Abstract
Background
Tranexamic acid (TXA) is widely used in the orthopedic field and particularly in total knee arthroplasty (TKA). Its efficacy and safety in reducing the blood loss in TKA have been well-documented in the current literature. Little data regarding TKA without tourniquet and TXA exist. Our aim is to compare three different dosages of intravenous (IV) TXA in TKA without tourniquet.
Materials and methods
A total of 180 patients undergoing TKA for knee osteoarthritis were stratified in three equal groups. All surgeries were performed under spinal anesthesia, without tourniquet. Group A (60 patients) received 15 mg/kg of IV TXA given on induction, Group B (60 patients) received an additional dose of IV TXA (15 mg/kg) 3 h after incision and Group C (60 patients) received an additional (third) dose 3 h later (15 mg/kg). The measured outcomes were the change in hemoglobin (Hb) from pre-operatively to post-operatively, the amount of blood transfusion given (units), the functional and quality of life (QoL) and pain assessment based on their corresponding scoring system.
Results
Calculated blood loss, Hb decrease and transfusion rate were significantly lower in Group C (p value < 0.05). Additionally, patients that had been included in the three-dosage group benefited much more in terms of faster rehabilitation, better QoL, decreased post-operative pain, with no increase in complications.
Conclusion
According to our results, three doses of IV TXA have effectively and safely reduced blood loss and the need of allogeneic blood transfusion in patients undergoing TKA without tourniquet, with additional patients-related benefits.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) becomes increasingly widespread with an expected sixfold increase in the next few years [1]. Total knee arthroplasty (TKA) is an excellent procedure for patients with end-stage knee arthritis and thus has been characterized as a “revolution” regarding the care of these patients. A successful TKA offers remarkable benefits that result in painless knee movement and allow patients to regain most of their daily activities [2]. The need for allogenic blood transfusion (ABT) is of great importance in terms of post-operative complications. Although nowadays many pre-, peri- and post-operative methods have been adopted to minimize blood loss and the subsequent anemia, serious ABT-related complications such as viral infections, immunological reactions, graft vs host disease (GvHD) and the economic impact are being reported in the literature [3, 4].
Two commonly worldwide-used methods to reduce blood loss are the use of pneumatic tourniquet and the administration of tranexamic acid (TXA) [5, 6]. The safety and effectiveness of the tourniquet are debated by many studies and reviews [7,8,9,10]. Several complications such as skin blistering, increased muscle injury, nerve palsy, knee stiffness, thigh pain, deep vein thrombosis (DVT) and pulmonary embolism (PE) are being associated with the use of tourniquet [7, 11]. Besides the fact that no obvious difference is being reported in terms of total blood loss, tourniquet’s application seems to enhance the hyperfibrinolysis and increase the perioperative/post-operative blood loss [7, 12]. On the other hand, TXA’s safety and efficacy in TKA have been well described.
TXA is a synthetic analog of the amino acid lysine that produces its antifibrinolytic effect by inhibiting the activation of plasminogen to plasmin [13]. Numerous systematic reviews and meta-analyses have highlighted the significant decrease of the total blood loss after TKA without apparent increased risk of DVT/PE [14,15,16]. In particular, a recent well-designed meta-analysis concluded that both 1.5 g intra-articular TXA and 1 g IV TXA are effective in reducing total blood loss and post-operative hemoglobin drop without increasing complications of DVT or PE [17]. Nevertheless, the majority of the studies conclude that further research is required to find the ideal TXA dose.
In the current orthopedic department, TKA is routinely performed without tourniquet. We have previously reported the superior results of intravenous/topical TXA application in TKA without tourniquet [18]. Taking all these facts into account and based on the previous pharmacokinetic studies that highlight the half-life time of TXA in 2.5–3 h and the peak of fibrinolysis at 6 h post-operatively, we decided to take the next step and organize a prospective, randomized controlled study (RCT) to answer the following questions [19]: (1) are multiple doses of IV TXA able to further reduce the total blood loss/hemoglobin drop? (2) Are there any additional advantages of multiple IV TXA dosages in terms of function, quality of life and pain in the early and late post-operative period? (3) Is there any increase in complication rates using this regimen of post-operative IV TXA?
