Abstract
Introduction
Fixed-bearing unicompartmental knee arthroplasty (UKA) closely replicates native knee kinematics. As few studies have assessed kinematics following mobile-bearing (MB) UKA, the current study aimed to investigate whether MB UKA preserves natural knee kinematics.
Materials and methods
Seven fresh-frozen full-leg cadaver specimens were prepared and mounted in a kinematic rig that allowed all degrees of freedom at the knee. Three motion patterns, passive flexion–extension (0°–110° flexion), open-chain extension (5°–70° flexion) and squatting (30°–100° flexion), were performed pre- and post-implantation of a medial MB UKA and compared in terms of rotational and translational knee joint kinematics in the different anatomical planes, respectively.
Results
In terms of frontal plane rotational kinematics, MB UKA specimens were in a more valgus orientation for all motion patterns. In the axial plane, internal rotation of the tibia before and after UKA was consistent, regardless of motion task, with no significant differences. In terms of frontal plane, i.e., inferior–superior, translations, the FMCC was significantly higher in UKA knees in all flexion angles and motor tasks, except in early flexion during passive motion. In terms of axial plane, i.e., anteroposterior (AP), translations, during open-chain activities, the femoral medial condyle center (FMCC) tended to be more posterior following UKA relative to the native knee in mid-flexion and above. AP excursions of the FMCC were small in all tested motions, however. There was substantial AP translation of the femoral lateral condyle center during passive motion before and after UKA, which was significantly different for flexion angles > 38°.
Conclusions
Our study data demonstrate that the kinematics of the unloaded knee following MB UKA closely resemble those of the native knee while relative medial overstuffing with UKA will result in the joint being more valgus. However, replacing the conforming and rigidly fixed medial meniscus with a mobile inlay may successfully prevent aberrant posterior translation of the medial femoral compartment during passive motion and squatting motion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For patients presenting with unicompartmental osteoarthritis (OA) and an intact anterior cruciate ligament, unicompartmental knee arthroplasty (UKA) is a viable alternative to total knee arthroplasty (TKA), and may offer several clinical and functional benefits [1, 2]. In vivo [3] and in vitro [4, 5] studies have demonstrated that fixed-bearing (FB) UKA closely replicates the kinematics of the native knee. Nevertheless, in vivo studies have revealed significant differences in kinematics [6, 7]. These are consistent with the impact that the loss of the stabilizing effect of the meniscus has on knee kinematics, which leads to decreased internal tibial rotation and increased medial femoral condyle posterior translation [5].
The design rationale of mobile-bearing (MB) UKA is that, relative to the FB design, the higher degree of conformity between the articular surfaces mimics how the meniscal bearings reduce surface and subsurface contact stresses [8,9,10,11]. Furthermore, it has been suggested that MB knees may be superior to FB designs in their restoration of native tibiofemoral biomechanics, thus permitting more natural joint mechanics for younger, more demanding patients [9, 12,13,14]. Few biomechanical studies have assessed kinematics following MB UKA, however [9].
We hypothesize that near-normal physiological kinematic patterns can be achieved with MB UKA. We therefore compared knee kinematics patterns in the native knee and following MB UKA during passive flexion–extension, open-chain extension and squatting in an in vitro study. Additionally, we also compared contact pressure in the lateral compartment during these kinematic patterns.
Materials and methods
Seven right fresh-frozen full-leg specimens [74.4 years (range 56–93), all female] were disarticulated at the hip. All specimens had functional ligaments, no evidence of bone deformities and no history of lower-limb trauma. A single specimen was found to have grade IV osteoarthritis in the medial compartment, while all others displayed no signs of osteoarthritis. A previously validated and well-described testing methodology was used [15], the main details of which are described below. Ethical approval for the study was obtained prior to study commencement.
Marker frames containing four retro-reflective spheres were rigidly attached to the femur and tibia using two pairs of bi-cortical bone pins. Volumetric computed tomography (CT) scans (Siemens Definition Flash; Siemens Healthcare GmbH, Erlangen, Germany) of the frozen specimens were taken at a slice thickness of 0.75 mm. One day prior to testing, specimens were thawed and resected 32 cm proximally and 28 cm distally from the knee joint line. The surrounding skin and subcutaneous tissue were removed, with care taken to preserve the joint capsule, ligaments and tendons. The femur and tibia were placed in physiologic alignment and embedded in metal containers using a cold-cure acrylic resin (VersoCit2; Struers, Ballerup, Denmark). The hamstrings tendons were exposed and suture loops attached. The quadriceps tendon was prepared and a custom clamping system was attached 6 cm proximal to the patella.
