Abstract
Introduction
To evaluate the long-term survival of unicompartmental knee arthroplasty (UKA) in the Asian population and assess differences in clinical outcomes between mobile- and fixed-bearing UKA.
Materials and methods
Among 111 cases of UKA that were performed by 1 surgeon from January 2002 to December 2009, we retrospectively reviewed 96 cases (36 mobile-bearing, 62 fixed-bearing) for this study. We examined cause of revision or failure, type of reoperation/revision, and duration from the surgery date to the revision upon reviewing the medical record. Survival analysis was conducted using the Kaplan–Meier method. Functional outcomes were evaluated based on range of motion and patient-reported outcome (PRO) measures (Knee Injury and Osteoarthritis Outcome Score) for cases with at least 8 years of follow-up (average, 10.2 years).
Results
Overall, the 10-year survival was 88% [95% confidence interval (CI) 0.81–0.95], and the estimated mean survival time was 13.4 years (95% CI 12.5–14.2). In a comparison of survival between the mobile- and fixed-bearing groups, the former had a 10-year survival of 85% (95% CI, 0.72–0.97) and an estimated mean survival time of 13.5 years (95% CI 12.2–14.7) and the latter had a 10-year survival of 90% (95% CI 0.82–0.99) and an estimated mean survival time of 13.4 years (95% CI 12.3–14.4). Thus, there was no significant difference in survival between the two groups (log-rank test, p = 0.718). In addition, no significant difference in functional outcomes was observed between the two groups (p > 0.05 for all).
Conclusions
UKA performed in the Asian population showed a relatively good functional outcome and survival rate at an average 10-year follow-up. No difference in survival and PROs was observed according to the bearing type. Although the present study demonstrated a good survival rate, similar to that in other Western studies, further studies investigating the impact of the Asian lifestyle on the long-term survival of UKA is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous studies have reported long-term clinical results of unicompartmental knee arthroplasty (UKA). Despite the slight difference in results among the studies, the 10–15-year survival rate is reported to be as high as 90% [1,2,3,4,5,6,7]. Based on these results, UKA is considered a useful treatment option in cases of osteoarthritis limited to a single compartment in the knee joint. UKA is divided into mobile- and fixed-bearing types according to the design of the polyethylene insert [8]. As with total knee arthroplasty (TKA), many studies have investigated the differences in clinical outcomes between the two designs in UKA. Although most previous studies reported good clinical outcomes for both designs, whether survival differs according to the design is still controversial [1, 9, 10].
More evidence is required to prove the usability of UKA as a treatment method for osteoarthritis limited to a single compartment, because most of the previously mentioned long-term follow-up studies on UKA reported clinical outcomes for the Western population where only one bearing type was used. In addition, there are virtually no long-term studies comparing the clinical outcomes between mobile- and fixed-bearing UKA as these are mostly short- or mid-term studies [11,12,13]. We believe it is necessary to evaluate the long-term results of UKA using a sample including diverse races and nationalities. Asians frequently perform high-flexion activities in daily life, such as sitting cross-legged, kneeling, or squatting [14,15,16], which could affect survival or clinical outcomes in the long-term follow-up of UKA [17,18,19,20]. Hence, it is necessary to determine whether UKA performed in the Asian population shows results similar to those in the Western population.
The purpose of this study was to evaluate the long-term survival of UKA in the Asian population and assess the differences in clinical outcomes between mobile- and fixed-bearing UKA. We assumed that UKA performed in the Asian population would have good long-term survival, similar to that reported among the Western population, and that the clinical outcome would not differ according to the bearing design.
Materials and methods
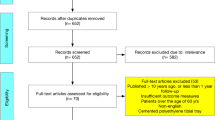
This study was approved by our institutional review board. From January 2002 to December 2009, a total of 111 cases of medial UKA (44 mobile bearings, 67 fixed bearings) were performed by 1 surgeon in our institution. In this study, we included patients with a minimum follow-up of 8 years after UKA and those who underwent revision surgery due to implant-related problems regardless of the follow-up duration. Because this study assessed the long-term survival and clinical outcomes, patients with a follow-up duration < 8 years were excluded from the sample.
Two patients died due to medical problems prior to reaching the minimum follow-up (5 and 6 years after the surgery). In total, 96 UKA cases (86.5%) (36 mobile bearings, 60 fixed bearings) were included in the study. 13 patients were lost to follow-up (3.5–7.5 years after surgery). We attempted to contact the 13 patients, but could not reach them.