Materials and methods
Study design and randomization method
This study is a prospective, randomized, double-blinded, controlled trial approved by our institutional review board. 203 patients who underwent primary unilateral TKA (without tourniquet) at our orthopedic department from November 2015 to March 2017 were enrolled.
Inclusion criteria were osteoarthritis, primary unilateral TKA without tourniquet, at least 12-week follow-up and normal coagulation profile. Furthermore, the pre-operative deformity criteria were: (i) varus deformity less than 10°, (ii) lack of extension not more than 10\(^\circ , \text{and}\)(iii) flexion of at least 90\(^\circ\).
The exclusion criteria were: (1) uncontrolled medical diseases/comorbidities; (2) allergy and/or hypersensitivity to TXA; (3) a known history of thromboembolic disease, cardiovascular disease; (4) coronary or vascular stent placed within the past 12 months; (5) cerebral vascular disease (a history of stroke); (6) subarachnoid hemorrhage; (7) pre-operative coagulopathy [a platelet (PLT) count < 150,000/mm3 or an international normalized ratio greater than 1.5]; (8) pre-operative renal or hepatic dysfunction; (9) retinal vein or artery occlusion; (10) patients with anemia (< 12 g/dL for female, < 13 g/dL for male) [20, 21]. According to these criteria, 23 patients were excluded, and the remaining 180 patients were included in the analysis. Written informed consent was obtained before surgery from all participants.
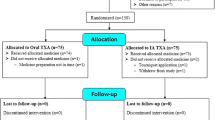
The remaining 180 patients were randomized using the technique of stratified randomization by minimization. The randomization was based on three parameters: age, gender, and body mass index (BMI). Patients were allocated into one of three TXA groups (Fig. 1): (1) Group A: 1 dose of IV TXA (15 mg/kg) in 100-ml normal saline, 10 min before incision, administered during the induction of the anesthesia, (2) Group B: 1 dose of IV TXA (15 mg/kg) in 100-ml normal saline, 10 min before incision and an additional dose of IV TXA (15 mg/kg) in 100-ml normal saline 3 h after skin incision, (3) Group C: 1 dose of IV TXA (15 mg/kg) in 100-ml normal saline, before incision and two additional doses of IV TXA (15 mg/kg) in 100-ml normal saline 3 and 6 h after skin incision, respectively. Two nurses that were not involved in the trial handed out the medications and implemented the post-operative protocol. The patients, surgeons, and data collector/analyst were blinded. Many trials and reviews/meta-analyses, further to our previous RCT, have proved the superiority/safety of a single IV TXA dose over the placebo control group and thus we did not recruit any control group [16, 18, 22,23,24]. Patients’ demographics, pre-operative lab tests and scoring results were comparable and are being demonstrated in Table 1.
Operative technique and post-operative protocol
All operations were performed by the same senior surgeon KK, under spinal anesthesia and prophylactic IV antibiotics were administered prior to skin incision. Standard midline incision followed by medial parapatellar capsular incision to expose knee joint was used in all patients. All procedures were performed using the same posterior cruciate retaining hybrid TKA with a cemented tibial and a press fit femoral component, without patellar resurfacing (Evolis® Total Knee System, Medacta, Switzerland). Intramedullary guide was used for femoral preparation and extramedullary guide for tibial preparation. Femoral medullary canal was filled by an autologous bone to further reduce the blood loss. Additionally, an intra-articular injection of 20 ml ropivacaine (0.2%) was administered in all patients, following our post-operative pain management protocol. Closure was performed carefully and a negative suction drain was applied. Regardless the group, the drain was clamped for 1 h and was opened at the recovery room or orthopedic department.
Pre-operative blood tests such as hemoglobin (Hb), hematocrit (Ht), platelet count (PLT) and biochemical analysis (sodium, potassium, glucose, urea, creatinine, SGOT, SGPT, ALP) were carried out. The same blood tests were performed on the 1st, 2nd, and 4th post-operative days. Apart from the above tests, patients’ (pre-operative) knee function, quality of life and pain were assessed using the knee society score (KSS)/functional knee society score (FKSS), the EuroQol (EQ-5D-5L) descriptive system and the visual analog scale (VAS) of pain, respectively [25,26,27,28]. KSS, FKSS, EQ-5D-5L, VAS pain tests were repeated at 6th week and 12th week post-operatively in routine outpatient visits. VAS pain test was further assessed in 2nd and 4th post-operative day.
