Abstract
Purpose
Unicompartmental knee arthroplasty (UKA) offers clinical and functional advantages over total knee arthroplasty. The aim of this study was to compare the functional recovery of patients with mobile UKA versus fixed-bearing designs by state-of-the-art gait analysis and, in particular, by assessing muscular activity.
Methods
Ten patients with the Oxford (mobile bearing) and ten patients with Optetrak (fixed bearing) UKA were evaluated at a minimum follow-up of 1 year post-operatively by gait analysis, which includes the main time–distance parameters, kinematics and kinetics of the replaced knee, and muscular activity of the main relevant muscles. Twenty healthy young subjects were used as controls.
Results
The mean International Knee Society score was 92.7 ± 11.2 for all 20 UKA knees; for the Oxford UKA, it was 94.1 ± 9.5; and for the Optetrak UKA, it was 91.5 ± 12.9, although follow-up was significantly lower for the latter. Time–distance parameters showed a slower gait in both groups compared with that of controls, and the Oxford group had values closer to the controls. Knee joint flexion was similar to that of controls at initial contact and loading response with no differences between groups. In all patients, the joint moments were smaller to that of controls. Residual abnormalities such as the prolonged rectus femoris activity were present in both designs, and the only difference distinguishing the Optetrak group from the others was the combined co-contraction of the hamstrings.
Conclusions
A good restoration of gait was achieved by most unicompartmental knee patients independently of the UKA design, although some abnormalities persisted in muscle activity around the knee.
Level of evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) for selected patients with intact anterior cruciate ligament (ACL) and unicompartmental osteoarthritis has shown advantages in comparison with total knee arthroplasty [30]. These include smaller skin incision and a minimally invasive surgical technique, more rapid recovery and rehabilitation, smaller overall costs, and potentially normal kinematics and physiological function at the replaced knee because of the preservation of the original joint structures [30].
Currently, two different UKA concepts are available with regard to the polyethylene insert in between the two metal components: one features a mobile bearing, the other an insert fixed to the tibial component. The mobile-bearing design analysed in the present study has fully conforming articular surfaces and a large contact area. This should reduce the contact stress also at the bone–prosthesis interface and result in a low wear penetration rate of the bearing [29]. With this design, a precise alignment and a careful balancing of extension and flexion gaps are essential, to prevent dislocation of the mobile bearing [7]. Fixed-bearing unicompartmental designs are not fully conforming, and this results in higher contact stresses at the articulating surfaces and a higher wear penetration rate [9]; on the other hand, there is no risk of bearing dislocation and an easier surgical technique is claimed [11, 15]. A survivorship rate of 90% at 10 years for fixed bearings and 93% at 15 years for mobile bearings has been reported [30]. However, clinical and functional results from these designs are still controversial [10, 22, 31].
Clinical outcome is usually measured by the traditional score systems, which give only a rough assessment of pain and walking abilities, with a poor ability to discriminate between functional impairments [25]. In this respect, gait analysis has been largely used to measure patients’ function objectively following total knee replacement, particularly providing accurate measurements of sagittal plane kinematics and kinetics [26]. The gait analysis studies on UKA have shown great improvements in the time–distance parameters after surgery [6, 8, 13, 18, 25, 34–37]. A regular biphasic pattern of knee flexion/extension during the stance phase of gait was also observed in most of the patients [8, 18, 34, 37], thus supporting further the findings from both in vitro [27, 28, 33] and fluoroscopy-based in vivo tests [1, 2, 16] that normal knee joint kinematics can be restored in UKA patients. This is probably due to the complete preservation of the cruciate ligaments, in particular the ACL. However, to the authors’ knowledge, no studies have compared joint kinematics and kinetics of mobile-bearing and fixed-bearing designs by complete gait analysis, and, in particular, no studies have explored muscular activation. The retention of the cruciate ligaments, in fact, is supposed to provide not only normal joint kinematics [22], but also physiological muscular activation [8, 13].
