Abstract
Purpose
When performing unicondylar knee arthroplasty (UKA), the surgeon can choose between two fundamentally different designs: a mobile-bearing (MB) inlay with high conformity, or a low-conformity, fixed bearing (FB) inlay. There is an ongoing debate in the orthopaedic community about which design is superior. To date, there have been no comparative biomechanical studies regarding each system’s effects on the quadriceps force and the medial contact pressure. The purpose of this study was to investigate these alterations in vitro before and after UKA with two prosthesis systems, representing the MB and FB designs.
Methods
FB and MB unicondylar knee prosthesis designs were tested in sequence under isokinetic extension in an in vitro simulator. In each case, the required quadriceps extension force was determined before and after implantation of a medial UKA. Furthermore, the tibiofemoral contact pressures were evaluated for both prosthesis designs.
Results
The quadriceps force maximum was achieved at 106° and 104° of flexion with the FB and MB designs, respectively. Implantation of the FB UKA resulted in a significant increase in the necessary maximum quadriceps force (p = 0.006). In addition, implantation of the MB UKA resulted in a significantly higher extension force (p = 0.03). The difference between the two groups was statistically significant in deep flexion (p = 0.03), with higher forces in MB UKA.
Conclusion
The MB design showed significantly increased quadriceps extension force compared with the FB inlay in deep flexion. Although the FB design showed higher maximum peak pressures concentrated on a smaller area, the pressure introduction in deep flexion was lower, compared to MB inserts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicondylar knee arthroplasty (UKA) is an interesting alternative to total knee arthroplasty in the treatment of unicompartmental knee arthritis. A variety of studies have reported good joint survival and excellent function following this surgery, especially in young and very active patients [9, 10, 20, 28]. Several in vitro and in vivo studies have indicated better and more physiological joint biomechanics with the bicruciate-retaining principle of UKA, as compared with total knee arthroplasty designs.
When performing UKA, the surgeon can choose between two fundamentally different designs: mobile-bearing (MB) and fixed bearing (FB) UKA [3]. There is an ongoing debate in the orthopaedic community about which design is superior. Six prospective randomised studies [6, 11, 12, 17, 19, 27] and a meta-analysis (level of evidence 1) [26] have shown no superiority in clinical, radiological or kinematic outcomes of one design over the other. Furthermore, a recent retrospective study focusing on quality of life also found no differences [2]. These studies have therefore failed to develop criteria to facilitate decision making when choosing between MB and FB UKA. We are interested in decision making—for example, whether more physiological biomechanics and high reflection are of advantage to young, athletic patients. Only sparse data exist for in vitro biomechanics: a common reason for the failure of early UKAs was delamination of the polyethylene bearing [16, 25]. Burton et al. [5] recently evaluated the effects of kinematics and femoral lift-off on the wear of FB and MB UKAs. In this study, the FB design had lower wear than the MB design under all conditions. In particular, improvements in the material properties of FB inlays make the FB design an equivalent alternative and highlight the potential for a longer osteolysis-free clinical outcome with these devices.
To date, however, there have been no comparative biomechanical studies of MB and FB inlays with respect to quadriceps extension forces or tibiofemoral pressures introduction that might influence the referred discussion of physiological biomechanics and reduced wear. This study focuses on quadriceps force as an important parameter for joint biomechanics that is influenced by friction resistance or changes of the lever arms, for example. In addition, differences in the tibiofemoral articulation with respect to pressure distribution patterns were evaluated, as the contact area and the pressure peaks influence the wear and display motion pattern.
The purpose of this in vitro study was to investigate the amount of quadriceps force required to extend the knee during an isokinetic extension cycle before and after UKA with two prosthesis systems, representing MB and FB designs. The hypothesis was that the two designs would not differ significantly with respect to the necessary quadriceps extension force; however, the pressure introduction onto the tibial platform is expected to be quite different.
Materials and methods
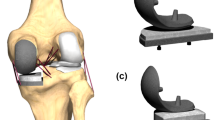
FB and MB unicondylar knee prosthesis designs were tested in sequences under isokinetic extension in an in vitro simulator, which can simulate muscular traction power using hydraulic cylinders, which cross over the knee joint. Thus, a knee movement like in a seated leg extension machine can be simulated. The kinemator (Fig. 1) has been described and used in a number of previous studies investigating knee biomechanics [7, 14, 15, 24]. In our study, 12 fresh frozen cadaver knees (64–78 years of age) with intact soft tissue, no previous surgery and no significant arthritis were randomised into one of two groups: (1) FB medial slide (Sigma® High Performance Partial Knee; DePuy, Warsaw, IN, USA); and (2) MB slide (Oxford® medial unicompartmental knee, III generation; Biomet, Warsaw, IN, USA). In each case, the required quadriceps extension force was determined before and after implantation of a medial UKA. Furthermore, the tibiofemoral contact pressures were evaluated for both prosthesis designs.