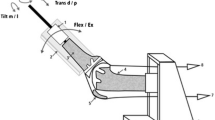
The prepared specimens were mounted in a dynamic knee rig capable of replicating physiologic knee motion during various functional tasks (Fig. 1). The rig consisted of two linear actuators, simulating the hip position and quadriceps action, two constant load springs (50 N) to simulate the medial and lateral hamstrings, and a mechanical ankle joint, which allowed mediolateral translation and all rotational degrees of freedom. The vertical position of the hip (e.g., knee flexion) was the only controlled rig position; all other degrees of freedom were free and dictated by the specimen’s anatomy. For loaded motions, both hamstring springs were attached to the specimen and the quadriceps clamp connected to the quadriceps linear actuator. Calibrated load cells, in-line with the quadriceps actuator and below the ankle joint, measured applied loads and moments.
Three functional motions were undertaken: passive flexion–extension cycles (0°–110° flexion), loaded open-chain extension (5°–70° flexion) and loaded squatting (30°–100° flexion). During open-chain extension, a 3 kg dead weight was fixed to the end of the tibial container and the quadriceps actuator was engaged at a constant rate to induce knee extension. For squatting, the vertical position of the hip was manipulated to cause knee flexion, while the quadriceps were actuated with a variable force to maintain a vertical ankle load of 110 N. For all motion trials, six MX40+ infrared cameras (Vicon Motion Systems, Oxford, UK) operating at 100 Hz recorded the trajectories of the reflective spheres, which were post-processed using a custom pipeline (Nexus 1.8.5; Vicon Motion Systems).
Contact pressure during squatting in the lateral compartment of the specimens was recorded on a resistive-based sensor (K-scan 4000; Tekscan, South Boston, MA, USA) held in place with several sutures through the posterior capsule. Prior to testing, the sensors were covered with Teflon tape to reduce shear/friction and calibrated using a testing frame [16].
After performing all three motion trails on the native knee, specimens were implanted with a medial MB UKA (Oxford; Zimmer Biomet, Warsaw, IN, USA) by UKA-experienced surgeons (G.P. and T.H.) using a minimally invasive medial parapatellar approach and following the manufacturer’s guidelines. The motion trials were then repeated for each specimen, using the same methodology. As it was not possible to attach a pressure sensor to the polyethylene insert due to its high curvature, no medial compartment pressure measurements were taken.
Anatomic landmarks identified in preoperative CT scans using medical image processing software (Mimics 18.0; Materialise, Leuven, Belgium) were used to define a joint coordinate system based on the method described by Grood and Suntay [17]. The reflective spheres were also identified on the scans, and their position relative to the anatomic landmarks determined. This allowed for transforming the marker trajectories recorded during the motion trials into anatomical translations and rotations. Translations of the femoral medial and lateral condyle centers (FMCC and FLCC) were scaled to the maximum anterior–posterior (AP) width of the medial and lateral tibial plateau, respectively, to enable comparisons between different-sized specimens. Strain in the superficial medial collateral ligament (sMCL) was calculated from the change in distance between the femoral and tibial insertion sites [18], using a previously described method [19].
All motion trials were resampled at increments of 1° knee flexion within the shared common range between all specimens to allow comparisons between tests. Kinematic patterns were averaged between specimens and are presented as mean ± standard deviation, where applicable. For the obtained kinematic and contact pressure data, statistical analysis was performed using a multivariate repeated-measures analysis of variance with Tukey’s HSD post hoc analysis. All statistical analysis was performed using Statistica 12 (Statsoft, Tulsa, OK, USA) with a significance level of 0.05. Previously published work using the same testing methodology demonstrated that six specimens were sufficient to achieve a statistical power of 80% [20].
Results
Results in terms of kinematics are presented below per anatomical plane for rotational and translational degrees of freedom, respectively, both as a function of the flexion angle.
In terms of frontal plane rotational kinematics, specimens following implantation of the MB prosthesis were in a more valgus orientation than in the native knee (Fig. 2). During open-chain and squat motions, the UKA was significantly in more valgus for all tested flexion angles, while, during passive motion, only early flexion (20°–30°) was significantly different between the UKA and native knees (Table 1). During passive and open-chain motions, there was a greater variation in valgus orientation over the flexion cycle, whereas the orientation tended to stay more constant during squatting.
In the axial plane, internal rotation of the tibia was consistent between the two conditions, regardless of motion task and no significant differences were found. During passive motion, the classic screw-home mechanism of the knee was observed in both conditions, with the tibia externally rotating as it approached full extension.