The aim of this study was to explore the patterns of knee kinematics (i.e. knee rotations), kinetics (i.e. joint moments), and muscular activity during gait in UKA patients. The first hypothesis was that nearly physiological such patterns can be restored in these patients because of the conservative surgery. Two very different UKA designs were analysed, together with a control group, with the second hypothesis of very similar relevant performances.
Materials and methods
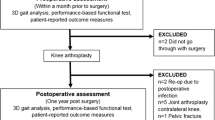
Among all the patients treated at our Orthopaedic Division with medial UKA, 20 patients were included in the study: 10 treated with the Oxford phase II mobile bearing (Biomet, Swindon, England) and 10 with the Optetrak unicondylar fixed bearing (Exactech, Gainsville, Florida). Inclusion in the study was determined by the availability of the patient for a complete gait analysis session at a minimum follow-up of 1 year, in addition to no complications, no comorbidities, and age over 60 years. All patients were treated by the same surgeon. There was a significant difference for follow-up (P < 0.005) because the surgeon implanted the Oxford and the Optetrak designs consecutively over time. Therefore, the follow-up for the Optetrak patients was 12.4 ± 0.7, whereas that of the Oxford group was 46.1 ± 24.8. The 20 patients were divided into two groups according to the UKA design (Table 1). No statistically significant differences were found for age, weight, or height. The criteria for performing UKA rather than total knee arthroplasty were those recommended by Kozinn and Scott [20], i.e., medial osteoarthritis or medial avascular necrosis, intact ACL, range of knee flexion larger than 90°, flexion contracture less than 5°, varus deformity less than 10°, and valgus deformity less than 15°. Standard antero-posterior and medio-lateral radiograms were used to check, respectively, that the lateral compartment was well preserved and that patello-femoral joint was only moderately involved. These patients all had limited pain and a relatively sedentary lifestyle. Furthermore, the patients did not have inflammatory arthritis, haemochromatosis, chondrocalcinosis, haemophilia, patello-femoral joint symptoms, parapatellar tenderness or knee instability in the replaced knee, or symptoms in the contralateral side. In both groups, a minimally invasive approach was used, through an incision from the medial pole of the patella to the medial side of the tibial tuberosity. The technique was performed to ensure an accurate ligament balance, and, in the Oxford UKA, to match extension to flexion gaps and to avoid impingement of the bearing with retained bone or cement throughout the range of flexion. For comparison, a control group of 20 healthy subjects was also analysed (11 men and 9 women, with an average age of 27.9 years).
Clinical–functional score
The International Knee Society (IKS) score [17] was administered to the patients. This score is divided into a knee-rating component, which includes pain, stability and range of motion on a 100-point scale, and a functional assessment component, which includes distance walked, ability to climb stairs, etc. on a 100-point scale. The femoro-tibial angle was measured on weight-bearing antero-posterior radiograms of the knee.
Gait analysis
Complete gait analysis, including simultaneous measurements of kinematics, kinetics and electromyography, was performed on patients and control subjects during level walking. Patients walked with their comfortable shoes at self-selected speed on a 15-m walkway for three successful trials. Marker trajectories were collected by an 8-camera motion system (Vicon Motion System, Oxford, UK), and ground reaction forces from two forceplates (Kistler, Winterthur, Switzerland). A recently proposed [21] and validated [24] protocol was used to calculate pelvic and lower limb joints kinematics and kinetics. This entails positioning and tracking 26 markers placed at anatomical landmarks, which are used to calculate segment and joint rotations and moments in the three anatomical planes. Relevant characteristic parameters were extracted [4] from these time histories, for a quantitative comparison on a statistical basis.
The surface myoelectric signal of the following eight muscles was recorded by the TELEMG system (BTS, Milan, Italy): ipsilateral and contralateral erector spinae, gluteus medius, rectus femoris, lateral and medial hamstrings, tibialis anterior, and gastrocnemius (medial head). Each EMG signal was then processed off-line by means of a statistical detection algorithm to obtain muscle on–off timing [5] in accordance with a previously described procedure [3].
For each gait analysis variable, the means and standard deviations (SD) were taken for the three trials of each patient.