Analogous to previous studies conducted by our group [24], the knees were transected 30 cm proximally and distally to the knee joint line. After removal of the skin and subcutaneous fat, the remaining soft tissues were preserved. In this simulator, the specimens were positioned with the femur fixed horizontally and the patella facing downwards. The femoral and tibial bone stumps were fixed in metal sleeves with bone cement to reproduce the same positioning before and after removal. The tibia was attached to the simulator at mid-length by means of a linear rotational bearing, which allowed axial sliding and turning as well as rotation transverse to the axis of the tibia. The bearing itself was attached to a swing arm that allowed motion in the varus/valgus plane.
The resulting arrangement gave complete freedom of motion of the joint, with the exception of flexion–extension, which was determined by the position of the swing arm. The swing arm was equipped with a strain gauge-based load-measuring device that allowed continuous monitoring of a torsional moment applied to the tibia. The tibia was moved through the coordinated activation of three hydraulic cylinders, which were attached to the specimens’ tendons by special clamps: one to simulate quadriceps muscle force; one to simulate a co-contraction of the hamstring muscles; and the third to apply an external flexion moment.
The test cycle simulated an isokinetic extension cycle from 120° knee flexion to full extension. The quadriceps cylinder thereby applied sufficient force to the quadriceps tendon in a closed-loop control cycle to generate a constant knee extension moment of 31 Nm. The hamstrings cylinder simulated co-contraction of the hamstring muscles with a constant co-contractive flexion force of 100 N. Initially, the swing arm was activated to bring the specimen into a position of 120° of flexion. The quadriceps cylinder was then activated in feedback control to provide a constant net joint extension moment by applying the constant extension moment at the swing arm. The joint moment was measured by the load cell in the swing arm, allowing continuous control of quadriceps force throughout the complete motion to maintain the nominal extension moment of 31 Nm. This constant extension moment was resisted by a constant swing arm flexion moment, which was generated by a third hydraulic cylinder, creating an isokinetic extension movement. After one complete extension cycle, the specimen could be driven back to 120° of knee flexion without remounting.
Quadriceps force was measured at a frequency of 10 Hz and with an accuracy of ±0.1 N using a load cell (Hottinger Baldwin Messtechnik GmbH, Darmstadt, Germany) attached between the tendon clamp and the quadriceps cylinder. The degree of knee flexion was measured using a custom-made electronic goniometer attached to the tibial swing arm at a frequency of 10 Hz and with an accuracy of ±0.05°.
The articulation and pressure distribution between the femoral and tibial component was displayed using a 33 × 22-mm electronic pressure-sensitive film (K-Scan 4000; Tekscan, Boston, MA, USA). After preconditioning and calibration of the films, as described previously [1], the foil was glued directly onto the surface of the inlay in the FB prosthesis or onto the tibia tray in the MB design. In addition, a 0.1-mm Teflon film was glued onto the sensor to protect the film against shear forces. Using the recorded pressure distribution and the load on each “sensel”, the pressure calibration was computed using Tek-scan! software (version 4.23; Tekscan). Area and peak contact pressures were evaluated, and the centre of pressure as the geometric centre of the loaded pressure area was used to follow the tibiofemoral contact pressures during the extension cycle.
All test cycles were run at room temperature.
Statistics
Because comparisons of these types of prostheses have not previously been quantified, power analysis was not performed. A D’Agostino & Pearson omnibus normality test was performed to analyze normality distribution. If normality test passed, a non-parametric unpaired t test was performed. If normality test failed, a Mann–Whitney test was performed to compare results.
The significance level was set to p = 0.05. We used SPSS version 21 for statistical analysis and randomisation.
Results
The maximum and minimum quadriceps extension forces for the native knee joints were similar for both groups (difference not significant, p = 0.273 and p = 0.6, respectively; Table 1). The force maximum was achieved at 106° or 104° of flexion with the FB and MB designs, respectively. Implantation of the FB UKA resulted in a slight (mean 75 N) but significant increase in the necessary maximum quadriceps force (p = 0.006). Implantation of the MB UKA also resulted in a significantly higher maximum extension force (p = 0.03); however, the increase in this case was approximately 158 N, leading to a statistically significant difference between the FB and MB groups (p = 0.03, Table 1).