UKA was performed in patients with Kellgren–Lawrence [21] grade 3 or 4 osteoarthritis limited to a single compartment in the knee joint, or in patients with osteonecrosis. Contraindications for UKA were as follows: inflammatory arthritis, such as rheumatoid arthritis, osteoarthritis in multiple compartments, ligamentous instability, angular deformity over 10°, severe obesity, and flexion contracture over 10° or range of motion below 90° [20]. There was no absolute standard to determine the type of implant to be used. Implant type was randomly selected by the surgeon, without considering patient demographics or other factors such as osteoarthritis severity. No case required conversion to TKA during the performance of UKA.
Surgical procedures were followed as per company’s brochure. The Oxford (Biomet, Warsaw, IN, USA) and Miller-Galante (Zimmer Inc., Warsaw, IN, USA) systems were used for mobile- and fixed-bearing UKA, respectively. The patients began range-of-motion exercises using continuous passive motion immediately after their surgery (or 1 day after surgery). Weight-bearing with a crutch or walker was permitted within a tolerable range. Patients were allowed full weight-bearing without a walker or crutch from 1 week after the surgery.
Weight-bearing whole-leg anteroposterior (AP), standing knee AP, knee lateral, Rosenberg, and Merchant views were used for the radiologic assessments. Lower extremity alignment and existence of implant loosening were examined using the radiographs taken prior to surgery and at the final follow-up. Lower extremity alignment was evaluated using the mechanical femorotibial angle, which was defined as an angle formed by a line connecting the center of the femoral head and the center of the knee joint with a line connecting the center of the knee and the center of the ankle on the weight-bearing whole leg AP view [22]. Loosening was defined as the change of implant position in serially obtained radiographs. Radiolucency thickness > 2 mm that was progressive and poorly defined was considered an indication of aseptic loosening [11, 23].
We assessed the follow-up duration, types of complications, types of reoperation/revision, and duration from the surgery date to the revision upon reviewing the medical records. Kaplan–Meier survival curve analysis was used for survival analysis where the endpoint was defined as revision for any reason. Survival was evaluated using the total number of cases (96 cases). In addition, we evaluated whether there was a survival difference between the mobile- (36 cases) and fixed-bearing groups (60 cases) using the log-rank test.
We evaluated the clinical outcomes of 83 cases (31 mobile bearings, 52 fixed bearings) with at least 8 years of follow-up using range of motion (ROM) and patient-reported outcome measures (PROs). The average follow-up duration was 10.2 years (range 8–15 years). The Knee Injury and Osteoarthritis Outcome Score (KOOS) [24] was used to evaluate the clinical results based on PROs using data obtained prior to the surgery and at the final follow-up.
We used IBM SPSS Statistics, version 25.0 (IBM Corp., Armonk, NY, USA) for statistical analysis. The significance level was set at p < 0.05. An independent t test was used to compare the PROs (KOOS) between the mobile- and fixed-bearing groups.
Results
Table 1 illustrates the overall demographics. There was no significant difference in pre- and postoperative demographic data and radiologic results between the mobile- and fixed-bearing groups. Overall, the 10-year survival was 88% (95% CI 0.81–0.95) and the estimated mean survival time was 13.4 years (95% CI 12.5–14.2; Fig. 1). A survival comparison between the mobile- and fixed-bearing groups (Fig. 2) showed that the mobile-bearing group had a 10-year survival of 85% (95% CI 0.72–0.97) and an estimated mean survival time of 13.5 years (95% CI 12.2–14.7). The fixed-bearing group had a 10-year survival of 90% (95% CI 0.82–0.99) and an estimated mean survival time of 13.4 years (95% CI 12.3–14.4). Hence, no significant difference in survival was seen between the two groups (log-rank test, p = 0.718).
Kaplan–Meier survivorship curve for mobile-bearing group and fixed-bearing group. Considering revision for any reason as the end point, the 10-year survival rate of the mobile-bearing group was 85% (95% CI 0.72–0.97), and the 10-year survival rate of the fixed-bearing group was 90% (95% CI 0.82–0.99). No significant difference in survival was seen between the two groups
In total, revision was performed in 13 cases. Five cases in the mobile-bearing group underwent revision (13.9%) due to wear of the polyethylene insert (2 cases), dislocation of the insert (2 cases), and aseptic loosening (1 case). Eight cases in the fixed-bearing group underwent revision due to aseptic loosening (2 cases), wear of the polyethylene insert (2 cases), osteoarthritis progression in the lateral compartment (2 cases), and periprosthetic joint infection (2 cases). Table 2 summarizes the specific details of the revision in each group.
