Abstract
Background
Robotic assisted total knee arthroplasty (RTKA) has shown improved knee alignment and reduced radiographic outliers. However, there remains debate on functional outcomes and patient-reported outcomes (PROMs). This study compares the 1-year clinical outcomes of a new imageless robotically assisted technique (ROSA Knee System, Zimmer Biomet, Warsaw, IN) with an imageless navigated procedure (NTKA, iAssist Knee, Zimmer, Warsaw, IN).
Methods
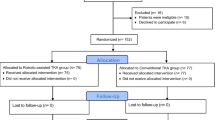
The study is a retrospective analysis of prospectively collected data that compared the functional outcomes and PROMs of 50 imageless RTKA with 47 imageless NTKA at 1-year follow-up. Baseline characteristics, intraoperative and postoperative information were collected including complications, revisions, Knee Society Score (KSS), Knee injury and Osteoarthritis Outcome Score (KOOS) score, and Forgotten Joint Score (FJS-12). Radiographic analysis of preoperative and postoperative images evaluating hip–knee–ankle (HKA) angle was performed.
Results
There was no difference regarding baseline characteristics between the groups. Mean operative time was significantly longer in the RTKA group (122 min vs. 97 min; p < 0.0001). Significant differences were reported for the “Pain” (85 [RTKA] vs 79.1 [NTKA]; p = 0.0283) subsection of the KOOS score. In addition, RTKA was associated with higher maximum range of motion (119.4° vs. 107.1°; p < 0.0001) and better mean improvement of the arc of motion by 11.67° (23.02° vs. 11.36°; p < 0.0001). No significant differences were noted for other subsections of KOOS, KSS, FJS-12, complications, or limb alignment at 1-year follow-up.
Conclusions
Imageless RTKA was associated with longer surgical time, better pain perception and improved ROM at 12-month follow-up compared with NTKA. No significant differences were reported on other PROMs, complication rates and radiographic outcomes.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total Knee Arthroplasty (TKA) is considered the gold standard treatment for end-stage knee osteoarthritis [1, 2]. Limb alignment and implant positioning are considered among the most important prognostic factors for long-term implant survivorship, patient satisfaction and clinical outcomes [1, 3, 4]. To improve that, computer navigation and robotic-assisted surgery have gained interest as tools that help the surgeon to perform TKA with greater precision and accuracy.
Robotic technologies have been introduced with the expectation to improve component positioning providing increased accuracy and consistency in bone resections while reducing soft tissue damages [5, 6]. Instability, aseptic loosening, malalignment, and increased polyethylene wear are among the most frequent causes of implant failure, and all of them are related to a poorly balanced and malaligned knee [7]. In addition, components malpositioning is frequently associated with patient dissatisfaction, patellofemoral complications, and it may leads to implant failure and early revision surgery [8, 9]. Robotic surgeries have proven successful in increasing early functional outcomes and reducing radiographic outliers compared with conventional technique, however, mid-to-long term studies have yet to prove meaningful enhancement in terms of implant survivorship, patient satisfaction, and functional outcomes [10]. However, most of the available literature refers to CT-guided robotic TKA [11,12,13], while few studies report on imageless robotic systems [14, 15]. In fact, avoiding the need of a preoperative CT-scan, imageless robotic systems have the advantages of reducing the radiation exposition of the patients while ensuring smoother preoperative and intraoperative procedures.
Imageless navigation is a simple solution, relatively recently introduced as a tool to drive the distal femoral and proximal tibial cuts, to facilitate and improve the precision of TKAs’ coronal alignment, avoiding intramedullary canal guides, when aiming for a mechanical axis of the lower limb [16].
Different studies have been published on potential functional and alignment advantages of robotic-assisted TKA (RTKA) compared to conventional manual TKA, but to the best of the authors’ knowledge, there is a lack of evidence on comparison between RTKA and navigated TKA (NTKA). The primary endpoint of this study was to compare the 1-year clinical outcomes following imageless RTKA and imageless NTKA. Our hypothesis was that RTKA was associated with improved patient-reported outcome measures (PROMs) and range of motion (ROM) at 1-year follow-up.