As shown in Fig. 2 and Table 2, there was a significant increase in the necessary quadriceps force with both implants during the further extension cycle from 120° to 40° or 30°, respectively, compared with native joint quad forces. However, significant differences between the implant types could only be detected for deep flexion between 120° and 90°, to higher values of the MB inlay.
There was a significant increase in the necessary quadriceps force with both implants during the further extension cycle from 120° to 40° or 30°, respectively, compared with native joint. However, significant differences between the implant types could only be detected for deep flexion between 120° and 90°, to the disadvantage of the MB inlay
Close to extension (<30° flexion), no difference could be detected between native joint quadriceps forces and either UKA scenario.
The contact area and pressure distribution on the tibia component differed fundamentally between the two UKA designs. A mean peak pressure of 14.11 MPa (standard deviation 7.27) was detected across the flexion–extension cycle in the FB group, compared with 5.78 MPa (standard deviation 3.47) in the MB group. Furthermore, the peak pressure curves were different in relation to the maximum values. The maximum pressure introduction was observed in deep flexion with the FB inlay and close to extension with the MB inlay. Analogously to the different peak pressures, the area contact pressures also differed between the two systems. With the FB inlay, this was concentrated to a relatively constant mean value of 0.4 cm2, whereas a minimum of 1 cm2 across the whole tibial tray surface was detected in the MB group. According to these findings, the mean pressure was 6.68 MPa (standard deviation 0.59) for the FB and 1.0 (0.34 standard deviation) for the MB.
Discussion
The most important finding of this study is that the MB design showed significant increased quadriceps extension force compared with the FB inlay in deep flexion. The hypothesis that the two designs would not differ significantly with respect to the necessary quadriceps extension force has to be rejected.
One general limitation of this in vitro study is that only a simplified model of the in vivo biomechanics of the knee joint was used. Unlike the varying peak extension moments during gait [13], only one constant moment during the whole extension cycle was simulated. As reported previously, this was set to 31 Nm and orientated on the mean extension moment reached by patients over an isokinetic extension cycle in vivo [22]. As a co-contraction force of the hamstrings, we choose to apply 100 Nm according to Durselen et al.’s analysis of the physiological muscle co-contractions around the knee [8]. This achieves a close to natural, additional stabilisation of the knee joint. Because of this simplification, the quantitative results of this study cannot be directly translated to in vivo conditions. In this study an isokinetic knee extension was simulated, more complex movements like gait or squatting cannot be assessed with this setup. However, the methodology is suitable to illustrate biomechanical effects and the differences between the two compared prosthesis designs both in vitro and in vivo. The second general limitation is the placement of the Tekscan sensor: for pressure distribution measurements of the medial compartment, the Tekscan sensor was put on top of the PE in FB UKA, and underneath it in MB UKA. It seems to be obvious that this will lead to lower peak pressures in the MB group as the contact area will be much higher. The third general limitation is that more complex knee motions as squatting, gait etc. cannot be assessed with this experimental setup.
Quadriceps force
Quadriceps force is a key parameter in the evaluation of prosthetic biomechanics, with a low force required to extend the same extension moment considered to be biomechanically advantageous [24]. Furthermore, the tibiofemoral contact pressure and contact point are of special interest in the assessment of UKA, as this system is designed to mimic physiological joint movements with a physiological femoral rollback due to intact cruciate ligaments. Our study evaluated both of these key parameters for the two available fundamental UKA designs—the FB and MB inlays—to enable a biomechanical comparison of the two systems. This study demonstrated that both MB and FB UKA have an impact on the quadriceps force required to extend the knee compared with the native situation. This is consistent with the findings of other studies evaluating the impact of different prostheses on quadriceps extension force with the same test setup [21–23].
Although the quadriceps curves of both prostheses were very similar in our evaluation, our data indicate that the MB inlay has biomechanically inferior characteristics in deep flexion, requiring an increased extension force compared with the FB inlay. Similar effects have been demonstrated for total knee arthroplasties and are often attributed to changes in the physiological lever arm and insufficient restoration of the tibiofemoral trajectories. However, taking the performed analyses of the tibiofemoral contact pressures into account, we consider that this is not caused by an altered motion pattern with the MB versus the FB inlay, but might be attributed to the larger surface friction of the MB on the tibial tray, especially in deep flexion. In this particular situation, the MB inlay showed the highest motion relative to the tibia tray. This would also explain the lower pressure introduction to the tibia in deep flexion.