Statistical analysis
To compare gait parameters between the control group and the UKA, both pooled and separated according to the two designs, the unpaired t test was used (P < 0.05). When variances of the groups were not homogeneous, the Mann–Whitney non-parametric test with the exact method for small groups (P < 0.05) was used. All the statistical analyses were performed using SPSS 11.0 (SPSS, Chicago, Illinois, USA).
Results
All UKA patients showed excellent IKS results, with no statistically significant difference between the designs. The mean and standard deviation of the rating component were 92.7 ± 11.2 in the 20 UKA patients, 94.1 ± 9.5 in the Oxford group, and 91.5 ± 12.9 in the Optetrak group. The corresponding figures for the functional assessment were 92.6 ± 13.8, 93.3 ± 8.7, and 92.0 ± 17.7. In particular, the implants were found to be stable in both the sagittal and coronal planes. The coronal plane femoro-tibial angle was 5.4 ± 2.2° for the Oxford group and 1.9 ± 1° for the Optetrak group.
All time–distance parameters from the UKA patients were significantly different from controls (Table 2). Stance duration, on both the treated and contralateral side, was prolonged (P < 0.0005), stride length (P < 0.0005) was shorter and cadence slower (P = 0.015), and consequently walking speed was also lower (P < 0.0005). Comparison between the two designs revealed that the stride length, cadence, and speed in the Oxford group were closer to the corresponding normal values than were those of the Optetrak group.
Kinematic analysis (Table 3) showed that knee flexion in the UKA groups was similar to that of the control group at initial contact and during the loading response phase. Small differences were found in knee extension in mid-stance (P = 0.05), and significant differences only for the maximum knee flexion in swing (P < 0.0005), and for the full range of flexion (P < 0.0005). No significant differences were found between the two UKA groups.
Kinetics analysis (Table 3) revealed that all knee joint moment parameters for the entire UKA group, except the first maximum in extension and the maximum of external rotation, were smaller than those of the control group. Between the two UKA groups, statistically significant difference was found only in the coronal plane, i.e., the Oxford group showed a larger reduction in both the first and second peak of external adduction moment (P = 0.01 and P = 0.004, respectively), compared with the controls.
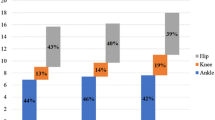
The EMG analysis (Fig. 1) revealed a prolonged activity along the gait cycle of the rectus femoris in the initial stance in about 80% of the Oxford patients and in 100% of the Optetrak patients. The peak of rectus activity at the stance-to-swing transition (about 60% of the cycle) was missing. Nine of the ten patients of the Optetrak group had prolonged activity of lateral hamstrings, in co-contraction with the rectus femoris. Lumbar muscles were also active during swing in a higher number of subjects from the Optetrak group. Finally, eight patients in each group showed a prolonged activity of the tibialis anterior during mid-stance, in many cases associated with a premature activity of the medial gastrocnemius, with no differences between the two UKA groups.
Patterns of muscular activity in the treated leg in the form of On–Off muscle timing percentage: at each sample over the gait cycle (% stride), the percentage of gait trials (three for each patient) with the muscle active (on) in that sample is shown. Patterns from the control and the two UKA groups are superimposed. This is shown for the homolateral (HES) and contralateral erector spinae (CES), gluteus medius (GM), rectus femoris (RF), lateral (LH) and medial hamstrings (MH), tibialis anterior (TA), and gastrocnemius (GAST)
Discussion
The most important finding of the present study was that in UKA patients not only high clinical-functional scores can be obtained, but also excellent functional performances during gait. This was revealed by means of state-of-the-art gait and EMG analyses, and in both of the two UKA designs here analyzed, one being long established with a mobile bearing, and the other being a recently devised fixed-bearing. Despite a slower gait, compared to young controls, the pattern of knee joint flexion did not show considerable abnormalities during the loading response phase, i.e., no such ‘quadriceps-avoidance pattern’ [8] was found. This is considered to be a key parameter for a good functional recovery, the knee in this weight-bearing phase being able thus to absorb the load as supported by the activity of the muscle extensor apparatus, which is subjected to an external flexion moment. In patients with total knee arthroplasty, loss of knee flexion–extension range has been observed, and explained by the small posterior displacement of the femur over the tibial baseplate, probably because of the absence of the ACL [1]. This pattern has been reported in a number of studies and is thought to increase the risk of wear in the polyethylene insert and damage the quadriceps mechanism [32]. In the present UKA patients, normal flexion in the replaced knee was observed, in agreement with other studies [8, 18, 34]. The natural rollback mechanism was also generally restored, guided by the cruciate ligaments, which were preserved, as previously shown by fluoroscopy [16]. This also implies an adequate load absorption mechanism, which might preserve the implant, the residual structures of the knee and the nearby joints from stress and wear [22].