Patients’ age, BMI, gender, physical health status classification [based on American Society of Anaesthesiologists (ASA)], surgery duration, units of ABT, hospitalization duration and complications were collected by a blinded data collector. In case of clinical suspicion (during their hospitalization and for 6 weeks post-operatively) of DVT or PE (according to Wells and Geneva score) patients were screened using Doppler ultrasound, d-dimers test and spiral computed tomography (CT) [29,30,31]. Last, on the 1st post-operative day and two times daily thereafter until discharge, all patients followed the same supervised physical therapy protocol including quadriceps strengthening, active/passive range of motion (ROM) and gait training.
Regarding the ABTs’ protocol, the transfusion trigger was Hb < 10 g/dl or any anemic symptoms (fatigue, dizziness, tachycardia, shortness of breath, pale skin) or anemia-related organ dysfunction. Patients received transfusion up to 4th post-op day. The same post-operative protocol was followed in all patients in terms of analgesia, chemical prophylaxis and anticoagulation regime with a low molecular heparin to prevent venous thromboembolism. Negative pressure drain was removed in the 2nd post-operative day and all patients used compression stockings to reduce the risk of DVT.
Outcome measurements
Hb decrease, total blood loss (TBL), PLT count, transfusion rate/quantity were assessed post-operatively during the inpatient hospital stay. Nadler’s formula was used to estimate patients’ blood volume and Bourke and Smith’s formula was used to calculate the change of blood volume [32, 33]. The TBL was calculated as the sum of the change in blood volume plus the volume of transfused blood. As post-operative level of Hb/Ht was considered the lowest measurement of Hb/Ht of the three post-operative lab tests on 1st, 2nd, and 4th post-operative day. Based on these values and taking into account the correlation of transfusion volume to Hb and Ht’s change, as Elzik et al. have stated in their study, we managed to calculate the real Hb drop [34]. The used calculation formulas are being described briefly in Fig. 2. Any complication and/or organ dysfunction was evaluated and measured directly in clinical follow-up for up to 12 weeks post-operatively.
KSS, FKSS, EuroQol and VAS pain were evaluated and compared between groups. Due to EQ-5D-5L scoring system’s peculiarity we managed to assess the changes in patient’s quality of life using the crosswalk index calculator provided by Euroqol group association [35, 36].
Statistical analysis
Sample size calculations were performed using PASS 2011 (NCSS, LLC, Kaysville, UT, USA) software. Sample size was calculated on the outcome of total Hb loss and on our preliminary data. To detect a difference of 1 g/dl, 47 patients were needed per group with a power of 0.90 and an alpha of 0.05. After a 10% drop-out rate was considered, the patients required for each group was 52 (at least). To exclude unexpected protocol violations, 60 patients per group were enrolled in this study.
Statistical Package for the Social Sciences (SPSS), version 23.0 (IBM) was used to analyze the data. The normality of quantitative variables was verified by Kolmogorov–Smirnov test. Differences of demographic and clinical characteristics between the three groups were assessed by one-way analysis of variance [ANOVA; age, BMI, ASA, surgery duration, length of stay (LOS), Hb, Ht, PLT, KSS, FKSS, EQ-5D-5L, VAS pain] and the Chi-square test (gender) were used. Between-group differences of blood loss/KSS/FKSS/EQ-5D-5L/VAS, transfusion rates, and used number of units were assessed by ANOVA, the Chi-square test, and Kruskal–Wallis test, respectively. Post hoc analysis was performed using Tukey’ test (blood loss) and Mann–Whitney U test (transfusion quantity). Odds ratios (ORs) with their 95% confidence intervals (CIs) were estimated by means of logistic regression models as the measure of association between transfusion and different groups of patients. All tests were two tailed and a p value < 0.05 was considered statistically significant.
Results
Patients’ demographics (Table 1)
All of the 180 patients that were included in this study were followed up to the 12th week and none was lost to follow-up. No statistically significant differences were noted in the demographic data and pre-operative blood tests between the three groups (Table 1). Additionally, all groups were comparable in terms of pre-operative functional test, quality of life and pain scale and not statistically significant (p > 0.05; Table 1).