Contact pressure
The data presented for the different peak pressures, mean pressures and contact areas for the two designs are as expected. The tibiofemoral contact area is concentrated to a minimum of 0.4 cm2 with the low-conformity FB inlay, with relative high peak and mean pressure occurring. With the MB design, these high peaks are prevented by the high-conformity design of the inlay to the femur. However, it has to be discussed that the pressure-sensitive films were placed on top of the FB polyethylene insert and underneath the MB insert, respectively. This setup leads to the lower peak pressures recorded on the tibia in the MB group as the contact area between inlay and tibia is much higher than between femur and inlay. The intension of this approach was to display the femoral pressure introduction on the tibia as well as the contact point that was defined as coordinate of the peak pressure. This could not be displayed when recording the insert surface in the MB UKA, because with the high conformity and the constant movement of the insert, this would be more or less the same during the whole range of motion. As a result, the pressure shows a better distribution on the tibial tray. This was shown in a recent study by Kwon et al. [18], and also by van den Heever et al. in 2011 [29]. The literature describes high failure rates due to wear for both the FB and MB prostheses [25]. The initial consideration supporting the MB design was that the larger contact area and lower contact pressures would lead to better wear characteristics. A recent meta-analysis focusing on the question of reduced polyethylene wear and longer survival with the MB design did not disconfirm this theory [30]. However, recent biomechanical analyses have reported higher wear with MB versus FB designs, caused by back side wear between the tibia tray and inlay [4]. Referring to our results, this might be a significant problem in patients who frequently use deep flexion motions, because of the relevant relative motion of the inlay here.
Transferring our in vitro findings to the in vivo situation, both the MB and FB UKA designs showed similar effects. The quadriceps force curve and tibiofemoral contact pressures indicated a closer-to-physiological behaviour of UKA compared with most of the total knee arthroplasty designs evaluated in earlier studies by our group. However, the MB design showed increased quadriceps extension force versus the FB inlay solution especially in deep flexion. This seemed to be attributed to high friction forces when extending the knee from deep flexion. This might result in higher wear, especially in very active and regularly deep-flexing patients.
The clinical significance of these data must be evaluated in further studies.
Conclusions
The MB design showed significantly increased quadriceps extension force compared with the FB inlay in deep flexion. Although the FB design showed higher maximum peak pressures concentrated on a smaller area, the pressure introduction in deep flexion was lower, compared to MB inserts.
References
Becher C, Huber R, Thermann H, Tibesku CO, von Skrbensky G (2009) Tibiofemoral contact mechanics with a femoral resurfacing prosthesis and a non-functional meniscus. Clin Biomech (Bristol, Avon) 24(8):648–654. doi:10.1016/j.clinbiomech.2009.05.013
Biau DJ, Greidanus NV, Garbuz DS, Masri BA (2013) No difference in quality-of-life outcomes after mobile and fixed-bearing medial unicompartmental knee replacement. J Arthroplasty 28(2):220.e1–226.e1. doi:10.1016/j.arth.2012.05.017
Bonutti PM, Dethmers DA (2008) Contemporary unicompartmental knee arthroplasty: fixed vs mobile bearing. J Arthroplasty 23(7 Suppl):24–27. doi:10.1016/j.arth.2008.06.025
Brockett CL, Jennings LM, Fisher J (2011) The wear of fixed and mobile bearing unicompartmental knee replacements. Proc Inst Mech Eng H 225(5):511–519
Burton A, Williams S, Brockett CL, Fisher J (2012) In vitro comparison of fixed- and mobile meniscal-bearing unicondylar knee arthroplasties: effect of design, kinematics, and condylar liftoff. J Arthroplasty 27(8):1452–1459. doi:10.1016/j.arth.2012.02.011
Confalonieri N, Manzotti A, Cerveri P, De Momi E (2009) Bi-unicompartmental versus total knee arthroplasty: a matched paired study with early clinical results. Arch Orthop Trauma Surg 129(9):1157–1163. doi:10.1007/s00402-008-0713-8
Daniilidis K, Holl S, Gosheger G, Dieckmann R, Martinelli N, Ostermeier S, Tibesku CO (2013) Femoro-tibial kinematics after TKA in fixed- and mobile-bearing knees in the sagittal plane. Knee Surg Sports Traumatol Arthrosc 21(10):2392–2397. doi:10.1007/s00167-012-1986-6