In terms of frontal plane, i.e., inferior–superior (IS), translations, the FMCC was significantly higher in MB UKA than native knees in all flexion angles for all tested motions, except in early flexion during passive motion (Table 2). No significant differences in the IS position of the FLCC were observed (data not show).
In terms of axial plane, i.e., anteroposterior (AP), translations, AP positions of the FMCC and FLCC as a function of flexion are shown in Fig. 3. In mid-flexion and above, the AP translation of the FMCC tended to be more posterior following UKA relative to the native knee for all motor tasks. The difference was significant only during open-chain motion at flexion angles > 26°, however. Overall, the excursions in the AP position of the FMCC were relatively small in all tested motions, regardless of knee flexion angle. AP translation of the FLCC during passive motion revealed substantial posterior translation for both before and after UKA, and was significantly different for flexion angles > 38°. During passive motion, the native and MB UKA knees exhibited femoral rollback with increasing flexion angles. During open-chain and squat motions, MB UKA knees tended to be more posteriorly positioned, with significant differences from the native knee identified during mid- to deep-flexion. In addition, the FLCC exhibited paradoxical anterior sliding in deep-flexion during squatting for both native and UKA knees.
The anterior–posterior (AP) translation of the femoral medial and lateral condyle centers (FMCC and FLCC) for the three tested motions. Solid lines represent the average values and the shaded regions the standard deviations. Values are normalized to the maximum AP width of the medial and lateral tibial plateaus, respectively (e.g., 0 represents completely posterior and 1 completely anterior)
Strain in the superficial medial collateral ligament was significantly higher for MB UKA knees in all tested motions during open-chain and squatting, and above 20° flexion during passive motion (Fig. 4). During passive and open-chain motions, sMCL strain peaked during mid-flexion, whereas peak strain occurred at the start of the motion trial during squatting, i.e., when the specimen was in an extended position. Peak strain values of 0.071, 0.068, and 0.079 (mm/mm) were measured during flexion–extension, open-chain, and squatting, respectively, in the MB UKA knee. During all motions, sMCL strain tended to decrease in deep-flexion.
Contact pressure in the lateral compartment of the knee during squatting tended to be higher in the MB UKA knee relative to the native knee; however, these findings were not significant, regardless of knee flexion angle (Fig. 5). Peak differences in pressure occurred at 80° knee flexion, where contact pressures were 8.7 ± 2.6 MPa in native and 10.7 ± 3.8 MPa in MB UKA knees (p = 0.0655). For both knees, contact pressures peaked at the highest knee flexion angle and followed the same trend. Finally, the peak quadriceps force during squatting required to induce a vertical ankle load of 110 N was 2.4 ± 0.3 and 2.7 ± 0.3 kN for the native and MB UKA knees, respectively, which was not significantly different.
Discussion
This in vitro biomechanical study demonstrated that following MB UKA most knee kinematics are close to those of the native knee, particularly during passive motion. Based on the current findings, it appears that the bony geometry of the native medial femoral condyle and tibial plateau is functionally restored by the implant. There were, however, some significant differences between the native and postoperative knee, particularly during open-chain extension, and specifically in the inferior–superior position of the medial femoral condyle, the AP translation of the lateral femoral condyle and the varus–valgus tilting of the tibia. The femoral medial condyle also had a more posterior position during open-chain motion.
We hypothesize that, compared to the native condition, increased stiffness in the MB UKA-replaced medial compartment leads to biomechanical changes similar to those induced by overstuffing of the medial compartment: proximalization of the medial condyle, slight valgization, increased tightness of the MCL, and reduced frontal plane mobility into varus [20, 21]. With respect to kinematics, increased medial stiffness is hypothesized to have additionally led to increased femoral rollback in the lateral compartment during flexion, as the latter was unaffected by the medial overstuffing. Following MB UKA, the medial femoral compartment had a marginally more posterior position during open-chain activities than in the native knee. This is likely to be caused by the PCL, which is tighter due to the superior position of the femur [5]. The MB insert in the current study appeared to successfully prevent this aberrant posterior translation during passive motion and squat motion, although the lateral condyle had increased rollback during all activities. A previous study with a FB UKA conducted using the same knee rig and experimental protocol, found less internal tibial rotation and a more posterior femoral medial condyle position during squatting, which is also seen after medial meniscectomy [5]. For FB UKA, this kinematic pattern may be due to difficulties in accurately reproducing the contact point, as the PE inlay of most FB UKAs is relatively flat and differs from the more conforming wedge shape of the medial meniscus. MB UKA designs, including the one used in this study, typically make use of more conforming PE inserts. As a result no differences in internal rotation were found between the MB UKA and the native knees of the study. Furthermore, any significant differences in AP translation of the medial femoral condyle occurred only during open-chain activities. We hypothesize this more pronounced difference during open-chain to be additionally due to the free floating tibia, and more specifically the absence of any anterior–posterior constraint at the distal end of the tibia to counteract the anterior pull on the tibia generated by the quadriceps through the patellar tendon.