In patients with total knee arthroplasty, a reduced knee flexion during loading response [26], a reduction in the net quadriceps moment [8] and a stiff knee with quadriceps and hamstrings co-contractions [3, 26] have been observed. These have been partially explained by the sacrifice of the ACL, which is preserved in UKA. It has been shown that UKA can result in nearly physiological knee kinematics during walking [8, 34] but more comprehensive measurements were necessary, besides clinical, radiographic, and survivorship data, to show the good functional recovery of this treatment. The present study supports the evidence that good joint function and nearly physiological muscle activity during gait can be achieved in patients undergoing UKA, and this was true in two well-known UKA designs. All this evidence would encourage further the use of UKA with a correct indication, for possible better outcomes than total knee arthroplasty.
The present results also reveal that the replaced knee, after the nearly normal flexion during loading response, seems not be able to extend correctly in late stance, regardless of UKA design. This is consistent with a few studies from the literature [34, 37] but inconsistent with one [13]; the discrepancy, however, might be due to the different gait analysis method used. The strength of the triceps surae is usually considered for this abnormality, as the tibia might not be adequately stabilized during terminal stance while the femur advances over it. Unfortunately, calf strength was not measured in these patients.
The presence of a prolonged rectus activity without co-contraction of the hamstrings found in 8 patients of the Oxford group is a very atypical pattern after total knee replacement [3]. A possible explanation might be a deficient ACL function over time, due to unrecognized degeneration at the time of surgery or deterioration after surgery as previously shown [1]. However, this is not necessarily interpreted as pathologic, as UKA data were compared in the present study with a control group of young subjects and can be misleading. Since there are no other reports in the literature on muscle activity in patients with UKA and age-matched controls, this original finding cannot be discussed comparatively.
In the Optetrak group, the prolonged activity of the rectus femoris was associated with a prevalent lateral hamstrings co-contraction during the initial stance. One explanation for this is that the shorter follow-up might have affected the gait performance. In fact, Kleijn et al. [19] showed that functional recovery in UKA patients progresses beyond 6 months up to 2 years after surgery, with knee flexion range reaching a maximum at one year, whereas quadriceps muscle recovery may take 1 to 2 years to recover due to the pre-operative atrophy secondary to osteoarthritis [32]. It is reasonable to assume that the present Optetrak patients might have been affected by the muscular limitation present before surgery, as also reported by Fuchs [14]. Another possible explanation might be found in the very different concepts behind the UKA designs assessed in the present study. The Optetrak design has never been explored by gait analysis before, and hence no comparison is possible with other similar studies. As in these patients, the muscle co-contraction observed did not seem to limit the knee kinematics during loading response, and hence not aimed at stiffening the knee, it might have been responding to the increased demand for muscle-guided motion. Unlike the Oxford UKA where ligaments are tensioned as a result of balancing flexion and extension gaps [7], in the Optetrak UKA restoring a natural ligament tension is more difficult. In the latter, this may result in an antagonistic muscle action request aimed at stabilizing the joint in activity. Other biomechanical factors intrinsic to the implant can also play a role in this. A high co-contraction around the ankle joint was also present in both groups due to the prolonged activity of the tibialis anterior. Slow gait might be responsible for this, or tibialis anterior activity during stance might be aimed at managing knee loading on the coronal plane, as previously hypothesized for total knee replacement [3]. However, recent literature reveals that the early onset of the gastrocnemius together with the prolonged activity of the tibialis anterior is a recurrent pattern in patients with ACL chronic deficiency, used by the patients, respectively, to stabilize posteriorly the tibia and to control the inversion of the foot, thus causing external rotation of the tibia and stabilizing the knee [23]. Further analyses are required in this respect to understand possible relationships between muscular control and possible ligament efficiency, also with respect to the prosthesis design.