Materials and methods
Patients that underwent total knee arthroplasty (TKA) for primary knee osteoarthritis between February and September 2020 were prospectively followed and retrospectively evaluated. All surgical procedures were performed by experienced knee arthroplasty surgeons at a high-volume institution. After excluding the first 25 robotic cases to allow for an appropriate learning curve window for the surgical equipe, patients’ data were collected and analyzed. During this time, a total of 173 primary TKAs were performed in the orthopaedic department, including 87 consecutive navigated TKAs (imageless NTKA, iAssist Knee, Zimmer, Warsaw, IN) and 61 consecutive robotic TKAs (RTKA, ROSA Knee System, Zimmer Biomet, Warsaw, IN) using a single implant design (Persona PS Knee, Zimmer, Warsaw, IN). Eleven patients in the RTKA group were excluded from this cohort for different reasons such as: patients with ligament insufficiency that required higher level of constraint, patients with a diagnosis other than primary osteoarthritis, patients with a deformity requiring augmentation, neurological movement disorders, patients with severe varus deformity (> 15°), patients with valgus deformity, and patients that did not complete their 1-year clinical and radiographic follow-up. Fifty RTKA patients with mild-to-moderate varus deformity (≤ 15°) undergoing primary unilateral TKA were, finally, included for final analysis with a mean follow-up of 13.4 months (± 1.3, range 12–15). Varus deformity was defined as a hip–knee–ankle (HKA) angle greater than or equal to 1° with the mechanical axis (MA) passing medial to the knee joint. A matched cohort of 47 consecutive navigated TKAs performed during the same period, was used for comparison with a mean follow-up of 13.6 months (± 1.2, range 12–15).
The electronic medical records were collected prospectively and reviewed retrospectively for preoperative basic demographic information, intraoperative events and postoperative function and complications. Demographic information included age (years), weight (kg), height (m), sex, body mass index (BMI, kg/m2), and operated side. Intraoperative information included operating room (OR) time (min). OR time was considered from when the patient entered the theatre to when he/she left it, including robotic device setup time. Surgical anesthesia was performed before entering the theatre. Complications were classified as wound complications, including cellulitis or wound drainage of the surgical site or the pin insertion site (treated conservatively), and reoperation for any cause (debridement, antibiotics and implant retention [DAIR], two-stage revision for periprosthetic joint infection [PJI], and revision for any other cause). If a patient with a superficial wound infection was later found to have a PJI, he/she was excluded from the wound complication count and only included in the reoperation group.
Patients were followed-up clinically and radiographically at 3, 6, and 12 months postoperatively. Full medical records were reviewed, including preoperative Knee Society Knee (KSSk) and Function score (KSSf), range of motion (ROM), and lower limb alignment (hip–knee–ankle angle [HKA]). Knee function at postoperative evaluation was assessed at 12-month follow-up with the KSSk score, KSSf score, Knee injury and Osteoarthritis Outcome Score (KOOS) score, and Forgotten Joint Score (FJS-12) [17, 18]. Clinical scores were collected by a trained research-fellow at 1-year follow-up. Radiographic analysis of preoperative and postoperative images evaluating HKA angle was performed by independent fellowship-trained orthopedic surgeon [19, 20]. Radiographic outliers were considered when falling outside of a cutoff of ± 3° from MA.
All surgical procedures were performed through a standard medial parapatellar approach, and the same prosthetic implant was used in every case (Persona Posterior Stabilized [PS] Knee, Zimmer, Warsaw, IN). The ROSA Knee System (Zimmer Biomet, Warsaw, IN) is a collaborative robotic device that allows the surgeon to proceed with an image-based planning using a 3D virtual model based on specific preoperative 2D radiographs, or an image-less planning based on intraoperative bony landmarks collection and ligament balancing evaluation. All cases included in this study were performed with the image-less procedure. The surgical technique of ROSA Knee System has been previously described [21] and its accuracy demonstrated both in vitro and in vivo [22]. Preoperatively, the robotic-assisted procedure aimed for a functional personalized aliment with an under correction of the original deformity leaving 2° of varus. The aimed femoral coronal angle was 90° (LDFA), the femoral sagittal angle (FSA) was 3° according to the implant’s surgical technique, the tibial coronal angle was 88° (MPTA), and the tibial sagittal angle was 3° (TSA) according to the implant’s surgical technique.