Operation duration and LOS (Table 2)
The mean values of operative duration in TXA 1, TXA 2 and TXA 3 group were 48.48 ± 11.57 min, 49.13 ± 10.65 min and 46 ± 7.87 min, respectively, with no significant intergroup difference (p value 0.207). Furthermore, no statistically significant difference was noted in length of stay between the three groups (p value 0.207). Discharge day (based on our protocol) could not be earlier than the 5th post-operative day and consequently no difference was found in hospitalization’s duration. Rapid discharge was not included in our goals, as we aimed at collecting the post-operative blood results and test scores determined by our protocol.
Blood loss (Table 2; Fig. 3)
In terms of blood loss, the outcome can be summarized in Table 2. The mean values of post-operative Hb (based on the lowest post-operative values) in TXA 1, TXA 2 and TXA 3 groups were 11.02 ± 0.87, 11.18 ± 0.67, and 11.2 ± 0.86 mg/dL, respectively, with no significant intergroup difference (p value 0.335). Likewise, the mean values of post-operative Ht were 32.67 ± 2.22, 33.63 ± 2.28, and 33.67 ± 2.54% with no significant difference between the three groups (p value 0.112).
To calculate the real Hb drop we took into consideration two variables: the drop of Hb (according to blood results) and the amount of transfused red blood cells. Significant difference was noticed between the three groups (TXA 1: 3.83 mg/dl, TXA 2: 2.97 mg/dl and TXA 3: 2.33 mg/dl) with p value < 0.001. This statistically significant difference was found between both TXA 1 vs TXA 2, TXA 2 vs TXA 3 and TXA 1 vs TXA 3. Similar results were extracted regarding the mean TBL (TXA 1: 1281 ml, TXA 2: 1181 ml and TXA 3: 971 ml) with intergroup’s p value < 0.001 (Fig. 3). Pairwise comparisons and statistical analyses between the three groups also revealed significant differences.
Blood transfusions were required in 15%, 13% and 5% of TXA 1, TXA 2 and TXA 3 patients, respectively, with intergroup p value 0.002 (Fig. 3). Finally, Kruskal–Wallis test showed statistically significant differences in transfusion quantity between the three groups of patients (p value < 0.001). Post hoc analysis using Mann–Whitney test revealed that the number of units used in TXA 3 group was significantly lower compared to TXA 1 group (p value 0.004). No significant difference was noticed in TXA 1 vs TXA 2 (p value 0.27) and TXA 2 vs TXA 3 (p value 0.211) group.
Functional, QoL and pain assessment (Table 2; Figs. 4, 5)
To assess the function, we used both FKSS and KKSS. In FKSS aspect of view, TXA 3 group showed a statistically significant difference in 6th post-operative week compared to TXA 1 and TXA 2 (p values: < 0.001 and 0.002, respectively). Nevertheless, in 12th post-operative week, although TXA 3 group scored higher FKSS, there was no significant difference between the three groups (p value 0.106). The same results were obtained in terms of KKSS; in the 6th post-operative week, the TXA 3 vs TXA 1 and TXA 3 vs TXA 2 differences reached statistical significance (p value: 0.027 and 0.048, respectively). On the contrary, in the 12th post-operative week no difference approached significantly between the groups (p value 0.379).
The EQ-5D-5L questionnaire was used to assess the quality of patients’ life both pre- and post-operatively. Although no significant difference was noticed between the three groups in 6th post-operative week (p value 0.205), this difference reached statistical significance in the 12th post-operative week (p value < 0.001). It is noteworthy mentioning that the TXA 3 group benefited the most, with the TXA 2 group benefiting the second most.
According to our results, there were also favorable effects in decreasing post-operative pain in TXA 3 group compared to the other two groups not only at the immediate post-operative period (2nd and 4th post-operative days, with p value < 0.001) but also at the later periods too (6th and 12th post-operative weeks, with p value < 0.001 and 0.022, respectively).