In agreement with the literature [18, 37], the joint moments in the present UKA patients were found to be smaller than those in the control group. It is interesting to note that the external rotation moment during stance in the replaced knee is not altered, thus confirming the mechanism of good load absorption in the loading response phase, where this joint experiences flexion and internal rotation to accommodate for the subtalar joint pronation. The two UKA groups showed a reduced knee adduction moment, with small differences between implants, consistent with the knee alignment measured. Similarly to the literature, the mobile Oxford group showed a more valgus alignment than did the fixed Optetrak group [11].
The present study has some limitations, particularly with regard to the patient populations. The follow-up between the two groups of patients was different. However, the other characteristics of the two groups were very similar (see Table 1 and IKS scores), and it is recognised that 12 months after surgery, the progression of functional recovery in UKA has a plateau; in other words, little additional functional improvement is expected [12, 19, 30]. In addition, the present control group was significantly younger than the two UKA groups, which can also account for the large differences in the speed of progression. However, the present comparisons over gait performances were based on the most possible physiological patterns, particularly for very well-performing patients, as these in fact were.
Conclusion
The present gait analysis study revealed that UKA patients have nearly physiological knee function, in terms of joint flexion, particularly during the loading response phase of walking, kinetics, and also muscular activity. Residual abnormalities were a prolonged rectus femoris activity in both the mobile- and fixed-bearing UKA designs, and a co-contraction of the hamstrings during the stance phase in the fixed-bearing design. Very small differences were found between the two prosthesis designs analysed.
References
Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty 17:1049–1054
Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S (2005) Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports Traumatol Arthrosc 13:551–556
Benedetti MG, Catani F, Bilotta TW, Marcacci M, Mariani E, Giannini S (2003) Muscle activation pattern and gait biomechanics after total knee replacement. Clin Biomech 18:871–876
Benedetti MG, Catani F, Leardini A, Pignotti E, Giannini S (1998) Data management in gait analysis for clinical applications. Clin Biomech 13:204–215
Bonato P, Knaflitz M, D’Alessio T (1998) A statistical method for the measurement of muscle activation intervals from surface myoelectric signal during gait. IEEE Trans Biomed Eng 45:287–299
Borjesson M, Weidenhielm L, Mattsson E, Olsson E (2005) Gait and clinical measurement in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee 12:121–127
Borus T, Thornhill T (2008) Unicompartmental knee arthroplasty. J Am Acad Orthop Surg 16:9–18
Chassin EP, Mikosz RP, Andriacchi TP, Rosenberg AG (1996) Functional analysis of cemented medial unicompartmental knee arthroplasty. J Arthroplasty 11:553–559
Collier MB, Anderson Engh C, McAuley JP, Engh GA (2007) Factors associated with the loss of thickness of polyethylene tibial bearing after knee arthroplasty. J Bone Joint Surg Am 89:1306–1314
Confalonieri N, Manzotti A, Pullen C (2004) Comparison of a mobile with a fixed tibial bearing unicompartmental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee 11:357–362
Emerson RH, Hansborought T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Fisher DA, Dalury DF, Adams MJ, Shipps MR, Davis K (2010) Unicompartmental and total knee arthroplasty in the over 70 population. Orthopedics 33(9):668
Fuchs S, Tibesku CO, Frisse D, Genkinger M, Laaß H, Rosenbaum D (2005) Clinical and functional comparison of uni- and bicondylar sledge prostheses. Knee Surg Sports Traumatol Arthrosc 13:197–202