Dürselen L, Claes L, Kiefer H (1995) The influence of muscle forces and external loads on cruciate ligament strain. Am J Sports Med 23(1):129–136
Engh GA, Ammeen DJ (2014) Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat Res 472(1):73–77. doi:10.1007/s11999-013-2982-y
Felts E, Parratte S, Pauly V, Aubaniac JM, Argenson JN (2010) Function and quality of life following medial unicompartmental knee arthroplasty in patients 60 years of age or younger. Orthop Traumatol Surg Res 96(8):861–867. doi:10.1016/j.otsr.2010.05.012
Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH (2004) Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee 11(5):379–384. doi:10.1016/j.knee.2004.06.006
Harrington MA, Hopkinson WJ, Hsu P, Manion L (2009) Fixed- vs mobile-bearing total knee arthroplasty: does it make a difference? A prospective randomized study. J Arthroplasty 24(6 Suppl):24–27. doi:10.1016/j.arth.2009.04.031
Hatfield GL, Hubley-Kozey CL, Astephen Wilson JL, Dunbar MJ (2011) The effect of total knee arthroplasty on knee joint kinematics and kinetics during gait. J Arthroplasty 26(2):309–318. doi:10.1016/j.arth.2010.03.021
Heyse TJ, Becher C, Kron N, Ostermeier S, Hurschler C, Schofer MD, Fuchs-Winkelmann S, Tibesku CO (2010) Quadriceps force in relation of intrinsic anteroposterior stability of TKA design. Arch Orthop Trauma Surg 130(1):1–9. doi:10.1007/s00402-009-0927-4
Heyse TJ, Becher C, Kron N, Ostermeier S, Hurschler C, Schofer MD, Tibesku CO, Fuchs-Winkelmann S (2010) Patellofemoral pressure after TKA in vitro: highly conforming vs. posterior stabilized inlays. Arch Orthop Trauma Surg 130(2):191–196. doi:10.1007/s00402-009-0920-y
Insall J, Aglietti P (1980) A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am 62(8):1329–1337
Jacobs WC, Christen B, Wymenga AB, Schuster A, van der Schaaf DB, ten Ham A, Wehrli U (2012) Functional performance of mobile versus fixed bearing total knee prostheses: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 20(8):1450–1455. doi:10.1007/s00167-011-1684-9
Kwon OR, Kang KT, Son J, Kwon SK, Jo SB, Suh DS, Choi YJ, Kim HJ, Koh YG (2014) Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplasty using finite element analysis. J Orthop Res 35(2):338–345. doi:10.1002/jor.22499
Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13(5):365–370. doi:10.1016/j.knee.2006.05.003
Murray DW, Pandit H, Weston-Simons JS, Jenkins C, Gill HS, Lombardi AV, Dodd CA, Berend KR (2013) Does body mass index affect the outcome of unicompartmental knee replacement? Knee 20(6):461–465. doi:10.1016/j.knee.2012.09.017
Ostermeier S, Friesecke C, Fricke S, Hurschler C, Stukenborg-Colsman C (2008) Quadriceps force during knee extension after non-hinged and hinged TKA: an in vitro study. Acta Orthop 79(1):34–38. doi:10.1080/17453670710014734
Ostermeier S, Hurschler C, Stukenborg-Colsman C (2004) Quadriceps function after TKA: an in vitro study in a knee kinematic simulator. Clin Biomech (Bristol, Avon) 19(3):270–276. doi:10.1016/j.clinbiomech.2003.11.006
Ostermeier S, Hurschler C, Windhagen H, Stukenborg-Colsman C (2006) In vitro investigation of the influence of tibial slope on quadriceps extension force after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 14(10):934–939. doi:10.1007/s00167-006-0078-x
Ostermeier S, Stukenborg-Colsman C (2011) Quadriceps force after TKA with femoral single radius. Acta Orthop 82(3):339–343. doi:10.3109/17453674.2011.574564
Palmer SH, Morrison PJ, Ross AC (1998) Early catastrophic tibial component wear after unicompartmental knee arthroplasty. Clin Orthop Relat Res 350:143–148
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605. doi:10.1016/j.otsr.2009.10.006
Sun PF, Jia YH (2012) Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee 19(2):103–106. doi:10.1016/j.knee.2011.01.006
Swedish Knee Arthroplasty Register. Annual Report 2010. Lund
van den Heever DJ, Scheffer C, Erasmus P, Dillon E (2011) Contact stresses in a patient-specific unicompartmental knee replacement. Clin Biomech (Bristol, Avon) 26 (2):159–166. doi:10.1016/j.clinbiomech.2010.09.007
Zeng Y, Shen B, Yang J, Zhou ZK, Kang PD, Pei FX (2013) Is there reduced polyethylene wear and longer survival when using a replacement? A meta-analysis of randomised and non-randomised controlled trials. Bone Joint J 95-B (8):1057–1063. doi:10.1302/0301-620X.95B8.31310
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ettinger, M., Zoch, J.M., Becher, C. et al. In vitro kinematics of fixed versus mobile bearing in unicondylar knee arthroplasty. Arch Orthop Trauma Surg 135, 871–877 (2015). https://doi.org/10.1007/s00402-015-2214-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2214-x