The iASSIST (Zimmer, Warsaw, IN, US) navigation device is a handheld computer‐assisted accelerometer-based stereotaxic system integrated into a small pod which attaches to the femoral and tibial resection cutting jigs, guiding the resection at the appropriate angles in both the coronal and sagittal planes. After bone resection, the accuracy of the alignment can be validated, confirming the position of both the femoral and tibial components. The surgical workflow follows the classic method of femoral and tibial bone resection with each bone resected independently along the mechanical axis [16]. Preoperatively, the navigated assisted procedures aimed to achieve a neutral MA.
All patients in both groups followed the same standardized postoperative rehabilitation protocol. However, even though specific differences were addressed to each patient, typically rehabilitation started the day of surgery with active and passive ROM and partial weight bearing as tolerated. Stretching exercises and a light strength training program were started to reinforce the surrounding muscles. Each physiotherapy session was performed by the same multidisciplinary team in both groups. Discharge was between 4 and 7 days (mean, 5 days) after pain control, knee flexion to minimum 90°, independent mobilization with the use of crutches, and independent ascent and descent of stairs was achieved. All patients completed the above protocol with a combination of outpatient and at-home physical therapy.
The study is performed in accordance with the ethical standards in the 1964 Declaration of Helsinki and with the HIPAA regulation. The Institutional Review Board (IRB) of the author’s institution defined this study as exempt from IRB approval (prospective study on a well-established surgical procedure and commercialized implant).
Statistical analysis
A power analysis was performed using a two-sided test at an alpha level of 0.05 with a power or 80% to determine the required sample size for statistical significance according to our main endpoints with a medium effect size. Based on the power analysis, 90 patients (45 in each group) were needed to detect a significant difference. Considering a potential 5–10% dropout, the outcomes of 98 patients were analyzed. Baseline patients’ characteristics and functional scores were compared between the two cohorts with univariate analyses. Data were described using frequencies for categorical data and mean (SD) and range as appropriate for continuous data. Wilcoxon Rank Sum Test was performed for continuous variables to compare means, while Fisher Exact Test was performed for categorical variables. Histograms were created to compare the distribution of KSSk, KSSf, FJS, and KOOS score between RTKA and NTKA cohorts. ROM, HKA angle, KSS, KSSf, FJS, and KOOS were compared between the two groups using a Wilcoxon Rank Sum Test. Multivariate general linear models with baseline characteristics as covariates were used to evaluate the associations of the surgical technique with functional outcomes using the F Test based on Type III sum squares in the ANCOVA model. The covariates analyzed were surgical technique (NTKA vs RTKA), age, sex, and BMI. All these variables were included in the regression model, and variables with the weakest correlations were sequentially removed in subsequent models until that with the strongest association was identified.
All data were analyzed using SAS 9.4 (SAS Institute, North Carolina, US) and statistical significance was maintained at a p value of less than 0.05.
Results
Demographics and perioperative outcomes
There were no significant differences in age, gender, and BMI between the two groups (Table 1). Compared to the NTKA group, the RTKA group reported a statistically significant longer surgical duration (122 min vs. 97 min; p < 0.0001), while no significant difference was reported for mean recovery days (5.1 days vs. 4.9 days; p = 0.2975) (Table 2, Fig. 1).
PROMs
There were no significant differences in preoperative KSSk and KSSf score and postoperative FJS and overall KOOS score. Significant differences were reported for the “Pain” (p = 0.0283) and “Function” (p = 0.0360) subsection of the KOOS score, however, the model F test p values showed that “age” was an influencing cofounding factor for the “Function” subsection (F Test p = 0.1087), and after having covariate age in the model, treatment impact to KOOS Function score was not significant anymore (F Test p = 0.0550) (Fig. 2). Postoperative KSS knee and function scores were significantly higher in the RTKA group (p < 0.0001), however, F test p values based on Type III sum squares in the ANCOVA model indicated that treatment (p < 0.0001) and gender (p = 0.0226) had significant impact on subjects’ KSS Knee Score. The interaction between gender and treatment arm were not significant at level of 0.05 (p = 0.3000). In addition, F test based on Type III sum squares indicated that both BMI (p = 0.0381) and treatment (p < 0.0001) had significant impact on KSS Function Score (Table 3).