Complications
Neither clinical DVT nor PE occurred in any patient. Additionally, no adverse effects such as pale skin, cardiac infraction, acute renal failure, nausea, unusual tiredness or weakness, vomiting, or hypersensitivity occurred during the patients’ hospital stay and 12-week follow-up. No superficial/deep wound infection was noticed during the post-operative period.
Discussion
Blood loss and the subsequent complications in TKA have been well described in the literature. Therefore, reducing the total blood loss during and after a TKA, has always been an important goal [37]. In the current RCT, after taking into account the encouraging results of previous studies, the aim of this study was to define which is the most efficient and safe TXA regimen in TKA surgery without tourniquet and to analyze the results not only in terms of actual blood loss but also in a more detailed way.
The main finding in this study, is that multiple doses of TXA reduced significantly the Hb drop and the need for ABTs in comparison with the single dose. Particularly, the two-dosage scheme reduced Hb drop by 22% and the three-dosage by 40%. As a result, a significant decrease in need for ABTs was noticed, which has been largely expressed in the three-dosage group. Moreover, the patients that had been included in the three-dosage group benefited in other aspects including decreased post-operative pain, faster rehabilitation and better quality of life without any increase of complications or adverse events.
The advantages of TXA have been well-documented in many RCTs and systematic reviews/meta-analyses [16, 38]. TXA is an antifibrinolytic drug, an analog of the amino acid lysine, and irrespective of intravenous, oral, topical or combined administration has proven its efficacy. When it comes to safety, the up-to-date literature failed to prove any increase in terms of venous thromboembolism in patients undergoing TKA [18, 39,40,41,42]. In addition, a large retrospective study (including 3490 knees/1745 bilateral TKAs), from Korea, concluded that TXA managed to reduce the transfusion rate without increasing the prevalence of DVT/PE. In this study, mechanical compression devices were applied in all patients without any chemical thromboprophylaxis [43]. The findings of the current study are aligned with the above studies and reinforce the safety of TXA in TKA without tourniquet.
Debate exists regarding the optimal dosage and duration of IV TXA [44]. Recent literature revealed that only one RCT has been conducted on this topic [45]. Xie et al. concluded that multiple IV TXA doses can effectively reduce TBL in TKA without tourniquet. In support of these findings, in the current study, the three doses of IV TXA group (Group C) benefited more, gaining a smaller Hb decline, less pain, better knee function and quality of life. In contrast, a well-designed meta-analysis by Fillingham et al. investigated the effect of re-dosing TXA on the ability to reduce blood loss and the risk of transfusion. These authors concluded that regardless of whether IV TXA is administrated as a single dose or multiple doses, no statistically significant differences were noted in blood loss or transfusion rates [46]. Τhe current study, in contrast, supports that multiple doses of TXA resulted in additional decrease of blood loss/transfusion rate compared with a single dose.
The use of tourniquet is still debatable. Although its advantages include better visualization of the surgical area and better control of blood loss, its potential complications such as thigh pain, compromised wound healing due to soft tissue hypoxia, DVT and nerve palsy outweigh the benefits. Additionally, many studies have highlighted the reduced post-operative ROM in patients who underwent TKA with tourniquet [7].
The current study clearly demonstrates the beneficial effects of a multiple dosing regimen of TXA. The most important aspect is the significant decrease in Hb drop and ABT. Interestingly, patients in Group C experienced significantly less pain during the immediate and late post-operative period. Furthermore, the results also revealed that three doses of TXA helped patients score higher FKKS and KKSS. This resulted in improved motor performance and shorter recovery. Early ambulation is a validated predictor of favorable TKA outcomes. This might explain the higher, long-term EQ-5D score that Group C obtained in terms of quality of life.
There are some limitations in our study. The study lacked a control group. However, since the current literature, including our previous study and its results, has already established the efficacy and safety of TXA, we decided not to recruit patients in a placebo group. One more limitation might be the lack of longer follow-up (longer than 12th post-operative week) and the addition of scores to the outcome measures. The strengths of the current study include the fact that it is a carefully and meticulously designed prospective RCT. The baseline characteristics of our patients (Age, BMI, ASA, etc.) were comparable between the three groups. All TKAs were performed by the same surgeon without tourniquet. The transfusion protocol was implemented strictly in order not to extract biased results.