Although these findings may imply that the conforming inlay of MB UKA reproduces native kinematics more closely than that of FB UKA, we nevertheless detected other relevant statistically significant differences between native and UKA kinematics. For example, the FMCC of the UKA knee was positioned more superiorly than in the native knee and, probably as a result, the tibia was more in valgus. Similar findings have been noted with FB UKA designs [5].
Several limitations of this study should be noted. Due to cadaver availability and the associated high cost, only a limited number of specimens were tested. This, however, did not prevent the observation of significant differences in kinematic patterns. Additionally, the axial loads applied using the knee rig do not approach those seen in the knee during functional activities [22]; however, this was deliberately chosen to reduce the risk of damaging the specimen and allow for repeat testing under different conditions. Furthermore, previous analysis of the described set-up in terms of the effect of different magnitudes of vertical ankle forces on tibiofemoral kinematics showed only small impact [23]. Secondly, despite the non-physiologic axial load, both the magnitude and evolution of the contact pressures reported in this study closely agrees with recently published contact pressures following knee arthroplasty [24]. Thirdly, also the quadriceps force fell well within ranges previously reported in the literature for comparable set-ups [25]. Nevertheless, the absence of physiological axial loading might also prevent the investigation of potential bearing dislocation, which has previously been observed for MB UKA [26, 27]. Additionally, since bearing dislocation typically occurs at deep-flexion angles (> 120°) [28], we speculate that the lack of physiological axial loads had minimal impact on the measured kinematics since flexion angles exceeding 120° were not investigated. As a final limitation, only three motion tasks were investigated; however, resulting kinematic patterns may differ for more complex tasks such as strain climbing and gait. Despite these limitations, cadaver tests allow trials with different joint components using controlled forces and moments, and the isolation of variables such as the effects of overstuffing, which is not possible with in vivo tests such as biplanar fluoroscopy-based studies [29].
In conclusion, our study data demonstrate that the kinematics of the unloaded knee following MB UKA closely resemble those of the native knee while relative medial overstuffing with UKA will result in the joint being more valgus. However, replacing the conforming and rigidly fixed medial meniscus with a mobile inlay may successfully prevent aberrant posterior translation of the medial femoral compartment during passive motion and squatting motion.
References
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt J 97-B(6):793–801
Wiik AV, Aqil A, Tankard S, Amis AA, Cobb JP (2015) Downhill walking gait pattern discriminates between types of knee arthroplasty: improved physiological knee functionality in UKA versus TKA. Knee Surg Sports Traumatol Arthrosc 23(6):1748–1755
Catani F, Benedetti M, Bianchi L, Marchionni V, Giannini S, Leardini A (2012) Muscle activity around the knee and gait performance in unicompartmental knee arthroplasty patients: a comparative study on fixed- and mobile-bearing designs. Knee Surg Sports Traumatol Arthrosc 20(6):1042–1048
Becker R, Mauer C, Starke C, Brosz M, Zantop T, Lohmann CH, Schulze M (2013) Anteroposterior and rotational stability in fixed and mobile bearing unicondylar knee arthroplasty: a cadaveric study using the robotic force sensor system. Knee Surg Sports Traumatol Arthrosc 21(11):2427–2432
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Scheys L, Innocenti B, Fuchs-Winkelmann S, Labey L (2014) UKA closely preserves natural knee kinematics in vitro. Knee Surg Sports Traumatol Arthrosc 22(8):1902–1910
Mochizuki T, Sato T, Blaha JD, Tanifuji O, Kobayashi K, Yamagiwa H, Watanabe S, Matsueda M, Koga Y, Omori G, Endo N (2014) Kinematics of the knee after unicompartmental arthroplasty is not the same as normal and is similar to the kinematics of the knee with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 22(8):1911–1917