Range of motion
Preoperative ROM was not significantly different between the two groups. F test p value based on Type III sum squares in the ANCOVA model showed that treatment had significant impact on ROM at final follow-up (p < 0.0001). Comparing least square means from general linear model, RTKA group had higher maximum range of motion compared to NTKA group (119.4° vs. 107.1°; p < 0.0001), and the mean delta improvement in the arc of motion from preoperative was significantly higher in the RTKA group at the last follow-up by 11.67° (23.02° vs. 11.36°; p < 0.0001) (Table 4).
Radiographic outcomes
No significant difference was reported on the preoperative and postoperative HKA angle between the two groups; however, the overall number of postoperative outliers was higher in the RTKA group (30.00% vs. 17.02%; p = 0.1570). (Table 5, Fig. 3).
The mean postoperative HKA angle in the RTKA group was 177.42° (SD ± 1.7°), the mean femoral coronal alignment based on LDFA was 89.77° (SD ± 1.4°), the mean FSA was 87.47° (SD ± 1.5°), the mean MPTA was 87.99° (SD ± 0.9°), and the mean TSA was 86.29° (SD ± 1.0°). Considering the preoperatively aimed angles, the mean HKA deviation from target was 1.5° (range, 4.2°–0.1°), the mean LDFA deviation from target was 1.3° (range, 3.6°–0.1°), the mean FSA deviation from target was 1.3° (range, 3.8°–0.1°), the mean MPTA deviation from target was 0.7° (range, 2.3°–0.1°), the mean TSA deviation from target was 0.9° (range, 3.2°–0.1°).
Complications and reoperations
Overall, one case required reoperation in the RTKA group (2%) compared with three cases in the NTKA group (6.4%, n.s.) (Table 6). Wound complications were reported in two cases in the RTKA group (4%) as compared to four cases in the NTKA group (8.7%, n.s.). None of the wound complications were directly related to the specific devices used and none of them were at pin sites used for intraoperative planning and reference. No cases of periprosthetic fractures or fractures at pin sites were reported.
Discussion
The most important findings of this study were that at 12-month follow-up the robotic-arm assisted imageless TKA reported better improvement in ROM and KOOS pain score compared to navigated TKA suggesting favorable functional outcomes at short-term follow-up. This is in line with what recently reported in the literature [10], however, there is a lack of evidence on clinical outcomes of imageless RTKA compared to the conventional technique, while numerous studies have described the outcomes of CT-based robotic systems. To the best of authors’ knowledge, this is the first study that compares the ROSA Knee System with an imageless navigation system instead of a conventional technique.
This study reports a significant mean OR time difference of 25 min between the two groups (122 min RTKA vs 97 min NTKA). As previously stated, we intended the OR time from the moment the patient entered the surgical theatre and not only from skin incision to wound closure. Clearly, time for surgical anesthesia was not included since it was performed outside the theatre. For this reason, our results contrast with the current literature on robotic surgery ranging from 70 to 90 min [23,24,25,26], where OR time is usually intended from skin incision to wound closure. The difference between the two groups is probably related to the time necessary to prepare and drape the robot, placing and removing the tracking pins, positioning of the camera, acquisition of the bony landmarks, and the intraoperative planning. However, as it is shown in the graph (Fig. 1), in some cases, the surgical procedure lasted 95 min as it was for the majority of the navigated TKAs suggesting that with a trained surgical team, it is possible to reduce remarkably the time of the additional steps required for the robotic technique. In addition, it is worth pointing out that in this study the surgical team was not always the same, enhancing the fact that an untrained team may slow down the procedure. Although, the surgical time registered were in line with what reported in the literature especially with the addition of newer techniques aiming to increase the accuracy and precision of the surgery as reported by Shah et al. [27].