Average ROM increased from 125.3° ± 7.4° before the surgery to 132.9° ± 7.3° after the surgery (p < 0.001), and all KOOS subscales demonstrated a statistically significant improvement (p < 0.001 for all). However, no significant difference was observed between the two groups in a comparison of preoperative and final follow-up ROM and PROs (KOOS score) (all subscales, p > 0.05; Table 3).
Discussion
In this study, the clinical outcomes and survival rates of UKA performed in the Asian population demonstrated good results at the 10-year follow-up. In addition, no significant difference was observed between mobile and fixed bearings. The current study showed good long-term survival, similar to that in previous studies of UKA performed in the Western population.
UKA has many advantages including faster recovery and improved range of motion [25,26,27]. The recent increased popularity of UKA is associated with improvements in implant design, surgical technique, and survival [28,29,30,31]. Numerous studies have reported excellent outcomes for UKA. The 10–15-year survival following UKA has been reported to be ≥ 90% [1,2,3,4,5,6]. However, existing studies on long-term survival of UKA have limitations—they have included mainly Western subjects. The major failure modes of UKA include progression of osteoarthritis, aseptic loosening, polyethylene wear, or polyethylene dislocation, etc. Several studies have investigated the difference in failure mode according to the time to failure of UKA due to complications or the design of the polyethylene insert [25, 32]. Asians frequently perform high-flexion activities in daily life, such as sitting cross-legged, kneeling, or squatting [14, 15, 30], whether such lifestyle activities affect the survival and long-term clinical results of UKA or TKA remains unclarified. Hence, long-term follow-up results of UKA or TKA on knee joints should be evaluated using subjects from more diverse nationalities, ethnicities, and races [30, 33]. Although Kim et al. [34] reported long-term follow-up results for UKA in Asian patients, their study was limited to those aged < 60 years using only the mobile-bearing type.
Kim et al. [34] reported a 10-year survival rate of 89.3% in a long-term follow-up study (average follow-up of 12.1 years) of 106 cases receiving Oxford UKAs. Xue et al. [30] reported the clinical results of UKA (mean follow-up of 6.2 years) in a Chinese population sample. In their study, 13 (1.88%) of 708 cases of medial Oxford UKAs underwent revision. The study reported a 5-year cumulative survival rate of 98.8% and a 10-year survival rate of 94.3%. In both studies, which reported mid- and long-term results of UKA among the Asian population, PROs and ROM were significantly improved after the surgery. Although the studies reported good clinical outcomes and survival rates for UKA among the Asian population, they have limitations that they involved a single type of UKA. In addition, Xue et al. [30] reported mid-term follow-up results, and the study of Kim et al. [34] was restricted to patients aged < 60 years.
Evaluation of the total UKA cases in the present study demonstrated a 10-year survival of 89.4% and a 14-year survival of 80.8%. The survival rate in the present study is similar to that in other studies at 10–15 years following UKA in a Western population or Asian population [1,2,3,4,5, 34]. Few studies have reported the correlation between high flexion and polyethylene wear or loosening in TKA. Several authors have reported that high flexion can affect survival, while others have argued that the two are not related, and this issue is still controversial [17,18,19,20, 35,36,37]. However, some studies have reported the correlation between a high flexion-related lifestyle and survival in UKA [33]. It is difficult to directly compare the difference in UKA results according to race or lifestyle. We can only indirectly evaluate them by referring to the UKA survival rates reported in other countries or cultural areas. These study results are meaningful as we demonstrated 10-year survival rates as high as 90% in Asian subjects with UKA who frequently perform high-flexion activities.