Fuchs S, Frisse D, Laass H, Thorwesten L, Tibesku CO (2004) Muscle strength in patients with unicompartmental arthroplasty. Am J Phys Med Rehabil 83:650–654
Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH (2004) Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Sci Direct 11:379–384
Hanson GR, Moynihan AL, Suggs JF, Kwon YM, Johnson T, Li G (2009) Kinematics of medial unicondylar knee arthroplasty: an in vivo investigation. J Knee Surg 22:237–242
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rational of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jefferson RJ, Whittle MW (1989) Biomechanical assessment of unicompartmental knee arthroplasty, total condylar arthroplasty and tibial osteotomy. Clin Biomech 4:232–242
Kleijn LL, van Hemert WL, Meijers WG, Kester AD, Lisowski L, Grimm B, Heyligers IC (2007) Functional improvement after unicompartmental knee replacement: a follow-up study with a performance based knee test. Knee Surg Sports Traumatol Arthrosc 15:1187–1193
Kozinn SC, Scott RD (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71A:145–150
Leardini A, Sawacha Z, Paolini G et al (2007) A new anatomically based protocol for gait analysis in children. Gait Posture 26:560–571
Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13:365–370
Lindstrom M, Fellander-Tsai L, Wredmark T, Henriksson M (2010) Adaptations of gait and muscle activation in chronic ACL deficiency. Knee Surg Sports Traumatol Arthrosc 18:106–114
Manca M, Leardini A, Cavazza S, Ferraresi G, Marchi P, Zanaga E, Benedetti MG (2010) Repeatability of a new protocol for gait analysis in adult subjects. Gait Posture 32:282–284
Mattsson E, Olsson E, Broström L-Å (1990) Assessment of walking before and after unicompartmental knee arthroplasty. Scand J Rehab Med 22:45–50
McClelland JA, Webster KE, Feller JA (2007) Gait analysis of patients following total knee replacement: a systematic review. Knee 14:253–263
Patil S, Colwell CW Jr, Ezzet KA, D’Lima DD (2005) Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Joint Surg Am 87:332–338
Price AJ, Oppold PT, Murray DW, Zavatsky AB (2006) Simultaneous in vitro measurement of patellofemoral kinematics and forces following Oxford medial unicompartmental knee replacement. J Bone Joint Surg Br 88:1591–1595
Psychoyios V, Crawford RW, O’Connor JJ, Murray DW (1998) Wear of congruent meniscal bearings in unicompartmental knee arthroplasty. J Bone Joint Surg Br 80-B:876–882
Saccomanni B (2010) Unicompartmental knee arthroplasty: a review of literature. Clin Rheumatol 29:339–346
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta analysis. Orthop Traumatol Surg Res 95:599–605
Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG (2010) Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res 468:2460–2468
Suggs JF, Li G, Park SE, Sultan PG, Rubasi HE, Freiberg AA (2006) Knee biomechanics after UKA and its relation to the ACL-A robotic investigation. J Orthop Res 24:588–594
Webster KE, Wittwer JE, Feller JA (2003) Quantitative gait analysis after medial unicompartmental knee arthroplasty for osteoarthritis. J Arthroplasty 6:751–759
Weidenhielm L, Olsson E, Broström LA, Börjesson-Hederström M, Mattsson E (1993) Improvement in gait one year after surgery for knee osteoarthrosis: a comparison between high tibial osteotomy and prosthetic replacement in a prospective randomized study. Scand J Rehabil Med 25:25–31
Weinstein JN, Andriacchi TP, Galante JO (1986) Factors influencing walking and stair climbing following unicompartmental knee arthroplasty. J Arthroplasty 1:109–115
Whittle MW, Jefferson RJ (1989) Functional biomechanics assessment of the Oxford meniscal knee. J Arthroplasty 4:231–243
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catani, F., Benedetti, M.G., Bianchi, L. et al. Muscle activity around the knee and gait performance in unicompartmental knee arthroplasty patients: a comparative study on fixed- and mobile-bearing designs. Knee Surg Sports Traumatol Arthrosc 20, 1042–1048 (2012). https://doi.org/10.1007/s00167-011-1620-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1620-z