A significant difference in total range of motion (119.4° vs. 107.1°; p < 0.0001) was detected as well as a mean delta improvement from preoperative baseline condition between RTKA and NTKA (23.02° vs. 11.36°; p < 0.0001). In addition, despite the detected differences on KSS and the overall KOOS being not significant, a significant improvement in the “pain” subsection of the KOOS in the RTKA group was reported compared to the NTKA (p = 0.0283). Similarly, Marchand et al. [28] reported the clinical outcomes of 53 RTKA compared to 53 manual TKA and noted that the RTKA cohort had significantly improved mean Western Ontario and McMaster Universities (WOMAC) total (p = 0.03) and physical function scores (p = 0.02) when compared with the manual cohort. Furthermore, the authors reported that the mean pain score was also lower in the RTKA group, however, without reaching statistical significance (p = 0.06). Moreover, in the recent meta-analysis by Agarwal et al. [10], the authors reported a significant clinical improvement using the Hospital for Special Surgery (HSS) and WOMAC scores when the robotic-assisted technique was used compared to the conventional one. However, none of the studies included referred to robotic devices as the ROSA Knee System, but all of them were CT-based instead. Nevertheless, despite several studies included in the review reported significant improvement in pain perception and ROM, it was unclear to the authors whether the differences in PROMs resulted in a clinically significant differences in pain reduction and improved function between robotic and conventional arthroplasty techniques. Conversely, Held et al. [29] compared the outcomes of 111 imageless RTKA with 110 conventional TKA at 12- and 24-month follow-up and reported no significant differences between the two groups in terms of PROMs and total ROM. However, the authors used a different handheld imageless robotic device (NAVIO™, Smith & Nephew, Memphis, US). The difference detected in this study may be related to a personalized component positioning and joint line restoration of the robotically assisted technique, however, larger prospective randomized investigations are necessary to eventually confirm these preliminary results on imageless RTKA.
This study reported no significant differences in postoperative alignment of the knee between the two groups (HKA angle), however, the overall number of outliers was higher in the RTKA group compared to the NTKA (30% vs 17%). The proportion of outliers of the NTKA group is in line with what currently reported in the literature ranging from 5 to 20% [14, 23, 26, 30,31,32,33]. However, the number of outliers in the RTKA group contrast with what has been lately reported on robotic TKA, even though most of the studies that analyzed postoperative alignment used a different robotic device and were aiming for a MA [10, 14, 23]. This could be explained considering that the surgical technique of iAssist aims to a pure MA technique, while the ROSA-assisted knee is based on the concept of personalized TKA recreating the patient anatomy and restoring the joint line orientation allowing a more precise placement of the femoral and tibial component in the coronal plane. Moreover, the targeted alignment with ROSA in mild-to-moderate varus knees was an undercorrection to 2° varus. The MPTA and LDFA were accurate with the targeted angles, with a mean deviation of 0.8° and 1.3°, respectively. The standard deviations revealed very small distribution widths of ± 0.6° and ± 0.9°, respectively. The HKA was also precise to within 1.5° ± 1.1°, and the TSA within an error of 0.9° ± 0.7°. These results are consistent with the findings reported in the current literature for robotic-assisted TKA [23, 24, 26, 34,35,36,37], despite the limited data available on imageless robotic systems. However, further studies are necessary to clarify if this personalized alignment is responsible for the improved clinical outcomes and ROM and if there is a significative difference for the component placements in all three planes.