Mobile-bearing design has theoretical advantages over fixed-bearing design. Mobile-bearing type implant has congruent bearing with lower contact stresses and polyethylene wear rates [38,39,40]. However, which bearing type provides better clinical outcome in UKA remains to be clarified. In this study, no significant difference in survival or PROs was observed between the mobile- and fixed-bearing groups. Due to the small number of cases receiving revision, we could not conduct statistical analysis on the difference in the cause of failure between the two groups. Focusing only on implant-related issues rather than periprosthetic joint infection, loosening and polyethylene wear were commonly observed in both the mobile- and fixed bearing-groups. The occurrence timing of these complications was also similar in the two groups. Bearing dislocation and progression of osteoarthritis in the lateral compartment are among the main complications related to the survival following UKA. Ro et al. [33] reported that these two complications show different tendencies between Asian and Western patients. In a meta-analysis on complications following mobile-bearing UKA, they reported that reoperation due to osteoarthritis progression in the lateral compartment is frequently observed in the Western population, while reoperation due to bearing dislocation is frequently observed in the Asian population. In the current study, no case in the mobile-bearing group received revision due to the progression of osteoarthritis in the lateral compartment, although there were two cases of bearing dislocation in this group. The progression of osteoarthritis in the lateral compartment was observed only in the fixed-bearing group. Due to the number of cases included in this study, it is unclear whether these observations in our study are characterized by the Asian population. Further follow-up is necessary in the future.
This study has several limitations. First, only a small number of cases were included in this study. Second, this study examined case series that were implemented by one experienced surgeon in one institution. Hence, it is difficult to generalize the outcomes of this study to all Asian patients. However, our study is meaningful as few studies have examined the long-term results of UKA among the Asian population. Third, although gender was not included in the surgical indication, most recipients of UKA were female. Fourth, this study potentially has selection bias because the patients were not randomly allocated when choosing the types of bearings in UKA.
Conclusions
UKA performed in the Asian population demonstrated a relatively good functional outcome and survival rate at the average 10-year follow-up. No difference in survival or PROs was observed according to the bearing type. Although the survival rate in the current study was good, similar to rates in other studies evaluating a Western population, further studies are required to investigate the impact of an Asian lifestyle on the long-term survival of patients undergoing UKA.
References
Murray DW, Goodfellow JW, O'Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Jt Surg Br 80(6):983–989
Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Jt Surg Br 83(2):191–194
Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO (2005) Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Jt Surg Am 87(5):999–1006
Cartier P, Sanouiller JL, Grelsamer RP (1996) Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty 11(7):782–788
Foran JR, Brown NM, Della Valle CJ, Berger RA, Galante JO (2013) Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res 471(1):102–108
Saragaglia D, Bevand A, Refaie R, Rubens-Duval B, Pailhe R (2018) Results with nine years mean follow up on one hundred and three KAPS(R) uni knee arthroplasties: eighty six medial and seventeen lateral. Int Orthop 42(5):1061–1066
Scott CEH, Wade FA, MacDonald D, Nutton RW (2018) Ten-year survival and patient-reported outcomes of a medial unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Arch Orthop Trauma Surg 138(5):719–729
Ozcan C, Simsek ME, Tahta M, Akkaya M, Gursoy S, Bozkurt M (2018) Fixed-bearing unicompartmental knee arthroplasty tolerates higher variance in tibial implant rotation than mobile-bearing designs. Arch Orthop Trauma Surg 138(10):1463–1469
Emerson RH Jr, Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V (2008) Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop 79(4):499–507
Parratte S, Pauly V, Aubaniac JM, Argenson JN (2012) No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res 470(1):61–68
Ko YB, Gujarathi MR, Oh KJ (2015) Outcome of unicompartmental knee arthroplasty: a systematic review of comparative studies between fixed and mobile bearings focusing on complications. Knee Surg Relat Res 27(3):141–148
Cho WJ, Kim JM, Kim WK, Kim DE, Kim NK, Bin SI (2018) Mobile-bearing unicompartmental knee arthroplasty in old-aged patients demonstrates superior short-term clinical outcomes to open-wedge high tibial osteotomy in middle-aged patients with advanced isolated medial osteoarthritis. Int Orthop 42(10):2357–2363