Conclusion
Multiple intravenous doses of tranexamic acid can effectively and safely reduce a drop in the hemoglobin and concomitant blood transfusions after total knee arthroplasty without tourniquet. In addition, the three dose regimen of tranexamic acid resulted in an additional decrease in hemoglobin drop with concurrently less post-operative pain, higher function and QoL scores at 12 weeks post-operatively.
References
Maradit Kremers H, Larson DR, Crowson CS et al (2015) Prevalence of total hip and knee replacement in the United States. J Bone Jt Surg Am 97(17):1386–1397
da Silva RR, Santos AA, de Sampaio Carvalho Junior J, Matos MA (2014) Quality of life after total knee arthroplasty: systematic review. Rev Brasil Ortop 49(5):520–527
Vamvakas EC, Blajchman MA (2009) Transfusion-related mortality: the ongoing risks of allogeneic blood transfusion and the available strategies for their prevention. Blood 113(15):3406–3417
Chandra S, Kulkarni H, Westphal M (2017) The bloody mess of red blood cell transfusion. Crit Care (London England) 21(Suppl 3):310–310
Themistoklis T, Theodosia V, Konstantinos K, Georgios DI (2017) Perioperative blood management strategies for patients undergoing total knee replacement: where do we stand now? World J Orthop 8(6):441–454
Parvizi J, Diaz-Ledezma C. Total knee replacement with the use of a tourniquet: more pros than cons. Bone Jt J 2013;95-b(11 Suppl A):133–134
Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L (2014) The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res 9:13–13
Zhang Q, Dong J, Gong K, Li X, Zheng S, Wen T (2016) Effects of tourniquet use on perioperative outcome in total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (Chinese). J Repar Reconstr Surg 30(4):421–425
Du Z, Liu P, Zhang Y, Li D, Li M (2013) Effect of tourniquet on perioperative blood loss and short-term effectiveness in total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (Chinese). J Repar Reconstr Surg 27(11):1318–1323
Li X, Yin L, Chen ZY et al (2014) The effect of tourniquet use in total knee arthroplasty: grading the evidence through an updated meta-analysis of randomized, controlled trials. Eur J Orthop Surg Traumatol (Orthop Traumatol) 24(6):973–986
Liu D, Graham D, Gillies K, Gillies RM (2014) Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res 26(4):207–213
Schnettler T, Papillon N, Rees H (2017) Use of a tourniquet in total knee arthroplasty causes a paradoxical increase in total blood loss. J Bone Jt Surg Am 99(16):1331–1336
Dunn CJ, Goa KL (1999) Tranexamic acid: a review of its use in surgery and other indications. Drugs 57(6):1005–1032
Wei Z, Liu M (2015) The effectiveness and safety of tranexamic acid in total hip or knee arthroplasty: a meta-analysis of 2720 cases. Transfus Med 25(3):151–162
Wang Z, Shen X (2017) The efficacy of combined intra-articular and intravenous tranexamic acid for blood loss in primary total knee arthroplasty: a meta-analysis. Medicine 96(42):e8123
Alshryda S, Sarda P, Sukeik M, Nargol A, Blenkinsopp J, Mason JM (2011) Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Jt Surg Br 93(12):1577–1585
Mi B, Liu G, Zhou W et al (2017) Intra-articular versus intravenous tranexamic acid application in total knee arthroplasty: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 137(7):997–1009
Tzatzairis TK, Drosos GI, Kotsios SE, Ververidis AN, Vogiatzaki TD, Kazakos KI (2016) Intravenous vs topical tranexamic acid in total knee arthroplasty without tourniquet application: a randomized controlled study. J Arthroplast 31(11):2465–2470
Blanie A, Bellamy L, Rhayem Y et al (2013) Duration of postoperative fibrinolysis after total hip or knee replacement: a laboratory follow-up study. Thrombosis Res 131(1):e6–e11
Beutler E, Waalen J (2006) The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood 107(5):1747–1750
Pabinger I, Fries D, Schöchl H, Streif W, Toller W (2017) Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis. Wiener Klin Wochenschr 129(9):303–316
Zhang P, Liang Y, Chen P, Fang Y, He J, Wang J (2016) Intravenous versus topical tranexamic acid in primary total hip replacement: a meta-analysis. Medicine 95(50):e5573