Regarding complications, one reoperation for acute infection was reported (2%) and two cases of wound complications not related to pin sites (4%) in the RTKA group, in line with what reported in the current literature regarding similar robotic devices with a mean complication rate between 0 and 5%, including NAVIO® Surgical System (Smith and Nephew, Memphis, USA) [23, 26, 38] and MAKO robotic system (Stryker, Mahwah, NJ) [25, 39]. No cases of pin sites infections and pin related fractures were reported, and no significant difference was reported between the two groups regarding surgical site infection. According to the current literature, periprosthetic knee fracture pins related have been reported with a rate ranging from 0.06 to 4.8% in case of robotic-assisted UKA [29], and 0.16% in computer-assisted TKA [40]. The authors reported that a transcortical pin trajectory, large pin diameter (> 4 mm), diaphyseal fixation, multiple placement attempts, and the use of non-self-drilling, non-self-tapping pins were the most commonly reported risk factors. In addition, it has been reported an incidence of pin site superficial infection between 0.47 and 0.6% [41, 42]. Despite the promising results, it needs to be mentioned that the two cohorts analyzed were formed by a small number of patients suggesting that such rare complication may not be clearly detected in so small groups. Considering that each robotic device has specific pins and trackers with clear differences among them in terms of size and distance between the pins, we believe that further studies focused on only one robotic device with larger cohorts are necessary to clearly establish the incidence of pin related complications. However, according to the results of this study, the use of ROSA knee system was not associated with increased incidence of complications compared to other robotic devices currently available suggesting its safeness and reliability.
This study has several limitations. First, as a retrospective study, although patients were prospectively followed, its nature makes it susceptible to selection and detection bias since patient were not randomized and postoperative evaluation was not blinded. Second, the study has a relatively short follow-up, and these patients, therefore, still need to be followed to evaluate survivorship, revision rates, and patient satisfaction. However, a recent study reported no different outcomes at 12- and 24-month follow-up after TKA suggesting that although the longer follow-up periods are clearly necessary, there may not be of additional value in collecting short-term outcomes in routine practice at both 1 and 2 years [43]. Third, the clinical scores used to evaluate the postoperative outcomes are not free from controversies. In fact, despite the KOOS scale has been defined more effective than the KSS-F scale in measuring patient outcomes following TKA allowing the use of a smaller cohort to show a significant difference and being more sensitive in measuring improvements after an intervention, the “pain” subsection is characterized by a higher “ceiling effect” that decreases validity [44]. Fourth, considering the nature of the personalized approach allowed by the ROSA knee system where the final alignment is chosen by the surgeon according to its personal preferences and experience, the fact that the surgical procedures have been performed by different surgeons, despite their experience, may lead to a potential performance bias. However, considering the recent diffusion of this innovative device and the lack of studies currently available, we had to include the patients of the two surgeons to have a sufficient group with minimum 12-month follow-up.
Conclusion
In conclusion, at minimum 12-month follow-up, the imageless ROSA knee system proved comparable safety with NTKA including similar length of stay, overall alignment, complication, reoperation, and revision rates despite the longer operative time. In addition, the robotically assisted technique showed higher overall ROM and improvement from preoperative condition with increased PROMs compared to the NTKA group. However, high-quality randomized control trials are necessary to support these preliminary findings and support the broad adoption of this technology.
References
Bourne RB, Chesworth BM, Davis AM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63. https://doi.org/10.1007/s11999-009-1119-9
Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC (2009) Causes and predictors of patient’s dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty 24:263–271. https://doi.org/10.1016/j.arth.2007.11.005
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW (2017) Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty 32:3854–3860. https://doi.org/10.1016/j.arth.2017.07.021