Mochizuki T, Sato T, Tanifuji O, Kobayashi K, Koga Y, Yamagiwa H, Omori G, Endo N (2013) In vivo pre- and postoperative three-dimensional knee kinematics in unicompartmental knee arthroplasty. J Orthop Sci 18(1):54–60
Emerson RJ, Hansborough T, Reitman R, Rosenfeldt W, Higgins L (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Smith T, Hing C, Davies L, Donell S (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605
Ettinger M, Zoch JM, Becher C, Hurschler C, Stukenborg-Colsman C, Claassen L, Ostermeier S, Calliess T (2015) In vitro kinematics of fixed versus mobile bearing in unicondylar knee arthroplasty. Arch Orthop Trauma Surg 135(6):871–877
Walker T, Heinemann P, Bruckner T, Streit MR, Kinkel S, Gotterbarm T (2017) The influence of different sets of surgical instrumentation in Oxford UKA on bearing size and component position. Arch Orthop Trauma Surg 137(7):895–902
Gleeson R, Evans R, Ackroyd C, Webb J, Newman J (2004) Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee 11(5):379–384
Li M, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13(5):365–370
Suzuki T, Ryu K, Kojima K, Iriuchishima T, Saito S, Nagaoka M, Tokuhashi Y (2015) Evaluation of spacer block technique using tensor device in unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 135(7):1011–1016
Victor J, Van Glabbeek F, Vander Sloten J, Parizel PM, Somville J, Bellemans J (2009) An experimental model for kinematic analysis of the knee. J Bone Jt Surg Am 91(Suppl 6):150–163
Brimacombe JM, Wilson DR, Hodgson AJ, Ho KC, Anglin C (2009) Effect of calibration method on Tekscan sensor accuracy. J Biomech Eng 131(3):034503
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone Jt Surg Am 89(9):2000–2010
Heyse TJ, El-Zayat BF, De Corte R, Scheys L, Chevalier Y, Fuchs-Winkelmann S, Labey L (2014) Biomechanics of medial unicondylar in combination with patellofemoral knee arthroplasty. Knee 21(Suppl 1):S3–S9
Heyse TJ, El-Zayat BF, De Corte R, Scheys L, Chevalier Y, Fuchs-Winkelmann S, Labey L (2016) Balancing UKA: overstuffing leads to high medial collateral ligament strains. Knee Surg Sports Traumatol Arthrosc 24(10):3218–3228
Heyse TJ, Tucker SM, Rajak Y, Kia M, Lipman JD, Imhauser CW, Westrich GH (2015) Frontal plane stability following UKA in a biomechanical study. Arch Orthop Trauma Surg 135(6):857–865
Mundermann A, Dyrby CO, D’Lima DD, Colwell CW Jr, Andriacchi TP (2008) In vivo knee loading characteristics during activities of daily living as measured by an instrumented total knee replacement. J Orthop Res 26(9):1167–1172
Victor J (2009) A comparative study on the biomechanics of the native human knee joint and total knee arthroplasty. Katholieke Universiteit, Leuven
Navacchia A, Rullkoetter PJ, Schutz P, List RB, Fitzpatrick CK, Shelburne KB (2016) Subject-specific modeling of muscle force and knee contact in total knee arthroplasty. J Orthop Res 34(9):1576–1587
Patil S, Colwell CW Jr, Ezzet KA, D’Lima DD (2005) Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Jt Surg Am 87(2):332–338
Jeong JH, Kang H, Ha YC, Jang EC (2012) Incarceration of a dislocated mobile bearing to the popliteal fossa after unicompartmental knee arthroplasty. J Arthroplast 27(2):323.e325–323.e327
Singh VK, Apsingi S, Balakrishnan S, Manjure S (2012) Posterior dislocation of meniscal bearing insert in mobile bearing unicompartmental knee arthroplasty mimicking a Baker cyst. J Arthroplasty 27(3):494.e413–494.e496
Lee SY, Bae JH, Kim JG, Jang KM, Shon WY, Kim KW, Lim HC (2014) The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case–control study. Bone Jt J 96(7):914–922
Argenson J, Komistek R, Aubaniac J, Dennis D, Northcut E, Anderson D, Agostini S (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplast 17(8):1049–1054
Acknowledgements
The study was funded by a German Knee Society Grant (Deutsche Kniegesellschaft) and a research Grant of the Rhön-Klinikum AG (Innovations- und Förderpool). The implants were donated by Zimmer Biomet, Europe.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Peersman, G., Slane, J., Vuylsteke, P. et al. Kinematics of mobile-bearing unicompartmental knee arthroplasty compared to native: results from an in vitro study. Arch Orthop Trauma Surg 137, 1557–1563 (2017). https://doi.org/10.1007/s00402-017-2794-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2794-8