Ha CW, Park YB, Song YS, Kim JH, Park YG (2016) Increased range of motion is important for functional outcome and satisfaction after total knee arthroplasty in Asian patients. J Arthroplasty 31(6):1199–1203
Ohno H, Murata M, Ozu S, Matsuoka N, Kawamura H, Iida H (2016) Midterm outcomes of high-flexion total knee arthroplasty on Japanese lifestyle. Acta Orthop Traumatol Turc 50(5):527–532
Watanabe T, Muneta T, Koga H, Horie M, Nakamura T, Otabe K, Nakagawa Y, Katakura M, Sekiya I (2016) In-vivo kinematics of high-flex posterior-stabilized total knee prosthesis designed for Asian populations. Int Orthop 40(11):2295–2302
Paterson NR, Teeter MG, MacDonald SJ, McCalden RW, Naudie DD (2013) The 2012 Mark Coventry award: a retrieval analysis of high flexion versus posterior-stabilized tibial inserts. Clin Orthop Relat Res 471(1):56–63
Han HS, Kang SB, Yoon KS (2007) High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Jt Surg Br 89(11):1457–1461
Namba RS, Inacio MC, Cafri G (2014) Increased risk of revision for high flexion total knee replacement with thicker tibial liners. Bone Jt J 96-B(2):217–223
Cho KY, Kim KI, Song SJ, Kim KJ (2018) Intentionally increased flexion angle of the femoral component in mobile bearing unicompartmental knee arthroplasty. Knee Surg Relat Res 30(1):23–27
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kim CW, Seo SS, Lee CR, Gwak HC, Kim JH, Jung SG (2017) Factors affecting articular cartilage repair after open-wedge high tibial osteotomy. Knee 24(5):1099–1107
Tibrewal SB, Grant KA, Goodfellow JW (1984) The radiolucent line beneath the tibial components of the Oxford meniscal knee. J Bone Jt Surg Br 66(4):523–528
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Ernstbrunner L, Imam MA, Andronic O, Perz T, Wieser K, Fucentese SF (2018) Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop 42(8):1827–1833
Bin Abd Razak HR, Acharyya S, Tan SM, Pang HN, Tay KD, Chia SL, Lo NN, Yeo SJ (2017) Predictors of midterm outcomes after medial unicompartmental knee arthroplasty in Asians. Clin Orthop Surg 9(4):432–438
Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S (2018) Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 138(12):1765–1771
Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S (2017) Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 41(11):2265–2271
Saragaglia D, Marques Da Silva B, Dijoux P, Cognault J, Gaillot J, Pailhe R (2017) Computerised navigation of unicondylar knee prostheses: from primary implantation to revision to total knee arthroplasty. Int Orthop 41(2):293–299
Xue H, Tu Y, Ma T, Wen T, Yang T, Cai M (2017) Up to twelve year follow-up of the Oxford phase three unicompartmental knee replacement in China: seven hundred and eight knees from an independent centre. Int Orthop 41(8):1571–1577
Riddle DL, Jiranek WA, McGlynn FJ (2008) Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty 23(3):408–412
van der List JP, Zuiderbaan HA, Pearle AD (2016) Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty 31(5):1016–1021
Ro KH, Heo JW, Lee DH (2018) Bearing dislocation and progression of osteoarthritis after mobile-bearing unicompartmental knee arthroplasty vary between asian and western patients: a meta-analysis. Clin Orthop Relat Res 476(5):946–960
Kim KT, Lee S, Lee JS, Kang MS, Koo KH (2018) Long-term clinical results of unicompartmental knee arthroplasty in patients younger than 60 years of age: minimum 10-year follow-up. Knee Surg Relat Res 30(1):28–33
Daines SB, Koch CN, Haas SB, Westrich GH, Wright TM (2017) Does achieving high flexion increase polyethylene damage in posterior-stabilized knees? A retrieval study. J Arthroplasty 32(1):274–279
Kim YH, Park JW, Kim JS (2012) High-flexion total knee arthroplasty: survivorship and prevalence of osteolysis: results after a minimum of ten years of follow-up. J Bone Jt Surg Am 94(15):1378–1384
Lee BS, Chung JW, Kim JM, Kim KA, Bin SI (2013) High-flexion prosthesis improves function of TKA in Asian patients without decreasing early survivorship. Clin Orthop Relat Res 471(5):1504–1511
Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty 17(8):1049–1054
Cheng T, Chen D, Zhu C, Pan X, Mao X, Guo Y, Zhang X (2013) Fixed- versus mobile-bearing unicondylar knee arthroplasty: are failure modes different? Knee Surg Sports Traumatol Arthrosc 21(11):2433–2441
Sathasivam S, Walker PS, Campbell PA, Rayner K (2001) The effect of contact area on wear in relation to fixed bearing and mobile bearing knee replacements. J Biomed Mater Res 58(3):282–290
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Informed consent
For this type of study formal consent is not required.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. This study was approved by the Institutional Review Board in our institution (Inje University Busan Paik Hospital, IRB No. 18-0059).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seo, SS., Kim, CW., Lee, CR. et al. Long-term outcomes of unicompartmental knee arthroplasty in patients requiring high flexion: an average 10-year follow-up study. Arch Orthop Trauma Surg 139, 1633–1639 (2019). https://doi.org/10.1007/s00402-019-03268-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03268-7