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 2006:35–43. https://doi.org/10.1097/01.blo.0000238825.63648.1e
Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ et al (2019) Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 32(3):239–250. https://doi.org/10.1055/s-0038-1641729
Parratte S, Price AJ, Jeys LM, Jackson WF, Clarke HD (2019) Accuracy of a new robotically assisted technique for total knee arthroplasty: a cadaveric study. J Arthroplasty 34(11):2799–2803. https://doi.org/10.1016/j.arth.2019.06.040
Lombardi AV, Berend KR, Adams JB (2014) Why knee replacements fail in 2013: patient, surgeon, or implant? Bone Joint J. 96-B(11 Suppl A):101–104. https://doi.org/10.1302/0301-620X.96B11.34350
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153. https://doi.org/10.1097/00003086-199811000-00021
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD (2007) Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136. https://doi.org/10.1097/BLO.0b013e3180332d97
Agarwal N, To K, McDonnell S, Khan W (2020) Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 35(11):3393-3409.e2. https://doi.org/10.1016/j.arth.2020.03.005
Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T et al (2020) Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg 33(7):685–690. https://doi.org/10.1055/s-0039-1684014
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL et al (2017) Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg 30(9):849–853. https://doi.org/10.1055/s-0037-1607450
Batailler C, Fernandez A, Swan J, Servien E, Haddad FS, Catani F et al (2020) MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06283-z
Bollars P, Boeckxstaens A, Mievis J, Kalaai S, Schotanus MGM, Janssen D (2020) Preliminary experience with an image-free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur J Orthop Surg Traumatol 30(4):723–729. https://doi.org/10.1007/s00590-020-02624-3
Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P (2020) Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06353-2
Scuderi GR, Fallaha M, Masse V, Lavigne P, Amiot LP, Berthiaume MJ (2014) Total knee arthroplasty with a novel navigation system within the surgical field. Orthop Clin North Am 45(2):167–173. https://doi.org/10.1016/j.ocl.2013.11.002
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(3):430–436
Ewald FC (1989) Roentgenographic evaluation and scoring system. Clin Orthop Related Res 248:9–12
Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR (2015) Development of a modern Knee Society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty 30(12):2311–2314. https://doi.org/10.1016/j.arth.2015.05.049
Batailler C, Hannouche D, Benazzo F, Parratte S (2021) Concepts and techniques of a new robotically assisted technique for total knee arthroplasty: the ROSA knee system. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04048-y
Rossi SMP, Sangaletti R, Perticarini L, Terragnoli F, Benazzo F (2022) High accuracy of a new robotically assisted technique for total knee arthroplasty: an in vivo study. Knee Surg Sports Traumatol Arthrosc 4:1–9. https://doi.org/10.1007/s00167-021-06800-8
Savov P, Tuecking LR, Windhagen H, Ehmig J, Ettinger M (2021) Imageless robotic handpiece-assisted total knee arthroplasty: a learning curve analysis of surgical time and alignment accuracy. Arch Orthop Trauma Surg 141(12):2119–2128. https://doi.org/10.1007/s00402-021-04036-2
Onggo JR, Onggo JD, De Steiger R, Hau R (2020) Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: a meta-analysis and systematic review. Arch Orthop Trauma Surg 140(10):1533–1549. https://doi.org/10.1007/s00402-020-03512-5
King CA, Jordan M, Bradley AT, Wlodarski C, Tauchen A, Puri L (2022) Transitioning a practice to robotic total knee arthroplasty is correlated with favorable short-term clinical outcomes-a single surgeon experience. J Knee Surg 35(1):78–82. https://doi.org/10.1055/s-0040-1712984
Thiengwittayaporn S, Uthaitas P, Senwiruch C, Hongku N, Tunyasuwanakul R (2021) Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. Int Orthop 45(11):2851–2858. https://doi.org/10.1007/s00264-021-05179-y
Shah RP, Lauthen D, Geller JA, Cooper HJ (2019) Average operative times for 1,313 primary total hip arthroplasty and 1,300 primary total knee arthroplasty over 39 months are roughly equal to medicare attributed operative times. J Arthroplasty 34(8):1553–1556. https://doi.org/10.1016/j.arth.2019.04.053
Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K et al (2019) One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg 32(11):1063–1068. https://doi.org/10.1055/s-0039-1683977
Held MB, Gazgalis A, Neuwirth AL, Shah RP, Cooper HJ, Geller JA (2021) Imageless robotic-assisted total knee arthroplasty leads to similar 24-month WOMAC scores as compared to conventional total knee arthroplasty: a retrospective cohort study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06599-4