Shen PF, Hou WL, Chen JB, Wang B, Qu YX (2015) Effectiveness and safety of tranexamic acid for total knee arthroplasty: a prospective randomized controlled trial. Med Sci Monit 21:576–581
Aguilera X, Martinez-Zapata MJ, Hinarejos P et al (2015) Topical and intravenous tranexamic acid reduce blood loss compared to routine hemostasis in total knee arthroplasty: a multicenter, randomized, controlled trial. Arch Orthop Trauma Surg 135(7):1017–1025
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470(1):3–19
Jansson K-Å, Granath F (2011) Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop 82(1):82–89
Ramkumar PN, Harris JD, Noble PC (2015) Patient-reported outcome measures after total knee arthroplasty: a systematic review. Bone Jt Res 4(7):120–127
Kjeldsen HB, Klausen TW, Rosenberg J (2016) Preferred presentation of the visual analog scale for measurement of postoperative pain. Pain Pract 16(8):980–984
Daabiss M (2011) American Society of Anaesthesiologists physical status classification. Indian J Anaesth 55(2):111–115
Wolf SJ, McCubbin TR, Feldhaus KM, Faragher JP, Adcock DM (2004) Prospective validation of Wells criteria in the evaluation of patients with suspected pulmonary embolism. Ann Emerg Med 44(5):503–510
Modi S, Deisler R, Gozel K et al (2016) Wells criteria for DVT is a reliable clinical tool to assess the risk of deep venous thrombosis in trauma patients. World J Emerg Surg (WJES) 11:24
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Bourke DL, Smith TC (1974) Estimating allowable hemodilution. Anesthesiology 41(6):609–612
Elzik ME, Dirschl DR, Dahners LE (2006) Correlation of transfusion volume to change in hematocrit. Am J Hematol 81(2):145–146
Guzik TJ, Adamek-Guzik T, Czerniawska-Mysik A, Dembinska-Kiec A (2002) Nitric oxide metabolite levels in children and adult patients with atopic eczema/dermatitis syndrome. Allergy 57(9):856
van Hout B, Janssen MF, Feng YS et al (2012) Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 15(5):708–715
Sikorski JM (2008) Alignment in total knee replacement. J Bone Jt Surg Br 90(9):1121–1127
Guo P, He Z, Wang Y et al (2018) Efficacy and safety of oral tranexamic acid in total knee arthroplasty: a systematic review and meta-analysis. Medicine 97(18):e0587
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Jt J 96-B(8):1005–1015
Chen X, Cao X, Yang C, Guo K, Zhu Q, Zhu J (2016) Effectiveness and safety of fixed-dose tranexamic acid in simultaneous bilateral total knee arthroplasty: a randomized double-blind controlled trial. J Arthroplast 31(11):2471–2475
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The efficacy of tranexamic acid in total knee arthroplasty: a network meta-analysis. J Arthroplast
Yuan X, Li B, Wang Q, Zhang X (2017) Comparison of 3 routes of administration of tranexamic acid on primary unilateral total knee arthroplasty: a prospective, randomized, controlled study. J Arthroplast 32(9):2738–2743
Kim YH, Park JW, Kim JS, Seo DH (2018) Does tranexamic acid increase the risk of thromboembolism after bilateral simultaneous total knee arthroplasties in Asian population? Arch Orthop Trauma Surg 138(1):83–89
Levine BR, Haughom BD, Belkin MN, Goldstein ZH (2014) Weighted versus uniform dose of tranexamic acid in patients undergoing primary, elective knee arthroplasty: a prospective randomized controlled trial. J Arthroplast 29(9 Suppl):186–188
Xie J, Ma J, Yao H, Yue C, Pei F (2016) Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplast 31(11):2458–2464
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The efficacy of tranexamic acid in total knee arthroplasty: a network meta-analysis. J Arthroplast 33(10):3
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tzatzairis, T., Drosos, G.I., Vogiatzaki, T. et al. Multiple intravenous tranexamic acid doses in total knee arthroplasty without tourniquet: a randomized controlled study. Arch Orthop Trauma Surg 139, 859–868 (2019). https://doi.org/10.1007/s00402-019-03173-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03173-z