mid to long-term results of open acromioclavicular-joint reconstruction using polydioxansulfate cerclage augmentation. Arch Orthop Trauma Surg 129(6):735–740. https://doi.org/10.1007/s00402-008-0688-5
Natera-Cisneros L, Sarasquete-Reiriz J, Escolà-Benet A, Rodriguez-Miralles J (2016) Acute high-grade acromioclavicular joint injuries treatment: arthroscopic non-rigid coracoclavicular fixation provides better quality of life outcomes than hook plate ORIF. Orthop Traumatol Surg Res 102(1):31–39. https://doi.org/10.1016/j.otsr.2015.10.007
Gerhardt C, Kraus N, Pauly S, Scheibel M (2013) Arthroskopisch assistierte Stabilisierung akuter Schultereckgelenkverletzungen in Doppel-TightRope™-Technik. Unfallchirurg 116(2):125–130. https://doi.org/10.1007/s00113-011-2065-z
Venjakob AJ, Salzmann GM, Gabel F, Buchmann S, Walz L, Spang JT et al (2013) Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations: 58-month findings. Am J Sports Med 41(3):615–621. https://doi.org/10.1177/0363546512473438
Gerhardt C, Kraus N, Greiner S, Scheibel M (2011) Arthroskopische Stabilisierung der akuten Schultereckgelenksprengung. Orthopade 40(1):61–69. https://doi.org/10.1007/s00132-010-1680-7
Kraus N, Minkus M, Scheibel M (2014) Schultereckgelenksprengungen. Trauma und Berufskrankheit 16(4):251–257. https://doi.org/10.1007/s10039-014-2147-6
Lim YW, Sood A, van Riet RP, Bain GI (2007) Acromioclavicular joint reduction, repair and reconstruction using metallic buttons-early results and complications. Tech Shoulder Elb Surg 8(4):213–221. https://doi.org/10.1097/BTE.0b013e3181578965
Walz L, Salzmann GM, Fabbro T, Eichhorn S, Imhoff AB (2008) The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med 36(12):2398–2406. https://doi.org/10.1177/0363546508322524
Berthold D, Dyrna F, Imhoff A, Martetschläger F (2019) Innovationen bei der Therapie von Instabilitäten des Akromioklavikulargelenks. Arthroskopie 32(1):11–14. https://doi.org/10.1007/s00142-018-0245-3
Tischer T, Salzmann GM, El-Azab H, Vogt S, Imhoff AB (2009) Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. Am J Sports Med 37(1):136–139. https://doi.org/10.1177/0363546508322891
Balke M, Schneider M, Akoto R, Bäthis H, Bouillon B, Banerjee M (2015) Die akute Schultereckgelenkverletzung. Unfallchirurg 118(10):851–857. https://doi.org/10.1007/s00113-013-2547-2
Stein T, Müller D, Blank M, Reinig Y, Saier T, Hoffmann R et al (2018) Stabilization of acute high-grade acromioclavicular joint separation: a prospective assessment of the clavicular hook plate versus the double double-button suture procedure. Am J Sports Med 46(11):2725–2734. https://doi.org/10.1177/0363546518788355
Krueger-Franke M, Siebert C, Rosemeyer B (1993) Surgical treatment of dislocations of the acromioclavicular joint in the athlete. Br J Sports Med 27(2):121–124. https://doi.org/10.1136/bjsm.27.2.121
Scheibel M, Dröschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 39(7):1507–1516. https://doi.org/10.1177/0363546511399379
Kraus N, Haas NP, Scheibel M, Gerhardt C (2013) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations in a coracoclavicular Double-TightRope technique: V-shaped versus parallel drill hole orientation. Arch Orthop Trauma Surg 133(10):1431–1440. https://doi.org/10.1007/s00402-013-1804-8
Schliemann B, Roßlenbroich SB, Schneider KN, Theisen C, Petersen W, Raschke MJ et al (2015) Why does minimally invasive coracoclavicular ligament reconstruction using a flip button repair technique fail? An analysis of risk factors and complications. Knee Surg Sports Traumatol Arthrosc 23(5):1419–1425. https://doi.org/10.1007/s00167-013-2737-z
Faggiani M, Vasario G, Mattei L, Calò M, Castoldi F (2016) Comparing mini-open and arthroscopic acromioclavicular joint repair: functional results and return to sport. Musculoskelet Surg 100(3):187–191. https://doi.org/10.1007/s12306-016-0411-6
Loriaut P, Casabianca L, Alkhaili J, Dallaudiere B, Desportes E, Rousseau R et al (2015) Arthroscopic treatment of acute acromioclavicular dislocations using a double button device: clinical and MRI results. Orthop Traumatol Surg Res 101(8):895–901. https://doi.org/10.1016/j.otsr.2015.09.024
Porschke F, Schnetzke M, Aytac S, Studier-Fischer S, Gruetzner PA, Guehring T (2017) Sports activity after anatomic acromioclavicular joint stabilisation with flip-button technique. Knee Surg Sports Traumatol Arthrosc 25(7):1995–2003. https://doi.org/10.1007/s00167-016-4287-7
Saier T, Plath J, Beitzel K, Minzlaff P, Feucht J, Reuter S et al (2016) Return-to-activity after anatomical reconstruction of acute high-grade acromioclavicular separation. BMC Musculoskelet Disord 17(1):145. https://doi.org/10.1186/s12891-016-0989-8
Xu J, Liu H, Lu W, Li D, Zhu W, Ouyang K et al (2018) A retrospective comparative study of arthroscopic fixation in acute Rockwood type IV acromioclavicular joint dislocation: single versus double paired Endobutton technique. BMC Musculoskelet Disord 19(1):170. https://doi.org/10.1186/s12891-018-2104-9
Kraus N, Hann C, Gerhardt C, Scheibel M (2018) Dynamic instability of the acromioclavicular joint. Obere Extremitaet 13(4):279–285. https://doi.org/10.1007/s11678-018-0469-x
Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B (2006) Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med 34(6):993–999. https://doi.org/10.1177/0363546505284189
Rhee YG, Ha JH, Cho NS (2006) Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med 34(6):979–985. https://doi.org/10.1177/0363546505283267
Funding
The authors declare that they have not received any financial funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
A positive vote from the ethics committee of Baden-Württemberg was granted prior to the study (08/15/2013; registry number: F-2013-052).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koch, M., Werner, A., Engel, G. et al. Mini-open vs. arthroscopic double tight-rope reconstruction after acute AC-joint dislocation: a comparison in functional outcome and sports activity. Arch Orthop Trauma Surg 143, 5491–5500 (2023). https://doi.org/10.1007/s00402-023-04828-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04828-8