Kazarian GS, Lawrie CM, Barrack TN, Donaldson MJ, Miller GM, Haddad FS et al (2019) The impact of surgeon volume and training status on implant alignment in total knee arthroplasty. J Bone Joint Surg Am 101(19):1713–1723. https://doi.org/10.2106/JBJS.18.01205
Pauzenberger L, Munz M, Brandl G, Frank JK, Heuberer PR, Laky B et al (2019) Patient-specific instrumentation improved three-dimensional accuracy in total knee arthroplasty: a comparative radiographic analysis of 1257 total knee arthroplasties. J Orthop Surg Res 14(1):437. https://doi.org/10.1186/s13018-019-1465-6
Yang HY, Seon JK, Shin YJ, Lim HA, Song EK (2017) Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg 9(2):169–176. https://doi.org/10.4055/cios.2017.9.2.169
Shah SM, Sciberras NC, Allen DJ, Picard F (2019) Technical and surgical causes of outliers after computer navigated total knee arthroplasty [published correction appears in J Orhop 2020 Dec 14;23:274. J Orthop 18:171–176. https://doi.org/10.1016/j.jor.2019.10.016
Mannan A, Vun J, Lodge C, Eyre-Brook A, Jones S (2018) Increased precision of coronal plane outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. Surgeon 16(4):237–244. https://doi.org/10.1016/j.surge.2017.12.003
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Higuera CA, Stearns KL et al (2018) Coronal correction for severe deformity using robotic-assisted total knee arthroplasty. J Knee Surg 31(1):2–5. https://doi.org/10.1055/s-0037-1608840
Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS (2019) Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev. 4(10):611–617. https://doi.org/10.1302/2058-5241.4.190022
Elliott J, Shatrov J, Fritsch B, Parker D (2021) Robotic-assisted knee arthroplasty: an evolution in progress. A concise review of the available systems and the data supporting them. Arch Orthop Trauma Surg 141(12):2099–2117. https://doi.org/10.1007/s00402-021-04134-1
Collins K, Agius PA, Fraval A, Petterwood J (2021) Initial experience with the NAVIO robotic-assisted total knee replacement-coronal alignment accuracy and the learning curve [published online ahead of print, 2021 Jan 28]. J Knee Surg. https://doi.org/10.1055/s-0040-1722693
Batailler C, Fernandez A, Swan J, Servien E, Haddad FS, Catani F et al (2021) MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 29(11):3585–3598. https://doi.org/10.1007/s00167-020-06283-z
Smith TJ, Siddiqi A, Forte SA, Judice A, Sculco PK, Vigdorchik JM et al (2021) Periprosthetic fractures through tracking pin sites following computer navigated and robotic total and unicompartmental knee arthroplasty: a systematic review. JBJS Rev. 9(1):e2000091. https://doi.org/10.2106/JBJS.RVW.20.00091
Brown MJ, Matthews JR, Bayers-Thering MT, Phillips MJ, Krackow KA (2017) Low incidence of postoperative complications with navigated total knee arthroplasty. J Arthroplasty 32(7):2120–2126. https://doi.org/10.1016/j.arth.2017.01.045
Kamara E, Berliner ZP, Hepinstall MS, Cooper HJ (2017) Pin site complications associated with computer-assisted navigation in hip and knee arthroplasty. J Arthroplasty 32(9):2842–2846. https://doi.org/10.1016/j.arth.2017.03.073
Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP (2018) No Difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty 33(7):2322–2329. https://doi.org/10.1016/j.arth.2018.02.056
Steinhoff AK, Bugbee WD (2016) Knee injury and osteoarthritis outcome score has higher responsiveness and lower ceiling effect than knee society function score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(8):2627–2633. https://doi.org/10.1007/s00167-014-3433-3
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
SMPR and FB designed the study. FB FT and SMPR performed the surgeries. FM, RS and LL collected the data. FM drafted the manuscript. SMPR critically revised it. FB gave final approval before submission. This Manuscript is original and not published elsewhere.
Corresponding author
Ethics declarations
Conflict of interest
Prof. Francesco Benazzo declares a teaching contract with the manufacturer (Zimmer Biomet); Dr. Fabio Mancino received a research grant from the manufacturer (Zimmer Biomet); The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript; All other authors declare no conflict of interest related to the present study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required. All patients signed an informed consent for the surgical procedure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mancino, F., Rossi, S.M.P., Sangaletti, R. et al. A new robotically assisted technique can improve outcomes of total knee arthroplasty comparing to an imageless navigation system. Arch Orthop Trauma Surg 143, 2701–2711 (2023). https://doi.org/10.1007/s00402-022-04560-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04560-9